Abstract
Soybean-derived phosphatidylserine (Soy-PS) is a phosphatidylserine made from soybean lecithin by enzymatic reaction with L-serine. A double-blind, randomized controlled study was conducted to investigate the effects of Soy-PS on the cognitive functions of the elderly Japanese subjects with memory complaints. Seventy-eight elderly people with mild cognitive impairment (50–69 years old) were randomly allocated to take Soy-PS (100 mg, 300 mg/day) or placebo for 6 months. As a result, there was no difference in blood markers and vital signs during Soy-PS treatment and any side effect caused by Soy-PS treatment was not observed. Neuropsychological test scores were similarly increased in all groups including placebo group. However, in the subjects with relatively low score at baseline, the memory scores in PS treated groups were significantly increased against the baseline, while those of placebo group remained unchanged. And the memory improvements in Soy-PS-treated groups were mostly attributed to the increase in delayed verbal recall, a memory ability attenuated in the earliest stage of dementia. In conclusion, Soy-PS used in this study is considered as safety food ingredient and 6 months of Soy-PS supplementation could improve the memory functions of the elderly with memory complaints.
Keywords: phosphatidylserine, soybean, elderly, memory functions, delayed verbal recall
Introduction
Phosphatidylserine (PS) is a member of the membrane phospholipids that is especially abundant in the brain. Because of its presence in the brain, effects of PS on the central nervous system have been widely investigated [1–5]. Several clinical studies in the US and Europe have shown that PS extracted from bovine cortex (BC-PS) improves the cognitive function of the elderly [6–10] including Alzheimer’s disease patients [8, 9] and people with age-associated memory impairment (AAMI) [10]. However, the use of BC-PS in medicine or dietary supplements is now discouraged because of the risk of bovine spongiform encephalopathy (BSE) [11]. In addition, only about 3 grams of PS can be obtained from one bovine cortex, which is too small for inexpensive supply.
Efforts to overcome these problems have led to the development of soybean-derived PS (Soy-PS), a BSE risk-free PS that is enzymatically made from soybean lecithin [12]. Even though the acyl-groups of Soy-PS are quite different from that of BC-PS, studies using drug-induced amnesic and aged rodents have suggested that the effects of Soy-PS on cognitive function are identical to that of BC-PS [13–16].
However, the results of clinical studies using Soy-PS are controversial. In 1995, Gindin et al. [17] first reported a clinical study of Soy-PS, where Soy-PS treatment (300 mg/day for 3 months) on elderly people with AAMI improved their Wechsler Memory test scores, especially in the components of the test that evaluated visual memory. In their study, the effect of Soy-PS was evident only in the subgroup of subjects that had higher pre-treatment scores. Crook et al. [18] reported that Soy-PS (300 mg/day for 12 weeks) was effective in improving memory functions, such as memorizing names and faces, of elderly people with AAMI. Schreiber et al. [19] also reported similar results that Soy-PS was most effective on memorizing faces.
Jorissen et al. [20] performed a double-blind placebo-controlled study to evaluate the efficacy of two different doses of Soy-PS (300 or 600 mg/day for 12 weeks) on the elderly with AAMI. Although various aspects of cognitive function including memory, information processing speed, selective attention and planning were measured, no difference was found between placebo and Soy-PS treated groups even with the higher dosage. Thus, it is still controversial whether Soy-PS is effective for the elderly with memory impairment. Furthermore, there has been no clinical study that evaluates the effects of PS on memory impairment using Japanese subjects.
To clarify whether Soy-PS is beneficial for cognitive function of the elderly, we conducted a preliminarily open-trial test in 2005 and found that 12 weeks of Soy-PS treatment (300 mg/day) on elderly people with mild memory impairment improved their scores on the revised version of Hasegawa’s dementia scale (HDS-R) [21], a general test used for diagnosis of dementia in Japan. Improvement was especially evident in the delayed 3 words recall (DWR) subtest. In addition, the effect of Soy-PS on DWR was maintained for 12 weeks after the treatment period was over. Based on these results, we next planned a double-blind, placebo-controlled clinical study.
The present study was designed as a double-blind, placebo-controlled trial to evaluate the efficacy of Soy-PS (100 mg or 300 mg/day for 6 months) on the Japanese elderly with mild memory impairment. For the selection of subjects with mild memory impairment, we used the Rivermead behavioral memory test (RBMT) [22], which focuses on evaluating memory functions, especially everyday memory. The treatment period of Soy-PS was set to 6 months, with an additional 3-month follow-up period to see whether the effects of Soy-PS would be maintained after discontinuing its intake.
Materials and Methods
Subjects
Men and women living in the Tokyo metropolitan area, ranging from 50 to 69 years old, with subjective memory complaints were recruited from the volunteer bank of clinical research organization (Huma R&D Co. Ltd., Tokyo). Prior to the screening with neuropsychological tests, a preliminary assessment was conducted at the recruiting process to evaluate objective memory loss. Specifically, the DWR subtest of HDS-R was done over the phone, and those with 3 to 5 points out of 6 were selected. For further screening, people who passed this preliminary assessment took part in three neuropsychological tests (RBMT, HDS-R and Mini-Mental State Examination: MMSE [23]) and a medical interview, and those who fulfilled the selection criteria became the subjects for this clinical study.
To screen out people with severe cognitive disorder who need medical treatment, the selection criteria were set so as to include people with mild memory impairment (RBMT standard profile score<22) while excluding those with possible dementia (HDS-R<21, MMSE<24).
Procedures for this study were approved by the institutional review board of the testing agency, Tokyo Heart Center (Tokyo, Japan). All subjects gave a written informed consent before entering the study.
