Abstract
BACKGROUND
Primary percutaneous coronary intervention (PCI) is more effective on average than fibrinolytic therapy (FT) in the treatment of ST-segment elevation myocardial infarction (STEMI). Yet most U.S. hospitals are not equipped for PCI and FT is still widely used. This study evaluated the comparative effectiveness of STEMI regionalization strategies to increase the use of PCI against standard emergency transport and care.
METHODS AND RESULTS
We estimated incremental treatment costs and quality-adjusted life expectancies of 2,000 patients with STEMI who received PCI or FT in simulations of emergency care in a regional hospital system. To increase access to PCI across the system, we compared a base case strategy to 12 hospital-based strategies of building new PCI labs or extending the hours of existing labs, and one emergency medical services (EMS)-based strategy of transporting all patients with STEMI to existing PCI-capable hospitals. The base case resulted in 609 (569, 647) patients getting PCI. Hospital-based strategies increased the number of patients receiving PCI, the costs of care, and quality-adjusted life years (QALYs) saved, and were cost effective under a variety of conditions. An EMS-based strategy of transporting every patient to an existing PCI facility was less costly and more effective than all hospital expansion options.
CONCLUSION
Our results suggest that new construction and staffing of PCI labs may not be warranted if an EMS strategy is both available and feasible.
Keywords: cost-benefit analysis, fibrinolysis, Percutaneous coronary intervention, ST-segment elevation myocardial infarction, thrombolysis
Background
For patients with ST-segment myocardial infarction (STEMI), primary percutaneous coronary intervention (PCI) is better than fibrinolytic therapy (FT) at reducing mortality if administered in a timely manner.1-3 However, PCI is available only at hospitals with cardiac catheterization labs and FT remains the standard of care in the majority of US hospitals.4 One recent study indicates that 80% of the US population lives within a one-hour drive of a PCI facility, but empirical estimates suggest far fewer than 80% of eligible patients with STEMI actually receive PCI.5, 6
To increase access to PCI, there is considerable interest in regional planning for the procedure,7,8 but few opportunities are available to evaluate regionalization strategies in head-to-head comparisons. In this study, we used our recently developed triage and allocation model9 to compare the incremental benefits and costs of two approaches for increasing patient access to PCI: 1) hospital-based strategies, in which new PCI capacity is added to a region through hospital lab construction and staffing and 2) an emergency medical service (EMS)-based strategy, in which patients with STEMI are transported by EMS to existing PCI-capable hospitals.
Methods
To estimate the costs and effectiveness of alternative strategies for increasing access to PCI, we compared a strategy of standard emergency resources and transport procedures (the base case) with 13 scenarios in which hospital PCI capability was expanded (the hospital-based strategies) and one scenario in which EMS was used to transport all patients with suspected STEMI to an existing PCI-capable hospital (the EMS strategy). The strategies and scenarios are presented in Table 1. The base case (A) assumed that EMS providers transport patients to the closest hospital, regardless of which reperfusion method is available at the time of arrival. This scenario assumed no new PCI lab construction and no new staffing of existing PCI labs. In the base case, two hospitals were capable of performing PCI full time, 12 were capable part-time (Monday through Friday, 7 am – 5 pm), and two were capable of providing FT only. In scenario B, a high-volume hospital that was capable of providing FT only was selected for PCI expansion. This hospital built and staffed a part-time PCI lab and operated it Monday through Friday, 7 am to 5 pm. In this scenario, we assumed that back-up coronary artery bypass graft (CABG) surgery could be provided off site, saving the cost of building and staffing a new suite dedicated to the procedure. In scenario C, we added a CABG suite to the costs in scenario B. All new construction scenarios were tested both with and without a new on-site CABG suite (D and E, G and H, I and J, K and L, M and N). One scenario (F) involved only an increase in staffing hours at two existing PCI-capable hospitals and therefore construction of a new PCI lab and CABG suite were not necessary. The EMS strategy (O) involved EMS transport of patients with suspected STEMI to existing PCI-capable hospitals. In this scenario, we used the regional configuration of hospital PCI capability that existed in scenario A.
Table 1.
STEMI Regionalization Strategies
| Scenario | Strategy | Hospital Capabilities | ||
|---|---|---|---|---|
| Full-time PCI Hospitals |
Part-time PCI Hospitals |
FT-only Hospitals |
||
| Base Case | ||||
| A | No new construction or staffing | 2 | 12 | 2 |
| Hospital Strategies | ||||
| B | One new part-time lab* | 2 | 13 | 1 |
| C | One new part-time lab and CABG suite | 2 | 13 | 1 |
| D | One new full-time lab† | 3 | 12 | 1 |
| E | One new full-time lab and CABG suite | 3 | 12 | 1 |
| F | Night and weekend staffing for two part-time labs | 4 | 10 | 2 |
| G | Night and weekend staffing for two part-time labs and one new part-time lab |
4 | 11 | 1 |
| H | Night and weekend staffing for two part-time labs and one new part-time lab and CABG suite |
4 | 11 | 1 |
| I | Night and weekend staffing for two part-time labs and one new full-time lab |
5 | 10 | 1 |
| J | Night and weekend staffing for two part-time labs and one new full-time lab and CABG suite |
5 | 10 | 1 |
| K | Night and weekend staffing for two part-time labs and two new part-time labs |
4 | 12 | 0 |
| L | Night and weekend staffing for two part-time labs and two new part-time labs and CABG suites |
4 | 12 | 0 |
| M | Night and weekend staffing for two part-time labs and two new full-time labs |
6 | 10 | 0 |
| N | Night and weekend staffing for two part-time labs and two new full-time labs an CABG suites |
6 | 10 | 0 |
| EMS Strategy | ||||
| O | No new construction or staffing - EMS transports only to PCI-capable hospitals |
2 | 12 | 2 |
Staffed Monday-Friday 7 am to 5 pm
Staffed 24 hours/day 7 days/week
We simulated EMS transport, reperfusion strategy, clinical outcomes and costs for 2,000 patients, representing approximately one year of STEMIs in a municipal area the size of Dallas County. We bootstrapped the simulation 500 times and estimated the bootstrap mean and confidence intervals at the 2.5 and 97.5 percentiles.
