Abstract
It is now widely accepted that resident central nervous system (CNS) cells such as microglia and astrocytes initiate and/or augment inflammation following trauma or infection. However, the mechanisms by which glial cells perceive microbial challenges are only now becoming apparent. We have recently demonstrated that microglia and astrocytes constitutively express nucleotide-binding oligomerization domain-2 (NOD2), a member of the novel nucleotide-binding domain leucine-rich repeat region-containing family of proteins (NLR) that functions as an intracellular receptor for a minimal motif present in all bacterial peptidoglycans. Furthermore, we have shown that this NLR is essential for glial responses to Gram-negative pathogens and in vivo CNS inflammation elicited by these organisms. In the present study, we have established that intact Streptococcus pneumoniae, the major causative agent for Gram-positive bacterial meningitis in adults, is a potent stimulus for the activation of the pivotal inflammatory transcription factor NF-kB and production of inflammatory cytokines in primary murine microglia and astrocytes. We demonstrate that NOD2 is essential for the maximal responses of these cells to intact S. pneumoniae but not cellular lysates. Finally, we have shown that this cytosolic pattern recognition receptor is required for the elevated inflammatory mediator levels, astrogliosis, and demyelination, following in vivo administration of this Gram-positive CNS pathogen. As such, we suggest that NOD2 plays a critical role in the establishment of the lethal inflammation associated with streptococcal meningitis.
Keywords: microglia, astrocytes, Gram–positive bacteria, meningitis, NLR, cytokines
Introduction
The Gram-positive bacterium, Streptococcus pneumoniae, is the leading cause of bacterial meningitis in adults (as reviewed in Meli et al, 2002; Scheld et al 2002). Such central nervous system (CNS) infections are associated with an intense inflammatory host response (Liu et al, 2008; Meli et al, 2002; Neher and Brown, 2007; Scheld et al 2002) and a high degree of mortality (Meli et al, 2002; Scheld et al 2002). Furthermore, patients that survive S. pneumoniae-associated meningitis often exhibit serious neurological sequelae (Meli et al, 2002; Scheld et al 2002). As such, delineating the pathogenesis of these infections is essential if we are to improve disease outcome.
While the brain has traditionally been viewed as a “victim organ” of infiltrating leukocytes, it has become increasingly apparent that resident glial cells such as microglia and astrocytes play an important role in the initiation and/or progression of immune responses following pathogen invasion (as reviewed in Chauhan and Marriott, 2007). We have previously demonstrated that astrocytes and microglia constitutively express nucleotide-binding oligomerization domain-2 (NOD2) (Sterka and Marriott 2006; Sterka et al. 2006), a member of the novel nucleotide-binding domain leucine-rich repeat region-containing family of proteins (NLR) that functions as an intracellular receptor for a minimal motif present in all bacterial peptidoglycans (Girardin et al, 2003a; Girardin et al, 2003b; Inohara et al, 2003). Importantly, we have recently confirmed that NOD2 is functional in these cells by demonstrating that this NLR mediates the ability of muramyl dipeptide to augment Toll-like receptor (TLR)-induced inflammatory cytokine production by primary astrocytes and microglia (Chauhan et al, 2009). Furthermore, we have shown that this receptor is an important component in inflammatory CNS responses to the Gram-negative bacterial pathogens, Neisseria meningitidis and B. burgdorferi (Chauhan et al, 2009).
Gram-positive organisms have been demonstrated to elicit inflammatory immune responses by both astrocytes and microglia (Esen et al, 2004; Kielian, 2004). In addition, streptococcal cell walls and cellular components that serve as TLR ligands can induce inflammatory mediator production by glial cells (Brandenburg et al, 2008; Freyer et al, 1996; Kim and Tauber, 1996; Prinz et al, 1999). However, astrocyte and microglial responses to intact S. pneumoniae have not been reported. Furthermore, a role for NOD2 in CNS inflammation following Gram-positive bacterial infection has not been established. In the present study, we demonstrate that S. pneumoniae is a potent inflammatory stimulus for both astrocytes and microglia. Interestingly, we show that NOD2 is essential for the maximal responses of these cells to intact bacteria but not cellular lysates. Finally, we demonstrate that the expression of this cytosolic pattern recognition receptor is an important contributor to damaging CNS inflammation associated with in vivo S. pneumoniae infection.
Materials and Methods
Wild type and NOD2-deficient mice
B6.129S1-Nod2tm1Flv/J mice that are NOD2-deficient (NOD2-/-) and bred for > 10 generations onto a C57BL/6 background, as well as wild type C57BL/6j mice, were purchased from Jackson Laboratory (Bar Harbour, Maine). All studies were performed in accordance with relevant federal guidelines and institutional policies regarding the use of animals for research purposes.
Isolation of primary murine microglia
Mouse neonatal brain microglia were isolated as described previously by our laboratory (Rasley et al. 2002b) and cultured in RPMI 1640 medium with 10% fetal bovine serum (FBS) and 20% conditioned medium from LADMAC cells (ATCC number CRL-2420) as a source of colony stimulating factor-1. Cells isolated in this manner are > 95% authentic microglia as assessed by their characteristic morphology and expression of CD11b and F4/80 as determined by immunofluorescence microscopy.
Isolation of primary murine astrocytes
Mouse neonatal brain astrocytes were isolated as described previously by our laboratory (Rasley et al. 2004a) and cultured in RPMI 1640 containing 10% FBS. Cells isolated in this manner are > 97% authentic astrocytes due to their characteristic morphology, expression of glial fibrillary acidic protein (GFAP) and the absence of CD11b as determined by immunofluorescence microscopy.
Culture of Streptococcus pneumoniae and preparation of antigen lysates
In these studies, we have utilized S. pneumoniae strain CDC CS109 (ATCC 51915), a clinical isolate from a patient with meningitis. This organism was grown on tryptic soy agar with 5% defibrinated sheep blood and cultured overnight in brain heart infusion broth at 37°C with 5% CO2 as previously described (Liu et al, 2008). For in vitro exposure of isolated glia to S. pneumoniae, bacteria were harvested by centrifugation and washed twice in phosphate buffered saline. Confluent cell layers of glia were washed three times with 4 ml of PBS to remove growth media and then exposed to bacteria at multiplicities of infection (MOI) of between 25:1 and 250:1 bacteria to cells in media without antibiotics for 120 min at 37°C. Following this period, cell cultures were washed and incubated in media with 10% FBS supplemented with 25 μg/ml gentamicin to kill remaining extracellular bacteria. At 12-24 hours following this procedure, culture supernatants were collected. In other experiments, glial cells were exposed to cell lysates prepared from an equal number of S. pneumoniae pulsed three times with a cell sonicator and boiled for 3 minutes prior to addition to the culture medium.
Quantification of cytokine and chemokine secretion
Specific capture ELISAs were performed to quantify IL-6, IL-10, TNF-α, and MIP-1α secretion by glial cells as described previously by our laboratory (Chauhan et al, 2009). Cytokine and chemokine levels in brain homogenates were normalized to total brain weight and reported as ng/g of brain tissue.
