Abstract
Objective
Radiofrequency (RF) medial branch neurotomy is an effective management of lumbar facet syndrome. However, pain may recur after period of time. When pain recurs, it can be repeated, but the successful outcome and duration of relief from repeated procedures are not clearly known. The objective of this study was to determine the success rate and duration of pain relief from repeated radiofrequency medial branch neurotomy for lumbar facet syndrome.
Methods
A retrospective review of medical records was done on 60 consecutive patients, from March of 2006 to February of 2009, who had an initial successful RF neurotomy but subsequently underwent repeated procedures due to recurrence of pain. All procedures were done in carefully selected patients after at least two responsive medial branch nerve blocks. C-arm fluoroscopic guide, impedance, sensory and motor threshold monitoring tools were used for the precise placement of electrodes. Responses of repeated procedures were compared with initial radiofrequency neurotomy for success rates and duration of pain relief.
Results
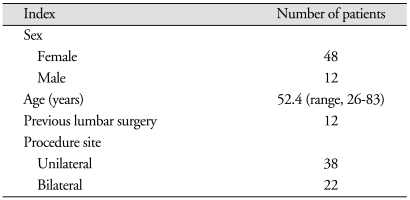
There were 48 females and 12 males. Mean age was 52.4 years (range, 26-83). RF medial branch neurotomy was done on one side in 38 and both sides in 22 patients, each covering at least three segments. Average visual analog scale at last procedure was 6.8. Twelve patients had previous lumbar operations, including 4 patients with instrumentations. Fifty-five patients had two procedures and five patients had three procedures. Mean duration of successful pain relief (> 50% of previous pain for at least 3 months period) after initial radiofrequency neurotomy was 10.9 months (range, 3-28) in 51 (85%) patients. From repeated procedures, successful pain relief was seen in 50 (91%) patients with average duration of 10.2 months (range, 3-24). Five patients had third procedure, which was successful in 4 (80%) patients with mean duration of 9.8 months (range, 5-16). This was not statistically different from initial results. There were no permanent neurological complications from the procedures.
Conclusion
Results of this study indicate that the frequency of success and durations of relief from repeated RF medial branch neurotomy for lumbar facet syndrome are similar to initial results that provided relatively prolonged period of pain relief without major side effects. Each procedure seems to provide successful pain relief for about 10 months in more than 85% of carefully selected patients when properly done.
Keywords: Facet syndrome, Zygapophyseal joint denervation, Radiofrequency neurotomy, Repeat operation, Outcome
INTRODUCTION
Chronic low back pain can be induced by many causes and may occur any time of life. According to the International Association for the Study of Pain7), the facet (zygapophyseal) joints are the sources of common cause of chronic low back pain (15% to 45% patients). It is synovial joint with cartilage surface which is encapsulated with fibrous sac called a joint capsule. Each joint has a superior and an inferior articular process, filled with fat or synovial fluid. As any synovial joint, the facet joint can be a source of pain11). The hypertrophic changes of the zygapophyseal processes secondary to injury or inflammatory change and disc degeneration may lead to lumbar spinal nerve irritation, and may cause low back pain3,13). When such pain is associated with buttock pain, pseudoradicular type pain in posterior thigh or inguinal pain, tenderness on paravertebral regions corresponding to zygapophyseal joints, and aggravation of pain from maneuvers that maximally irritate the joints (e.g., modified Patric tests) or from transitional movements (e.g., getting up or standing from sitting positions) it is can be considered as "facet syndrome". The diagnosis is made clinically and by excluding other origins of low back pain4). However, the most useful and confirmatory diagnosis is made with diagnostic facet joint block or on its innervating nerves (medial branch of posterior primary ramus) if there is a significant decrease in pain (50% or more)9,11,17). To control the nociceptive transmission of nerve impulses, several techniques have been developed and introduced14).
Shealy13) was the first to use radiofrequency (RF) for denervation of the lumbar facet joints. Since then, fluoroscopic radiofrequency medial branch neurotomy has been commonly used as an effective treatment for chronic back pain of such type5,8). The treatment technique has been advanced and modified since then. In 1999, van Kleef et al.16) reported the results of improved the effectiveness of RF medial branch neurotomy from double blind controlled study. Dreyfuss et al.1) also reported modest result of RF medial branch neurotomy under strict guidelines.
When pains recur after initial successful RF medial branch neurotomy, these studies recommend repeating RF medal branch neurotomy. Schofferman et al.10) reported results of repeated radiofrequency neurotomy that showed a mean duration of relief of 10.5 months and more than 85% of successful rate in 20 patients. In this study, we included 60 patients who have undergone repeated RF medial branch neurotomy with modified technique and compared with previous results to determine the success rate and duration of pain relief.