Patients
Patient data were sampled from the Atlantic Cardiovascular Patient Outcomes Research Team (C-PORT) Trial.10 C-PORT was a randomized controlled trial of 451 patients with STEMI conducted from July 1996 through June 1999 that compared PCI and FT at 11 community-based hospitals in Maryland and Massachusetts. Clinical data needed for the mortality predictive model were available for 408 of the 451 subjects recruited into C-PORT. All hospital-, EMS- and patient-level variables were used in or computed from a model of Dallas County that was built using ArcGIS version 9.1 (Environmental Systems Research Institute, Redlands, CA). The model is described further in previous work.9
Outcomes
We used the Percutaneous Coronary Intervention-Thrombolytic Predictive Instrument (PCI-TPI) to predict 30-day mortality for each patient.11, 12 For individual patients, the PCI-TPI trades off the incremental mortality benefit of PCI over FT with delays to treatment. Rates of post MI stroke, congestive heart failure (CHF) and re-infarction at 30 days and six months were taken from the outcomes literature (Table 2). Survival for each additional year was stochastically estimated from rates published in 2007 National Center for Health Statistics (NCHS) age- and sex-adjusted actuarial tables. We assumed a small additional mortality risk due to MI up to five years after the initial event, an approach that has been shown in previous work22 to calibrate well with five-year survival rates after STEMI.23 In our main analysis we added 0.005 risk of mortality for patients treated with PCI and 0.015 for patients treated with FT. In a sensitivity analysis, we added 0.01 risk to both groups, to explore how results would change if longer-term mortality were equal in the two treatment groups.
Table 2.
Follow up Events, Quality of Life Estimates and Event Rates
| Event | Quality of Life (Lower) |
Quality of Life (Upper) |
Event Rates (PCI) |
Event Rates (FT) |
|---|---|---|---|---|
| Mortality | ||||
| - in-hospital | 0.0413 | 0.06313 | ||
| - 4-6 weeks | 0.051 | 0.071 | ||
| - 6-18 months | ~ 0.0951 | ~ 0.1351 | ||
| Non-fatal Reinfarction | 0.7314 | 0.9114 | ||
| - in-hospital | 0.02513 | 0.06413 | ||
| - 4-6 weeks | 0.031 | 0.071 | ||
| - 6-18 months | ~ 0.051 | ~ 0.11 | ||
| Total Stroke | 0.6015 | 0.8516 | ||
| - in-hospital | 0.002213 | 0.014513 | ||
| - 4-6 weeks | 0.011 | 0.021 | ||
| - 6-18 months | 0.02210 | 0.0410 | ||
| Rescue PCI | ||||
| - in-hospital | 0.13317 | 0.6317 | ||
| - 4-6 weeks | 0.1910 | 0.4910 | ||
| - 6 months | 0.23610 | 0.49610 | ||
| CABG | ||||
| - in-hospital | 0.08217 | 0.1217 | ||
| - 4-6 weeks | 0.12410 | 0.18610 | ||
| - 6 months | (flat) | (flat) | ||
| CHF | 0.6318 | 0.8519 | ||
| - in-hospital | (flat) | 0.1820 | ||
| - 4-6 weeks | 0.15221 | (flat) | ||
| - 6 months | (flat) | (flat) |
For every year survived, we adjusted for reduced quality of life from complications related to the index event or to the mode of reperfusion. Utility estimates for stroke, CHF and re-infarction were drawn from the Cost Effectiveness Analysis Registry24 (Table 2). We used high and low estimates from a search of the Registry to estimate the upper and lower bounds for each utility measure. We assumed the higher bound in our main analysis, and the lower bound in a sensitivity analysis. Future years were discounted at 3% per year in our main analysis and at 5% in sensitivity analyses.
Our main analysis thus assumed unequal risk of death in the two treatment groups at year one after the index event, a high quality of life after complications, and a 3% discount for future years. In sensitivity analyses, we changed these assumptions individually and simultaneously to account for uncertainty surrounding survival, quality of life, and discounting.
Costs
We updated a previously developed framework for hospital operations and costs25 to 2008 U.S. dollars, using the National Income and Product Accounts (NIPA) GDP deflator.26 We assumed that newly purchased lab equipment and facilities would be in use for 10 years.
In randomized controlled trials comparing PCI and FT, the initial costs of PCI have been higher typically, but additional complication and procedure rates in the FT arm have been found to yield similar cumulative costs.27-29 Two studies from the mid-1990s drew different conclusions: one using registry data found lower costs in the FT group30 and another using administrative data found lower costs in the PCI group.31 Our base case assumed equal costs for PCI and FT over the lifetime of patients. In each successive scenario, we added costs when new construction, staffing, in-hospital CABG back-up or diverted transport was needed.
SAS version 9.1 (SAS Institute, Cary, NC) was used for all statistical analyses.
Results
Table 3 shows the number of new PCI patients, total costs, QALYs saved and cost per QALY for each of the 14 scenarios. In the base case (A), 609 (95% confidence interval: 569, 647) primary PCI procedures – representing 30.4% of all patients with STEMI – were performed annually in 14 hospitals. Roughly 250 of these were performed during weekdays at a time when elective procedures would otherwise be scheduled. With 14 PCI labs operating on 260 weekdays per year, we assumed that demand for elective PCI was already being met and that no additional elective procedures would be performed as a result of new capacity. In this context, new construction and staffing costs could not be defrayed with elective procedures.
