Abstract
This study examined the relationship between changes in coping and posttraumatic stress disorder (PTSD) symptomatology among recent female rape and physical assault victims as a function of assault type and perpetrator status. Participants were assessed within 1 month after trauma and again at 3 months after trauma. Results indicate that changes in coping strategies over time are associated with the severity of the PTSD symptoms. Assault type was not a significant factor in the association between changes in coping and PTSD, but perpetrator status was. Victims with known perpetrators, who coped more by social withdrawal, had more severe PTSD symptoms over time. The importance of examining the dynamic nature of coping in the development of PTSD is discussed.
Posttraumatic stress disorder (PTSD) frequently occurs in female rape and physical assault victims. Within one week of these traumas, female sexual assault victims (up to 94%) and physical assault victims (71%) have been found to meet the Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised (DSM-III-R; American Psychiatric Association, 1987) symptom criteria for PTSD (omitting Criterion E, which requires >1 month duration of symptoms; Riggs, Rothbaum, & Foa, 1995; Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992). By 3 months after the assault, these numbers diminish to 47% of sexual assault victims and 21% of physical assault victims, indicating that although PTSD exists at high rates for these types of victims, a large percentage of people naturally recover from traumatic events. This research indicates that the presence of a trauma alone is not sufficient for a person to develop PTSD; instead, it is likely that a range of factors contribute to the failure of recovery. Factors such as personality characteristics of the victim (Schnurr, Friedman, & Rosenberg, 1993), the relationship between the perpetrator and the victim (Leahy, Pretty, & Tenenbaum, 2004; Lucenko, Gold, & Cott, 2000), peritraumatic reactions such as dissociation and other responses (Birmes et al., 2003; Kaysen, Morris, Rizvi, & Resick, 2005), as well as different approaches to managing the effects of trauma (for a review, see Resick, 2001) have all been shown to play a role in the maintenance of PTSD symptomatology.
How one copes and responds after a trauma may provide valuable information on risk and resiliency factors in PTSD, although research in this area is surprisingly limited. Coping strategies utilized to deal with the effects of a trauma can be broadly categorized as cognitive or behavioral (Waldrop & Resick, 2004), as well as effective or ineffective in reducing distress (Resick, 2001). Cognitive strategies involve attempts to change the way one thinks about a situation, such as cognitive restructuring, wishful thinking, self-blame, and self-criticism, as a means of reducing distress about the situation or an attempt to make meaning of it. Behavioral strategies are observable actions one takes as an attempt to reduce the impact of stress, including withdrawing from others, or conversely seeking social support, and problem-avoidance.
Theories of PTSD (e.g., Ehlers & Clark, 2000; Foa & Kozak, 1986; Mowrer, 1960), have focused on the importance of escape and avoidance in preventing natural recovery and maintaining the symptoms of PTSD. For example, Foa and Kozak (1986) have proposed that, following traumatic events, people develop a fear network in which traumatic reminders and strong fear responses occur frequently. To decrease the intensity and frequency of these intrusive reminders, the person copes through avoidance of these stimuli, which ultimately leads to failure to process the fear responses effectively and the maintenance of PTSD symptoms. Social cognitive theorists, such as Benight and Bandura (2004), suggest that resource loss after experiencing trauma (Hobfoll, 1991) leads to a loss of perceived self-efficacy and avoidant coping. Resick (2001, 2004) has also described how coping through avoidance maintains distress because the affected person does not receive corrective information from others regarding any distorted beliefs about the event and does not have an opportunity to process emotions emanating from the event.
Consistent with these theories, research that has examined the relationship between coping strategies and PTSD has consistently found that avoidant coping strategies are associated with increased PTSD symptomatology after various traumatic events. Such events include motor vehicle accidents (Bryant & Harvey, 1995), child sexual abuse (Coffey, Leitenberg, Henning, Turner, & Bennett, 1996), adult sexual assault (Gibson & Leitenberg, 2001), and adult physical assault (Valentiner, Foa, Riggs, & Gershuny, 1996). Similarly, a more recent study showed that avoidant coping was related to increased PTSD symptoms in a sample of female domestic violence survivors (Street, Gibson, & Holohan, 2005).
Two studies have demonstrated that coping differs as a function of assault type. Valentiner et al. (1996) found that rape victims had higher levels of both wishful thinking and PTSD severity than physical assault victims at 3 months after the assault. A study conducted with recent female sexual and physical assault victims showed that levels of dissociation after trauma, which has been conceptualized as a form of avoidant coping (see Wagner & Linehan, 1998), declined over the course of the 3-month study (Dancu, Riggs, Hearst-Ikeda, Shoyer, & Foa, 1996). However, dissociation scores were only significantly related to PTSD diagnosis and symptom severity in the physical assault victims. These results indicate some potential differences in coping strategies between sexual and physical assault victims.
