Abstract
Purpose
To characterize differences in child abuse management resources between urban and rural emergency departments (EDs).
Methods
We surveyed ED directors and nurse managers at hospitals in Oregon to gain information about available abuse-related resources. Chi-square analysis was used to test differences between urban and rural EDs. Multivariate analysis was performed to examine the association between a variety of hospital characteristics, in addition to rural location, and presence of child abuse resources.
Findings
Fifty-five Oregon hospitals were surveyed. A smaller proportion of rural EDs had written abuse policies (62% vs 95%, P = .006) or on-site child abuse advocates (35% vs 71%, P = .009). Thirty-two percent of rural EDs had none of the examined abuse resources (vs 0% of urban EDs, P = .01). Of hospital characteristics studied in the multivariate model, only rural location was associated with decreased availability of child abuse resources (OR 0.19 [95% CI, 0.05 – 0.70]).
Conclusions
Rural EDs have fewer resources than urban EDs for the management of child abuse. Other studied hospital characteristics were not associated with availability of abuse resources. Further work is needed to identify barriers to resource utilization and to create resources that can be made accessible to all ED settings.
Keywords: access to care, child abuse, emergency medicine, health disparities, health services research
INTRODUCTION
Child abuse is prevalent across both rural and urban settings.1 While all emergency departments (EDs) should be fully prepared to recognize and manage child abuse, hospitals may have widely divergent abilities to rise to the challenge of addressing abuse. Although there is little published information characterizing the needs of rural EDs, they likely have fewer resources for managing abuse and less access to community abuse assessment centers for consultation and follow-up than do many urban hospitals.
The Joint Commission (formerly the Joint Commission on the Accreditation of Healthcare Organizations, or JCAHO) has defined basic standards for policies and procedures to optimize the identification and management of child abuse within EDs and hospital-based ambulatory care centers.2 Updated in 2004, the standards include maintenance of specific criteria for identifying victims, education of staff about abuse management, and appropriate assessment and referrals. However, these recommendations are uniform for all hospitals and do not acknowledge potential resource differences between rural and urban hospitals.
The objective of this study was to characterize differences between urban and rural hospitals with regard to the availability of resources for the management of child abuse in Oregon. Such information may enrich ongoing efforts to improve resources for the management of abuse in diverse practice settings.
MATERIALS AND METHODS
Study Design
We studied resources at Oregon hospitals using a standardized telephone survey of ED directors and nurse managers. We targeted ED physician directors and nurse managers from all hospitals in Oregon for participation in the survey, as these individuals are generally responsible for the protocols and services in use in the ED. Survey data were merged with hospital-level variables. The Institutional Review Board of Oregon Health & Science University approved this study.
Study Setting
Oregon has an estimated population of 3.8 million people.3 Rural areas in Oregon are defined as geographic areas 10 or more miles from the centroid of a population center of 40,000 or more, while frontier areas are defined as those with fewer than 6 people per square mile.4 Approximately 26% of the Oregon population lives in rural or frontier counties and 54% live in mixed urban and rural counties. Hospitals that service these areas are classified as rural. Of Oregon’s 57 acute care hospitals, 35 are rural.
A trauma system links Oregon’s rural hospitals to higher resource centers. The trauma system categorizes the majority of hospitals, regardless of size or rural setting, by level of trauma center (I to IV). Level I and II centers represent higher capacity trauma centers, whereas Level III and IV hospitals are smaller centers with limited capacity. Among the 57 Oregon hospitals, 44 are trauma centers: 2 Level I centers, 3 Level II centers, 22 Level III centers, and 17 Level IV centers.
Measurements
To assess availability of child abuse resources, we adapted survey questions from the “Delphi Instrument for Hospital-Based Domestic Violence Programs” developed by the Agency for Healthcare Research and Quality (AHRQ).5 In order to optimize participation, we limited our survey to 3 questions addressing policies and procedures relevant to the ED setting: (1)“Does the hospital or ED provide regular, ongoing training on child abuse for clinical staff working in the ED?” (2)“Is there a written hospital or ED policy for the management of child abuse in the ED?” and (3)”Are on-site victim advocacy services for child abuse provided in the ED (eg, by a social worker, counselor, or trained nurse)?” The survey was pilot tested on ED staff from Oregon Health & Science University unaffiliated with the study and revised based on feedback prior to study inception.
The telephone survey was administered to ED directors and nurse managers over a 1-month period from September to October 2008. A single individual was interviewed at each site. The survey response rate was 96% (55 out of 57 EDs). The director and nurse manager at 1 hospital could not be reached. Another hospital deferred participation.