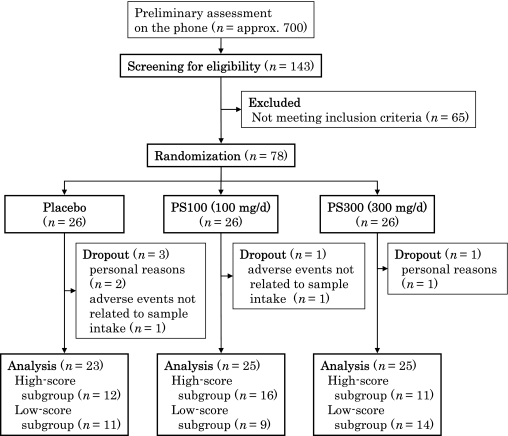
In total, 143 out of approximately 700 volunteers passed the preliminary assessment on the phone, and 78 of them fulfilled the selection criteria. Out of 78 subjects who entered the study, 73 completed the study and 5 dropped out (n = 3 in placebo, n = 1 in 100 mg Soy-PS and n = 1 in 300 mg Soy-PS). The reasons for dropout were either private circumstances or health problems not related to PS treatment. The design of this study and trial profile are shown in Fig. 1.
Fig. 1.
The study design and trial profile.
Study design
The study was designed as a randomized, double-blind, placebo-controlled, parallel-group trial. The subjects were randomly divided into three groups (n = 28 in each group), all similar in average age, sex, education year, neuropsychological test score, geriatric depression scale (GDS) [24] score and everyday memory checklist (EMC) score (Tables 1 and 5).
Table 1.
Baseline characteristics of each treatment group
| group | Placebo | PS100 | PS300 |
|---|---|---|---|
| Number of subjects | 23 | 25 | 25 |
| Number of male | 12 | 12 | 14 |
| Number of female | 11 | 13 | 11 |
| Age | 59.6 ± 1.1 | 59.1 ± 1.1 | 59.6 ± 1.0 |
| Education (year) | 14.2 ± 0.4 | 13.4 ± 0.4 | 13.8 ± 0.4 |
Values are mean ± SEM. The subjects in PS100 and PS300 groups took 100 mg/d and 300 mg/d of Soy-PS for 6 months, respectively. Placebo group took soybean lecithin containing no PS.
Within one month after the screening session, subjects started taking their respective test samples: placebo, 100 mg Soy-PS (PS100) or 300 mg Soy-PS (PS300), daily for 6 months. Six months of PS treatment was followed by a 3-month follow-up period during which subjects took no samples. For all measurements, the screening values were used as baseline values.
The following examinations were conducted at baseline, after 6 months of PS treatment and after 3 months of follow-up period: HDS-R and MMSE for evaluating cognitive function, GDS for evaluating depressive state, and blood/urine tests for evaluating safety. In addition, RBMT and EMC were conducted at baseline, at 1, 3 and 6 months of PS treatment and after 3 months of follow-up.
Treatment
Food-grade Soy-PS product (PS-20L, Yakult Honsha Co. Ltd., Japan) produced from soybean lecithin by enzymatic transphosphatidylation reaction was used in this study [25]. Test samples were taken in the form of soft gelatin capsules (200 mg of content per capsule). Subjects took 3 capsules after each meal, a total of 9 capsules per day, for 6 months. The timing of Soy-PS intake was decided according to previous papers [19, 20].
Nine capsules of PS300 contained 300 mg PS, 663 mg phospholipids other than PS (PL), 702 mg middle-chain triglycerides (MCT) and 135 mg vitamin E (VE). Nine capsules of PS100 contained 100 mg PS, 863 mg PL, 702 mg MCT and 135 mg VE. Nine capsules of placebo contained 963 mg PL, 702 mg MCT and 135 mg VE.
To prevent degradation of Soy-PS, a portion of the test samples was sent to the subjects every month and was kept under refrigeration at home.
Outcome measures
Primary outcome measures were cognitive functions assessed by HDS-R, MMSE and RBMT. Secondary outcomes were self-rating memory function assessed by EMC and depressive state assessed by GDS. Blood and urine parameters were also assessed for safety evaluation.
RBMT
RBMT is a standardized and validated test for memory functions [22]. It consists of 12 subtests for evaluating everyday memory such as of personal event, people’s names, newspaper articles and places visited. The Japanese version of RBMT was developed by Kazui et al. [26] in 2002. Standardized profile score is obtained by assigning a score of 0, 1, or 2 to each of the 12 subtests, summing up to a maximum total score of 24 points. Degree of memory impairment is categorized into 4 classes according to the standardized profile score; 0–9: severely impaired, 10–16: moderately impaired, 18–21: poor memory, >21: normal. Four parallel forms (A, B, C and D) of the test were used in the present study to avoid practice or learning effects.
HDS-R
HDS-R is a neuropsychological battery commonly used for diagnosis of dementia in Japan [27], along with MMSE. Those who score less than 21 points out of 30 are diagnosed as “possible dementia”. The test assesses orientation, memory, attention and verbal fluency. We especially focused on the DWR subtest, because Soy-PS was most effective on that subtest in our preliminary study [21]. In DWR, a subject is presented with 3 unrelated words and is later asked to recall them. For each word, the subject is given 2 points for voluntarily recalling the word, and 1 point for recalling the word with a hint (e.g. “vehicle” for the word “car” or “animal” for the word “dog”). Two lists of 3 words were prepared and the list was alternately used in this study to minimize practice effect.
EMC
EMC is a questionnaire developed together with RBMT for evaluating difficulties in daily life caused by memory impairment [28]. It consists of a list of 13 memory problems or difficult situations that likely happen in daily life. Occurrence of each problem or situation is rated from 0 (none) to 3 (always), with a maximum score of 39 points.
Safety
Medical interview by a physician was conducted at every evaluation point. Blood and urine tests were done at baseline, end of PS treatment (6 months) and 3 months after the end of treatment. Blood pressure and heart rate were also measured as vital signs.