Coping strategies have also been investigated by perpetrator status in one study. In a sample of female sexual assault victims, sexual distress following the trauma was more common for women whose perpetrator was an intimate, whereas fear and anxiety were more common characteristics when the perpetrator was unknown to the victim (Ullman & Siegel, 1993). Additionally, women assaulted by a stranger were more likely to talk about the assault with others than women who had known the perpetrator. Aside from these two specific differences, there were few differences in psychological sequelae and social support seeking by victim–perpetrator relationship.
Despite this growing body of research on coping strategies and PTSD, there are a number of problems with existing studies that limit their generalizability and applicability. Waldrop and Resick (2004) in their review of coping literature determined that cross-sectional methodology was the central limitation of past coping research. To our knowledge, all of the existing research on coping strategies after trauma have employed cross-sectional analyses or have asked participants to provide retrospective data covering large periods. Therefore, it is impossible to draw any conclusions about the causal influences of coping strategies on the development of (or resilience to) PTSD.
Cross-sectional analyses also fail to take into account the dynamic nature of these processes and PTSD symptomatology. Rather than conceptualizing coping and response strategies as static entities, it seems more likely that they change over time as the person adapts (or fails to adapt) after the trauma. In the current study, this oversight is addressed by examining changes in coping strategies among recent female rape and physical assault victims over a 3-month period, and their relationship to changes in PTSD symptomatology. Changes in coping and PTSD symptoms were also examined as both a function of assault type (sexual vs. physical assault) and perpetrator status (known vs. stranger) to better understand the role that these variables play in posttrauma psychological distress. We hypothesize that increases in certain adaptive strategies such as problem solving, cognitive restructuring, social support, and expressed emotion will be linked to greater improvements in PTSD symptomatology, whereas increases in maladaptive forms of coping such as problem avoidance, wishful thinking, social withdrawal, and self-criticism will be linked to less improvement over time.
Method
Participants
All participants were part of a larger project designed to investigate the recovery process following a sexual or physical assault. One hundred twenty-two women who were assessed both at Time 1 (<1 month after the assault; M = 16.3 days, SD = 8.0 days) and at Time 2 (3 months after the assault) were included in the current study. The sample included 74 rape victims and 48 physical assault victims. Rape was defined as any crime involving vaginal, oral, or anal penetration. First-degree physical assault was defined according to Missouri statutes as a physical assault where the participant experienced an injury or felt that the perpetrator was trying to kill or injure them.
The mean age of the sample was 31.6 years (SD = 8.50; range = 18–55 years). Average education level was 12.4 years (SD = 2.50; range = 2–20). The racial composition of the sample was 69.5% African American, 27.5% White, and 3.3% of other ethnicity. At the time of the first assessment, 55.1% were single, 16.9% were married or living with someone, and the remainder were separated, divorced or widowed. Sixty-six percent of the sample had a personal income of less than $10,000 in the past year.
Measures
A larger battery of interviews and self-report questionnaires were given to participants to assess various aspects of the trauma as well as current psychological functioning. The subset of measures used in the current investigation listed below, except for the Trauma Interview, were administered at both Time 1 and Time 2.
Coping Strategies Inventory
The Coping Strategies Inventory (CSI; Tobin, Holroyd, & Reynolds, 1984) is a 72-item self-report questionnaire that assesses methods of coping via thoughts and behaviors in response to a specific stressor. Responses are rated on a 5-point Likert scale (1 = none to 5 = very much). There are eight primary scales of the CSI, each composed of nine items: Problem Solving, Cognitive Restructuring, Social Support, Expressed Emotion, Problem Avoidance, Wishful Thinking, Social Withdrawal, and Self-Criticism. The Problem-Solving subscale includes items pertaining to behavioral and cognitive strategies used to eliminate the source of stress by changing the stressful situation. The Cognitive-Restructuring subscale includes cognitive strategies that alter the meaning of stressful transactions to make them less threatening and to view them from a new, more positive, perspective. The Social Support subscale consists of items that refer to seeking emotional support from others. The Expressed Emotion subscale examines releasing and expressing emotions. The Problem Avoidance subscale consists of items involving the denial of problems and the avoidance of thoughts or actions surrounding the stressful event. The Wishful Thinking subscale consists of cognitive strategies that reflect the inability or reluctance to reframe or alter a situation symbolically, as well as hoping and wishing things could be better. The Social Withdrawal subscale involves withdrawing from family and friends, most specifically in terms of one’s emotional reaction to the stressor. The self-criticism subscale includes items that reflect blaming oneself for the situation and criticizing oneself. Scores for each subscale range from 5 to 45, where higher scores indicate greater endorsement of the coping strategy. Previous research has documented reliability coefficients for the eight scales; they range from .71 to .94 (M = .83; Tobin, Holroyd, Reynolds, & Wigal, 1989). For the current study, reliability coefficients ranged from .80 to .94 (M = .82), with the exception of the Problem Avoidance subscale which had a coefficient of .61.