Hospital-level variables were obtained from the Office for Oregon Health Policy and Research. Variables included urban/rural designation, hospital bed size, a nurse staffing score, and trauma level. The nurse staffing score represents the number of nursing full-time equivalents (FTE) for every 100 hospital admissions. Trauma level was converted to an ordinal variable, with 1 to 4 corresponding to level (eg, 1 for Level I, 2 for Level II) and 5 indicating non-trauma centers.
Data Analysis
We used descriptive statistics (frequencies, means, and proportions) to characterize the availability of child abuse resources among the Oregon hospitals surveyed. Univariate analysis (chi square) was used to identify associations between rural location and availability of abuse resources. Ordinal logistic regression was used to test the association between number of abuse resources (0, 1 or 2–3), rural setting, and other available hospital characteristics. Due to small sample sizes for higher trauma levels, the trauma variable was included in the model as a dichotomous variable, divided into “higher capability” trauma centers (Levels I–III) and “lower capability” trauma centers (Level IV and non-trauma).
Statistical significance was defined as a probability of a type I error of less than 5% (2-tailed). Results are expressed as confidence intervals and P values. Analyses were conducted with Stata, version 10.1 (StataCorp LP, College Station, Texas).
RESULTS
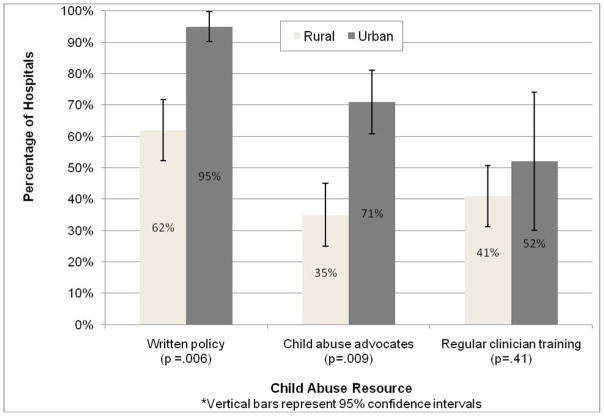
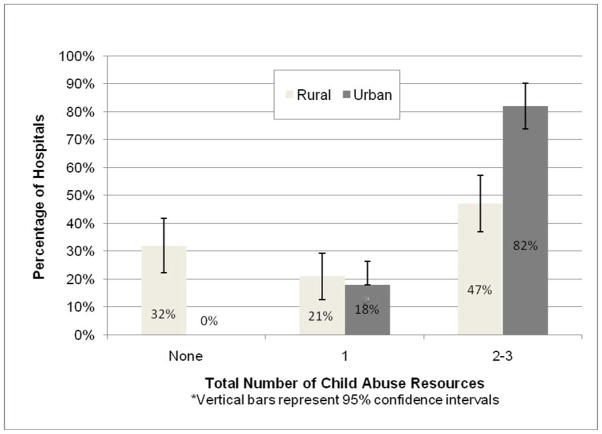
Table 1 compares the characteristics of rural and urban hospitals in our study. Thirty-four (62%) of participating hospitals were classified as rural. Figure 1 shows ED survey results by practice setting. Urban hospitals were more likely than rural settings to have written policies regarding abuse and on-site child abuse advocates. Availability of regular clinician training was greater in urban settings, although this difference was not statistically significant. The breadth of services offered differed significantly between urban and rural hospitals, as well (Figure 2). Thirty-two percent of rural services had none of the 3 resources examined, while all urban hospitals had at least 1 child abuse resource and 82% had more than 1.
Table 1.
| Rural | Urban | P value†† | |
|---|---|---|---|
| Total N (%) | 34 (62%) | 20 (38%) | |
| Mean inpatient bed count (Median) | 90 (39) | 119 (78) | 0.19 |
| Mean nursing FTE per 100 patients (median) | 1.33 (1.15) | 1.56 (1.50) | 0.06 |
| Trauma Level | 0.01 | ||
| Level 1(%) | 0 (0) | 2 (100%) | |
| Level 2 (%) | 1 (33%) | 2 (67%) | |
| Level 3 (%) | 13 (62%) | 8 (38%) | |
| Level 4 (%) | 15 (88%) | 2 (12%) | |
According to the Oregon Office of Rural Health.
Of hospitals that participated in the survey (55 of 57 total Oregon hospitals)
P values from univariate analysis
Figure 1.
Availability of Individual Child Abuse Resources, Rural Versus Urban Hospitals (N=55)
Figure 2.