Western blot analyses for NF-kB activation
Nuclear protein extracts were prepared from microglia and astrocytes and immunoblot analysis performed for the presence of the p65 subunit of NF-kB (RelA) as previously described by our laboratory (Marriott et al, 2000). The primary antibodies used were a purified rabbit polyclonal antibody directed against mouse RelA (Millipore, Temecula, CA). Densitometric analyses of Western blots were performed using ImageJ (obtained from the Web site: http://rsbweb.nih.gov/ij/download.html). Results are presented as mean values +/- SEM of arbitrary densitometric units corrected for background intensity.
Intracerebral administration of bacteria
Viable S. pneumoniae (1×106 bacteria) were administered via intracerebral (i.c.) injection into NOD2-/- or wild-type mice as previously described by our laboratory (Chauhan et al, 2008). Anesthetized animals were secured in a stereotaxic platform and stand, and received an i.c. injection containing pathogens resuspended in Ringer's solution (final volume of 1 μL) or Ringer's solution only, 1 mm lateral and 1 mm posterior to the bregma using a Hamilton positive displacement syringe (7001 series) with a 25-gauge needle and a tubing guard to ensure constant depth of administration (3-3.5 mm). Four animals per group were used and animals displaying signs such as seizures, abnormal gait/ataxia, failure to open eyes, or other physical disabilities were euthanized immediately. At 1, 3, and 5 days post-infection, animals were euthanized and all brain tissue removed. Brain tissue was prepared for microscopy or mechanically disrupted in a glass homogenizer in 3 mL PBS for assessment of bacterial burden by plate counting and analysis of cytokine and chemokine content by specific capture ELISA.
Histochemical and immunofluorescence analyses of murine brain sections
Infected and non-infected mice were euthanized 1, 3, and 5 days post infection and the brains were perfused with Prefer fixative (Anatech, Battel creek, MI) via intra-atrial injection. Samples were embedded in paraffin and sectioned serially (5-7 um). Demyelination was visualized in coronal sections by Luxol fast blue-Cresyl violet staining according to the directions provided by the manufacturer (American MasterTech Scientific Inc., Lodi, CA), and as previously described by our laboratory (Chauhan et al, 2009). Briefly, paraffin embedded sections were heated and rehydrated with decreasing concentrations of ethyl alcohol prior to rinsing in distilled water and Luxol fast blue staining at 60°C for 18 hrs. Grey and white matter was further differentiated using 0.05% lithium carbonate and washing with 70% alcohol. Finally, the slides were placed in Cresyl Echt violet stain for 10 min and differentiated with alcohol. After dehydration, slides were washed in xylene and coverslips were mounted using permanent mounting media and myelination of the corpus callosum visually assessed in a low power (10× objective) microscopy field in animals from each experimental group (n = 4).
Astrogliosis was assessed in deparaffinized coronal sections blocked with goat serum (Zymed laboratories, San Francisco, CA) according to GFAP expression. GFAP was detected using a monoclonal mouse antibody directed against murine GFAP (Molecular Probes, Eugene, Oregon) and an AlexaFluor 488 conjugated chicken anti-mouse secondary antibody (Molecular Probes). Cell nuclei were co-visualized with 4′,6-diamidino-2-phenylindole (DAPI). GFAP expression was assessed in multiple microscopy fields (40× objective) of the same cortical locations in animals from each experimental group using an Olympus IX70 Fluoroview confocal microscopy system. GFAP expression was quantified from the fluorescence micrographs by conversion of the green channel images to grayscale mode and densitometric analysis of these images using ImageJ software. GFAP-associated fluorescence is reported as the average densitometric value in arbitrary units normalized to cell-free background fluorescence measured in each micrograph quadrant of 10 microscopy fields for each animal in the experimental groups (n = 4).
Statistical Analyses
All results are presented as the mean +/- SEM and were tested statistically by Student's t test or one-way analysis of variance (ANOVA) with Tukey's post hoc test as appropriate, using commercially available software (Sigma Stat; Systat Software, San Jose, CA). Results were considered to be statistically significant at a probability of < 0.05.
Results
S. pneumoniae-induced inflammatory cytokine expression by isolated microglia and astrocytes is mediated by NOD2
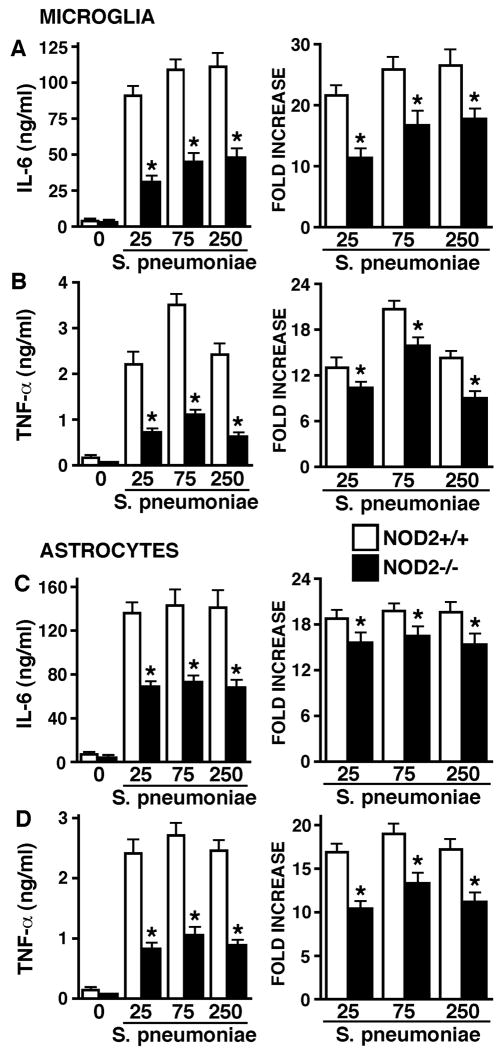
Recognition of S. pneumoniae by glia and subsequent expression of proinflammatory cytokines such as IL-6 and TNF-α is a key component in the development of brain injury during bacterial meningitis (Meli et al, 2002; Neher and Brown, 2007; Scheld et al 2002). To begin to define the role of NOD2 in S. pneumoniae-mediated glial inflammatory responses, primary murine microglia and astrocytes were derived from wild type and NOD2-deficient mice, and untreated or infected with viable S. pneumoniae (MOI of 25:1, 75:1 or 250:1 bacteria to each glial cell). As shown in Figures 1A and 1B, microglia derived from wild type animals (NOD2+/+) exposed to S. pneumoniae produced large amounts of IL-6 and TNF-α at 24 hours following bacterial challenge. Importantly, microglia derived from NOD2 deficient animals (NOD2-/-) produced significantly less of these cytokines following S. pneumoniae challenge than wild type cells both in terms of absolute cytokine levels in the culture supernatant and as fold increases in cytokine production (Figures 1A and 1B).