Clinician-Administered PTSD Scale
The Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995) is a widely used interview-based diagnostic instrument for PTSD. Additionally, the CAPS yields a total severity score, which is computed by summing the frequency and intensity scores, rated on a scale of 0 (low) to 4 (high) for both frequency and intensity, for all 17 items. The CAPS has been shown to have excellent psychometric properties (see Weathers, Keane, & Davidson, 2001 for a review). For the current study, reliability coefficients of the CAPS frequency and intensity scores were .91 at Time 1 and .94 at Time 2.
Trauma Interview
The Trauma Interview (Resick, 1982; Resick, Jordan, Girelli, Hutter, & Marhoefer-Dvorack, 1988) is a structured interview used to gather characteristics about the participants, as well as information about their traumatic experiences. Relevant to the current study, the relationship between the victim and the perpetrator was assessed. Participants were asked about their relationship with the perpetrator through 12 yes or no questions, which were used to create two categories of perpetrator status: known or stranger. The stranger variable consisted of those who endorsed the perpetrator as a complete stranger or someone they had not talked to but had seen before. The known variable consisted of those who endorsed the perpetrator as someone they talked to, dated, a coworker, a friend, a boyfriend, an ex-boyfriend, a cohabitant, a fiancé, a spouse, or another relationship.
Procedure
Postcards describing the study with the researchers’ phone number and detachable return postcards were sent by agency personnel to women who reported being raped or assaulted to police departments, hospitals, or victim-assistance agencies. The total possible pool of participants and participant rates is unknown because the initial contact was through mailings by staff members of agencies such as police departments and victim service agencies and researchers were not given access to reporting lists, possible duplications across agencies, or whether the mailings were actually received by the intended recipients. After expressing interest in the study through a returned postcard or telephone call, potential participants were contacted by phone or mail and were screened and scheduled for the first assessment within 1 month of the crime. Individuals were ineligible for participation if they were unable to come in for an assessment within the 4-week window subsequent to their crime or if they were illiterate, demonstrated psychosis, or were intoxicated at the time of assessment (for consent and validity purposes). No treatment was offered as part of the study, but referral lists were distributed at each assessment session. Interviewers were trained master’s-level clinicians who received ongoing supervision.
Data Analysis
Cross-sectional correlations were initially conducted to examine the association between coping strategies and PTSD symptoms at each assessment point. The second set of analyses focused on the associations between changes in coping strategies and PTSD symptomatology over time. Toward this end, standardized residual change scores were computed for PTSD severity, as measured by the CAPS, and all of the CSI subscales. The residualized change scores were computed by regressing CAPS severity scores and CSI subscales within 1 month after the assault onto their within-variable measure at 3 months after the assault, resulting in residualized CAPS and CSI scores at the 3-month assessment. Residualized change scores have a statistical advantage over simple change scores in that they provide a smaller ratio of measurement error to true scores (see Cronbach & Furby, 1970). Correlations between the residualized CSI subscale scores and the CAPS scores were then computed. Finally, to investigate the role of type of assault (physical vs. sexual) and perpetrator status (known vs. stranger) in the association between changes in coping and PTSD symptomatology, a series of hierarchical regression equations were conducted. Residualized change in CAPS score was the dependent variable for all tests. The regression models included three sequential steps. In the first step, residualized change in a CSI subscale was entered into the equation. The main effect of either type of assault or perpetrator status was entered at the second step. The interaction term between assault type or perpetrator status and residualized change in a given coping strategy was entered as the third and final step. Tabachnik and Fidell (1996) conservatively estimate that 10 cases per predictor variable be used in linear regression analyses, therefore we had ample sample size to find the effects of any predictor variable.
RESULTS
Cross-Sectional Results
Within one month after the assault, 81% of sexual assault victims and 63% of physical assault victims met DSM-III-R symptom criteria for PTSD, minus Criterion E, which requires greater than 1-month duration of symptoms. By 3 months after the assault, these numbers decreased to 53% of sexual assault and 31% of physical assault meeting full DSM-III-R criteria for PTSD. Mean CAPS severity score within 1 month after trauma was 66.73 (SD = 26.15) and at 3 months was 42.95 (SD = 28.23) for the overall sample.
Table 1 provides Pearson correlations between the CSI subscales and CAPS scores at Time 1 and 2. At Time 1, there were significant relationships in the expected direction between the CAPS and the following subscales of the CSI: Cognitive Restructuring, Social Support (both associated with lower CAPS scores), Wishful Thinking, Self-Criticism, and Social Withdrawal (associated with higher CAPS scores). Similarly, at Time 2, there were significant relationships in the expected direction between CAPS severity scores and the following subscales: Social Support, Problem Avoidance, Wishful Thinking, Self-Criticism, and Social Withdrawal. The CSI subscales of Problem Solving and Expressed Emotion were not significantly correlated with PTSD severity at either time point.