Data analysis
Data analyses were conducted according to the protocol for statistical analysis pre-determined before key-opening. Neuropsychological tests, EMC and GDS scores were analyzed by Steel’s multi-comparison test against the baseline score (within group) or against placebo (between groups). Blood parameters and vital signs were analyzed by Dunnett’s multi-comparison test against placebo group for each evaluation point.
Stratified analyses based on RBMT score at baseline were also conducted. Since the average score of healthy Japanese adults in their 40s and 50s is reported to be 22.0 ± 2.0 points [27], the score below 1.5 standard deviation from the average (= 19 points) was used as the stratification criteria. Regarding stratified analyses, changes in score against the baseline were used in order to correct for initial differences among the groups. SAS 8.2 for Windows was used for statistical analyses, with significance set at p<0.05.
Safety of Soy-PS was evaluated by the deviation from the normal range of blood and urine parameters, and its clinical significance was judged by a physician.
Results
Safety
Throughout the test period, no adverse event was observed in relation to sample intake. There was also no clinically significant change in hematological and biological blood parameters in all groups (Tables 2 and 3). Although a significant difference in blood glucose level at 6 month between placebo and PS100 group appeared, such difference was not observed at higher dose (PS300) and therefore it is considered clinically insignificant. Vital signs (Table 4) and urine parameters (glucose, protein, occult blood and pH; data not shown) didn’t show any significant changes.
Table 2.
Changing in hematological blood parameters during the test period
| 0 month (baseline§) |
6 months (treatment) |
9 months (follow-up) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Placebo (n = 23) | PS100 (n = 25) | PS300 (n = 25) | Placebo (n = 23) | PS100 (n = 25) | PS300 (n = 25) | Placebo (n = 23) | PS100 (n = 25) | PS300 (n = 25) | |
| White blood count (×109/L) | 5.8 (1.3) | 6.2 (1.4) | 6.1 (1.1) | 5.5 (1.2) | 5.8 (1.2) | 5.3 (1.2) | 5.6 (1.2) | 6.0 (1.4) | 5.7 (1.3) |
| Platelet count (×1010/L) | 24.1 (5.3) | 24.7 (5.9) | 24.3 (4.8) | 23.8 (6.1) | 24.2 (5.2) | 22.8 (4.9) | 23.8 (5.7) | 24.8 (5.0) | 23.5 (5.1) |
| Red blood count (×1012/L) | 4.5 (0.4) | 4.5 (0.3) | 4.6 (0.3) | 4.4 (0.3) | 4.4 (0.3) | 4.5 (0.3) | 4.4 (0.3) | 4.4 (0.4) | 4.5 (0.3) |
| Hemoglobin (×10 g/L) | 13.8 (1.0) | 13.7 (1.0) | 13.7 (1.0) | 13.5 (1.0) | 13.4 (1.1) | 13.5 (1.2) | 13.4 (0.8) | 13.5(1.3) | 13.5 (1.2) |
| Hematocrit (%) | 42.9 (2.8) | 42.5 (2.9) | 42.7 (2.8) | 42.0 (2.8) | 41.6 (2.9) | 42.0 (2.9) | 41.3 (2.3) | 41.4 (3.5) | 41.8 (3.1) |
Values are means (standard deviation). §The values at screening were used as baseline values. Subjects started taking the samples within one month after screening. The follow-up period consisted of 3 months after finishing the 6 months of sample intake, during which subjects took no sample.
Table 3.
Changing in biological blood parameters during the test period
| 0 month (baseline§) |
6 months (treatment) |
9 months (follow-up) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Placebo (n = 23) | PS100 (n = 25) | PS300 (n = 25) | Placebo (n = 23) | PS100 (n = 25) | PS300 (n = 25) | Placebo (n = 23) | PS100 (n = 25) | PS300 (n = 25) | |
| AST (units/L) | 25.3 (15.3) | 24.0 (6.6) | 22.2 (9.3) | 26.1 (18.7) | 23.2 (6.6) | 22.8 (7.5) | 24.0 (14.6) | 21.6 (5.1) | 21.2 (8.5) |
| ALT (units/L) | 30.7 (31.2) | 24.7 (15.6) | 23.0 (14.0) | 26.7 (26.1) | 20.2 (8.0) | 23.3 (13.3) | 26.2 (24.5) | 22.2 (8.9) | 22.1 (11.7) |
| Alkaline phosphatase (units/L) | 225.7 (56.0) | 212.8 (51.8) | 230.1 (45.7) | 228.3 (61.2) | 220.6 (53.5) | 214.2 (41.2) | 220.2 (60.1) | 218.7 (47.1) | 215.4 (45.1) |
| Lactose dehydrogenase (units/L) | 191.7 (39.6) | 197.5 (37.0) | 187.2 (23.7) | 187.4 (40.9) | 183.9 (24.7) | 180.6 (26.0) | 191.5 (41.9) | 193.1 (25.6) | 189.1 (18.9) |
| γ-GTP (units/L) | 33.9 (17.8) | 29.7 (17.5) | 34.9 (30.6) | 32.4 (21.1) | 27.8 (19.8) | 32.8 (31.4) | 30.6 (18.9) | 27.9 (18.0) | 30.8 (27.8) |
| Creatine phosphokinase (units/L) | 121.6 (54.8) | 166.3 (115.1) | 115.3 (57.5) | 125.1 (41.4) | 149.8 (114.1) | 116.5 (56.4) | 128.2 (55.9) | 175.0 (153.7) | 113.5 (45.7) |
| Creatinine (mg/dL) | 0.7 (0.1) | 0.8 (0.2) | 0.7 (0.2) | 0.7 (0.1) | 0.7 (0.2) | 0.7 (0.2) | 0.7 (0.1) | 0.8 (0.1) | 0.7 (0.2) |