Table 3. Cost Effectiveness of Strategies to Increase Access to PCI.
Incremental cost-effectiveness ratios are presented in the last column, measured as the cost in 2008 dollars per quality-adjusted life year saved. Strategies are presented in order from least to most cost-effective. Results assume: risk of death is unequal for the two treatment groups through 5 years after treatment; an upper bound for health-related quality of life if survival with STEMI is followed by stroke, CHF, or re-infarction; and future years discounted at 3%.
| Scenario | Strategy | PCI Patients N=2,000 % (s.d.) |
New PCI Patients (n) |
Costs in 2008 Dollars (1000s) |
QALYs Saved (95% CI) |
Cost per QALY (95% CI) |
|---|---|---|---|---|---|---|
| Base Case | ||||||
| A | No new construction or staffing | 30.4 (1.0) |
||||
| EMS Strategy | ||||||
| O | No new construction or staffing - EMS transports only to PCI-capable hospitals |
100 (0.0) |
1391 | 1,391 | 2749.8 (2678.4-2936.6) |
506 (474-519) |
| Hospital Strategies | ||||||
| F | Night and weekend staffing for two part-time labs |
45.6 (1.1) |
304 | 6,052 | 605.2 (550.8-788.8) |
10,000 (7,673-10,988) |
| I | Night and weekend staffing for two part-time labs and one new full-time lab |
59.2 (1.1) |
576 | 13,863 | 1125.6 (1109.4-1210.6) |
12,316 (11,451-12,496) |
| G | Night and weekend staffing for two part-time labs and one new part-time lab |
49.7 (1.1) |
385 | 10,837 | 754.0 (719.2-877.0) |
14,373 (12,357-15,068) |
| D | One new full-time lab | 44.0 (1.1) |
272 | 7,811 | 529.0 (544.8-650.2) |
14,765 (12,013-14,337) |
| M | Night and weekend staffing for two part-time labs and two new full-time labs |
61.3 (1.1) |
617 | 21,674 | 1247.0 (1147.2-1356.0) |
17,381 (15,984-18,893) |
| K | Night and weekend staffing for two part-time labs and two new part-time labs |
50.3 (1.1) |
398 | 15,622 | 788.6 (803.0-1039.0) |
19,810 (15,035-19,454) |
| J | Night and weekend staffing for two part-time labs and one new full-time lab and CABG suite |
59.2 (1.1) |
576 | 22,462 | 1125.6 (1109.4-1210.6 |
19,956 (18,555-20,247) |
| H | Night and weekend staffing for two part-time labs and one new part-time lab and CABG suite |
49.7 (1.1) |
385 | 19,436 | 754.0 (719.2-877.0) |
25,778 (22,162-27,025) |
| B | One new part-time lab | 34.5 (1.0) |
82 | 4,785 | 157.4 (37.2-302.8) |
30,399 (15,802-128,623) |
| E | One new full-time lab and CABG suite |
44.0 (1.1) |
272 | 16,410 | 529.0 (544.8-650.2) |
31,021 (25,239-30,122) |
| N | Night and weekend staffing for two part-time labs and two new full-time labs and CABG suites |
61.3 (1.1) |
617 | 38,873 | 1247.0 (1147.2-1356.0 |
31,173 (28,667-33,885) |
| L | Night and weekend staffing for two part-time labs and two new part-time labs and CABG suites |
50.3 (1.1) |
398 | 32,820 | 788.6 (803.0-1039.0) |
41,619 (31,588-40,872) |
| C | One new part-time lab and CABG suite |
34.5 (1.0) |
82 | 13,384 | 157.4 (37.2-302.8) |
85,032 (44,201-359,787) |
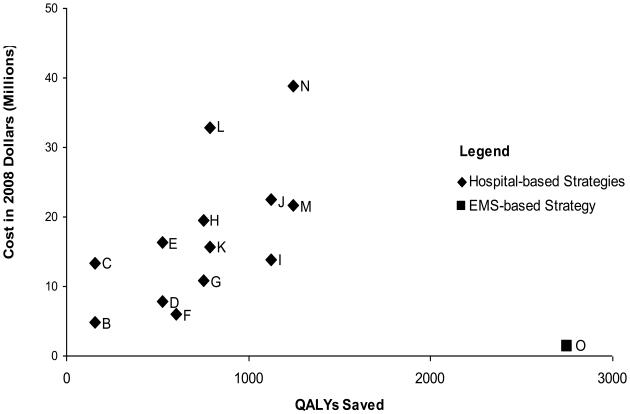
The costs and effectiveness of each successive scenario (B-O) were compared with the base case (A). An additional 82 patients had access to PCI after construction of a new part-time lab in a hospital seeing more than 200 patients with STEMI annually (B). This scenario resulted in nearly $4.8M additional costs over 10 years and the additional 82 PCI procedures performed over this period saved 157.4 QALYs. The cost per QALY saved was $30,399, well under the costs of other accepted life-saving therapies. When that same hospital built a new lab and staffed it full time (D), an additional 272 PCI treatments could be performed in a year and the cost per QALY saved dropped to $14,765. If a new program of on-site CABG back-up was needed for this new lab, costs increased to $85,032 per QALY saved in the part-time scenario (C) and to $31,021 in the full time scenario (E). Building a new lab was most cost-effective if it could be opened full time and if a new on-site CABG back-up program was unnecessary (D). Costs per QALY saved are graphed for each scenario in Figure 1.
Figure 1. STEMI Regionalization Strategies - Cost per Quality Adjusted Life Year.
Quality-adjusted life years saved are presented on the x-axis and cost in 2008 dollars on the y-axis. The base strategy is positioned at (0,0). Hospital strategies (B-N) are depicted with a diamond. The EMS strategy (O) is depicted with a square.
