Abstract
Inclusion of concerned significant others (SO) in alcohol use treatment has demonstrated efficacy but has not been tested in the context of brief interventions. In this study, individual Motivational Interviewing (MI) sessions were compared to MI sessions including a significant other (SOMI) on within treatment outcomes (alliance, fidelity, client satisfaction and engagement). Participants (N = 382) were adult alcohol users recruited in a Level I Trauma Center. Perceived alliance did not differ across conditions, but patients and SOs reported higher alliance, satisfaction and engagement than was perceived by the therapist. The occurrence of MI components, or discussion areas, was consistent across conditions. Higher baseline SO drinking was associated with lower patient engagement, while higher baseline SO acceptance of patient drinking was associated with lower SO engagement. Results suggest individual MI sessions can be adapted to include an SO with minimal impact on patient acceptability and treatment fidelity. Research should, however, consider SOs’ influence on participant outcomes and the relevance of specific SO characteristics.
Keywords: Alcohol Treatment, Emergency Department, Motivational Interviewing, Significant Others, Treatment Fidelity
1. Introduction
Past studies have shown that motivational interventions delivered with hospital populations are effective in reducing alcohol use and associated consequences (e.g., Havard, Shakeshaft, & Sanson-Fisher, 2008; Longabaugh et al., 2001; Monti et al., 1999; Schermer, Moyers, Miller, & Bloomfield, 2006). To date, these interventions have been delivered almost exclusively in an individual format (Cordova, Zepeda-Warren, & Gee, 2001) despite the established efficacy of marital and family therapy alcohol treatment approaches (e.g., Edwards & Steinglass, 1995). Including spouses or partners in alcohol treatment can result in improved relationship functioning and reduced drinking (O’Farrell, 1993), but the acceptability of this approach by both patients and significant others (SO) in brief treatment is not well-studied. We also know little about whether brief treatments such as motivational interviewing (MI) can be delivered with fidelity when SOs are involved in sessions. Complicated relationship dynamics and SO characteristics may influence the therapy process, causing individually-delivered and conjoint MI sessions to look quite different. These are essential implementation questions to examine if including an SO in brief alcohol treatment is to be considered a feasible adaptation with hospital populations.
1.1. SO Involvement and Intervention Efficacy and Acceptability
Social network members may be positive or negative influences on substance abuse treatment process and outcome. Reviews of the literature suggest that SO-involved interventions reliably increase the probability that an at-risk alcohol user will initiate change (O’Farrell & Fals-Stewart; 2003) as well as aid general improvements in treatment retention and efficacy (O’Farrell, 1993). There is also evidence that intervention exclusively with the SO can result in reduced resistance to treatment in the drinking partner (Meyers, Apodaca, Flicker, & Slesnick, 2002). On the other hand, a drinker’s social network may include other drinkers, which can negatively influence treatment engagement (Havassy, Hall, & Wasserman, 1991; Mohr, Averna, Kenny, & DelBoca, 2001) or increase risk of relapse (Havassy, Hall, & Wasserman, 1991; McCrady, 2004). Alcoholic men and women also often drink with their partners (e.g., Fernandez-Pol, Bluestone, Missouri, Morales, & Mizruchi, 1986). Therefore, although there is support for involving an SO in MI sessions to enhance outcomes, individual social network members may also hinder drinking reduction (McCrady, 2004).
Although effective, SO-involved interventions typically require multiple sessions, which presents a barrier to delivery in “opportune settings” such as hospital Emergency Departments or Trauma Centers. Most often, the patients in these settings are recruited following a screening for alcohol risk, and brief motivational interventions are delivered in the moment, capitalizing on the emotional charge of the hospital experience (e.g., Longabaugh, Minugh, Nirenberg, Clifford, Becker, & Woolard, 1995). With SO involvement, a provider must build rapport with not one, but two patients in the course of a single session. It is unknown whether this would negatively impact treatment acceptability, patient satisfaction and engagement, and therefore progress toward change-related goal setting.
There is good theoretical rationale for including an SO in MI sessions; SOs represent one form of natural support that can facilitate patient intrinsic movement toward change (Miller & Rollnick, 2002). Created for Project MATCH, Motivational Enhancement Therapy (MET; see Miller, Zweben, DiClemente, & Rychtarik, 1992) suggested including an SO in one or two of the early treatment sessions to help the patient explore and resolve ambivalence regarding change in drinking behavior. SO participants, actively involved in MI sessions, can describe alcohol-related consequences, offer supportive statements, and identify possible change options that may be more easily received than if offered by the therapist. In Project MATCH, however, only 17% of outpatient and 13% of aftercare MET participants elected SO involvement (Carroll et al., 1998). Further, in an MI study guided by the Project MATCH manual, participants in the MI group requested that an SO participate in only 2 of 104 cases (Miller, Yahne, & Tonigan, 2003). Project COMBINE delayed SO involvement until after the delivery of feedback, and achieved a higher percent (30%) of clients with SO involvement in one or more treatment sessions (Longabaugh, Zweben, Locastro, & Miller, 2005). Given these findings, potential barriers to SO participation as well as the nature of SO influence in MI sessions warrants further consideration. To our knowledge, no past studies have included random assignment to SO-involved (SOMI) or individual (IMI) MI sessions. Therefore examining the comparative acceptance of and fidelity to the intervention may have important implications for adaptation and implementation within opportune hospital settings.