| Blood urea nitrogen (mg/dL) | 14.9 (2.9) | 14.7 (3.6) | 14.5 (2.6) | 15.3 (3.4) | 15.1 (4.1) | 14.3 (2.8) | 15.7 (3.7) | 15.9 (3.7) | 15.6 (3.1) |
| Uric acid (mg/dL) | 5.2 (1.3) | 5.7 (1.4) | 4.9 (1.3) | 5.3 (1.5) | 5.5 (1.4) | 5.1 (1.4) | 5.2 (1.4) | 5.6 (1.5) | 4.9 (1.4) |
| HDL-cholesterol (mg/dL) | 65.5 (14.7) | 71.9 (14.7) | 65.1 (14.8) | 65.2 (15.3) | 72.1 (14.6) | 65.1 (11.5) | 63.3 (16.1) | 69.3 (13.6) | 63.2 (13.5) |
| LDL-cholesterol (mg/dL) | 141.0 (38.2) | 128.3 (25.9) | 134.3 (34.7) | 130.5 (29.1) | 127.7 (25.4) | 142.3 (36.9) | 130.9 (31.6) | 126.3 (28.7) | 134.2 (31.9) |
| Triglyceride (mg/dL) | 111.9 (60.8) | 89.6 (34.8) | 116.1 (63.6) | 121.6 (92.0) | 104.7 (56.5) | 113.0 (48.0) | 124.0 (103.7) | 99.8 (35.5) | 125.7 (73.9) |
| Blood glucose (mg/dL) | 91.3 (10.7) | 86.2 (10.8) | 87.5 (6.1) | 94.7 (13.3) | 86.9 (7.5)# | 89.6 (8.7) | 94.4 (11.3) | 91.5 (9.4) | 93.2 (11.0) |
Values are means (standard deviation). §The values at screening were used as baseline values. Subjects started taking the samples within one month after screening. The follow-up period consisted of 3 months after finishing the 6 months of sample intake, during which subjects took no sample. #p<0.05 vs placebo group (Dunnett’s multi-comparison test). AST; Asparate amino transferase, ALT; Alanine transaminase.
Table 4.
Changing in vital signs during the test period
| 0 month (baseline§) |
6 months (treatment) |
9 months (follow-up) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Placebo (n = 23) | PS100 (n = 25) | PS300 (n = 25) | Placebo (n = 23) | PS100 (n = 25) | PS300 (n = 25) | Placebo (n = 23) | PS100 (n = 25) | PS300 (n = 25) | |
| Diastolic pressure (mm Hg) | 84.1 (10.6) | 82.2 (12.9) | 85.2 (11.3) | 72.7 (13.8) | 71.1 (10.9) | 71.3 (11.0) | 69.0 (12.5) | 71.8 (10.7) | 68.4 (10.0) |
| Systolic pressure (mm Hg) | 129.1 (16.5) | 124.8 (18.8) | 128.2 (14.4) | 123.9 (19.8) | 118.7 (14.7) | 122.9 (14.9) | 123.3 (16.8) | 121.1 (15.4) | 122.6 (13.8) |
| Heart rate (bpm) | 70.0 (7.7) | 72.4 (9.7) | 70.6 (7.6) | 71.1 (10.2) | 71.7 (9.5) | 71.7 (11.0) | 71.7 (8.0) | 74.1 (9.0) | 72.1 (9.3) |
Values are means (standard deviation). §The values at screening were used as baseline values. Subjects started taking the samples within one month after screening. The follow-up period consisted of 3 months after finishing the 6 months of sample intake, during which subjects took no sample.
Cognitive functions
Table 5 shows the score changes in RBMT. The scores significantly increased against the baseline in all 3 groups, with no difference between Soy-PS and placebo groups at any evaluation point. In stratified analysis based on the subjects’ degree of memory impairment at baseline, there was still no difference between placebo and Soy-PS groups either in the high-score subgroup (RBMT = 19 or more) or the low-score subgroup (RBMT<19) (data not shown).
Table 5.
Results of the neuropsychological tests and the questionnaires of memory and mood
| Group | 0 month (baseline§) | 1 month (treatment) | 3 months (treatment) | 6 months (treatment) | 9 months (follow-up) | |
|---|---|---|---|---|---|---|
| RBMT | Placebo | 18.3 ± 0.52 | 18.3 ± 0.91 | 20.4 ± 0.57** | 22.2 ± 0.46*** | 22.2 ± 0.48*** |
| PS100 | 18.4 ± 0.59 | 19.4 ± 0.44 | 20.1 ± 0.44 | 22.3 ± 0.29*** | 22.6 ± 0.24*** | |
| PS300 | 18.0 ± 0.49 | 19.5 ± 0.44 | 19.1 ± 0.50 | 21.6 ± 0.32*** | 21.6 ± 0.41*** | |
| HDS-R | Placebo | 28.0 ± 0.38 | — | — | 29.1 ± 0.25* | 28.5 ± 0.29 |
| PS100 | 27.8 ± 0.42 | — | — | 29.2 ± 0.22* | 29.2 ± 0.19* | |
| PS300 | 27.4 ± 0.32 | — | — | 28.4 ± 0.31* | 28.6 ± 0.35** | |
| MMSE | Placebo | 27.9 ± 0.38 | — | — | 28.5 ± 0.37 | 28.2 ± 0.35 |
| PS100 | 27.7 ± 0.39 | — | — | 29.0 ± 0.26* | 29.2 ± 0.29** # | |
| PS300 | 27.6 ± 0.39 | — | — | 28.0 ± 0.30 | 28.2 ± 0.35 | |
| EMC | Placebo | 29.1 ± 1.20 | 26.8 ± 1.13 | 26.1 ± 1.12 | 24.6 ± 0.90** | 25.1 ± 1.09* |
| PS100 | 28.8 ± 1.24 | 28.0 ± 1.26 | 27.8 ± 1.49 | 27.4 ± 1.25 | 27.2 ± 1.46 | |
| PS300 | 28.7 ± 1.04 | 27.0 ± 0.97 | 26.3 ± 1.04 | 26.0 ± 1.02 | 24.6 ± 0.98* | |
| GDS | Placebo | 10.7 ± 1.05 | — | — | 7.1 ± 0.91* | 5.2 ± 0.81*** |
| PS100 | 10.7 ± 1.10 | — | — | 8.7 ± 1.21 | 7.1 ± 1.02* | |
| PS300 | 11.4 ± 1.51 | — | — | 8.9 ± 1.38 | 8.1 ± 1.35 | |
Values are mean ± SEM. §The values at screening were used as baseline values. Subjects started taking the samples within one month after screening. The follow-up period consisted of 3 months after finishing the 6 months of sample intake, during which subjects took no sample. *p<0.05, **p<0.01, ***p<0.001 vs baseline, #p<0.05 vs placebo group (Steel’s multi-comparison test).