Table 1.
Cross-Sectional Correlations Between Coping and PTSD Symptoms at Time 1 and Time 2
| CAPS T1 | CAPS T2 | |
|---|---|---|
| CSI Problem Solving (T1) | −.15 | |
| Problem Solving (T2) | −.08 | |
| CSI- Cognitive Restructuring (T1) | −.20* | |
| Cognitive Restructuring (T2) | −.18 | |
| CSI- Expressed Emotion (T1) | −.15 | |
| Expressed Emotion (T2) | −.14 | |
| CSI- Social Support (T1) | −.23* | |
| Social Support (T2) | −.23* | |
| CSI- Problem Avoidance (T1) | .09 | |
| Problem Avoidance (T2) | .18* | |
| CSI- Wishful Thinking (T1) | .24** | |
| Wishful Thinking (T2) | .39*** | |
| CSI- Self-Criticism (T1) | .46*** | |
| Self-Criticism (T2) | .27** | |
| CSI- Social Withdrawal (T1) | .51*** | |
| Social Withdrawal (T2) | .57*** |
Note. CAPS = Clinician-Administered Posttraumatic Stress Disorder Scale-Total Severity Score, CSI = Coping Strategies Inventory.
p < .05.
p < .01.
p < .001.
Relationships Between Changes in Coping and Posttraumatic Stress Disorder
Simple correlations between residualized CAPS scores and the eight residualized CSI subscale scores are reported in Table 2. There were significant correlations between residualized CAPS and the following CSI subscales: Cognitive Restructuring, Expressed Emotion, Social Support, Wishful Thinking, and Social Withdrawal. Specifically, as the use of cognitive restructuring, expressed emotion, and social support coping strategies increased over time, PTSD symptoms decreased. Conversely, when wishful thinking and social withdrawal coping strategies increased over time, PTSD symptoms also increased.
Table 2.
Correlations Between Residualized CAPS Score and the Eight Residualized CSI Subscale Scores
| CSI Subscales | Residualized CAPS |
|---|---|
| Residualized Problem Solving | −.14 |
| Residualized Cognitive Restructuring | −.24** |
| Residualized Expressed Emotion | −.19* |
| Residualized Social Support | −.21* |
| Residualized Problem Avoidance | .04 |
| Residualized Wishful Thinking | .20* |
| Residualized Self-criticism | .13 |
| Residualized Social Withdrawal | .34** |
p < .05.
p < .01.
Changes in Posttraumatic Stress Disorder and Coping by Assault Type
Results from the hierarchical regressions are presented in Tables 3 and 4. In the first series of regression equations investigating the role of assault type (physical vs. sexual) in the associations between changes in coping and PTSD symptoms, there were no significant relationships between the type of assault and changes in PTSD symptomatology, after controlling for changes in coping (see Step 2). Similarly, in the final step, there were no interaction effects of assault type by changes in coping strategies, indicating that there were not differential relationships between changes in coping and PTSD symptoms based on whether the victims were sexually assaulted or physically assaulted.
Table 3.
Hierarchial Regression Analyses of Residualized CAPS Scores by CSI Scores and Assault Type
| Outcome Step | β | R2/ΔR2 | Model F (df) |
|---|---|---|---|
| CSI-Problem Solving | 0.72 (3, 109) | ||
| 1. Δ in problem solving | −.17 | .02 | |
| 2. assault type | .01 | .00 | |
| 3. Δ in problem solving by assault type | .05 | .00 | |
| CSI-Cognitive Restructuring | 2.56 (3, 111) | ||
| 1. Δ in cognitive restructuring | −.16 | .06 | |
| 2. assault type | .03 | .00 | |
| 3. Δ in cognitive restructuring by assault type | −.11 | .01 | |
| CSI-Emotional Expression | 1.90 (3, 112) | ||
| 1. Δ in emotional expression | −.30* | .04 | |
| 2. assault type | .01 | .00 | |
| 3. Δ in emotional expression by assault type | .15 | .01 | |
| CSI-Social Support | 1.71 (3, 111) | ||
| 1. Δ in social support | −.21 | .04 | |
| 2. assault type | −.01 | .00 | |
| 3. Δ in social support by assault type | .00 | .00 | |
| CSI-Problem Avoidance | .57 (3, 110) | ||
| 1. Δ in problem avoidance | −.02 | .00 | |
| 2. assault type | .02 | .00 | |
| 3. Δ in problem avoidance by assault type | .13 | .01 | |
| CSI-Wishful Thinking | 1.63 (3, 111) | ||
| 1. Δ in wishful thinking | .23 | .04 | |
| 2. assault type | .02 | .00 | |
| 3. Δ in wishful thinking by assault type | −.04 | .001 | |
| CSI-Self-Criticism | 1.04 (3, 112) | ||
| 1. Δ in self-criticism | .24 | .02 | |
| 2. assault type | .10 | .01 | |
| 3. Δ in self-criticism by assault type | −.08 | .01 | |
| CSI-Social Withdrawal | 6.10 (3, 113)** | ||
| 1. Δ in social withdrawal | .50*** | .12 | |
| 2. assault type | .11 | .01 | |
| 3. Δ in social withdrawal by assault type | −.18 | .01 |
Note. βs are for the final model.
p < .05.
p < .01.
p < .001.