1.2. MI Fidelity
Evaluating the relationship between patient outcomes and clinician competence in MI delivery is a key emerging area of research (Apodaca & Longabaugh, 2009; Burke, Arkowitz, & Dunn, 2002; Moyers, Martin, Manuel, Hendrickson, & Miller, 2005). Collaboration between therapist and patient, as well as empathy, acceptance, genuineness, and egalitarianism expressed by the therapist has been noted as important elements of the “spirit” of MI (Miller & Rollnick, 2002). These qualities, well-established in the general psychotherapy literature, have been linked with improved outcomes in MI (Moyers, Miller, & Hendrickson, 2005). Past research has also identified good adherence to MI components (e.g., Pros and Cons of Alcohol Use, Personalized Feedback, Change Plan) in individually-delivered MI sessions, which have resulted in reduced drinking behaviors (e.g., Barnett, Murphy, Colby, & Monti, 2007; Borsari & Carey, 2005; Wood, et al., 2010). We are not aware of any past studies that have examined therapist fidelity to MI components when also including an SO. Given the brief nature of MI, the addition of a concerned family member or friend may have implications on therapists’ abilities to complete all discussion areas, while also adhering to MI principles and spirit.
The purpose of this study was to examine treatment implementation and characteristics in individual and significant other MI sessions conducted in an opportune hospital setting. Of particular interest was whether treatment processes differed when romantic partners, family, or concerned friends are involved in an MI session. Specifically, we sought to: (1) describe the general characteristics of SOs that may be seen in this setting, (2) assess whether treatment alliance, satisfaction, and engagement differed across therapist, patient, and SO reports, (3) examine differences in specific MI components across IMI and SOMI sessions, and finally, (4) determine whether specific characteristics of patients and SOs involved in SOMI sessions were associated with patient and SO satisfaction and engagement in the session.
2. Method
2.1. Sample
This study was conducted with baseline and treatment process data from a randomized controlled trial that compared the efficacy of an individual MI session to an MI session that included a concerned significant other (SOMI). Participants in this study (N = 382) were adult emergency and trauma department patients from a Level I trauma center in the northeast United States. Patients were 18 years or older who (a) had a blood alcohol concentration greater than. 01% or self-reported alcohol use in the six hours prior to the event precipitating hospital entry, or scored eight or higher on the Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, De La Fuente, & Grant, 1993) and (b) identified at least one significant other for inclusion in the study. Participants who did not speak English, failed a mini-mental status exam, had a self-inflicted injury, or were in police custody were excluded. To be eligible to participate as an SO, individuals had to be rated by patients as at least “supportive” in the patient’s life and be no more than a “moderate” drinker (Important People Instrument; Longabaugh & Zywiak, 1998). All procedures were approved by the university and hospital Institutional Review Boards and participants gave written informed consent.
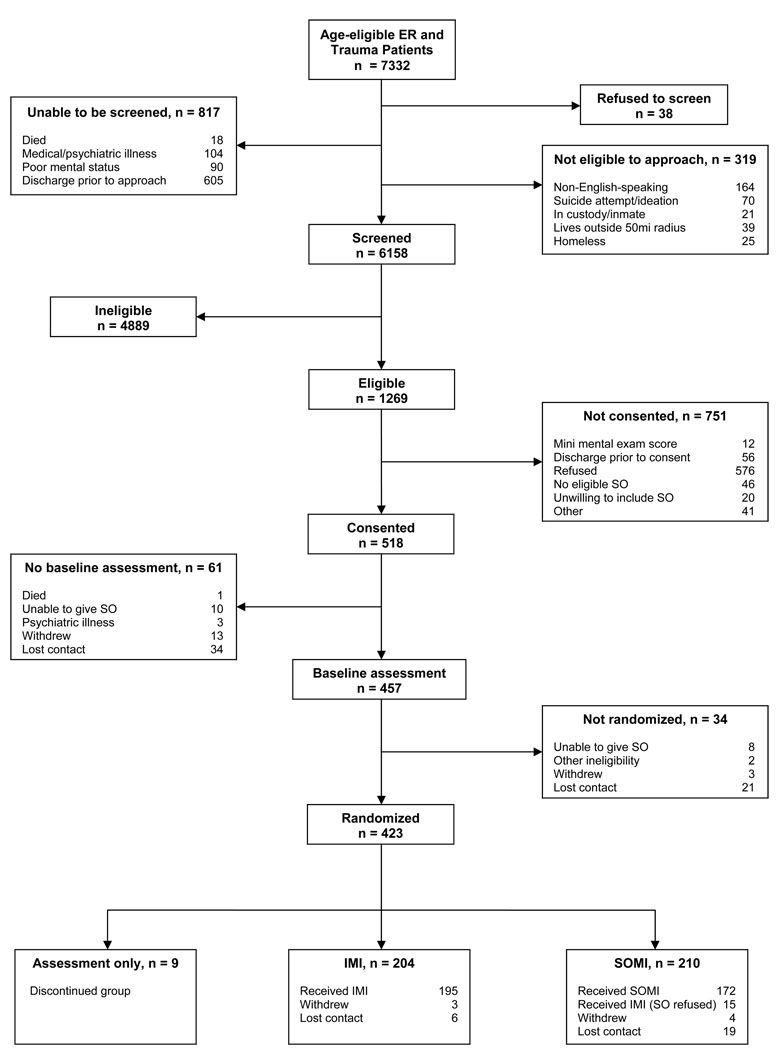
Of eligible participants (N = 1269), 5.6% were not consented or did not receive a baseline assessment for SO reasons (no eligible SO or refusal to name SO). An additional 5% of assessed individuals (n = 457) either did not receive treatment (n = 8) or did not receive SOMI treatment (n = 15) due to inability to name an SO or SO refusal. Please see Figure One for further information on participant recruitment and retention. Patients and SOs were compensated for their participation in baseline assessment, the treatment sessions, and at follow-ups.