Expansion of PCI capability in the two highest volume hospitals that already had a part-time PCI lab in place (F) resulted in 304 additional procedures and 605.2 QALYs saved at a cost of $10,000 per QALY saved. This expansion, involving only the additional costs of night and weekend on-call staff, was the most cost effective of hospital-based scenarios. We explored a series of combinations involving new lab construction and expansion of part-time PCI labs to full-time hours (G-N). When compared with the base case, each scenario cost less than $100,000 per QALY saved.
Finally, we estimated the incremental costs and effectiveness of one EMS strategy for increasing access to PCI (O). In this scenario, EMS personnel identified patients with STEMI prior to hospital arrival and transported directly to PCI-capable hospitals. Because our previous work on EMS triage strategies for PCI9 showed this approach to achieve the largest reduction in short-term mortality, we selected direct transport as the EMS strategy of interest for the present study. A strategy of inter-hospital transfer performed almost as well in our previous work and is of interest for our future work. For the present study, we assumed the EMS transport strategy would cost an additional $1,000 per diverted patient.
In 2,000 patients, this strategy resulted in 1,391 diversions at a cost of nearly $1.4M and a cost per QALY saved of $506. Because it was less costly and more effective than any of the hospital-based strategies, we considered the EMS strategy to be dominant. It would no longer be the most cost-effective strategy if the average cost per diverted patient rose to more than $19,769 (a 20-fold increase). Alternatively, it would no longer be the most cost effective strategy if the most favorable hospital-based scenario (F) cost less than $306,231 (a 20-fold decrease).
We assumed 100% adherence to each tested strategy, including that all patients call 9-1-1 for assistance. This assumption could lead to an overestimate of benefit for the EMS strategy in an actual regional emergency system, where nearly half of all patients with STEMI arrive at the hospital via transportation other than EMS.32 Evidence suggests patients who arrive via EMS are older, higher risk, and more likely to benefit from PCI than those who arrive by other means.32 To test the sensitivity of our results to 100% adherence, we iteratively reduced the EMS strategy's total benefit by the average benefit per diverted patient until the strategy was no longer more effective than the next most effective hospital strategy. This method would indicate how many walk-ins would be needed until the EMS strategy was no longer dominant. In the EMS strategy (O), 1391 patients were diverted, producing a total benefit of 2749.8 QALYs, or an average benefit of 1.98 QALYs per diverted patient. The next most beneficial strategy (M) produced 1247.0 QALYs. To fall below this level of benefit, 762 of 1391 diversions (55%) would have to be replaced by walk-ins. The EMS strategy would therefore continue to be more effective and less costly than the next best hospital strategy if at least 45% of all patients with STEMI were to call 9-1-1 for assistance. Below that number, the EMS strategy would continue to be more cost effective but would not dominate hospital strategies. This calculation is conservative if patients who are more likely to benefit from PCI are more likely to call 9-1-1, as the evidence suggests they are.
Conclusion
To increase access to PCI in our model of a large urban, suburban and rural region, an EMS strategy of transporting all patients to existing PCI-capable hospitals was more effective and less costly than 13 hospital-based strategies of new construction and staffing. While hospital strategies were cost-effective under a variety of conditions, the EMS strategy dominated in all of the scenarios we tested and in multivariate sensitivity analyses. Our results strongly suggest that construction and staffing of new PCI hospitals may not be warranted if an EMS strategy is both available and feasible. Demonstration programs have shown that EMS detection and diversion of patients with STEMI for delayed PCI are both safe and effective.33,34 Our results suggest that, in EMS systems where STEMI detection and diversion are feasible, such a strategy is more effective and less costly than hospital-based regionalization alternatives. This finding persisted even when the estimated new cost of an EMS strategy was multiplied by a factor of nearly 20, or when its expected benefits were decreased by 55% or more.
Expansion of access to timely PCI is widely considered to be critical for improving outcomes after STEMI. To accomplish this goal, a range of regionalization approaches have been reviewed or evaluated in the research literature.35-39 In order to understand the potential of STEMI regionalization strategies in their full context, however, it is critical that the benefits, risks and costs of all hospital- and EMS strategies be compared in head-to-head match-ups. While the preferred method to compare such strategies might be a randomized effectiveness trial,40 such an approach would not likely be feasible given the large numbers needed to measure rare outcomes after heart attack, as well as the ethical problem of randomizing patients to receive FT when timely PCI is known to be superior.
In this context, the use of mathematical modeling to compare predicted outcomes from PCI expansion strategies is a promising approach. The model we employed combined empirical data from clinical, health systems and geographic sources with clinical predictive instruments to perform head-to-head comparisons of regionalization strategies. Our model for estimating outcomes was sensitive to the number of new PCI treatments resulting from an expansion strategy, and therefore to the regional population's baseline rate of access to PCI. In our model of Dallas County, we estimated a baseline access rate of 30.4%. Two aspects of our model explain why our baseline rate was 50 percentage points lower than a recent national estimate indicating that 80% of the population lives within a one-hour drive of a PCI-capable hospital.4 First, patients in our base case were transported to the closest hospital even if PCI was available within a one-hour drive. Second, the 80% estimate assumes that hospitals with a PCI lab operate the lab 24 hours per day, 7 days per week. Of the 16 hospitals in our model of a large county, 14 had a PCI lab but only two operated the lab full-time. In the base case, we operated the part-time PCI labs from Monday through Friday, 7 am to 5 pm. Two classic papers on the circadian and weekly patterns of heart attack onset estimate that approximately 39% begin during these weekday hours.41,42 We used these estimates to stochastically estimate STEMI onset day and time. In our model, therefore, approximately 61% of patients with STEMI onset in locations served by a part-time lab received immediate FT in the local hospital or delayed PCI after transport to a more distant full-time lab. We believe that our method of accounting for the part-time operation of PCI labs is reflective of actual operations in a region that has not yet introduced regionalization measures. Assuming full-time operation at all hospitals would have led to a significant overestimate of the true baseline access rate.
