Summary
Telecardiology allows for the remote specialist interpretation of electrocardiographic recordings via telephone transmission. It has the potential to change the way cardiac care is being delivered in the primary care setting. This review discusses the current status of cardiac care in the community, and highlights how telecardiology can help support general practitioners in the diagnosis and management of acute and chronic cardiac disease, as well as provide the potential for screening opportunities in particular patients at risk. Also reviewed is the success of recent trials of a telecardiology service in the north west of England. Thanks to developments in technology and ever decreasing costs, telecardiology has the potential to save time, money and lives. Telecardiology, it would seem, is set to revolutionize cardiac care in the community, making savings and bridging the gap between primary and secondary care.
Introduction
Electrocardiography (ECG) is a useful diagnostic tool in the diagnosis and management of ischaemic heart disease and cardiac arrhythmia, and its availability in the primary care setting is now common. Routine availability of ECG at the primary care level can facilitate early referrals to secondary care, while reducing unnecessary referrals where appropriate. Telecardiology has been in use in one form or another for just over a century, and has multiple applications.1 We believe that recent advances in telecardiology provide an accurate, convenient and cost-effective solution for ECG testing in the primary care setting.
The ECG in primary care
The availability of both ECG equipment and interpretational skills are not universal at the primary care level. Obtaining rapid, accurate ECG reports with specialist input remains a challenge. Recent studies have found significant heterogeneity in the level of interpretational skill among the general practitioners (GPs) assessed.2–4 For example, one study found that many primary care professionals assessed were unable to diagnose atrial fibrillation.2 The lack of reliable ECG testing and reporting under these circumstances may mean that some cardiac conditions are being missed.
There are several reasons for having reliable ECG testing at the primary care level. Although the majority of patients with acute coronary syndrome present to secondary care, some may present to their GP.5–7 Under these circumstances, ECG testing is mandatory and reliable interpretation of the result may inform not just the diagnosis, but also the need for urgent referral. This is of particular importance for atypical presentations. From the perspective of diagnosing and managing cardiac disease, opportunistic screening programmes may detect ECG changes such as atrial fibrillation or left ventricular hypertrophy in high-risk individuals with conditions such as hypertension and dyslipidaemia. It may also aid the early detection of silent myocardial ischaemia in specific patient groups at high risk of coronary artery disease, e.g. diabetics or patients with chronic kidney disease. There is vast potential, and the idea that ECGs should be put to widespread use in the assessment and monitoring of heart failure and chest pain of recent onset is now reflected in guidelines published by the National Institute for Health and Clinical Excellence (NICE).8,9
Modern telecardiology in practice – how it works
Recent advances in telecardiology have allowed for rapid and reliable remote ECG interpretation. Using a specialized hand-held ECG unit (Figure 1), the user takes a 12-lead ECG in the usual manner. The device encodes the ECG into sound and, at the touch of a button, plays this over a telephone line to the telecardiology service. This sound is decoded electronically and displayed as a full 12-lead ECG on screen at the telecardiology centre. It can then be immediately interpreted by cardiologists and specialist nurses. Within minutes, an oral report is provided by telephone. A full written report is then sent to the general practice by email or fax. This is also stored securely at the telecardiology centre, meaning that future ECGs from the same patient can be compared and contrasted with ease.
Figure 1.