FIGURE 1.
Inflammatory cytokine responses of glia to intact S. pneumoniae are significantly lower in the absence of NOD2 expression. Microglia (Panels A and B) or astrocytes (Panels C and D) (2 × 106 cells per well) from wild type (NOD2+/+) and NOD2 knockout (NOD2-/-) animals were untreated or exposed to viable S. pneumoniae (MOI, of 25:1, 75:1, 250:1 bacteria to each glial cell). At 24 hrs following bacterial challenge culture supernatants were isolated and assayed for the presence of IL-6 (Panels A and C) or TNF-α (Panels B and D) by specific capture ELISA. Data are presented as the culture supernatant cytokine concentrations (Left panels) and as fold increases over levels in unstimulated cells (Right panels) and are the means of triplicate determinations of samples from three separate experiments +/- SEM. Asterisks indicate statistically significant differences in cytokine production between cells derived from wild type and NOD2 deficient animals (p < 0.05).
Consistent with our previous demonstration that astrocytes respond to Gram-negative bacterial pathogens including N. meningitidis (Chauhan et al, 2008; Chauhan et al, 2009. Rasley et al, 2006), this major glial cell type also demonstrated robust inflammatory cytokine production following exposure to S. pneumoniae (Figures 1C and 1D). Interestingly, astrocytes derived from NOD2-/- mice produced significantly lower concentrations and fold increases over basal levels of both IL-6 and TNF-α at 24 hours following bacterial challenge than NOD2+/+ derived cells (Figures 1C and 1D, respectively).
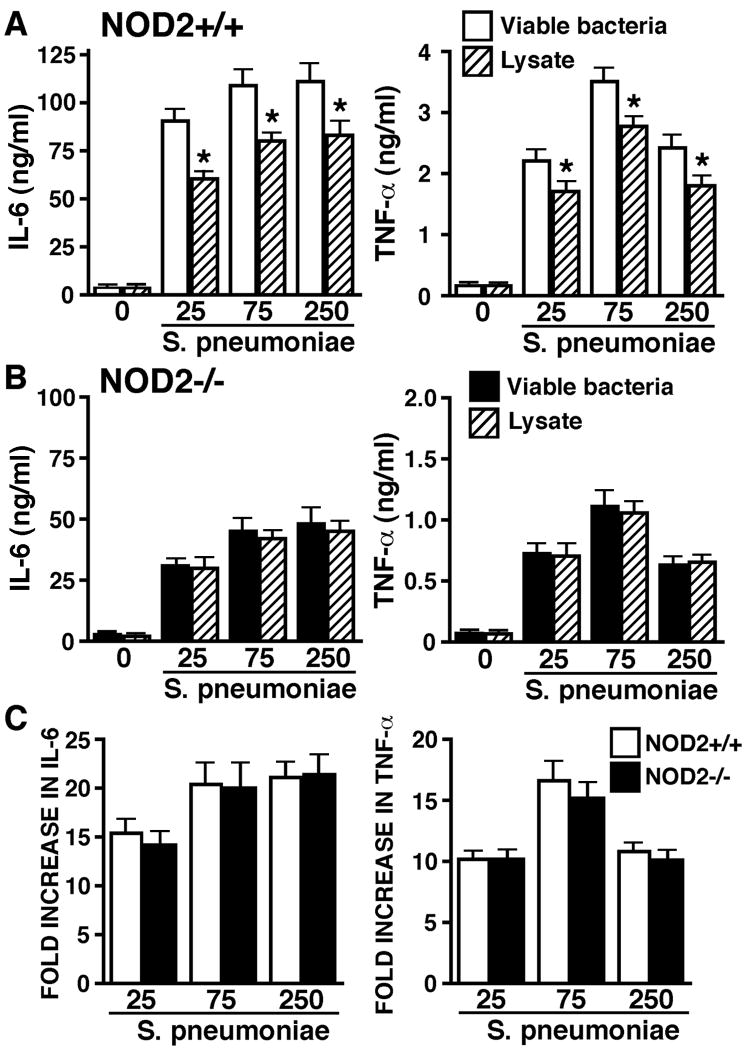
NOD2 is not required for maximal glial responses to S. pneumoniae lysates
To further explore the role of NOD2 in the inflammatory immune responses of resident CNS cells, we investigated the ability of S. pneumoniae lysates to induce IL-6 and TNF-α production by isolated cultures of primary glial cells. As shown in Figure 2A, while S. pneumoniae lysates elicit significant IL-6 and TNF-α production by microglia derived from NOD2+/+ mice, such production is significantly lower than that induced by an equal number of intact viable bacteria. Interestingly, this difference was not apparent in microglia derived from NOD2-/- animals where lysates and intact bacteria elicited almost identical levels of IL-6 and TNF-α production (Figure 2B). Furthermore, inflammatory cytokine production by NOD2-/- derived microglia following exposure to S. pneumoniae lysates was not significantly different from that produced by identically treated NOD2+/+ derived cells (Figure 2C).
FIGURE 2.
Microglial cytokine responses to S. pneumoniae lysates are significantly smaller than those elicited by intact bacteria and are not dependent on the expression of NOD2. Microglia (2 × 106 cells per well) from wild type (NOD2+/+) (Panels A and C) or NOD2 knockout (NOD2-/-) (Panels B and C) animals were untreated or exposed to either viable S. pneumoniae (MOI, of 25:1, 75:1, 250:1 bacteria to each glial cell) or lysates derived from an equal number of bacteria. At 24 hrs following bacterial challenge culture supernatants were isolated and assayed for the presence of IL-6 and TNF-α by specific capture ELISA. Data are presented as the culture supernatant cytokine concentrations (Panels A and B) and as fold increases over levels in unstimulated cells (Panel C) and are the means of triplicate determinations of samples from three separate experiments +/- SEM. Asterisks indicate statistically significant differences in cytokine production between cells treated with intact bacteria or bacterial lysates (p < 0.05).