The total score of HDS-R increased during the treatment period in all 3 groups, with no significant difference among the groups (Table 5). However, after the 3-month follow-up period, the score of the placebo group dropped back to its baseline score, while the scores of 100PS and 300PS groups were both maintained at a high level.
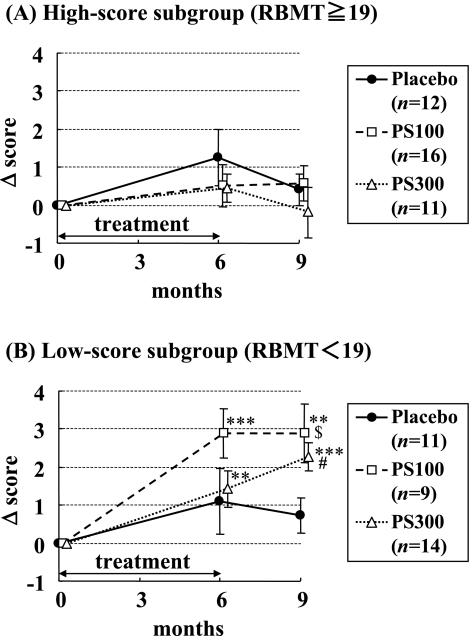
In the high-score subgroup, there was almost no score change in the total score of HDS-R throughout the trial (Fig. 2(A)). In contrast, total score of HDS-R in the low-score subgroup significantly increased against the baseline by Soy-PS treatment (Fig. 2(B)). There was a significant difference between placebo and 300PS groups after 3 months of follow-up (p<0.05). The difference between placebo and 100PS also showed a significant trend (p = 0.05).
Fig. 2.
Effect of Soy-PS on HDS-R performance in high-score and low-score subgroups. Subjects were divided into two subgroups based on their baseline RBMT score. (A) High-score subgroup (RBMT score = 19 or more). (B) Low-score subgroup (RBMT score<19). Values are means ± SEM and shown as changes in score against the baseline. **p<0.01, ***p<0.001 vs baseline, $p<0.1, #p<0.05 vs placebo group (Steel’s multi-comparison test).
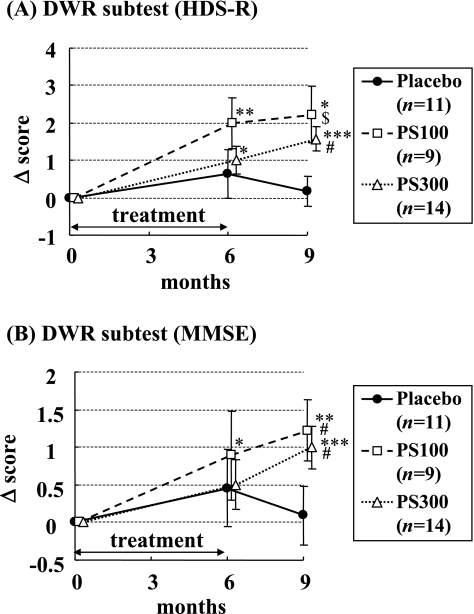
Fig. 3(A) shows the DWR score of HDS-R in the low-score subgroup. The scores of Soy-PS treated groups increased significantly against the baseline, and there were significant differences between placebo and both Soy-PS groups after 3 months of follow-up (p<0.05 for 300PS, p = 0.09 for 100PS). The magnitude of the score change in DWR was quite similar to that of total score (Fig. 2(B)). It is apparent that the change in total score was mainly attributed to the change in DWR subtest score. In fact, there were no significant changes in other subtest scores of HDS-R (data not shown).
Fig. 3.
Effect of Soy-PS on DWR subtest of HDS-R and MMSE in the low-score subgroup (RBMT score<19 at baseline). (A) DWR subtest of HDS-R. (B) DWR subtest of MMSE. Values are means ± SEM and shown as changes in score against the baseline. *p<0.05, **p<0.01, ***p<0.001 vs baseline, $p<0.1, #p<0.05 vs placebo group (Steel’s multi-comparison test).
Although the degree of change was smaller, the same trend was observed in the DWR subtest of MMSE (Fig. 3(B)). The score significantly increased against the baseline only in Soy-PS treated groups, and there were significant differences between placebo and Soy-PS groups (p<0.05 for both 100PS and 300PS). There was almost no change in other subtest scores of MMSE (data not shown).
Subjective changes in memory and mood
Both GDS and EMC scores showed a gradual decrease in all 3 groups, but there was no significant difference among the groups at any evaluation point (Table 5).
Discussion
This double-blind, placebo-controlled study is the first clinical trial which demonstrates that Soy-PS has positive effects on cognitive performance in Japanese subjects with memory complaints.