MATERIALS AND METHODS
A retrospective review on medical records of 60 consecutive patients, from March of 2006 to February of 2009, who had an initial successful radiofrequency medial branch neurotomy but subsequently underwent repeated procedures due to recurrence of pain was performed. The inclusion criteria were; 1) low back and buttock pain over 6 months of duration, 2) absence of neurological deficits, 3) pseudoradicular pain down to posterior thigh above the knee, 4) tenderness on paravertebral area corresponding to zygapophyseal joins, and 5) more that 50% of pain relief from at least two diagnostic nerve blocks on medial branches of posterior primary ramus. The study excluded patients who had coagulopathy, infection and compensation related to industrial or traffic accident. Previously, all patients had tried medication, physical therapy and other forms of treatments without satisfactory pain relief. Lumbar magnetic resonance imaging (MRI) and plain X-ray radiograph were performed in every patient to rule out other possible causes of low back pain.
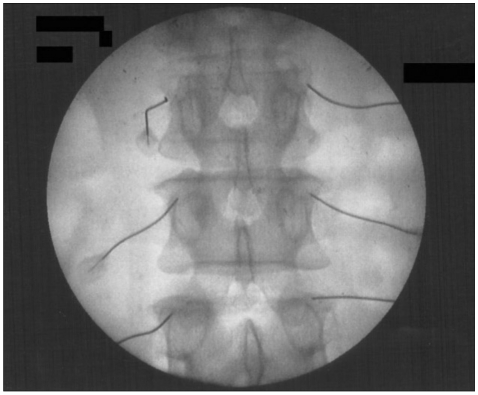
RF medial branch neurotomy was performed by single operator using a modified technique proposed by Dreyfuss et al.1). With the patient prone on the operative table, a C-arm image intensifier was used for adequate position of electrode. Neurostimulation and RF treatment were performed with a RF generator (RFG-3B, Radionics, Burlington, MA) in which a thermocouple with a 10 cm long electrode needle was used (22 gauge, 5 mm active tip for thoraco-lumbar region, Radionics) to access the medial branch of posterior primary ramus (Fig. 1). Upon placement of the needle, the electrical impedance was checked to confirm the continuity of electrical circuit, to detect any short circuits and to make sure the electrode is in contact with targeted nerves. The range of impedance is 300-600 Ω when in extra-dural tissue, 1000 Ω at spinal cord and 200 Ω in disc space. The impedance from posterior primary ramus nerve usually ranges from 500-700 Ω and the best result from RF treatment has been obtained at 600 ± 50 Ω from our previous experience, especially when such impedance is noted with onset of sharp pain response from the patient. Therefore, several adjustments were made to obtain such responses with ideal impedance. After confirmation of correct placement, sensory and motor stimulation were tested at 50 Hz and 2 Hz. First, stimulation at 50 Hz to ensure proximity of electrode to sensory fibers, then 2 Hz stimulation to detect muscle contractions in the multifidus muscle. The thresholds sensory stimulation was between 0.3 V to 0.9 V and motor threshold within 1.5 times of sensory stimulation. When multifidus muscle contraction did not occur in this range, the needle was repositioned. However, leg muscle contraction did not occur below 2 V. The radiofrequency thermal energy was applied gradually, 5-10 seconds every 10℃ increment usually from 50℃, for patients to tolerate the heat and pain. Final lesionings were made at 80℃ for 60 to 90 seconds until disappearance of pain. Several patients required a small dose of local anesthetic before final lesioning due to intolerability of pain. The successful RF medial branch neurotomy was defined as 50% or greater relief of pain and patients who had below 50% relief of pain after initial RF medial branch neurotomy were excluded. Each repeated RF medial branch neurotomy was compared with initial result and graded as success or failure. Duration of pain relief and post procedure visual analog scale (VAS) was also recorded.
Fig. 1.
Fluoroscopic radiograph shows the electrode positions of rodiofrequency medial branch neurotomy.
RESULTS
Sixty patients were eligible for assessment, and underwent repeated RF medial branch neurotomy. The overall demographics of followed through participants in this study are summarized in Table 1. There were 48 females and 12 males. Mean age was 52.4 years (range, 26-83). No patient had any permanent or major complications. All completed follow-up visit evaluation that consisted of 2-page questionnaire. RF medial branch neurotomy was performed on one side in 38 patients and both sides in 22 patients. Twelve patients had history of lumbar spine surgery, including 4 patients with instrumentation.
Table 1.