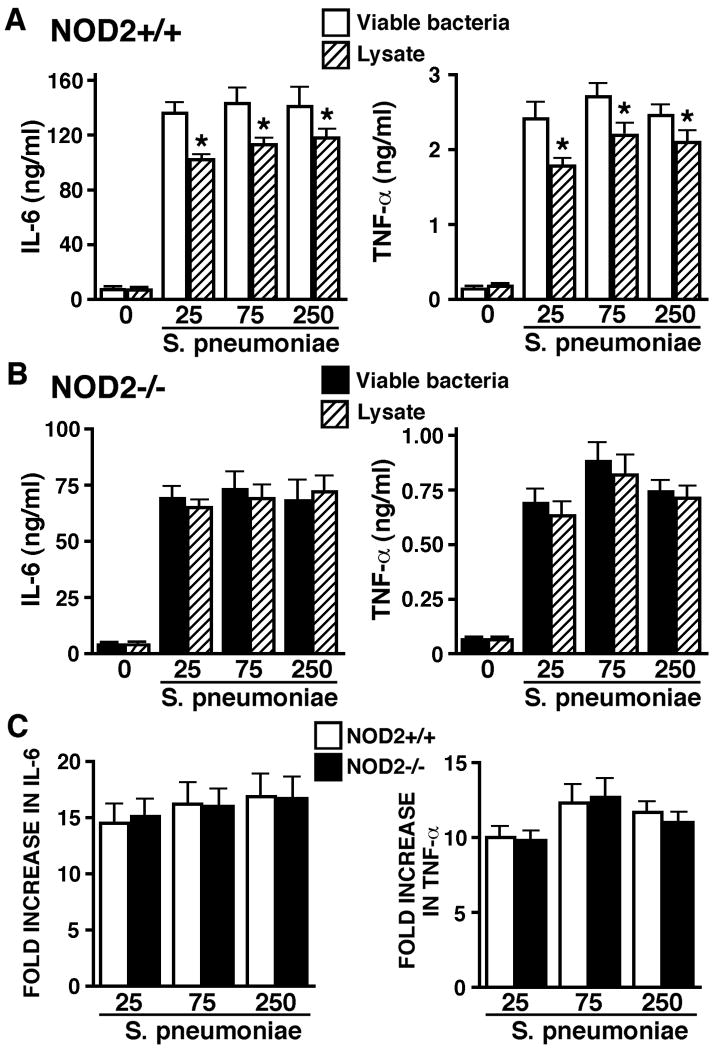
Similarly, S. pneumoniae lysates elicited significantly less inflammatory cytokine production by murine astrocytes than an equal number of intact bacteria (Figure 3A). Again, this disparity was absent in parallel experiments utilizing astrocytes isolated from NOD2-/- mice (Figure 3B). Furthermore, increases in IL-6 and TNF-α production by NOD2-/- cells following exposure to S. pneumoniae lysates were not significantly different from those produced by similarly treated NOD2+/+ derived cells (Figure 3C). Taken together, these data indicate that viable bacteria are a more potent stimulus for inflammatory cytokine production by wild type mice-derived glial cells than mixed bacterial components and this disparity is mediated by NOD2.
FIGURE 3.
Astrocyte cytokine responses to S. pneumoniae lysates are significantly smaller than those elicited by intact bacteria and are not dependent on the expression of NOD2. Astrocytes (2 × 106 cells per well) from wild type (NOD2+/+) (Panels A and C) or NOD2 knockout (NOD2-/-) (Panels B and C) animals were untreated or exposed to either viable S. pneumoniae (MOI, of 25:1, 75:1, 250:1 bacteria to each glial cell) or lysates derived from an equal number of bacteria. At 24 hrs following bacterial challenge culture supernatants were isolated and assayed for the presence of IL-6 and TNF-α by specific capture ELISA. Data are presented as the culture supernatant cytokine concentrations (Panels A and B) and as fold increases over levels in unstimulated cells (Panel C) and are the means of triplicate determinations of samples from three separate experiments +/- SEM. Asterisks indicate statistically significant differences in cytokine production between cells treated with intact bacteria or bacterial lysates (p < 0.05).
NOD2 expression is required for maximal S. pneumoniae-mediated increases in NF-kB activation in microglia and astrocytes
To further determine the role played by NOD2 in S. pneumoniae-mediated glial immune responses, we assessed NF-kB p65 subunit (RelA) nuclear translocation in microglia and astrocytes derived from NOD2+/+ and NOD2-/- mice following exposure to this bacterium. As shown in Figure 4, exposure of NOD2+/+ mice-derived microglia to S. pneumoniae elicited increases in NF-kB activation with 15 to 16 fold increases in nuclear RelA levels (Figure 4). Similarly, this bacterium also induces RelA translocation in astrocytes with up to 47-fold increases in the nuclear levels of this transcription factor (Figure 4). Importantly, such S. pneumoniae-induced NF-kB activation was markedly attenuated in microglia and astrocytes isolated from NOD2-/- mice (Figure 4) with maximal increases of only 15-27% of that seen in NOD2+/+ derived cells. As such, these data are in agreement with published studies in HEK293 cells (Opitz et al, 2004) and indicate that NOD2 is required for maximal S. pneumoniae-mediated activation of a pivotal pro-inflammatory transcription factor in resident CNS cells.
FIGURE 4.
Activation of NF-kB following exposure to intact S. pneumoniae is significantly lower in glia deficient in the expression of NOD2. Microglia (Upper immunoblot) or astrocytes (Lower immunoblot) (2 × 106 cells per well) from wild type (NOD2+/+) and NOD2 knockout (NOD2-/-) animals were untreated (0) or exposed to viable S. pneumoniae (MOI, of 25:1, 75:1, 250:1 bacteria to each glial cell). At 2 hrs following bacterial challenge nuclear protein isolates were prepared and assayed for the presence of NF-kB p65 (RelA) by immunoblot analysis. Fold increases in nuclear RelA levels following bacterial challenge were determined by densitometric analysis and are indicated below the bands. The immunoblots shown are representative of three separate experiments.
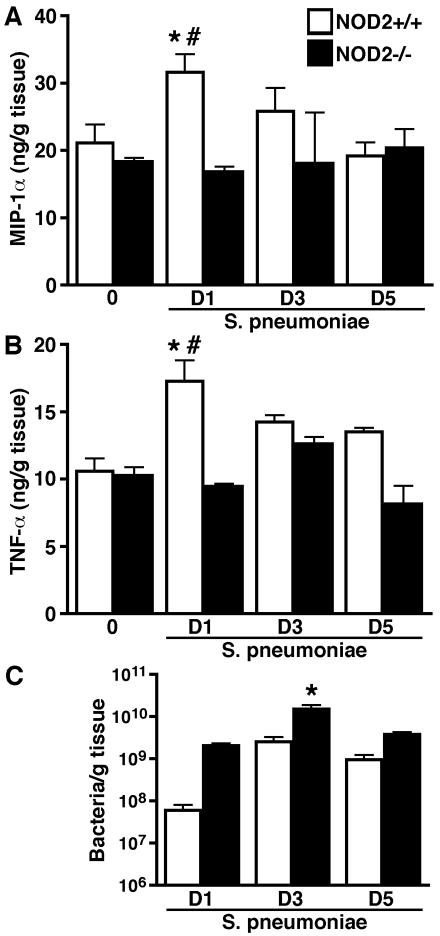
NOD2 is a major contributor to acute CNS inflammation following in vivo S. pneumoniae administration
To begin to establish the in vivo relevancy of our in vitro findings, we have extended our studies to a murine model of pneumococcal bacterial meningitis. Known numbers of S. pneumoniae (1×106 organisms) were directly administered via i.c. injection into NOD2+/+ and NOD2-/- mice. At 1, 3, and 5 days following administration, inflammatory cytokine levels were assessed in S. pneumoniae-infected brain tissue in the absence or presence of NOD2 expression. As shown in Figure 5A, levels of the chemokine MIP-1α were significantly increased in the brains of NOD2+/+ mice 24 hours following infection with this Gram-positive organism. However, such elevations were not observed in NOD2-/- animals (Figure 5A). Similarly, we have found that increases in CNS levels of the inflammatory cytokine TNF-α observed at 24 hours following S. pneumoniae administration were absent in NOD2-/- mice (Figure 5B). Furthermore, we have found that S. pneumoniae-induced decreases in the level of the immunosuppressive cytokine IL-10 at 24 hours following infection were markedly reduced in the absence of NOD2 expression (25.8 +/- 2.0% decrease in NOD2+/+ mice versus 3.6 +/- 6.1% decrease in NOD2-/- animals; n = 4, p < 0.05).