The effect of Soy-PS was dominant in verbal list recall tests such as the DWR of HDS-R and MMSE. This result reinforces our preliminary study in which the DWR score of HDS-R notably improved by Soy-PS treatment for 3 months [21]. The improving effects of PS on verbal list recall tests have also been consistently observed in many previous studies [29]. For example, a large clinical study of 494 elderly patients with moderate to severe cognitive decline showed that taking 300 mg of BC-PS daily for 6 months significantly improved their performance on the word list recall test [7]. The effect of BC-PS on list recall test was also observed in a study of subjects with AAMI [10]. The result of our present study is well consistent with these previous studies of BC-PS.
On the other hand, Jorissen et al. [20] reported that Soy-PS treatment was ineffective for word list recall. There are differences in study design such as the selection criteria for subjects and the duration of treatment, and what has caused the contradictory result is unclear. Nonetheless, we demonstrated that Soy-PS is also effective on the word list recall as BC-PS.
It has been reported that delayed verbal recall is the most effective cognitive domain for discriminating the earliest stage of dementia (early Alzheimer’s disease and mild cognitive impairment) from normal aging [30, 31]. Therefore the present result that Soy-PS was effective on delayed verbal recall tests suggests that Soy-PS is effective for treating the earliest stage of dementia. The scores of the subtests of HDS-R and MMSE other than the verbal delayed recall were already high at baseline. Thus, Soy-PS is probably more suitable for subjects with memory complaints rather than for subjects with advanced dementia who need medical treatment.
RBMT was also conducted to evaluate the effects of Soy-PS on everyday memory. RBMT includes subtests for evaluating facial recognition and name-face association, which have been reported to improve by PS treatment [18, 19]. However, the effect of Soy-PS on such tests was not observed in the present study. One of the reasons may be that the subjects already marked high scores at baseline and there was no room for further improvement. Since RBMT is intended for people with certain memory impairment, its level of difficulty was perhaps not appropriate for the subjects of this study whose memory functions were nearly normal.
Ceiling effects were also observed in HDS-R and MMSE. As mentioned above, the score of each subtest other than DWR was already high at baseline and there was no room for improvement. Consequently, the effect of Soy-PS on HDS-R and MMSE was only apparent in the low-score subgroup. The effects of Soy-PS may be observed more clearly by using a more sensitive neuropsychological test that enables the detection of subtle or mild memory impairment.
In this study, we tested two dosages of Soy-PS, 100 and 300 mg/day, to determine the optimal amount of intake for the elderly with memory complaints. The memory-improving effect of Soy-PS was equally observed in both groups. Although it is unclear whether taking 100 or 300 mg/day of Soy-PS for a period of less than 6 months exerts the same effect, Crook et al. [18] have reported that 100 or 300 mg/day of Soy-PS intake improved memory functions after 3 weeks and 12 weeks of treatment.
We did not measure blood PS levels in the present study, but some pharmacokinetics studies show that orally administrated PS can be rapidly absorbed and carried to the brain through the blood brain barrier [32]. Our previous observation that the intracerebroventricular injection of Soy-PS improved memory impairment of amnesic mice [15] suggests that Soy-PS could function in the brain directly.
Another study has shown that the oral administration of Soy-PS ameliorated the memory impairment of aged rats [16]. In these animals the acetylcholine release and Na+, K+-ATPase activity of the synaptosome were also improved. This suggests the involvement of cholinergic transmission, energy metabolism or the status of membrane potential of nerve cells in the mechanism of PS action. It is also reported that PS inhibited lipid peroxidation induced by inflammatory oxidants derived from neutrophil myeloperoxidase [33]. PS also decreased the production of reactive oxygen species from microglia induced by amyloid β peptide [34]. The anti-oxidative and/or anti-inflammatory properties of PS may be important for its nootropic mechanism. It is interesting to mention that astaxanthin, a potent antioxidant, improved delayed recall of subjects with memory complaints [35].
The effect of Soy-PS became more evident after the 3-month follow-up period rather than just after 6 months of Soy-PS treatment. A similar result has been reported by Amaducci et al., [8] who evaluated the effects of BC-PS (200 mg/day for 3 months) on the cognitive function of 142 Alzheimer’s disease patients. In their study, the effect of PS was more evident after the post-treatment follow-up period rather than immediately after 3 months of PS treatment. They proposed that PS may cause structural neuronal changes rather than transient metabolic changes, and therefore the beneficial effect might be maintained even after cessation of treatment.
As a supportive evidence, it has been reported that prolonged oral PS treatment elicits structural neuronal changes in aged rats [36]. In summary, the dendritic spine density of aged rats treated with BC-PS was maintained at the same level as that of young rats, whereas non-treated aged rats showed a significant decrease in dendritic density, with a mean loss of about 10%. It is unclear if such structural changes occurred in the subjects of our present study, but prolonged effects of PS have also been shown by other clinical studies using BC-PS, such as in AAMI subjects [10] and in early Alzheimer’s disease patients [9].
There is a concern that the placebo sample used in this study contained some components that have been reported to have a memory-improving function, such as phosphatidylcholine [37], MCT [38] and VE [39]. Although the amount of intake was supposedly much lower than the effective dosage of these components, there is a possibility that the placebo sample actually improved memory function by interacting synergistically and eliciting transient metabolic changes.
Conclusions
The oral administration of Soy-PS for 6 months improved memory function, especially delayed recall, in the elderly with memory complaints. This effect was equally observed at both low dose (100 mg/day) and high dose (300 mg/day). The safety of Soy-PS was also confirmed. Since delayed recall is thought to be one of the cognitive functions impaired at the earliest stage of dementia, Soy-PS may serve as a desirable supplement for preventing dementia development in people with memory complaints. In the future, the memory-improving effects of Soy-PS may be indicated more clearly by reconsidering the study design.
Acknowledgment
We thank M. Takada and C. Takahashi for helpful assistance during the preparation of this article.