Total Number of Child Abuse Resources Available, Rural Versus Urban Hospitals (N=55)
The results of the ordinal logistic multivariate analysis are shown in Table 2. Rural EDs had decreased proportional odds of having child abuse resources than urban EDs. High trauma level designation, hospital bed size, and nursing staffing were not associated with availability of abuse resources. We also examined rural hospitals separately, to see if we could distinguish characteristics that might make some rural facilities more likely to have child abuse resources than others. However, among rural hospitals, none of the examined hospital characteristics were associated with availability of abuse resources (high trauma level designation, OR 0.49 [95% CI, 0.12–1.95]; hospital bed size, OR 1.90 per 25 beds [95% CI, 0.86–1.39]; nurse staffing, OR 1.45 per 1-point increase in score [95% CI, 0.24–8.74]).
Table 2.
Results of Ordinal Logistic Regression: Proportional Odds of Child Abuse Resource Availability
| Hospital Characteristic | OR (95% CI) |
|---|---|
| Bed size (per 25 beds) | 1.07 (0.60–0.55) |
| Location | |
| Rural | 0.19 (0.05–0.70) |
| Urban | Reference |
| Nursing FTE score | 1.71 (0.30–9.86) |
| Trauma Level | |
| Higher capability (Level I-III) | 0.76 (0.23–2.45) |
| Lower capability (Level IV or non-trauma) | Reference |
DISCUSSION
Our study quantified differences in the availability of 3 basic child abuse resources in urban and rural EDs. Overall, rural EDs had fewer resources to address abuse. Only 62% of rural EDs reported having a written child abuse policy, compared to 95% of urban hospitals. Only 35% had on-site abuse advocates, compared to 71% of urban hospitals.
Standards do exist for interdisciplinary child abuse programs with comprehensive policies and services for the management of abuse. However, these standards are primarily aimed at pediatric specialty centers, which have the resources and expertise to provide a range of recommended services to address child abuse. Such services may include sexual assault forensic examiners, a trauma service for managing serious sequelae of non-accidental trauma, on-site social work, child psychiatry, and close relationships with child abuse assessment centers. These types of specialty centers are inaccessible to most hospitals and to most of the population.6 Of the 57 hospitals in Oregon, only 2 have pediatric specialty care, and both are located in 1 major metropolitan area.
The expense of maintaining comprehensive child abuse programs, particularly in smaller hospitals, may explain some of the variability between urban and rural EDs. Even children’s hospitals may lack a budgetary allowance for child abuse treatment,7 and the costs of victim care must often be underwritten by hospitals due to limited reimbursement. On-site child abuse advocacy (even if performed by an existing staff member such as a nurse or social worker) may be a service available only to larger, tertiary care hospitals. The same may be true for clinician training, particularly as training programs may need to be intensive and repeated in order to be effective.8, 9 Such considerations make basic and inexpensive resources such as a written abuse policy all the more important. Yet 38% of rural hospitals in our study lacked a policy for guiding the management of child abuse in the ED, suggesting that cost is only 1 barrier to utilization of resources.
There is little data on the impact of these types of resources on outcomes for victims of abuse. Existing recommendations, including Joint Commission standards, are based on expert opinion and provider experience.10, 11 These recommendations have clinical rationale. Studies of physician-identified barriers to child abuse identification and reporting consistently identify deficits in lack of knowledge of child abuse presentations, of reporting procedures, and of the implications of filing a report with child protective services.12–14 However, further research is needed to determine which resources or combination of resources have the greatest impact in improving identification and outcomes for children presenting to hospital settings with abuse. Such research may also allow hospitals to select the most cost-effective means of addressing abuse.
How can we support rural hospitals in the management of abuse? Potential solutions to the resource limitation in rural areas may include emphasizing the use of relatively inexpensive resources such as management guidelines or modifying existing leadership and CME activities to include material on child abuse. Rural sites may consider collaborations with abuse experts who can be available for phone consultations. Technology-based solutions such as videoconferencing have been effective in improving the quality of pediatric sexual assault examinations15 and may become increasingly common as a way to support rural hospitals in the treatment of child abuse.
LIMITATIONS
As with any survey data, our findings may be limited by recall bias. ED administrators may have been more likely to report the presence of resources even if they were not sure or the resources were not present, particularly if they were aware that certain resources are prescribed by the Joint Commission. However, there is no reason this bias should be present differentially between rural and urban hospitals.
Our multivariate model did not identify factors other than rural location to explain the variation in child abuse resources availability, and it did not identify factors that might explain why some rural hospitals were able to provide more child abuse resources than others. However, we examined a limited number of hospital characteristics. It is likely that there are unidentified variables that explain why certain hospitals, and not others, are able to provide a broader range of abuse services.