FIGURE 5.
In the absence of NOD2 expression, intracerebral S. pneumoniae administration fails to elicit rapid elevations in inflammatory mediator levels and is associated with higher bacterial burdens within the CNS. Vehicle (0) or S. pneumoniae (1 × 106 bacteria) was administered via i.c. injection into C57BL/6 wild type (NOD2+/+) and NOD2 deficient (NOD2-/-) mice. At 1 (D1), 3 (D3), and 5 (D5), days post-infection tissue homogenates were isolated for measurement of TNF-α (Panel A) and MIP-1α (Panel B) protein expression by specific capture ELISA, and assessment of bacterial burden (Panel C). Data are presented as the means of triplicate determinations of samples from four animals in each group +/- SEM. Asterisk indicates significant difference between levels in infected NOD2+/+ and NOD2-/- mice, and pound symbol indicates significant difference from uninfected animals (p < 0.05).
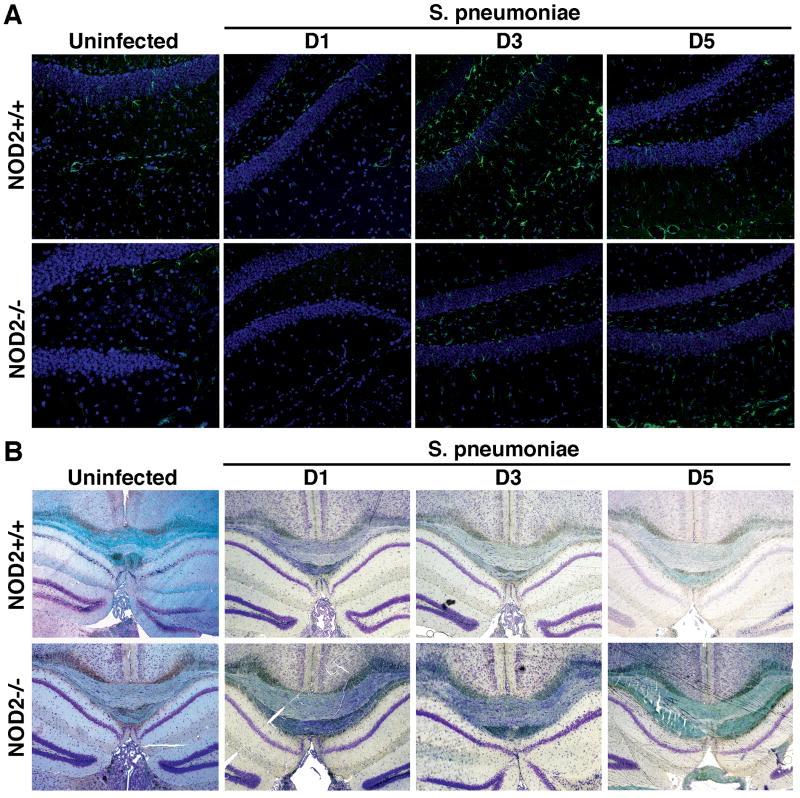
In addition, brain tissue was prepared for immunofluorescence microscopy to determine the relative proportion of cells positive for the astrocyte marker, GFAP, and its relative level of expression as a measure of reactive astrogliosis in infected mice. As shown in Figure 6A, S. pneumoniae elicits a pronounced increase in the number and fluorescence intensity of GFAP positive cells that peaked at 72 hours post-infection in wild type animals. Importantly, significantly lower GFAP-associated fluorescence was seen in infected NOD2-/- animals at 72 hours following S. pneumoniae administration compared to that seen in infected NOD2+/+ mice (1.63 +/- 0.44 versus 5.45 +/- 1.54 arbitrary intensity units, respectively; n = 4, p < 0.05) (Figure 6A).
FIGURE 6.
S. pneumoniae-induced astrogliosis and demyelination is attenuated in the absence of NOD2 expression. Vehicle or S. pneumoniae (1 × 106 bacteria) was administered via intracerebral injection into C57BL/6 wild type (NOD2+/+) and NOD2 deficient (NOD2-/-) mice. At day 1 (D1), 3 (D3), and 5 (D5), post-infection brain tissue was perfused in situ, isolated, and prepared for analysis by immunofluorescence and lightfield microscopy. Panel A shows astrocyte-associated GFAP (green) and cell nuclei-associated DAPI (blue) immunofluorescence in representative coronal cortical fields (40× objective) from one of the four animals in each group while Panel C shows representative Luxol blue staining of the corpus callosum in coronal fields (10× objective).
Finally, demyelination was assessed in parallel studies by Luxol blue staining and lightfield microscopy. As shown in Figure 6B, S. pneumoniae infection of NOD2+/+ mice elicits demyelination within the CNS as evidenced by the progressively reduced staining of the corpus callosum (n = 4). Importantly, S. pneumoniae-associated demyelination was less apparent in NOD2-/- animals (Figure 6B). Taken together, these data indicate that NOD2 is required for the inflammatory mediator production, gliosis, and demyelination, resulting from S. pneumoniae infection, and provides a compelling case for a role of this cytosolic receptor in the lethal CNS inflammation associated with a major Gram-positive bacterial pathogen.
Discussion
While it is likely that infiltrating immune cells contribute to inflammatory responses within the CNS, a growing body of evidence suggests that resident glial cells play an important role in the initiation and progression of inflammation following infection or trauma. To accomplish this role, resident cells such as microglia and astrocytes express multiple microbial pattern recognition receptors including TLRs to perceive bacterial pathogens and to initiate potentially damaging CNS inflammation (Bsibsi et al. 2002; Carpentier et al. 2008; Esen and Kielian 2005; Kielian et al. 2005; Olson and Miller 2004; Rasley et al. 2002a). Accordingly, our laboratory and others have demonstrated the ability of microglia and astrocytes to produce key inflammatory cytokines including TNF-α, and IL-6 in response to TLR ligands and Gram-negative bacterial pathogens of the CNS (Kielian 2004; Kielian et al. 2002; Rasley et al. 2002a; Rasley et al. 2004b; Bowman et al. 2003; Bsibsi et al. 2002; Carpentier et al. 2005; Dong and Benveniste 2001; Esen et al. 2004; Lieberman et al. 1989; Takeshita et al. 2001).