Nevertheless, in regions with a higher baseline rate of access to primary PCI, we would expect that an EMS strategy would fare better and the hospital strategies would fare worse than in our model. In a hospital strategy, the high fixed costs of construction can be defrayed only by increasing the number of patients with newly created access to PCI. In an EMS strategy, new costs are substantially lower and vary with the number of new transports that are needed. This relatively low variable cost is the primary advantage of an EMS strategy. A second advantage was explored in our previous work: the opportunity to select for transport to existing PCI hospitals only those patients who are predicted to benefit most from PCI. We did not exploit this opportunity in the present study; we transported every patient with suspected STEMI directly to a PCI-capable hospital regardless of predicted benefit. The EMS strategy dominated hospital strategies on the basis of its low variable costs and its potential to reach every patient with STEMI, but we believe an even stronger case could be made for a strategy that involves selective transport of only those patients who are individually predicted to benefit from delayed PCI.
Public policy remains unsettled on the optimal strategy to increase access to PCI. In some states, Certificate of Need laws are used to control the widespread diffusion of high cost and volume-sensitive procedures such as PCI. In 2008, these laws existed in 36 States, but only 23 had provisions for cardiac catheterization services review.43 From 2001 through 2006, American Hospital Association (AHA) data show a steady increase of 50-125 new hospitals with PCI capability in the US each year, in both urban and rural areas.44,45 There is substantial contradictory activity in the public arena that is aimed both at curtailing and at sustaining the diffusion of PCI labs. We believe our approach to comparing alternative strategies can help clarify the impact of such decisions.
For several reasons, Dallas County represents an ideal place to test our model. First, Dallas has a diversity of urban, suburban and rural areas. The majority of Census tracts in Dallas County are designated as urban (comprising 69.7% of the county's dry land area), but a substantial portion of the county is suburban and rural. Second, there is significant variation in PCI capability at hospitals inside the county. Our model showed that just 30.4% of the county's population lived closest to a PCI-capable hospital, leaving substantial room for growth in the availability of PCI. Third, Dallas is bordered to the north, east and south by sparsely populated areas and to the west by Dallas-Fort Worth Airport, creating natural and man-made barriers to EMS transport outside the County's borders. These factors allowed us to test the EMS strategy inside a diverse yet nearly closed emergency system.
While Dallas offered an excellent choice for the first test of our model, large and less densely populated regions are of great interest for further testing. In rural areas where access to PCI is lowest, the need for further study is especially urgent. Empirical evidence suggests that new hospital PCI capability results in modest new access to PCI.37 To answer the question about what works best in urban, suburban and rural counties, head-to-head comparisons of all available strategies are needed. Our triage and allocation model can help planners and policy-makers decide on the approach that best fits the specific features of a county or region.
Our main finding, that an EMS strategy is more effective and less costly than any hospital strategy, was based on the estimated societal impact of alternative regional planning strategies in the care of patients with STEMI. The implications for individual hospitals are less clear. However, if it were recast to take in the hospital perspective, our model could help to inform the business case for regional planning. This would lend a great deal of clarity to discussion about the implications of our main finding.
In some circumstances, we recognize that a hospital strategy may be warranted even when it is dominated by an EMS strategy. First, resource constraints may preclude EMS strategies from being considered. Ambulance staff must be able to identify patients with STEMI accurately, the vehicles must be equipped with electrocardiograms, and EMS-hospital handoff should be organized to pre-notify receiving hospitals. Second, hospital expansion may be of particular importance in some suburban and rural settings, where the risks of exceptionally lengthy drive times to PCI hospitals can be prohibitive. Third, hospital strategies may be acceptable or desirable if the geographic distribution of PCI hospitals is inequitable and hospital expansion could lead to outcome improvements for a presently underserved population.
Our study has limitations. First, there are limitations inherent to simulations, insofar that they incorporate empirical data from multiple sources and resort to assumptions where empirical data are not available. Our simulation was no different in this regard. However, we conducted a wide range of multivariate sensitivity analyses and the results were robust to all potential changes. Perhaps the strongest assumptions we made concerned the costs of EMS transport and hospital lab construction, which were estimated from a study of new construction and staffing at U.S. hospitals from the mid-1990s. We chose this model because it allowed us to compare a range of hospital costs in discrete categories and thus to compare 13 alternative hospital strategies with each other and with the EMS strategy. We updated the cost model using the most reliable index for inflation of medical care and construction costs, the National Income Products Account (NIPA) GDP deflator. In a sensitivity analysis, our main finding was robust to changes in baseline costs by a factor of nearly 20 across the board. A second important assumption included adherence to the tested strategies. We assumed that 100% of patients use 9-1-1, an assumption that would lead to overestimates of benefit in the EMS strategy in locales where hospital walk-ins occur at a high rate. In a post hoc sensitivity analysis, our findings were robust until 55% or more of patients arrive to the hospital by means other than EMS. A third important set of assumptions included the utility weights for quality adjustment. In sensitivity analyses, we used high and low estimates from a search of the Cost Effectiveness Analysis Registry to estimate the upper and lower bounds for each utility measure in our model. Quality adjustment had minor effects on the ordering of preferred hospital strategies, but did not change the main result showing that the EMS strategy was both more effective and less costly than all hospital strategies.
A second limitation was that we conducted the study in a single county. We selected Dallas County for its size, diversity, and composition of urban, suburban and rural districts, but the primary advantage of this setting was its self-contained emergency system. Further research is planned in a broadly representative sample of U.S. counties.