Overall demographics of patients
After initial RF medial branch neurotomy, 51 (85%) patients showed "successful" responses and 9 (15%) showed "fail" responses. Mean duration of pain relief was 10.9 months (range, 3-28), in 75% of patients at 12 months. 55 patients had second procedures; there were 50 (91%) successes and 5 failures. Mean duration of pain relief was 10.2 months (range, 3-24) in 85% of patients. Of five patients who underwent third procedures 4 (80%) showed successful responses and 1 failure. Mean duration of pain relief in these patients was 9.8 months (range, 5-16) in 60% of patients with 6.8 ± 1.9 of VAS twelve weeks after the last procedure. In overall, successful pain relief was 88% and mean duration of relief was 10.5 months (Table 2).
Table 2.
Success rates and pain relief duration of repeated RF medial branch neurotomy
RF : rediofrequency
There were no complications, such as motor weakness or sensory changes, from either from first procedures or repeated procedures except 6 patients (3 from first and 3 from repeated procedures) who experienced transient worsening of pain on back and buttock areas and paresthesia for several days. These symptoms were spontaneously relieved without residual neurological deficits after about one to two weeks. However, it is recommended that patients should be prescribed for analgesics to take when pain occurs during this period of time.
DISCUSSION
The present study demonstrates that a high percentage of patients (88%) treated with RF medial branch neurotomy have a good to excellent pain relief for a prolonged period (> 10 months) of time in patients diagnosed as facet syndrome similar or better to other reported series1,8,10,16,17). The current study also shows that repeated RF medial branch neurotomy from recurrent pain after successful pain relief is also effective in about 85% of patients that were also similar to previous reports6,10,15,17). There were no neurological complications from repeated procedures as in first cases.
In previous studies, Dreyfuss et al.1) and van Kleef et al.16) had mentioned the efficacy of repeat RF medial branch neurotomy. In 2004, Schofferman et al.10) reported usefulness of repeated RF medial branch neurotomy about 85% in 20 patients with successful pain relief and duration of relief of 10.5 months. For the result of our study, we analyzed 60 patients and showed 85% of successful rate from repeated procedure with a mean duration of 10.5 months. Although the mean duration of pain relief was similar to other series, our study showed a somewhat higher successful rate. One possible explanation is more strict patient selection as described earlier. Briefly, all patients were evaluated with at least two nerve blocks after through physical and neurological examination followed by lumbar MRI and plain X-ray radiographs for excluding other origins of low back pain. The other would be technical consistency. In this study, a single well experienced operator performed all procedures with same method. In all procedures, every patient was monitored with impedance, sensory and motor stimulation to confirm the precise location and may have several repositioning in order to obtain the parameters that showed the best results from our previous experience Also, RF lesionings were continued usually for 60-90 seconds (or longer) or longer until the disappearance of evoked pain that were similar to previous pain experienced by patients.
We included 12 patients who had undergone lumbar spine surgery or instrumentation. Some studies have shown no correlation between anatomical changes or deformity of facet joint and facet joint pain2,12). But, it seems that there may be some correlation with postoperative condition and facet joint pain. If we exclude 12 previously operated patients from our series, a higher successful rate would be expected.
The results of the current study have some limitations. We have not included the functional status of the patients in addition to the degrees of pain. The reason for this was that the majority of our patients were elderly females (although a wide range of age being 26-83), and most of these patients were not involved in active work environment. Functional impairments (usually activities of daily living) seem to be mostly related to the severity of pain and significant pain relief in turn usually improves such functional impairments. Unfortunately, such changes or correlation in statistical evaluation from functional improvement and pain relief were not evaluated in this study. Further study is underway to evaluate the long-term efficacy of this type of treatment in a larger population with regards to degrees of pain relief and functional improvement as well as patient satisfaction. Another weakness lies in our inability to control for other treatments or procedures that could have contributed to the patient's overall improvement in function and pain by the time follow-up was obtained. In addition, some of the improvements seen may be attributable to spontaneous relief or placebo effect. These factors are inherent in any non-controlled, retrospective study in patients with pain.
Current study also had some strength. To our knowledge, there has not been a report on a carefully selected number of patients with strict guidelines as in our study with a prolonged period of follow up evaluation without any lost patients. Also, all procedures were performed by one experienced specialist using same technique and protocol that could provide consistent results.
CONCLUSION
Repeated RF medial branch neurotomy provided substantial pain relief in majority of patients for relatively prolonged period of time. Thus, it may be considered to be an effective treatment in selected patients with recurrent pain from facet joints and its surrounding structures (so called "facet syndrome") unresponsive to other forms of therapy. However, further prospective study in a large group, controlled, blinded trial in a longer period of time should be followed.