In the present study, we demonstrate that mixed antigen lysates prepared from the Gram-positive organism, S. pneumoniae, are potent stimuli for both microglia and astrocytes. We show that bacterial lysate preparations elicit the production of significant quantities of TNF-α and IL-6 by these resident CNS cells. These findings are in agreement with the results of others demonstrating that S. pneumoniae cell wall preparations elicit MAP kinase activation by glial cells (Schumann et al, 1998) and inflammatory mediator and/or antimicrobial peptide production by both microglia and astrocytes (Freyer et al, 1996; Kim and Tauber, 1996; Prinz et al, 1999; Brandenburg et al, 2008). Similarly, heat killed S. pneumoniae has been demonstrated to induce NO production by astrocytes (Bernatowicz et al, 1995) while purified pneumolysin elicits release of this inflammatory mediator by primary mouse microglia (Ebert et al, 2005). Importantly, in the present study we report that acute in vitro exposure to viable intact S. pneumoniae results in significantly greater inflammatory immune production by both microglia and astrocytes than that elicited by a lysate preparation derived from an equal number of bacteria.
NLR proteins such as NOD2 have been identified as cytosolic pattern recognition receptors that play a role in the initiation of inflammatory host immune responses to bacterial challenge (Dziarski and Gupta 2005; Strober et al. 2006). NOD2 appears to function as an intracellular receptor for a minimal motif common to all bacterial peptidoglycans (Fournier and Philpott 2005; Girardin et al. 2003b; Takada and Uehara 2006). Previously, we have characterized the expression of NOD2 and its downstream effector molecule Rip2 kinase in primary cultures of murine glial cells (Sterka and Marriott 2006; Sterka et al. 2006). More recently, we have shown that that exposure of microglia and astrocytes to bacterial lysates increases the association of NOD2 with Rip2 kinase, and demonstrated that this cytosolic receptor underlies the ability of MDP to augment TLR-induced inflammatory responses of microglia and astrocytes (Chauhan et al, 2009). Furthermore, we demonstrated that this cytosolic receptor is required for maximal inflammatory immune responses of primary glia cells to the Gram-negative bacteria, N. meningitidis and B. burgdorferi, and is a significant contributor to the progression of inflammatory CNS damage caused by these organisms following in vivo administration (Chauhan et al, 2009).
In the present study, we have assessed the relative importance of NOD2 in the immune responses of isolated cultures of primary glia cells to Gram-positive pneumococci. We show that the activation of the pivotal inflammatory transcriptional activator NF-kB and the production of key inflammatory cytokines in both astrocytes and microglia following challenge with intact S. pneumoniae are significantly reduced in the absence of NOD2 expression. Importantly, we have established the in vivo relevancy of our in vitro studies by studying the CNS inflammation associated with direct i.c. bacterial administration in wild type animals and mice genetically deficient in the expression of NOD2. We have shown that infection of adult wild type mice with a sub-lethal dose of S. pneumoniae elicits a significant increase in inflammatory chemokine and cytokine production at 24 hours following infection with a concomitant decrease in the level of an immunosuppressive cytokine. The bacterial burden peaks within the CNS at 3 days post infection and this is associated with a pronounced astrogliosis and the onset of demyelination. This demyelination becomes progressively more apparent at 5 days following infection even as the bacterial burden diminishes. Importantly, we have found that the rapid increase in inflammatory mediators associated with S. pneumoniae administration is absent in NOD2-/- animals and we have demonstrated that the astrogliosis and demyelination following infection are markedly reduced in these animals, despite the presence of a significantly higher bacterial burden. Together, these studies suggest that NOD2 is an important component in the initiation and/or progression of damaging CNS inflammation associated with pneumococcal meningitis.
The present study indicates that the immune responses of glia to Gram-positive bacterial components are significantly smaller than those elicited by intact S. pneumoniae. Interestingly, we have found that inflammatory cytokine production by either microglia or astrocytes following exposure to pneumococcal lysates is unaffected by the absence of NOD2 expression. This finding is in contrast to the results obtained using intact S. pneumoniae and our previous studies in which we demonstrated that the glial responses to Gram-negative bacterial lysates were significantly attenuated in cells derived from NOD2 deficient animals (Chauhan et al, 2009).
A precedent for these somewhat surprising results can be found in other studies employing Gram-positive CNS pathogens. TLR2 has been implicated in the initiation of CNS inflammation following Gram-positive bacterial infections based upon the observed attenuation of glial responses to Staphylococcus aureus in the absence of TLR2, CD14, and/or MyD88 expression (Esen and Kielian, 2005; Esen and Kielian, 2006; Esen et al, 2004) and the ability of specific TLR2 ligands to mimic meningitis disease pathology (Hoffman et al, 2007). However, it is apparent that glial cells employ additional mechanisms to perceive such pathogens. Esen and coworkers (2004) have previously demonstrated that TLR2 expression is required for a portion, but not all, of the inflammatory response of murine astrocytes to S. aureus challenge. Importantly, these investigators have also shown that TLR2 and its co-receptor, CD14, are required for microglial responses to bacterial components but not intact S. aureus (Esen and Kielian, 2005; Kielian et al, 2005).
Based upon these observations and the present study, we suggest that maximal glial responses to intact Gram-positive bacterial pathogens require the involvement of cytosolic NOD2. While the notion that S. pneumoniae is internalized by resident glial cells is currently controversial, such a hypothesis is supported by the documented ability of this organism to invade human epithelial and endothelial cell lines (Opitz et al., 2004; Bergmann et al, 2009; Rajam et al, 2008; Pracht et al, 2005), and primary human brain microvascular and umbilical vein-derived endothelial cells (Pracht et al, 2005). As such, we propose a scenario in which S. pneumoniae is perceived by microglia and astrocytes via TLRs and NOD2 in a cooperative manner in which extracellular components are recognized by cell surface pattern recognition receptors such as TLR2, while internalized bacteria elicit maximal glial activation and potentially lethal inflammation in a NOD2-mediated manner.
Acknowledgments
This work is supported by grants NS050325 and NS057434 to IM from the National Institutes of Health.