Table 4.
Hierarchial Regression Analyses of Residualized CAPS Scores by CSI Scores and Perpetrator Status
| Outcome Step | β | R2/ΔR2 | Model F (df) |
|---|---|---|---|
| CSI-Problem Solving | 1.96 (3, 107) | ||
| 1. Δ in problem solving | −.11 | .02 | |
| 2. perpetrator status | −.18 | .03 | |
| 3. Δ in problem solving by perpetrator status | −.02 | .00 | |
| CSI-Cognitive Restructuring | 3.80 (3, 109)* | ||
| 1. Δ in cognitive restructuring | −.28* | .07 | |
| 2. perpetrator status | −.15 | .02 | |
| 3. Δ in cognitive restructuring by perpetrator status | .04 | .00 | |
| CSI-Emotional Expression | 2.50 (3, 110) | ||
| 1. Δ in emotional expression | −.22 | .04 | |
| 2. perpetrator status | −.16 | .03 | |
| 3. Δ in emotional expression by perpetrator status | .06 | .00 | |
| CSI-Social Support | 2.95 (3, 109)* | ||
| 1. Δ in social support | −.21 | .05 | |
| 2. perpetrator status | −.16 | .02 | |
| 3. Δ in social support by perpetrator status | .00 | .00 | |
| CSI-Problem Avoidance | 1.50 (3, 109) | ||
| 1. Δ in problem avoidance | .11 | .00 | |
| 2. perpetrator status | −.18 | .03 | |
| 3. Δ in problem avoidance by perpetrator status | −.11 | .01 | |
| CSI-Wishful Thinking | 3.14 (3, 109)* | ||
| 1. Δ in wishful thinking | .28* | .04 | |
| 2. perpetrator status | −.20* | .04 | |
| 3. Δ in wishful thinking by perpetrator status | −.07 | .00 | |
| CSI-Self-Criticism | 2.46 (3, 110) | ||
| 1. Δ in self-criticism | .25 | .01 | |
| 2. perpetrator status | −.22* | .05 | |
| 3. Δ in self-criticism by perpetrator status | −.12 | .01 | |
| CSI-Social Withdrawal | 8.61 (3, 111)*** | ||
| 1. Δ in social withdrawal | .53*** | .11 | |
| 2. perpetrator status | −.18* | .03 | |
| 3. Δ in social withdrawal by perpetrator status | −.30* | .05 |
Note. βs are for the final model.
p < .05.
p < .01.
p < .001.
Changes in Posttraumatic Stress Disorder and Coping by Perpetrator Status
A chi-square test was computed to determine if assault type was associated with perpetrator status. The relationship of perpetrator differed significantly by assault type, χ2(1, N = 119) = 5.14, p< .05, with physical assault victims more likely to have known the perpetrator (58%) compared to rape victims (37%). Additionally, a linear regression was computed taking into account the interaction of perpetrator status and assault type to ensure changes in PTSD symptoms over time were related to perpetrator status and not assault type. The relationship of perpetrator to changes in PTSD was significant whereas the relationship between both assault type and the interaction of perpetrator status and assault type were not significant. A series of hierarchical regression analyses were again computed with perpetrator status included at the second step and the interaction between perpetrator status and changes in coping strategy at the third step. In contrast to the results by assault type, after controlling for residualized changes in some of the coping strategies (i.e., wishful thinking, self-criticism, and social withdrawal), perpetrator status was significantly associated with residualized CAPS scores. In these cases, PTSD symptoms generally declined, but women who were assaulted by strangers had smaller decreases in their symptoms over time than women assaulted by someone known to them.
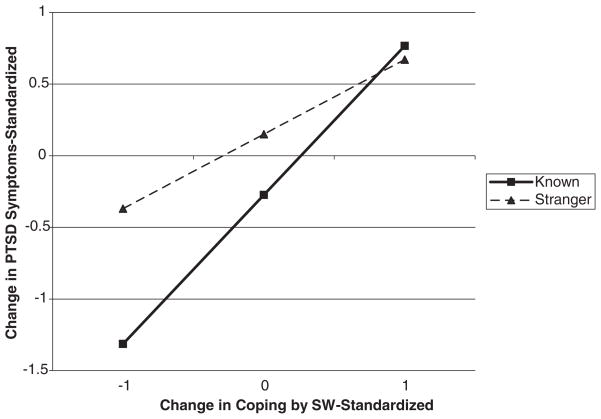
In the final step in which the interaction of coping changes and perpetrator status was included, there was a significant interaction between changes in social withdrawal and perpetrator type in predicting changes in PTSD symptoms. As shown in Figure 1, those who were assaulted by someone known to them and who also tended not to socially withdraw, had more reductions in their PTSD symptoms over time than did those who were assaulted by a stranger. As coping by social withdrawal increased, differences by type of perpetrator were less notable.