References
- 1.Wheeler K.P., Whittam R. ATPase activity of the sodium pump needs phosphatidylserine. Nature. 1970;225:449–450. doi: 10.1038/225449a0. [DOI] [PubMed] [Google Scholar]
- 2.Bruni A., Toffano G., Leon A., Boarato E. Pharmacological effects of phosphatidylserine liposomes. Nature. 1976;260:331–333. doi: 10.1038/260331a0. [DOI] [PubMed] [Google Scholar]
- 3.Drago F., Canonico P.L., Scapagnini U. Behavioral effects of phosphatidylserine in aged rats. Neurobiol. Aging. 1981;2:209–213. doi: 10.1016/0197-4580(81)90023-3. [DOI] [PubMed] [Google Scholar]
- 4.Tsakiris S., Deliconstantinos G. Influence of phophatidylserine on (Na+ + K+)-stimulated ATPase and acetylcholinesterase activities of dog synaptosomal plasma membranes. Biochem. J. 1984;220:301–307. doi: 10.1042/bj2200301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zanotti A., Valzelli L., Toffano G. Chronic phosphatidylserine treatment improves spatial memory and passive avoidance in aged rats. Psychopharmacology. 1989;99:316–321. doi: 10.1007/BF00445550. [DOI] [PubMed] [Google Scholar]
- 6.Delwaide P.J., Gyselynck-Mambourg A.M., Hurlet A., Ylieff M. Double-blind randomized controlled study of phosphatidylserine in senile demented patients. Acta. Neurol. Scand. 1986;73:136–140. doi: 10.1111/j.1600-0404.1986.tb03254.x. [DOI] [PubMed] [Google Scholar]
- 7.Cenacchi T., Bertoldin T., Farina C., Fiori M.G., Crepaldi G. Cognitive decline in the elderly: a double-blind, placebocontrolled multicenter study on efficacy of phosphatidylserine administration. Aging Clin. Exp. Res. 1993;5:123–133. doi: 10.1007/BF03324139. [DOI] [PubMed] [Google Scholar]
- 8.Amaducci L., the SMID group Phosphatidylserine in the treatment of Alzheimer’s disease: results of a multicenter study. Psychopharmacol. Bull. 1988;24:130–134. [PubMed] [Google Scholar]
- 9.Engel R.R., Satzger W., Günther W., Kathmann N., Bove D., Gerke S., Münch U., Hippius H. Double-blind cross-over study of phosphatidyl-serine vs. placebo in patients with early dementia of Alzheimer type. Eur. Neuropsychopharmacol. 1992;2:149–155. doi: 10.1016/0924-977x(92)90025-4. [DOI] [PubMed] [Google Scholar]
- 10.Crook T.H., Tinklenberg J., Yesavage J., Petrie W., Nunzi M.G., Massari D.C. Effects of phosphatidylserine in age-associated memory impairment. Neurology. 1991;41:644–649. doi: 10.1212/wnl.41.5.644. [DOI] [PubMed] [Google Scholar]
- 11.Prusiner S.B. Molecular biology of prion disease. Science. 1991;252:1515–1522. doi: 10.1126/science.1675487. [DOI] [PubMed] [Google Scholar]
- 12.Kudo S. Biosurfactants as food additives. Proceedings of the World Conference on Biotechnology for the Fats and Oils Industry. American Oil Chemist’s Society; Hamburg, Germany: 1987. pp. 195–201. [Google Scholar]
- 13.Sakai M., Yamatoya H., Kudo S. Pharmacological effects of Phosphatidylserine enzymatically synthesized from soybean lecithin on brain functions in rodents. J. Nutr. Sci. Vitaminol. (Tokyo) 1996;42:47–54. doi: 10.3177/jnsv.42.47. [DOI] [PubMed] [Google Scholar]
- 14.Furushiro M., Suzuki S., Shishido Y., Sakai M., Yamatoya H., Kudo S., Hashimoto S., Yokokura T. Effect of oral administration of soybean lecithin transphosphatidylated phosphatidylserine on impaired learning of passive avoidance in mice. Jpn. J. Pharmacol. 1997;75:447–450. doi: 10.1254/jjp.75.447. [DOI] [PubMed] [Google Scholar]
- 15.Suzuki S., Kataoka A., Furushiro M. Effect of intracerebroventricular administration of soybean lecithin transphosphatidylated phosphatidylserine on scopolamine-induced amnesic mice. Jpn. J. Pharmacol. 2000;84:86–88. doi: 10.1254/jjp.84.86. [DOI] [PubMed] [Google Scholar]
- 16.Suzuki S., Yamatoya H., Sakai M., Kataoka A., Furushiro M., Kudo S. Oral administration of soybean lecithin transphosphatidylated phosphatidylserine improves memory impairment in aged rats. J. Nutr. 2001;131:2951–2956. doi: 10.1093/jn/131.11.2951. [DOI] [PubMed] [Google Scholar]
- 17.Gindin J., Novikov M., Dedar D., Walter-Ginzburg A., Naor S., Levi S. The effect of plant phosphatidylserine of age—associated memory impairment and mood in the functioning elderly. The Geriatric Institute for Education and Research, and Department Geriatrics, Kapran Hospital. Rehovot; Israel: 1995. [Google Scholar]
- 18.Crook T.H. In: Treatment of age-related cognitive decline: effects of phosphatidylserine, in Anti-Aging Medical Therapeutics. Vol. II. Katz R.M., Goldman R., editors. Health Quest Publications; Marina del Rey, Carfornia: 1998. pp. 20–28. [Google Scholar]
- 19.Schreiber S., Kampf-Sherf O., Gorfine M., Kelly D., Oppenheim Y., Lerer B. An open trial of plant-source derived phosphatidylserine for treatment of age-related cognitive decline. Isr. J. Psychiatr. Relat. Sci. 2000;37:302–307. [PubMed] [Google Scholar]