In summary, while expansion of hospital PCI capability can be cost-effective for improving quality-adjusted survival after STEMI, a strategy of EMS transport to existing PCI-capable hospitals was dominant in a regional hospital system with 30% baseline access to PCI. Further inquiry is needed into the relationship of regional health system characteristics and optimal strategies for increasing access to PCI, and we have begun a five-year research project funded by the Agency for Healthcare Research and Quality (AHRQ) to explore these relationships. Our results suggest that regional planners should consider EMS strategies for increasing access to PCI before adopting strategies involving new construction or increased staffing of PCI hospitals.
Acknowledgements
Dr. Concannon was assisted by Daniel J. Baldor, B.A., in the preparation of the manuscript.
Funding Sources: Dr. Concannon was supported by the Agency for Healthcare Research and Quality (R01 HS010282, T32 HS00060-12; and K01 HS017726) and by the Tufts Medical Center-Pfizer Career Development Award. Dr. Kent was also supported through AHRQ (R01 HS010282). Dr. Selker, Dr. Griffith and Ms. Beshansky were supported by the Immediate Myocardial Metabolic Enhancement During Initial Assessment and Treatment in Emergency (IMMEDIATE) care trial, National Heart, Lung, and Blood Institute (U01 HL 0778241). Scientific assistance was also provided through the Tufts Clinical and Translational Science Award (UL1 RR025752).
Footnotes
Disclosures: The funding organizations had no role in the design and conduct of the study; collection management, analysis, and interpretation of the data; and preparation, review or approval of the manuscript.
Conflict of Interest Disclosures: None
References
- 1.Keeley EC, Boura JA, Grines CL. Primary Angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 2.Kent DM, Lau J, Selker HP. Balancing the benefits of primary angioplasty against the benefits of thrombolytic therapy for acute myocardial infarction: the importance of timing. Eff Clin Pract. 2001;4:214–20. [PubMed] [Google Scholar]
- 3.Nallamothu BK, Bates ER. Percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: is timing (almost) everything? Am J Cardiol. 2003;92:824–6. doi: 10.1016/s0002-9149(03)00891-9. [DOI] [PubMed] [Google Scholar]
- 4.Nallamothu BK, Bates ER, Wang Y, Bradley EH, Krumholz HM. Driving times and distances to hospitals with percutaneous coronary intervention in the United States: Implications for prehospital triage of patients with ST-elevation myocardial infarction. Circulation. 2006;113:1189–1195. doi: 10.1161/CIRCULATIONAHA.105.596346. [DOI] [PubMed] [Google Scholar]
- 5.Rogers WJ, Canto JG, Lambrew CT, Tiefenbrunn AJ, Kinkaid B, Shoultz DA, Frederick PD, Every N. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999: the National Registry of Myocardial Infarction 1, 2 and 3. J Am Coll Cardiol. 2000;36:2056–63. doi: 10.1016/s0735-1097(00)00996-7. [DOI] [PubMed] [Google Scholar]
- 6.Nallamothu BK, Blaney ME, Morris SM, Parsons L, Miller DP, Canto JG, Barron HV, Krumholz HM. Acute reperfusion therapy in ST-elevation myocardial infarction from 1994-2003. Am J Med. 2007;120:693.e1–693.e8. doi: 10.1016/j.amjmed.2007.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacobs AK, Antman EM, Ellrodt G, Faxon DP, Gregory T, Mensah GA, Moyer P, Ornato J, Peterson ED, Sadwin L, Smith SC. Recommendation to develop strategies to increase the number of ST-segment-elevation myocardial infarction patients with timely access to primary percutaneous coronary intervention. Circulation. 2006;113:2152–63. doi: 10.1161/CIRCULATIONAHA.106.174477. [DOI] [PubMed] [Google Scholar]
- 8.Jacobs AK, Antman EM, Faxon DP, Gregory T, Solis P. Development of systems of care for ST-elevation myocardial infarction patients. Executive Summary. Circulation. 2007;116:217–30. doi: 10.1161/CIRCULATIONAHA.107.184043. [DOI] [PubMed] [Google Scholar]
- 9.Concannon TW, Kent DM, Normand SL, Newhouse JP, Griffith JL, Ruthazer R, Beshansky JR, Wong JB, Aversano T, Selker HP. A geospatial analysis of emergency transport and inter-hospital transfer in ST-segment elevation myocardial infarction. Am J Cardiol. 2008;101:69–74. doi: 10.1016/j.amjcard.2007.07.050. [DOI] [PubMed] [Google Scholar]
- 10.Aversano T, Aversano LT, Passamani E, Knatterud GL, Terrin ML, Williams DO, Forman SA. Thrombolytic therapy vs primary percutaneous coronary intervention for myocardial infarction in patients presenting to hospitals without on-site cardiac surgery: a randomized controlled trial. JAMA. 2002;287:1943–51. doi: 10.1001/jama.287.15.1943. [DOI] [PubMed] [Google Scholar]
- 11.Kent DM, Ruthazer R, Griffith JL, Beshansky JR, Grines CL, Aversano T, Concannon TW, Zalenski RJ, Selker HP. Comparison of mortality benefit of immediate thrombolytic therapy versus delayed primary angioplasty for acute myocardial infarction. Am J Cardiol. 2007;99:1384–8. doi: 10.1016/j.amjcard.2006.12.068. [DOI] [PubMed] [Google Scholar]