Figure 1.
Changes in Posttraumatic Stress Disorder Symptoms and Social Withdrawal Coping By Perpetrator Type. Final model, F (3, 114) = 8.61, p < .001. βCSI-Social Withdrawal = .53, p < .001; βperpetrator type = −18, p < .05; βinteraction = −.30, p < .01. PTSD = posttraumatic stress disorder; SW = social withdrawal.
DISCUSSION
Our results highlight the previously neglected dynamic nature of coping strategies following a trauma. Although prior research has shown differences in coping and post-trauma distress by type of assault, our results highlight that changes in the use of various coping strategies are important to understanding the course of developing PTSD. For example, expressing emotion was not associated with the level of PTSD symptoms at either time point in the cross-sectional examination, but expressing more emotions over time was associated with decreases in symptoms. An additional significant finding was that the victims’ use of social withdrawal coping tendencies had a differentially strong relationship with PTSD symptoms over time for those assaulted by someone that they knew. Furthermore, our finding of the percentage of sexual and physical assault victims meeting DSM-III-R symptom criteria for PTSD within weeks after trauma and 3-months after trauma is consistent with incidence rates documented in previous research (Riggs et al., 1995; Rothbaum et al., 1992).
In general, changes in specific methods of coping over time were significantly related to changes in PTSD symptomatology. As the use of cognitive restructuring, expressed emotion, and social support increased over time, the level of PTSD symptomatology decreased. In contrast, the increased use of wishful thinking and social withdrawal over time was related to fewer improvements in PTSD symptomatology. These results provide different information than that gleaned from cross-sectional correlations alone. If cross-sectional analyses at either assessment point were the sole source of information, then some significant relationships between coping strategies and PTSD would have been overlooked. Moreover, the cross-sectional analyses indicated that self-criticism was significantly correlated with PTSD severity at both time points, but changes in self-criticism were not significantly associated with changes in PTSD symptoms. This pattern of findings is likely the result of minimal changes in the use of self-criticism over time in this non-treatment-oriented sample. These analyses simultaneously highlight the need to look at posttrauma reactions as a dynamic process, and suggest that some coping strategies may be relatively more static over time, but detrimental nonetheless.
These results are also consistent with research by Schnurr, Lunney, and Sengupta (2004) showing differences in the factors that contribute to a person developing PTSD and the factors that maintain PTSD. Results from that study indicated that initial PTSD status is related to factors occurring before, during, and after a traumatic event, whereas failure to recover (i.e., maintenance) is related to factors that occur to the individual during and after the event. It is possible that with regard to the maintenance of PTSD, it is more important to examine the dynamic nature of the factors, occurring after the trauma, such as coping methods, when examining failure to recover from PTSD, rather than static descriptors at a follow-up assessment.
In contrast to previous work that has suggested that type of assault (i.e., sexual versus physical assault) plays an important role in coping responses and PTSD severity (e.g., Dancu et al., 1996; Valentiner et al., 1996), results from the current study indicated that assault type was not related to changes in PTSD symptomatology. Instead, the results suggest that the victim’s relationship to the perpetrator plays a more important role. The main effect of perpetrator status indicates that PTSD symptoms were less likely to improve over time when the perpetrator was a stranger. This is consistent with other research (Thornhill & Thornhill, 1990) suggesting that assault by a stranger has greater negative consequences on the mental health of the victim than assault by a known assailant.
The significant interaction between changes in social withdrawal and perpetrator is an important finding that has not been reported in past research. Across all individuals, social withdrawal was associated with increased PTSD symptoms. However, this effect was significantly pronounced for those assaulted by someone known to them. This suggests that for individuals assaulted by someone known to them, a large contributor to whether they will recover after trauma is their level of social interaction in the weeks following the assault. This has implications for the focus of early intervention work following an assault. One of the most important aspects of early interventions may be a focus on counteracting social withdrawal as a coping mechanism, and the encouragement of active engagement in social situations as a means of reducing the likelihood that PTSD will develop. This is consistent with recent research by Wagner and colleagues (Wagner, Zatzick, Ghesquiere, & Jurkovich, 2006) that suggests that behavioral activation is effective for reducing distress immediately following a traumatic incident. It is also possible that reduced social interaction could be indicative of fear of disclosure to others about the assault and/or shame or guilt about what happened. If this is the case, early intervention work may want to focus on the importance of discussing information about the trauma with a trusted loved one. Future research to identify the underlying causes of social withdrawal should take this into consideration.