References
- Bergmann S, Lang A, Rohde M, Agarwal V, Rennemeier C, Grashoff C, Preissner KT, Hammerschmidt S. Integrin-linked kinase is required for vitronectin-mediated internalization of Streptococcus pneumoniae by host cells. J Cell Sci. 2009;122:256–267. doi: 10.1242/jcs.035600. [DOI] [PubMed] [Google Scholar]
- Bernatowicz A, Ködel U, Frei K, Fontana A, Pfister HW. Production of nitrite by primary rat astrocytes in response to pneumococci. J Neuroimmunol. 1995;60:53–61. doi: 10.1016/0165-5728(95)00053-5. [DOI] [PubMed] [Google Scholar]
- Bowman CC, Rasley A, Tranguch SL, Marriott I. Cultured astrocytes express toll-like receptors for bacterial products. Glia. 2003;43:281–291. doi: 10.1002/glia.10256. [DOI] [PubMed] [Google Scholar]
- Brandenburg LO, Varoga D, Nicolaeva N, Leib SL, Wilms H, Podschun R, Wruck CJ, Schröder JM, Pufe T, Lucius R. Role of glial cells in the functional expression of LL-37/rat cathelin-related antimicrobial peptide in meningitis. J Neuropathol Exp Neurol. 2008;67:1041–1054. doi: 10.1097/NEN.0b013e31818b4801. [DOI] [PubMed] [Google Scholar]
- Bsibsi M, Ravid R, Gveric D, van Noort JM. Broad expression of Toll-like receptors in the human central nervous system. J Neuropathol Exp Neurol. 2002;61:1013–1021. doi: 10.1093/jnen/61.11.1013. [DOI] [PubMed] [Google Scholar]
- Carpentier PA, Begolka WS, Olson JK, Elhofy A, Karpus WJ, Miller SD. Differential activation of astrocytes by innate and adaptive immune stimuli. Glia. 2005;49:360–374. doi: 10.1002/glia.20117. [DOI] [PubMed] [Google Scholar]
- Carpentier PA, Duncan DS, Miller SD. Glial toll-like receptor signaling in central nervous system infection and autoimmunity. Brain Behav Immun. 2008;22:140–147. doi: 10.1016/j.bbi.2007.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan VS, Marriott I. Bacterial infections of the central nervous system: a critical role for resident glial cells in the initiation and progression of inflammation. Curr Immunol Rev. 2007;3:133–143. [Google Scholar]
- Chauhan VS, Sterka DG, Jr, Furr SR, Young AB, Marriott I. NOD2 plays an important role in the inflammatory responses of microglia and astrocytes to bacterial CNS pathogens. Glia. 2009;57:414–423. doi: 10.1002/glia.20770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan VS, Sterka DG, Jr, Gray DL, Bost KL, Marriott I. Neurogenic exacerbation of microglial and astrocyte responses to Neisseria meningitidis and Borrelia burgdorferi. J Immunol. 2008;180:8241–8249. doi: 10.4049/jimmunol.180.12.8241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Y, Benveniste EN. Immune function of astrocytes. Glia. 2001;36:180–190. doi: 10.1002/glia.1107. [DOI] [PubMed] [Google Scholar]
- Dziarski R, Gupta D. The peptidoglycan recognition proteins (PGRPs) Genome Biol. 2006;7:232. doi: 10.1186/gb-2006-7-8-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebert S, Gerber J, Bader S, Mühlhauser F, Brechtel K, Mitchell TJ, Nau R. Dose-dependent activation of microglial cells by Toll-like receptor agonists alone and in combination. J Neuroimmunol. 2005;159:87–96. doi: 10.1016/j.jneuroim.2004.10.005. [DOI] [PubMed] [Google Scholar]
- Esen N, Kielian T. Recognition of Staphylococcus aureus-derived peptidoglycan (PGN) but not intact bacteria is mediated by CD14 in microglia. J Neuroimmunol. 2005;170:93–104. doi: 10.1016/j.jneuroim.2005.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esen N, Kielian T. Central role for MyD88 in the responses of microglia to pathogen-associated molecular patterns. J Immunol. 2006;176:6802–6811. doi: 10.4049/jimmunol.176.11.6802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esen N, Tanga FY, DeLeo JA, Kielian T. Toll-like receptor 2 (TLR2) mediates astrocyte activation in response to the Gram-positive bacterium Staphylococcus aureus. J Neurochem. 2004;88:746–758. doi: 10.1046/j.1471-4159.2003.02202.x. [DOI] [PubMed] [Google Scholar]
- Fournier B, Philpott DJ. Recognition of Staphylococcus aureus by the innate immune system. Clin Microbiol Rev. 2005;18:521–540. doi: 10.1128/CMR.18.3.521-540.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freyer D, Weih M, Weber JR, Bürger W, Scholz P, Manz R, Ziegenhorn A, Angestwurm K, Dirnagl U. Pneumococcal cell wall components induce nitric oxide synthase and TNF-alpha in astroglial-enriched cultures. Glia. 1996;16:1–6. doi: 10.1002/(SICI)1098-1136(199601)16:1<1::AID-GLIA1>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- Girardin SE, Boneca IG, Viala J, Chamaillard M, Labigne A, Thomas G, Philpott DJ, Sansonetti PJ. Nod2 is a general sensor of peptidoglycan through muramyl dipeptide (MDP) detection. J Biol Chem. 2003a;278:8869–8872. doi: 10.1074/jbc.C200651200. [DOI] [PubMed] [Google Scholar]
- Girardin SE, Travassos LH, Herve M, Blanot D, Boneca IG, Philpott DJ, Sansonetti PJ, Mengin-Lecreulx D. Peptidoglycan molecular requirements allowing detection by Nod1 and Nod2. J Biol Chem. 2003b;278:41702–41708. doi: 10.1074/jbc.M307198200. [DOI] [PubMed] [Google Scholar]
- Hoffmann O, Braun JS, Becker D, Halle A, Freyer D, Dagand E, Lehnardt S, Weber JR. TLR2 mediates neuroinflammation and neuronal damage. J Immunol. 2007;190:28–23. doi: 10.4049/jimmunol.178.10.6476. [DOI] [PubMed] [Google Scholar]
- Inohara N, Ogura Y, Fontalba A, Gutierrez O, Pons F, Crespo J, Fukase K, Inamura S, Kusumoto S, Hashimoto M, Foster SJ, Moran AP, Fernandez-Luna JL, Nunez G. Host recognition of bacterial muramyl dipeptide mediated through NOD2. Implications for Crohn's disease. J Biol Chem. 2003;278:5509–5512. doi: 10.1074/jbc.C200673200. [DOI] [PubMed] [Google Scholar]
- Kielian T. Microglia and chemokines in infectious diseases of the nervous system: views and reviews. Front Biosci. 2004;9:732–750. doi: 10.2741/1266. [DOI] [PubMed] [Google Scholar]
- Kielian T, Esen N, Bearden ED. Toll-like receptor 2 (TLR2) is pivotal for recognition of S. aureus peptidoglycan but not intact bacteria by microglia. Glia. 2005;49:567–576. doi: 10.1002/glia.20144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kielian T, Mayes P, Kielian M. Characterization of microglial responses to Staphylococcus aureus: effects on cytokine, costimulatory molecule, and Toll-like receptor expression. J Neuroimmunol. 2002;130:86–99. doi: 10.1016/s0165-5728(02)00216-3. [DOI] [PubMed] [Google Scholar]