- 12.Kent DM, Ruthazer R, Griffith JL, Beshanksy JR, Aversano T, Concannon TW, Grines CL, Zalenski RJ, Selker HP. A percutaneous coronary intervention-thrombolytic predictive instrument to assist choosing between immediate thrombolytic therapy versus delayed primary percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol. 2008;101:790–5. doi: 10.1016/j.amjcard.2007.10.050. [DOI] [PubMed] [Google Scholar]
- 13.Grines C, Patel A, Zijlstra F, Weaver WD, Granger C, Simes RJ. Primary coronary angioplasty compared with intravenous thrombolytic therapy for acute myocardial infarction: six-month follow up and analysis of individual patient data from randomized trials. Am Heart J. 2003;145:47–57. doi: 10.1067/mhj.2003.40. [DOI] [PubMed] [Google Scholar]
- 14.Nagata-Kobayashi S, Shimbo T, Matsui K, Fukui T. Cost-effectiveness of pravastatin for primary prevention of coronary artery disease in Japan. International Journal of Cardiology. 2005;104:213–223. doi: 10.1016/j.ijcard.2004.12.016. [DOI] [PubMed] [Google Scholar]
- 15.Brown DL, Lisabeth LD, Roychoudhury C, Ye Y, Morgenstern LB. Recurrent stroke risk is higher than cardiac event risk after initial stroke/transient ischemic attack. Stroke. 2005;36:1285–1287. doi: 10.1161/01.STR.0000165926.74213.e3. [DOI] [PubMed] [Google Scholar]
- 16.Chambers MG, Koch P, Hutton J. Development of a decision-analytic model of stroke care in the United States and Europe. Value Health. 2002;5:82–97. doi: 10.1046/j.1524-4733.2002.52011.x. [DOI] [PubMed] [Google Scholar]
- 17.Grines CL, Browne KF, Marco J, Rothbaum D, Stone GW, O'Keefe J, Overlie P, Donohue B, Chelliah N, Timmis GC. A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The Primary Angioplasty in Myocardial Infarction Study Group. N Engl J Med. 1993;328:673–9. doi: 10.1056/NEJM199303113281001. [DOI] [PubMed] [Google Scholar]
- 18.Capomolla S, Febo O, Ceresa M, Caporotondi A, Guazzotti G, La Rovere MT, Ferrari M, Lenta F, Baldin S, Vaccarini C, Gnemmi M, Pinna G, Maestri R, Abelli Paola, Verdirosi S. Cost/utility ratio in chronic heart failure: comparison between heart failure management program delivered by day-hospital and usual care. J Am Coll Cardiol. 2002;40:1259–1266. doi: 10.1016/s0735-1097(02)02140-x. [DOI] [PubMed] [Google Scholar]
- 19.Kuntz KM, Tsevat J, Weinstein MC, Goldman L. Expert panel vs decision-analysis recommendations for postdischarge coronary angiography after myocardial infarction. JAMA. 1999;282:2246–2251. doi: 10.1001/jama.282.23.2246. [DOI] [PubMed] [Google Scholar]
- 20.O'Connor GT, Quinton HB, Traven ND, Ramunno LD, Dodds TA, Marciniak TA, Wennberg JE. Geographic variation in the treatment of acute myocardial infarction: the Cooperative Cardiovascular Project. JAMA. 1999;281:627–633. doi: 10.1001/jama.281.7.627. [DOI] [PubMed] [Google Scholar]
- 21.The GUSTO Investigators An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. N Engl J Med. 1993;329:673–682. doi: 10.1056/NEJM199309023291001. [DOI] [PubMed] [Google Scholar]
- 22.Kent DM, Vijan S, Hayward RA, Griffith JL, Beshansky JR, Selker HP. Tissue plasminogen activator was cost-effective compared to streptokinase in only selected patients with acute myocardial infarction. J Clin Epidemiol. 2004;57:843–52. doi: 10.1016/j.jclinepi.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 23.Zijlstra F. Long-term benefit of primary angioplasty compared to thrombolytic therapy for acute myocardial infarction. Eur Heart J. 2000;21:1487–9. doi: 10.1053/euhj.2000.2192. [DOI] [PubMed] [Google Scholar]
- 24.Center for the Evaluation of Value and Risk in Health The Cost-Effectiveness Analysis Registry, Institute for Clinical Research and Health Policy Studies, Tufts Medical Center. 2009 Available from: www.cearegistry.org.
- 25.Lieu TA, Lundstrom RJ, Ray GT, Fireman BH, Gurley RJ, Parmley WW. Initial cost of primary angioplasty for acute myocardial infarction. J Am Coll Cardiol. 1996;28:882–889. doi: 10.1016/s0735-1097(96)00237-9. [DOI] [PubMed] [Google Scholar]
- 26.Newhouse JP. The Baxter Foundation Prize Address: Measuring medical prices and understanding their effects. The Journal of Health Administration Education. 1988;7:19–26. [PubMed] [Google Scholar]
- 27.Reeder GS, Bailey KR, Gersh BJ, Holmes DR, Jr., Christianson J, Gibbons RJ. Cost comparison of immediate angioplasty versus thrombolysis followed by conservative therapy for acute myocardial infarction: a randomized prospective trial. Mayo Coronary Care Unit and Catheterization Laboratory Groups. Mayo Clin Proc. 1994;69:5–12. doi: 10.1016/s0025-6196(12)61604-8. [DOI] [PubMed] [Google Scholar]
- 28.de Boer MJ, van Hout BA, Liem AL, Suryapranata H, Hoorntje JC, Zijlstra F. A cost-effective analysis of primary coronary angioplasty versus thrombolysis for acute myocardial infarction. Am J Cardiol. 1995;76:830–3. doi: 10.1016/s0002-9149(99)80238-0. [DOI] [PubMed] [Google Scholar]
- 29.Stone GW, Grines CL, Rothbaum D, Brown KF, O'Keefe J, Overlie PA, Donohue BC, Chelliah N, Vlietstra R, Catlin T, O'Neill WW. Analysis of the relative costs and effectiveness of primary angioplasty versus tissue-type plasminogen activator: the Primary Angioplasty in Myocardial Infarction (PAMI) trial. The PAMI Trial Investigators. J Am Coll Cardiol. 1997;29:901–7. doi: 10.1016/s0735-1097(97)00041-7. [DOI] [PubMed] [Google Scholar]
