Abstract
Staging systems aim to describe malignant tumours in a standardized fashion to assist in therapy planning and estimation of prognosis, allow comparison of different therapeutic strategies, facilitate communication between individuals and institutions, improve our knowledge of malignant disease and ultimately improve the outcome for patients. With the continuous increase in data and, ideally, our understanding of a disease and its potential therapy, every staging system requires continuous adjustment. The TNM staging system by the International Union against Cancer (UICC) is applied worldwide and revised regularly, with intervals aiming at a compromise between up-to-date information on the one hand and providing continuity by avoiding too short-lived revisions on the other hand. The 6th edition was published in 2002 and the 7th edition was published in 2009. The 7th edition became current from January 2010 on.
Keywords: Lung cancer, T staging, N staging, M staging, 7th edition
Tumour entities
With the introduction of the 7th edition of the TNM staging system, it was suggested that this system should be used not only for staging of non-small cell lung cancer (NSCLC) but also for small cell lung cancer (SCLC) and bronchopulmonary carcinoids. Thus, it replaces the much simpler staging system previously used for SCLC (Veteran Administration staging system) reflecting the advances in therapy and prognosis achieved recently (Table 1).
Table 1.
TNM staging system 7th edition
| Stage | Classification |
|---|---|
| T1 | Tumour <3 cm |
| New: T1a <2 cm | |
| New: T1b: 2–3 cm | |
| No infiltration of visceral pleura/main bronchus | |
| No atelectasis | |
| T2 | Tumour >3 cm |
| New: T2a: <5 cm | |
| New: T2b: 5–7 cm | |
| Infiltration of visceral pleura | |
| Infiltration of main bronchus ≥2 cm of carina | |
| Partial atelectasis | |
| T3 | Infiltration of parietal or mediastinal pleura, chest wall, pericardium, diaphragm infiltration of main bronchus <2 cm of carina |
| Atelectasis of complete lung | |
| New: Tumour >7 cm | |
| New: Satellite nodule in the same lobe (previously T4) | |
| T4 | Infiltration of irresectable structures/organs (mediastinum, heart, major vessels, trachea, recurrent laryngeal nerve, oesophagus, vertebral body, carina) |
| New: Satellite nodule in a different lobe of the ipsilateral lung (previously M1) | |
| New: No longer malignant pleural/pericardial effusion (now M1a) | |
| N1 | Ipsilateral peribronchial, hilar |
| N2 | Ipsilateral mediastinal (incl. subcarinal) |
| N3 | Contralateral hilar, mediastinal |
| Ipsi-/contralateral, supraclavicular or scalene lymph nodes (M1: cervical or abdominal lymph nodes) | |
| M1 | New: M1a: malignant pleural/pericardial effusion (previously T4) |
| New: M1b (previously M1): | |
| Haematogenous distant metastases (brain, liver, adrenal, bones, etc.) | |
| Lymphatic distant metastases (cervical, abdominal lymph nodes) | |
| Satellite nodules in contralateral lung (previously: in other lobes than the primary tumour) |
T staging
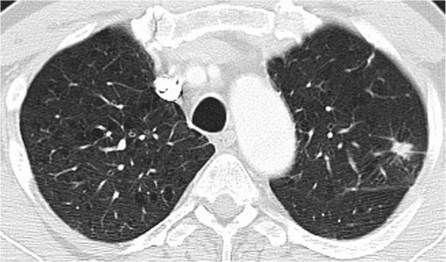
T staging describes the local extent of a tumour, i.e. infiltration of adjacent structures or organs that has an effect on resectability and prognosis. In the 6th edition tumour size was only used to differentiate between T1 (≤3 cm) and T2 (>3 cm). This has been modified so that tumours >7 cm are now classified as T3 independent of other features, and subclassifications have been introduced to describe tumours with a maximum diameter of up to 7 cm by their size more precisely: T1a (≤2 cm, T1b: >2–3 cm, T2a: >3–5 cm, T2b: >5–7 cm). The other features describing infiltration of visceral or parietal pleura, mediastinum, chest wall or other organs have not been changed (Fig. 1).
Figure 1.
NSCLC <2 cm. This is classified as T1a in the 7th edition and was classified as T1 in the 6th edition of the TNM staging system.
N staging
N staging describes whether a lymph node metastasis is located within the visceral pleura, the ipsilateral or contralateral mediastinum, which affects therapy (surgical resection, lymphadenectomy) and prognosis. No changes to the N staging have been introduced with the 7th edition.
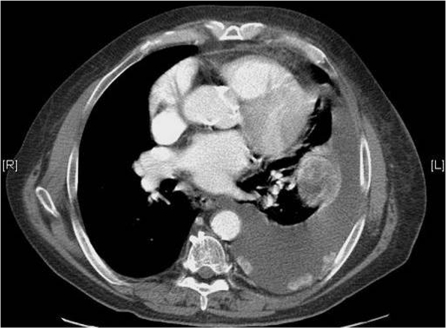
M staging
M staging describes the presence or absence of distant metastases. These usually represent systemic and irresectable disease and a very poor prognosis. With the 7th edition a differentiation was introduced between irresectable spread in the thorax, i.e. malignant pleural and pericardial effusion (now M1a, formerly T4) and extrathoracic spread (now M1b, formerly M1) (Fig. 2).
Figure 2.
Malignant pleural effusion and pleural tumour nodules of the left hemithorax. This is now classified as M1a (formerly T4).
Tumour stages
The changes in the T and in the M staging obviously affect tumour stages in individual cases. Otherwise, no changes have been introduced with the 7th edition.
References
- [1].Goldstraw P, Crowley J, Chansky K, et al. The IASCL international staging project on lung cancer. J Thor Oncol. 2006;1:281–6. doi:10.1097/01243894-200605000-00002. [Google Scholar]
- [2].Sobin LH, Gospodarowicz MK, Wittekind Ch, editors. TNM classification of malignant tumours. 7th. John Wiley & Sons; 2009. [Google Scholar]