The current study has a number of limitations that are important to address. The study was restricted to women, which may limit the generalizability of the results to male victims. Additionally, the sample is relatively small and not nationally representative, which may also influence its generalizability. However, the sample is also unique in terms of its longitudinal design and timing of the first assessment within 4 weeks after the crime. This methodology represents an improvement over other studies that assessed postassault coping retrospectively months or even years after the event. It also important to note that this study did not take into account other factors such as prior traumatization, which may play a role in changes in PTSD symptoms over time (Nishith, Mechanic, & Resick, 2000). Finally, although this study purposely examined changes over time in coping as it relates to changes in PTSD symptomatology, it is not possible to infer causality. That is, it is unclear whether increases in social withdrawal, for example, lead to increases in PTSD or whether increases in symptoms of PTSD causes one to withdraw more from social situations. Future research is necessary to examine the causal links of this process.
Future research on coping styles following a trauma should continue to take into account the dynamic nature of posttraumatic responding. Moreover, studies that have more long-term follow-up periods are essential to determine whether these findings remain relevant over time. In terms of the development of PTSD more broadly, it would also be important to determine whether the same types of coping mechanisms are related to PTSD for individuals who are victims of other types of trauma. Given the high degree of variability in how individuals respond after trauma and the implications for preventing the onset of PTSD, this is an area that warrants serious attention from researchers.
Acknowledgments
This work was supported by a grant from the National Institute of Mental Health (R01-MH6992), awarded to Patricia A. Resick. Portions of this study’s results were presented at the Association for Advancement of Behavior Therapy 39th Annual Meeting held in Washington, DC in November 2005.
Contributor Information
Cassidy A. Gutner, National Center for Posttraumatic Stress Disorder, Women’s Health Sciences Division, VA Boston Healthcare System, Boston, MA
Shireen L. Rizvi, National Center for Posttraumatic Stress Disorder, Women’s Health Sciences Division, VA Boston Healthcare System, and the Department of Psychiatry, Boston University School of Medicine, Boston, MA
Candice M. Monson, National Center for Posttraumatic Stress Disorder, Women’s Health Sciences Division, VA Boston Healthcare System, and the Department of Psychiatry, Boston University School of Medicine, Boston, MA
Patricia A. Resick, National Center for Posttraumatic Stress Disorder, Women’s Health Sciences Division, VA Boston Healthcare System, and the Department of Psychiatry, Boston University School of Medicine, Boston, MA
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3. Washington, DC: Author; 1987. rev. [Google Scholar]
- Benight CC, Bandura A. Social cognitive theory of posttraumatic recovery: The role of perceived self-efficacy. Behaviour Research and Therapy. 2004;42:1129–1148. doi: 10.1016/j.brat.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Birmes P, Brunet A, Carreras D, Ducasse JL, Charlet JP, Lauque D, et al. The predictive power of peritraumatic dissociation and acute stress symptoms for posttraumatic stress symptoms: A three-month prospective study. American Journal of Psychiatry. 2003;160:1337–1339. doi: 10.1176/appi.ajp.160.7.1337. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of the Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Harvey AG. Processing threatening information in posttraumatic stress disorder. Journal of Abnormal Psychology. 1995;104:537–541. doi: 10.1037//0021-843x.104.3.537. [DOI] [PubMed] [Google Scholar]
- Coffey P, Leitenberg H, Henning K, Turner T, Bennett RT. The relation between methods of coping during adulthood with a history of childhood sexual abuse and current psychological adjustment. Journal of Consulting and Clinical Psychology. 1996;64:1090–1093. doi: 10.1037//0022-006x.64.5.1090. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ, Furby L. How we should measure “change”: Or should we? Psychological Bulletin. 1970;74:68–80. [Google Scholar]
- Dancu CV, Riggs DS, Hearst-Ikeda DE, Shoyer BG, Foa EB. Dissociative experiences and posttraumatic stress disorder among female victims of criminal assault and rape. Journal of Traumatic Stress. 1996;9:253–267. doi: 10.1007/BF02110659. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of post-traumatic stress disorder. Behaviour Research and Therapy. 2000;38:319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. [PubMed] [Google Scholar]