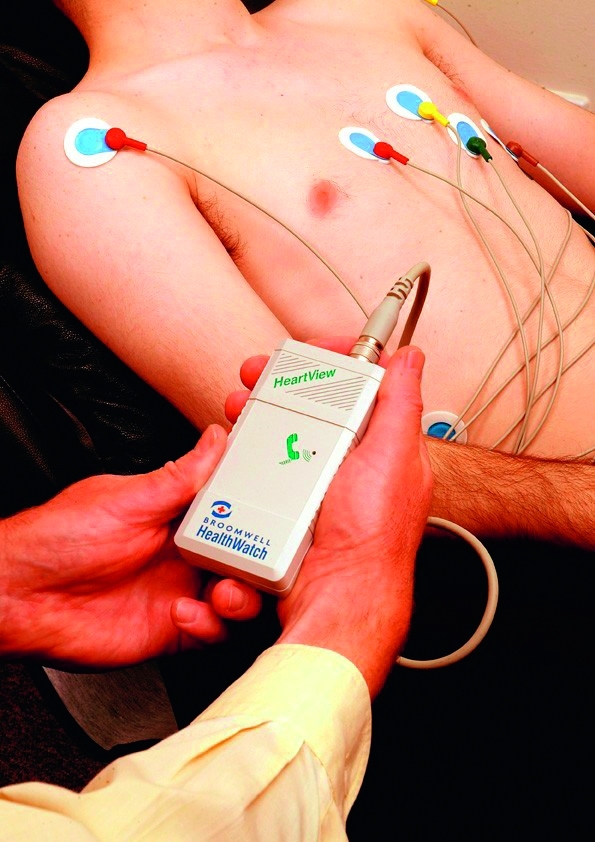
An example of a 12-lead telecardiology device in use. Reproduced with permission from Broomwell Healthwatch
In addition to the 12-lead ECG device, there is also a 1-lead variant. These devices are available in the form of a watch (Figure 2), which may be worn on the wrist quite comfortably for long periods at a time. The patient can then activate a recording at the touch of a button. This recording is stored on the watch, and may be transmitted electronically to the telecardiology centre via a device kept at the GP's practice.
Figure 2.
An example of a 1-lead tele-enabled ECG watch. Reproduced with permission from Broomwell Healthwatch
Empowering GPs
Telecardiology provides diagnostic support for GPs, enabling them to safely manage more of their own patients.5 Although contemporary guidelines mandate early specialist assessment of chest pain patients based on an appropriate clinical history and clinical examination, the ECG still has a powerful role in primary care, not least as a screening tool. As such, it seems that telecardiology has the potential to empower GPs to help make a more complete clinical assessment for cardiac patients. Also, it has been observed by some that bridging the gap between primary and specialist care improves the GP's own knowledge base, thus improving the standard of cardiac care provided.1,7
Reducing referrals to secondary care
Despite recent public awareness campaigns, some patients still present to their GP with the symptoms of acute coronary syndrome. Furthermore, fewer than 50% of all patients referred on to Accident & Emergency (A&E) will actually have acute coronary syndrome as their final diagnosis.10 Indeed, Klinkman et al. showed that 75% of all analysed chronic chest pain referrals from GPs to cardiologists were due to non-cardiac causes, being either musculoskeletal or non-specific in origin.11 Be that as it may, current NICE guidelines stipulate that patients with suspected acute coronary syndrome and current chest pain must be referred on to emergency secondary care, even in the presence of a normal ECG.9 The significant financial constraints on the health service currently make strategies to reduce referral to secondary care attractive.
There is evidence to suggest that the use of a telecardiology service can reduce the number of unnecessary hospital referrals and admissions. In 2002, a study by Molinari et al. looked at 100 GPs over the course of one month. One hundred and thirty-four out of 456 patients presenting with cardiac-type symptoms were suspected to have genuine coronary events. However, through the use of a telecardiology service, it was confidently demonstrated that 84 out of the 134 patients with suspected coronary events had no ECG abnormalities whatsoever. As such, unnecessary hospitalization was avoided. Based on an average hospital stay of three days per patient, and a daily hospitalization cost of $2000 per patient, the service was estimated to have saved $504,000.6
Accepting that the ECG represents only part of the clinical assessment of chest pain, these results demonstrate telecardiology's potential to reduce costs.
Reducing missed diagnoses
In the aforementioned study, Molinari et al. found that out of 322 patients deemed not to have had an acute coronary event, 56 patients (17%) were actually found to have had one following subsequent ECG testing and a tele-consultation with a cardiologist. Thirty-eight of these 56 patients were subsequently diagnosed with an acute coronary syndrome.6
As far as the detection and monitoring of chronic heart disease is concerned, and as already mentioned, there are many groups of patients who would benefit from opportunistic 12-lead ECGs. In terms of arrhythmia detection in particular, the 1-lead ECG watch holds enormous potential through its novel design. These devices enable the patient to activate cardiac monitoring as and when they feel unwell. This is unlike the current 24-hour Holter tape method, the application of which might not coincide with the next bout of arrhythmia. Indeed, there is evidence to suggest that this method is superior, as a study found that hand-held event recorders picked up arrhythmias in 70% of the patients assessed, compared to 35% in the Holter-monitored cohort.1 Monitoring patients in this way would improve not only the detection of suspected arrhythmias in the first place, but indeed the monitoring of arrhythmia after the commencement of medical treatment or post-atrial fibrillation ablation.