- Kim YS, Täuber MG. Neurotoxicity of glia activated by gram-positive bacterial products depends on nitric oxide production. Infect Immun. 1996;64:3148–3153. doi: 10.1128/iai.64.8.3148-3153.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman AP, Pitha PM, Shin HS, Shin ML. Production of tumor necrosis factor and other cytokines by astrocytes stimulated with lipopolysaccharide or a neurotropic virus. Proc Natl Acad Sci USA. 1989;86:6348–6352. doi: 10.1073/pnas.86.16.6348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Han Q, Sun R, Li Z. Dexamethasone regulation of matrix metalloproteinase expression in experimental pneumococcal meningitis. Brain Res. 2008;1207:237–243. doi: 10.1016/j.brainres.2008.01.106. [DOI] [PubMed] [Google Scholar]
- Marriott I, Mason MJ, Elhofy A, Bost KL. Substance P activates NF-kappaB independent of elevations in intracellular calcium in murine macrophages and dendritic cells. J Neuroimmunol. 2000;102:163–171. doi: 10.1016/s0165-5728(99)00182-4. [DOI] [PubMed] [Google Scholar]
- Meli DN, Christen S, Leib SL, Täuber MG. Current concepts in the pathogenesis of meningitis caused by Streptococcus pneumoniae. Curr Opin Infect Dis. 2002;15:253–257. doi: 10.1097/00001432-200206000-00007. [DOI] [PubMed] [Google Scholar]
- Neher JJ, Brown GC. Neurodegeneration in models of Gram-positive bacterial infections of the central nervous system. Biochem Soc Trans. 2007;35:1166–1167. doi: 10.1042/BST0351166. [DOI] [PubMed] [Google Scholar]
- Olson JK, Miller SD. Microglia initiate central nervous system innate and adaptive immune responses through multiple TLRs. J Immunol. 2004;173:3916–3924. doi: 10.4049/jimmunol.173.6.3916. [DOI] [PubMed] [Google Scholar]
- Opitz B, Püschel A, Schmeck B, Hocke AC, Rosseau S, Hammerschmidt S, Schumann RR, Suttorp N, Hippenstiel S. Nucleotide-binding oligomerization domain proteins are innate immune receptors for internalized Streptococcus pneumoniae. J Biol Chem. 2004;279:36426–36432. doi: 10.1074/jbc.M403861200. [DOI] [PubMed] [Google Scholar]
- Pracht D, Elm C, Gerber J, Bergmann S, Rohde M, Seiler M, Kim KS, Jenkinson HF, Nau R, Hammerschmidt S. PavA of Streptococcus pneumoniae modulates adherence, invasion, and meningeal inflammation. Infect Immun. 2005;73:2680–2689. doi: 10.1128/IAI.73.5.2680-2689.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prinz M, Kann O, Draheim HJ, Schumann RR, Kettenmann H, Weber JR, Hanisch UK. Microglial activation by components of gram-positive and -negative bacteria: distinct and common routes to the induction of ion channels and cytokines. J Neuropathol Exp Neurol. 1999;58:1078–1089. doi: 10.1097/00005072-199910000-00006. [DOI] [PubMed] [Google Scholar]
- Rajam G, Phillips DJ, White E, Anderton J, Hooper CW, Sampson JS, Carlone GM, Ades EW, Romero-Steiner S. A functional epitope of the pneumococcal surface adhesin A activates nasopharyngeal cells and increases bacterial internalization. Microb Pathog. 2008;44:186–196. doi: 10.1016/j.micpath.2007.09.003. [DOI] [PubMed] [Google Scholar]
- Rasley A, Anguita J, Marriott I. Borrelia burgdorferi induces inflammatory mediator production by murine microglia. J Neuroimmunol. 2002a;130:22–31. doi: 10.1016/s0165-5728(02)00187-x. [DOI] [PubMed] [Google Scholar]
- Rasley A, Bost KL, Marriott I. Murine gammaherpesvirus-68 elicits robust levels of interleukin-12 p40, but not interleukin-12 p70 production, by murine microglia and astrocytes. J Neurovirol. 2004a;10:171–180. doi: 10.1080/13550280490444119. [DOI] [PubMed] [Google Scholar]
- Rasley A, Bost KL, Olson JK, Miller SD, Marriott I. Expression of functional NK-1 receptors in murine microglia. Glia. 2002b;37:258–267. doi: 10.1002/glia.10034. [DOI] [PubMed] [Google Scholar]
- Rasley A, Marriott I, Halberstadt CR, Bost KL, Anguita J. Substance P augments Borrelia burgdorferi-induced prostaglandin E2 production by murine microglia. J Immunol. 2004b;172:5707–5713. doi: 10.4049/jimmunol.172.9.5707. [DOI] [PubMed] [Google Scholar]
- Rasley A, Tranguch SL, Rati DM, Marriott I. Murine glia express the immunosuppressive cytokine, interleukin-10, following exposure to Borrelia burgdorferi or Neisseria meningitidis. Glia. 2006;53:583–592. doi: 10.1002/glia.20314. [DOI] [PubMed] [Google Scholar]
- Scheld WM, Koedel U, Nathan B, Pfister HW. Pathophysiology of bacterial meningitis: mechanism(s) of neuronal injury. J Infect Dis. 2002;186:S225–S233. doi: 10.1086/344939. [DOI] [PubMed] [Google Scholar]
- Schumann RR, Pfeil D, Freyer D, Buerger W, Lamping N, Kirschning CJ, Goebel UB, Weber JR. Lipopolysaccharide and pneumococcal cell wall components activate the mitogen activated protein kinases (MAPK) erk-1, erk-2, and p38 in astrocytes. Glia. 1998;22:295–305. doi: 10.1002/(sici)1098-1136(199803)22:3<295::aid-glia8>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Sterka D, Jr, Marriott I. Characterization of nucleotide-binding oligomerization domain (NOD) protein expression in primary murine microglia. J Neuroimmunol. 2006;179:65–75. doi: 10.1016/j.jneuroim.2006.06.009. [DOI] [PubMed] [Google Scholar]
- Sterka D, Jr, Rati DM, Marriott I. Functional expression of NOD2, a novel pattern recognition receptor for bacterial motifs, in primary murine astrocytes. Glia. 2006;53:322–330. doi: 10.1002/glia.20286. [DOI] [PubMed] [Google Scholar]
- Strober W, Murray PJ, Kitani A, Watanabe T. Signalling pathways and molecular interactions of NOD1 and NOD2. Nat Rev Immunol. 2006;6:9–20. doi: 10.1038/nri1747. [DOI] [PubMed] [Google Scholar]
- Takada H, Uehara A. Enhancement of TLR-mediated innate immune responses by peptidoglycans through NOD signaling. Curr Pharm Des. 2006;12:4163–4172. doi: 10.2174/138161206778743510. [DOI] [PubMed] [Google Scholar]
- Takeshita S, Takeshita F, Haddad DE, Janabi N, Klinman DM. Activation of microglia and astrocytes by CpG oligodeoxynucleotides. Neuroreport. 2001;12:3029–3032. doi: 10.1097/00001756-200110080-00010. [DOI] [PubMed] [Google Scholar]