Finally, because our study was limited to the state of Oregon, the findings may not be generalizable to the entire US. However, the hospitals sampled represented a range of practice settings, with varying bed sizes, trauma capabilities, and urban and rural locations.
CONCLUSIONS
Child abuse management in rural EDs may be particularly challenging due to limited management resources. Centralizing abuse services at tertiary care centers does not obviate the need for individual hospitals to provide support for clinicians to identify abuse, perform critical clinical and legal actions, and manage cases that do not obviously require transfer to a higher level of care. Rural hospitals may benefit from further investigation into the barriers to uptake of resources and cost-effective means of supporting the initial assessment and care of victims of abuse.
Acknowledgments
The authors wish to acknowledge John Leventhal, MD, for feedback and guidance in the implementation of the study. This research has been supported in part by the National Heart, Lung and Blood Institute (NHLBI), supplement to U01/HL-04-001 (Training Core–Resuscitation Research). This study was previously presented at the Society for Academic Emergency Medicine Western Regional Research Forum in Park City, Utah, in January 2009, and at the Society for Academic Emergency Medicine Annual Assembly in New Orleans, Louisiana, in May 2009.
References
- 1.Cappelleri JC, Eckenrode J, Powers JL. The epidemiology of child abuse: findings from the Second National Incidence and Prevalence Study of Child Abuse and Neglect. Am J Public Health. 1993;83(11):1622–1624. doi: 10.2105/ajph.83.11.1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flitcraft A. Physicians and domestic violence: challenges for prevention. Health Aff. 1993;12(4):154–161. doi: 10.1377/hlthaff.12.4.154. [DOI] [PubMed] [Google Scholar]
- 3.Proehl RS. 2008 Oregon Population Report. Portland, OR: Population Research Center, Portland State University; 2009. [Google Scholar]
- 4.Oregon Office of Rural Health. [Accessed December 7, 2009];Rural Hospitals. Available at: http://www.ohsu.edu/ohsuedu/outreach/oregonruralhealth/hospitals/rural_hospitals.cfm.
- 5.Evaluating Domestic Violence Programs. Agency for Healthcare Research and Quality; [Accessed August 1, 2008]. Available at: http://www.ahrq.gov/research/domesticviol/ [Google Scholar]
- 6.Carr BG, Branas CC, Metlay JP, Sullivan AF, Camargo CA., Jr Access to Emergency Care in the United States. Ann Emerg Med. 2009;54(2):270–271. doi: 10.1016/j.annemergmed.2008.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Responding to Child Maltreatment: Children’s Hospitals Child Abuse Services. Alexandria, VA: National Association of Children’s Hospitals and Related Institutions; 2009. [Google Scholar]
- 8.Olson L, Anctil C, Fullerton L, Brillman J, Arbuckle J, Sklar D. Increasing emergency physician recognition of domestic violence. Ann Emerg Med. 1996;27(6):741–746. doi: 10.1016/s0196-0644(96)70193-2. [DOI] [PubMed] [Google Scholar]
- 9.Dienemann J, Trautman D, Shahan JB, et al. Developing a domestic violence program in an inner-city academic health center emergency department: the first 3 years. J Emerg Nurs. 1999;25(2):110–115. doi: 10.1016/s0099-1767(99)70155-8. [DOI] [PubMed] [Google Scholar]
- 10.Flaherty EG, Sege R. Barriers to physician identification and reporting of child abuse. Pediatr Ann. 2005;34(5):349–356. doi: 10.3928/0090-4481-20050501-08. [DOI] [PubMed] [Google Scholar]
- 11.Defining the Children’s Hospital Role in Child Maltreatment. Alexandria, VA: National Association of Children’s Hospitals and Related Institutions; 2006. [Google Scholar]
- 12.Flaherty EG, Jones R, Sege R. Telling their stories: primary care practitioners’ experience evaluating and reporting injuries caused by child abuse. Child Abuse Negl. 2004;28(9):939–945. doi: 10.1016/j.chiabu.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 13.Badger L. Reporting of Child Abuse: Influence of Characteristics of Physician, Practice and Community. South Med J. 1989;82(3):281–286. doi: 10.1097/00007611-198903000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Cohen S, DeVos E, Newberger E. Barriers to Physician Identification and Treatment of Family Violence: Lessons from Five Communities. Acad Med. 1997;72(1):S19–S24. [PubMed] [Google Scholar]
- 15.MacLeod KJ, Marcin JP, Boyle C, Miyamoto S, Dimand RJ, Rogers KK. Using telemedicine to improve the care delivered to sexually abused children in rural, underserved hospitals. Pediatrics. 2009;123(1):223–228. doi: 10.1542/peds.2007-1921. [DOI] [PubMed] [Google Scholar]