Reducing door-to-balloon time
For the minority of patients presenting to their GP rather than to A&E or to paramedics, telecardiology plays a significant role in allowing the timely diagnosis of ST-segment elevation myocardial infarction (STEMI) prior to hospitalization. This is of crucial importance, as a pre-hospital diagnosis of a STEMI reduces door-to-balloon time. Brown et al. demonstrated that the pre-hospital ECG was ‘the single most important factor’ in reducing door-to-balloon time.12 As the cardiologist's maxim goes, ‘time equals muscle’, and as such, reducing door-to-balloon time greatly decreases patient mortality.13,14 Terkelsen et al. demonstrated that a pre-hospital diagnosis of STEMI via telecardiology reduced door-to-balloon time to 38 minutes, as opposed to 81 minutes for those without a pre-hospital diagnosis. This stark difference was attributed to the fact that patients with a definite STEMI diagnosis were transferred directly to the cardiac catheterization lab, and the fact that the attending physician could be apprised prior to the patient's arrival.15 Even in London, where paramedics are now trained to read their own ECGs, this service could provide crucial support in their clinical decision-making, and help further reduce door-to-balloon time.
Convenience, mobility and ease of use
Telecardiology devices are small, mobile and usually operated by a single button. They can be moved easily from room to room within a practice, and can be taken out into the community. They can support the service of those GPs on-call and would prove indispensible to those practicing in remote areas. From a patient's perspective, it is also more convenient and comfortable to undergo ECG testing in one's own home or local GP practice, as opposed to in a hospital.16 These devices allow for a more convenient approach in investigating and managing heart disease, benefiting healthcare providers and improving patient compliance.
UK pilot studies and subsequent approval
Telecardiology in the primary care setting has already been piloted in the UK with great success. This is due to improvements in the technology, as well as affordability.17,18
In a recent audit conducted by the Greater Manchester and Cheshire Cardiac and Stroke Network, 29 GP practices trialled a local telecardiology service (Broomwell Healthwatch). It was demonstrated that out of the 24,541 patients assessed by the service, secondary care referrals were prevented in 65.8% of cases. It was estimated that the savings to the NHS were in excess of £300,000. These registrar or consultant cardiologist level ECG reports were provided in written form within 2 hours, whereas most practices in the UK previously would have had to wait anywhere between 1 and 7 days for their ECG analyses.18
Similar findings were echoed in a report by the Lancashire and Cumbria NHS trust, which also piloted the system.17 Specifically, the report estimated that when extrapolated to England as a whole, the implementation of this system would save £45 million per annum in preventing unnecessary hospital referrals. Furthermore, the ‘unbundled’ nature of the service would enable a trust to relate exact expenditure to the overall outcome. In these times of economic hardship, the ability to weigh up expenditure against results is all the more appealing. These findings have prompted primary care trusts in the northwest to roll this service out for every practice that opts for it. In addition, the NHS Technology Adoption Centre has identified the wider introduction of telecardiology in primary care as one of its priorities.19
Limitation of evidence and future directions
Despite positive results from many individual studies, telecardiology needs to be subjected to the kind of Cochrane-standard meta-analyses normally employed to assess the effectiveness of any medical intervention. It may take some time for these studies to materialize, and as such, it may take some time before the technology is more widely accepted.
Conclusion
Telecardiology, by bringing expert ECG interpretation to primary care, has the potential to save time, money and lives. It empowers GPs, providing a robust diagnostic tool to facilitate the management of cardiac patients in the community. Both physicians and patients benefit in terms of ease of access, speed of diagnosis, efficiency of management and the freeing up of resources. There remains a need for further large randomized controlled trials and cost-efficacy data to evaluate these findings on a wider scale. In conclusion, telecardiology has the potential to revolutionize the way various heart conditions are managed in the primary care setting. Telecardiology is here to stay and may represent a step change for the use of further clinical tools that harness information technology to augment patient care.