- 20.Jorissen B.L., Brouns F., Van Boxtel M.P., Ponds R.W., Verhey F.R., Jolles J., Riedel W.J. The influence of soy-derived phosphatidylserine on cognition in age-associated memory impairment. Nutr. Neurosci. 2001;4:121–134. doi: 10.1080/1028415x.2001.11747356. [DOI] [PubMed] [Google Scholar]
- 21.Asano T., Kato-Kataoka A., Sakai M., Tsuji A., Ebina R., Nonaka C., Takamizawa K. The effect of soybean derived phosphatidylserine on the cognitive function of the elderly. Jpn. J. Nutr. Ass. 2005;24:165–170. [Google Scholar]
- 22.Wilson B., Cockburn J., Baddeley A., Hiorns R. The development and validation of a test battery for detecting and monitoring everyday memory problems. J. Clin. Exp. Neuropsychol. 1989;11:855–870. doi: 10.1080/01688638908400940. [DOI] [PubMed] [Google Scholar]
- 23.Folstein M.F., Folstein S.E., McHugh P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 24.Yesavage J.A., Brink T.L., Rose T.L., Lum O., Huang V., Adey M., Leirer V.O. Development and validation of a geriatric depression screening scale: a preliminary report. J. Psychiatr. Res. 1983;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 25.Sakai M., Ebina R., Yamatoya H., Kudo S., inventor; Kabushiki Kaisha Yakult Honsha, assignee. Method for producing phospholipid United States patent 76959442010April13
- 26.Kazui H., Watamori T.S., Honda R., Tokimasa A., Hirono N., Mori E. The validation of the Japanese version of the Rivermead Behavioural Memory Test—A test for everyday memory—. Adv. Neurol. Sci. 2002;46:307–318. [Google Scholar]
- 27.Imai Y., Hasegawa K. The reviced Hasegawa’s dementia scale (HDS-R): evaluation of its usefulness as a screening test for dementia. J. Hong Kong Coll. Psychiatr. 1994;4:20–24. [Google Scholar]
- 28.Kazui H., Watamori T.S., Honda R., Mori E. The validation of the Japanese version of the Everyday Memory Checklist. Brain and Nerve. 2003;55:317–325. [PubMed] [Google Scholar]
- 29.McDaniel M.A., Maier S.F., Einstein G.O. “Brain-specific” nutrient: a memory cure? Nutrition. 2003;19:957–975. doi: 10.1016/s0899-9007(03)00024-8. [DOI] [PubMed] [Google Scholar]
- 30.Tombaugh T.N., McIntyre N.J. The mini-mental state examination: a comprehensive review. J. Am. Geriatr. Soc. 1992;40:922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- 31.Arnaiz E., Almkvist O. Neuropsychological features of mild cognitive impairment and preclinical Alzheimer’s disease. Acta. Neurol. Scand. Suppl. 2003;179:34–41. [PubMed] [Google Scholar]
- 32.Toffano G., Battistella A., Orlando P. Pharmacokinetics of radiorabelled brain phosphatidylserine. Clin. Trial. J. 1987;24:18–24. [Google Scholar]
- 33.Kawai Y., Kiyokawa H., Kimura Y., Kato Y., Tsuchiya K., Terao J. Hypochlorous acid-derived modification of phospholipids: characterization of aminophospholipids as regulatory molecules for lipid peroxidation. Biochemistry. 2006;45:14201–14211. doi: 10.1021/bi0610909. [DOI] [PubMed] [Google Scholar]
- 34.Hashioka S., Han Y.H., Fujii S., Kato T., Monji A., Utsumi H., Sawada M., Nakanishi H., Kanba S. Phosphatidylserine and phosphatidylcholine-containing liposomes inhibit amyloid beta and interferon-gamma-induced microglial activation. Free Radic. Biol. Med. 2007;42:945–954. doi: 10.1016/j.freeradbiomed.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 35.Satoh A., Tsuji S., Okada Y., Murakami N., Urami M., Nakagawa K., Ishikura M., Katagiri M., Koga Y., Shirasawa T. Preliminary clinical evaluation of toxicity and efficacy of a new astaxanthin-rich Haematococcus pluvialis extract. J. Clin. Biochem. Nutr. 2009;44:280–284. doi: 10.3164/jcbn.08-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nunzi M.G., Milan F., Guidolin D., Toffano G. Dendritic spine loss in hippocampus of aged rats. Effect of brain phosphatidylserine administration. Neurobiol. Aging. 1987;8:501–510. doi: 10.1016/0197-4580(87)90124-2. [DOI] [PubMed] [Google Scholar]
- 37.Little A., Levy R., Chuaqui-Kidd P., Hand D. A double-blind, placebo controlled trial of high-dose lecithin in Alzheimer’s disease. J. Neurol. Neurosurg. Psychiatry. 1985;48:736–742. doi: 10.1136/jnnp.48.8.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reger M.A., Henderson S.T., Hale C., Cholerton B., Baker L.D., Watson G.S., Hyde K., Chapman D., Craft S. Effects of beta-hydroxybutyrate on cognition in memory-impaired adults. Neurobiol. Aging. 2004;25:311–314. doi: 10.1016/S0197-4580(03)00087-3. [DOI] [PubMed] [Google Scholar]
- 39.Sano M., Ernesto C., Thomas R.G., Klauber M.R., Schafer K., Grundman M., Woodbury P., Growdon J., Cotman C.W., Pfeiffer E., Schneider L.S., Thal L.J. A controlled trial of selegiline, alpha-tocopherol, or both as treatment for Alzheimer’s disease. The Alzheimer’s Disease Cooperative Study. N. Engl. J. Med. 1997;336:1216–1222. doi: 10.1056/NEJM199704243361704. [DOI] [PubMed] [Google Scholar]