References
- 1.Dreyfuss P, Halbrook B, Pauza K, Joshi A, McLarty J, Bogduk N. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophysial joint pain. Spine (Phila Pa 1976) 2000;25:1270–1277. doi: 10.1097/00007632-200005150-00012. [DOI] [PubMed] [Google Scholar]
- 2.Gofeld M, Jitendra J, Faclier G. Radiofrequency denervation of the lumbar zygapophysial joints : 10-year prospective clinical audit. Pain Physician. 2007;10:291–300. [PubMed] [Google Scholar]
- 3.Hooten WM, Martin DP, Huntoon MA. Radiofrequency neurotomy for low back pain : evidence-based procedural guidelines. Pain Med. 2005;6:129–138. doi: 10.1111/j.1526-4637.2005.05022.x. [DOI] [PubMed] [Google Scholar]
- 4.Joy H, Ha SK, Kim SH, Lim DJ, Park JY, Suh JK. Prognostic factors of percutaneous radiofrequency neurotomy on the posterior primary ramus. J Korean Neurosurg Soc. 2003;33:51–55. [Google Scholar]
- 5.Kornick C, Kramarich SS, Lamer TJ, Todd Sitzman B. Complications of lumbar facet radiofrequency denervation. Spine (Phila Pa 1976) 2004;29:1352–1354. doi: 10.1097/01.brs.0000128263.67291.a0. [DOI] [PubMed] [Google Scholar]
- 6.Manejias EM, Hu J, Tatli Y, Lutz GE. Lumbar zygapophysial joint radiofrequency denervation : a long-term clinical outcome study. HSS J. 2008;4:180–187. doi: 10.1007/s11420-008-9082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Merskey H, Bogduk N. Classification of chronic pain : descriptions of chronic pain syndromes and definitions of pain terms. ed 2nd. Seattle: International Association for the Study Pain. Press; 1994. [PubMed] [Google Scholar]
- 8.North RB, Han M, Zahurak M, Kidd DH. Radiofrequency lumbar facet denervation : analysis of prognostic factors. Pain. 1994;57:77–83. doi: 10.1016/0304-3959(94)90110-4. [DOI] [PubMed] [Google Scholar]
- 9.Park J, Park JY, Kim SH, Lim DJ, Kim SD, Chung HS. Long term results from percutaneous radiofrequency neurotomy on posterior primary ramus in patients with chronic low back pain. Acta Neurochir Suppl. 2006;99:81–83. doi: 10.1007/978-3-211-35205-2_16. [DOI] [PubMed] [Google Scholar]
- 10.Schofferman J, Kine G. Effectiveness of repeated radiofrequency neurotomy for lumbar facet pain. Spine (Phila Pa 1976) 2004;29:2471–2473. doi: 10.1097/01.brs.0000143170.47345.44. [DOI] [PubMed] [Google Scholar]
- 11.Schulte T, Pietilä T, Heidenreich J, Brock M, Stendel R. Injection therapy of lumbar facet syndrome : a prospective study. Acta Neurochir (Wien) 2006;148:1165–1172. doi: 10.1007/s00701-006-0897-z. discussion 1172. [DOI] [PubMed] [Google Scholar]
- 12.Schwarzer AC, Wang SC, O'Driscoll D, Harrington T, Bogduk N, Laurent R. The ability of computed tomography to identify a painful zygapophysial joint in patients with chronic low back pain. Spine (Phila Pa 1976) 1995;20:907–912. doi: 10.1097/00007632-199504150-00005. [DOI] [PubMed] [Google Scholar]
- 13.Shealy CN. Percutaneous radiofrequency denervation of spinal facets. Treatment for chronic back pain and sciatica. J Neurosurg. 1975;43:448–451. doi: 10.3171/jns.1975.43.4.0448. [DOI] [PubMed] [Google Scholar]
- 14.Sim WS, Lee AR. Radiofrequency lumbar medial branch denervation using bipolar probe in patient with facet joint syndrome. J Korean Pain Soc. 2004;17:153–158. [Google Scholar]
- 15.Vallejo R, Benyamin RM, Kramer J, Stanton G, Joseph NJ. Pulsed radiofrequency denervation for the treatment of sacroiliac joint syndrome. Pain Med. 2006;7:429–434. doi: 10.1111/j.1526-4637.2006.00143.x. [DOI] [PubMed] [Google Scholar]
- 16.van Kleef M, Barendse GA, Kessels A, Voets HM, Weber WE, de Lange S. Randomized trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine (Phila Pa 1976) 1999;24:1937–1942. doi: 10.1097/00007632-199909150-00013. [DOI] [PubMed] [Google Scholar]
- 17.Zotti MG, Osti OL. Repeat percutaneous radiofrequency facet joint denervation for chronic back pain : a prospective study. Journal of Musculoskeletal Pain. 2010;18:153–158. [Google Scholar]