- Gibson LE, Leitenberg H. The impact of child sexual abuse and stigma on methods of coping with sexual assault among undergraduate women. Child Abuse & Neglect. 2001;25:1343–1361. doi: 10.1016/s0145-2134(01)00279-4. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE. Traumatic stress: A theory based on rapid loss of resources. Anxiety Research. 1991;4:187–197. [Google Scholar]
- Kaysen D, Morris M, Rizvi S, Resick PA. Peritraumatic responses and their relationship to perceptions of threat in female crime victims. Violence Against Women. 2005;11:1515–1535. doi: 10.1177/1077801205280931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leahy T, Pretty G, Tenenbaum G. Perpetrator methodology as a predictor of traumatic symptomatology in adult survivors of child sexual abuse. Journal of Interpersonal Violence. 2004;19:521–540. doi: 10.1177/0886260504262963. [DOI] [PubMed] [Google Scholar]
- Lucenko BA, Gold SN, Cott MA. Relationship to perpetrator and posttraumatic symptomatology among sexual abuse survivors. Journal of Family Violence. 2000;15:169–179. [Google Scholar]
- Mowrer OH. Learning theory and the symbolic processes. New York: Wiley; 1960. [Google Scholar]
- Nishith P, Mechanic MB, Resick PA. Prior interpersonal trauma: The contribution to current PTSD symptoms in female rape victims. Journal of Abnormal Psychology. 2000;109:20–25. [PMC free article] [PubMed] [Google Scholar]
- Resick PA. Psychological reactions of victims of rape and robbery. 1982. Unpublished manuscript. [Google Scholar]
- Resick PA. Stress & trauma. Hove, UK: Psychological Press, Ltd; 2001. [Google Scholar]
- Resick PA. Beyond cognitive processing: A reconceptualization of posttrauma pathology. Paper presented at the 38th Annual Meeting of the Association for Advancement of Behavioral Therapy; New Orleans, LA. 2004. Nov, [Google Scholar]
- Resick PA, Jordan CG, Girelli SA, Hutter CK, Marhoefer-Dvorack S. A comparative outcome study of behavioral group therapy for sexual assault victims. Behavior Therapy. 1988;19:385–401. [Google Scholar]
- Riggs DS, Rothbaum BO, Foa EB. A prospective examination of symptoms of posttraumatic stress disorder in victims of nonsexual assault. Journal of Interpersonal Violence. 1995;10:201–214. [Google Scholar]
- Rothbaum BO, Foa EB, Riggs DS, Murdock TB, Walsh W. A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress. 1992;5:455–475. [Google Scholar]
- Schnurr PP, Friedman MJ, Rosenberg SD. Premilitary MMPI scores as predictors of combat-related PTSD symptoms. American Journal of Psychiatry. 1993;150:479–483. doi: 10.1176/ajp.150.3.479. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Lunney CA, Sengupta A. Risk factors for the development versus maintenance of posttraumatic stress disorder. Journal of Traumatic Stress. 2004;17:85–95. doi: 10.1023/B:JOTS.0000022614.21794.f4. [DOI] [PubMed] [Google Scholar]
- Street AE, Gibson LE, Holohan DR. Impact of childhood traumatic events, trauma-related guilt, and avoidant coping strategies on PTSD symptoms in female survivors of domestic violence. Journal of Traumatic Stress. 2005;18:245–252. doi: 10.1002/jts.20026. [DOI] [PubMed] [Google Scholar]
- Tabachnik BG, Fidell LS. Using multivariate statistics. 3. New York: Harper Collins; 1996. [Google Scholar]
- Thornhill NW, Thornhill R. An evolutionary analysis of psychological pain following rape: II. The effects of stranger, friend, and family-member offenders. Ethology and Sociobiology. 1990;11:177–193. [Google Scholar]
- Tobin DL, Holroyd KA, Reynolds RVC. User’s manual for the Coping Strategies Inventory. Athens, OH: Ohio University, Department of Psychology; 1984. [Google Scholar]
- Tobin DL, Holroyd KA, Reynolds RVC, Wigal JK. The hierarchical factor structure of the Coping Strategies Inventory. Cognitive Therapy and Research. 1989;13:343–361. [Google Scholar]
- Ullman SE, Siegel JM. Victim-offender relationship and sexual assault. Violence and Victims. 1993;8:121–133. [PubMed] [Google Scholar]
- Valentiner DP, Foa EB, Riggs DS, Gershuny BS. Coping strategies and posttraumatic stress disorder in female victims of sexual and nonsexual assault. Journal of Abnormal Psychology. 1996;105:455–458. doi: 10.1037//0021-843x.105.3.455. [DOI] [PubMed] [Google Scholar]
- Wagner AW, Linehan MM. Dissociative behavior. In: Follette VM, Ruzek JI, Abueg FR, editors. Cognitive–behavioral therapies for trauma. New York: Guilford Press; 1998. pp. 191–225. [Google Scholar]
- Wagner AW, Zatzick DF, Ghesquiere A, Jurkovich GJ. Behavioral activation as an early intervention for post-traumatic stress disorder and depression among physically injured trauma survivors. Cognitive and Behavioral Practice in press. [Google Scholar]
- Waldrop AE, Resick PA. Coping among adult female victims of domestic violence. Journal of Family Violence. 2004;19:291–202. [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]