Footnotes
DECLARATIONS —
Competing interests WB worked temporarily doing ECG downloads and administration at Broomwell Healthwatch during the summer of 2009. He has no shares or other financial interest in the company. DB and RR have no competing interests to declare
Funding None
Ethical approval Not applicable
Guarantor RR
Contributorship WB is the conceiver, and collaborated with DB in researching and drafting the article. RR provided new areas of discussion, made crucial revisions and approved the finalversion with WB and DB
Acknowledgements
None
References
- 1.Scalvini S, Glisenti F. Centenary of tele-electrocardiography and telephonocardiography – where are we today? J Telemed Telecare 2005;11:325–30 [DOI] [PubMed] [Google Scholar]
- 2.Mant J, Fitzmaurice DA, Hobbs FD, et al. Accuracy of diagnosing atrial fibrillation on electrocardiogram by primary care practitioners and interpretative diagnostic software: analysis of data from screening for atrial fibrillation in the elderly (SAFE) trial. BMJ 2007;335:380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeyaseelan S, Struthers AD, Goudie BM, Pringle SD, Sullivan FM, Donnan PT. The accuracy of ECG screening by GPs and by machine interpretation in selecting suspected heart failure patients for echocardiography. Br J Cardiol 2006;13:216–18 [Google Scholar]
- 4.van Weert HCPM. Diagnosing atrial fibrillation in general practice. The combination of a clinical history, clinical signs, and an ECG will pick up most cases. BMJ 2007;335:355–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scalvini S, Zanelli E, Conti C, et al. Assessment of prehospital chest pain using telecardiology. J Telemed Telecare 2002;8:231–6 [DOI] [PubMed] [Google Scholar]
- 6.Molinari G, Reboa G, Frascio M, et al. The role of telecardiology in supporting the decision-making process of general practitioners during the management of patients with suspected cardiac events. J Telemed Telecare 2002;8:97–101 [DOI] [PubMed] [Google Scholar]
- 7.Molinari G, Valbusa A, Terrizzano M, et al. Nine years' experience of telecardiology in primary care. J Telemed Telecare 2004;10:249–53 [DOI] [PubMed] [Google Scholar]
- 8.The National Collaborating Centre for Chronic Conditions Chronic Heart Failure. National clinical guideline for diagnosis and management in primary and secondary care. London: NICE; 2003 [Google Scholar]
- 9.National Clinical Guideline Centre for Acute and Chronic Conditions NICE Clinical Guideline 95. Chest pain of recent onset. Assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin. London: NICE; 2010 [Google Scholar]
- 10.Capewell S, McMurray J. ‘Chest pain – please admit’: is there an alternative? A rapid cardiological assessment service may prevent unnecessary admissions. BMJ 2000;320:951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klinkman MS, Stevens D, Gorenflo DW. Episodes of Care for Chest Pain: A Preliminary Report from MIRNET. J Fam Pract 1994;38:345–52 [PubMed] [Google Scholar]
- 12.Brown JP, Mahmud E, Dunford JV, Ben-Yehuda O. Effect of prehospital 12-lead electrocardiogram on activation of the cardiac catheterization laboratory and door-to-balloon time in ST-segment elevation acute myocardial infarction. Am J Cardiol 2008;101:158–61 [DOI] [PubMed] [Google Scholar]
- 13.McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol 2006;47:2180–6 [DOI] [PubMed] [Google Scholar]
- 14.Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 2000;283:2941–7 [DOI] [PubMed] [Google Scholar]
- 15.Terkelsen CJ, Norgaard BL, Lassen JF, et al. Telemedicine used for remote prehospital diagnosing in patients suspected of acute myocardial infarction. J Intern Med 2002;252:412–20 [DOI] [PubMed] [Google Scholar]
- 16.Lieberman J. How telemedicine is aiding prompt ECG diagnosis in primary care. Br J Community Nurs 2008;13:123–6 [DOI] [PubMed] [Google Scholar]
- 17.Lancashire and South Cumbria Cardiac Network Delivering Benefits for Patients and the NHS in Lancashire & Cumbria. A report for commissioners. Manchester: NHS North West; 2009 [Google Scholar]
- 18.Albouaini K, Jones A, Rowe M, Shtrosberg S, Egred M. The use of telemedicine for ECG interpretation in primary care. Heart 2009;95 Suppl. 1:A1–A87: A34–A35 [Google Scholar]
- 19.12 Lead ECG in Primary Care using Telemedicine. Manchester: NHS Technology Adoption Centre; See http://www.technologyadoptionhub.nhs.uk/?page_id=769 (last checked 17 September 2010) [Google Scholar]