- 30.Every NR, Parsons LS, Hlatky M, Martin JS, Weaver WD. A comparison of thrombolytic therapy with primary coronary angioplasty for acute myocardial infarction. Myocardial Infarction Triage and Intervention Investigators. N Engl J Med. 1996;335:1253–60. doi: 10.1056/NEJM199610243351701. [DOI] [PubMed] [Google Scholar]
- 31.Lieu TA, Gurley RJ, Lundstrom RJ, Ray GT, Fireman BH, Weinstein MC, Parmley WW. Projected cost-effectiveness of primary angioplasty for acute myocardial infarction. J Am Coll Cardiol. 1997;30:1741–50. doi: 10.1016/s0735-1097(97)00391-4. [DOI] [PubMed] [Google Scholar]
- 32.Canto JG, Zalenski RJ, Ornato JP, Rogers WJ, Kiefe CI, Magid D, Shlipak MG, Frederick PD, Lambrew CG, Littrell KA, Barron HV. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the National Registry of Myocardial Infarction 2. Circulation. 2002;106:3018–23. doi: 10.1161/01.cir.0000041246.20352.03. [DOI] [PubMed] [Google Scholar]
- 33.Moyer P, Ornato JP, Brady WJ, Jr., Davis LL, Ghaemmaghami CA, Gibler BW, Mears G, Mosesso VN, Jr., Zane RD. Development of systems of care for ST-elevation myocardial infarction patients. The emergency medical services and emergency department perspective. Circulation. 2007;116:e43–e48. doi: 10.1161/CIRCULATIONAHA.107.184047. [DOI] [PubMed] [Google Scholar]
- 34.Le May MR, So DY, Dionne R, Glover CA, Froeschl MPV, Wells GA, Davies RF, Sherrard HL, Maloney J, Marquis J-F, O”Brien ER, Trickett J, Poirer P, Ryan SC, Ha A, Joseph PG, Labinaz M. A citywide protocol for primary PCI in ST-segment elevation myocardial infarction. N Engl J Med. 2008;358:231–40. doi: 10.1056/NEJMoa073102. [DOI] [PubMed] [Google Scholar]
- 35.Rokos IC, Larson DM, Henry TD, Koenig WJ, Eckstein M, French WJ, Granger CB, Roe MT. Rationale for establishing regional ST-elevation myocardial infarction receiving center (SRC) networks. Am Heart J. 2006;152:661–7. doi: 10.1016/j.ahj.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 36.Topol EJ, Kereiakes DJ. Regionalization of care for acute ischemic heart disease: a call for specialized centers. Circulation. 2003;107:1463–6. doi: 10.1161/01.cir.0000063680.45780.a0. [DOI] [PubMed] [Google Scholar]
- 37.Pollack CV, Diercks DB, Roe MT, Peterson ED. 2004 American College of Cardiology/American Heart Association guidelines for the management of patients with ST-elevation myocardial infarction: implications for emergency department practice. Annals of Emergency Medicine. 2005;45:363–76. doi: 10.1016/j.annemergmed.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 38.Moyer P, Feldman J, Levine J, Beshansky J, Selker HP, Barnewolt B, Brown DF, Cardoza JP, Jr., Grossman SA, Jacobs A, Kerman B, Kimmelstein C, Larson R, Losordo D, Perlmutter M, Pozner C, Ramirez A, Rosenfield K, Ryan TJ, Zane RD, Cannon CP. Implications of the Mechanical (PCI) vs. thrombolytic controversy for ST segment elevation myocardial infarction on the organization of emergency medical services: the Boston EMS experience. Crit Pat Cardiol. 2004;3:53–61. doi: 10.1097/01.hpc.0000128714.35330.6d. [DOI] [PubMed] [Google Scholar]
- 39.Jacobs AK, Antman EM, Faxon DP, Gregory T, Solis P. Development of systems of care for ST-elevation myocardial infarction patients: executive summary. Circulation. 2007;116:217–30. doi: 10.1161/CIRCULATIONAHA.107.184043. [DOI] [PubMed] [Google Scholar]
- 40.Tunis SM. Implementing Comparative Effectiveness Research: Priorities, Methods, and Impact. Engleberg Center for Health Care Reform at Brookings; 2009. Strategies to improve comparative effectiveness research methods and data infrastructure. Discussion Papers. [Google Scholar]
- 41.Muller JE, Stone PH, Turi ZG, Rutherford JD, Czeisler CA, Parker C, Poole K, Passamani E, Powers R, Robertson T, Sobel BE, Willerson JT, Braunwald E. the MILIS Study Group. Circadian variation in the frequency of onset of acute myocardial infarction. N Engl J Med. 1985;313:1315–1322. doi: 10.1056/NEJM198511213132103. [DOI] [PubMed] [Google Scholar]
- 42.Willich SN, Lowel H, Lewis M, Hormann A, Arntz HR, Keil U. Weekly variation of acute myocardial infarction. Increased Monday risk in the working population. Circulation. 1994;90:87–93. doi: 10.1161/01.cir.90.1.87. [DOI] [PubMed] [Google Scholar]
- 43.National Directory: State Certificate of Need Programs, Health Planning Agencies . American Health Planning Association. Fall Church, VA: 2008. [Google Scholar]
- 44.AHA Annual Survey Database (Fiscal Year 2001) American Hospital Association. Chicago, IL: 2002. [Google Scholar]
- 45.AHA Annual Survey Database (Fiscal Year 2006) American Hospital Association. Chicago, IL: 2007. [Google Scholar]
- 46.Buckley JW, Bates ER, Nallamothu BK. Primary percutaneous coronary intervention expansion to hospitals without on-site cardiac surgery in Michigan: a geographic information systems analysis. American Heart Journal. 2008;155:668–72. doi: 10.1016/j.ahj.2007.10.051. [DOI] [PubMed] [Google Scholar]