Figure 1.
Participant recruitment and retention within treatment
2.2. Intervention Conditions
Following baseline assessment, participants were urn randomized, by five variables: (age ≥ 24 years old; AUDIT ≥ 15 points; injury severity ≥ 4 days in trauma unit; gender, and romantic/non-romantic SO), to receive a single MI or SOMI session. Both intervention conditions followed central MI principles and techniques described by Miller and Rollnick (2002). The purpose of these sessions was to explore participant alcohol use and motivation to make changes in their drinking. The intervention conditions were manualized, but flexibly-tailored to individual patients with eight possible treatment components (i.e., discussion areas). The possible components were as follows: Describe the Accident/Injury, Typical Week of Alcohol Use, Pros and Cons of Alcohol Use, Personalized Feedback on Alcohol Use, Exploring Goals and Values, Looking Forward/Looking Back, Importance and Confidence Rulers, and a written Change Plan. In addition, SOMI sessions included strategies intended to facilitate SO involvement including Enhancing Patient Motivation and Supporting Efforts Toward Change (e.g., exploring the SO’s pros and cons regarding the patient’s drinking and past and future attempts to aid changes in drinking). Therapists also attempted to involve SOs throughout each component (Apodaca, Gogineni, Barnett, & Monti, 2006).
The MI sessions were conducted by 13 doctoral- and masters-level counselors; training included 25–30 hours of didactic learning, discussion, and role-play, and the therapists received MI supervision weekly. Therapists were trained to deliver both MI and SOMI sessions. Prior to conducting client sessions, each therapist was evaluated on MI skills and met a threshold level of competence as determined by the research team. Participants had follow-up assessments at 6 and 12 months (data not reported).
2.3. Measures
2.3.1. Treatment process measures
Session processes and characteristics were assessed with treatment quality and adherence measures designed for use within the study. These Likert-rated assessments were completed, in private, following each session by therapists, patients, and SOs. To minimize the effect of demand characteristics, patients were instructed to answer honestly, informed that their individual counselors would not see their results, and that these forms were to be used for the purpose of clinical supervision. Immediately after completion, patients and SOs placed the measures in sealed envelopes, which were delivered directly to the clinical supervisor.
Reported alliance, satisfaction and engagement were the primary within-session outcomes of interest. Alliance was measured with 9 items; the therapist version measured perceived patient alliance, and the patient and SO version measured self-reported alliance. Alliance items for therapists, patients, and SOs showed sound internal consistency (see Table 1), and were examined as composite measures in inferential analyses. Occurrence and perceived usefulness of MI discussion components (11 individual MI items and 16 SO items), satisfaction with session (1 item), and engagement in session (1 item) were also completed by therapists, patients and SOs.
Table 1.
Therapist, patient and SO views of treatment process
| Process Itema | Therapist M(SD) |
Patient M(SD) |
SO M(SD) |
|---|---|---|---|
| Individual MI Sessions | |||
| Alliance Itemsb | |||
| Was easy to talk to | 3.77(.49) | 3.81(.63) | |
| Was concerned about me | 3.51(.57) | 3.60(.71) | |
| Understood me | 3.54(.57) | 3.67(.67) | |
| Asked about my own ideas before presenting his/hers |
3.60(.53) | 3.71(.67) | |
| Helped me talk about my own reasons for change | 3.48(.66) | 3.70(.67) | |
| Treated me like an equal | 3.65(.53) | 3.82(.62) | |
| Respected my ideas about how change can occur | 3.62(.55) | 3.81(.57) | |
| Did not push me into something I was not ready for | 3.59(.57) | 3.80(.62) | |
| Accepted that I might choose not to change | 3.63(.53) | 3.54(.87) | |
| Total | 32.26(3.75)** | 33.55(4.98) | |
| Total Alliance Internal Consistency | .894 | .945 | |
| Satisfaction and Engagementc | |||
| How satisfied were you with the overall session? | 3.62(.92)** | 4.65(.55) | |
| How engaged did you feel? | 4.07(.89)** | 4.68(.63) | |
| SO MI Sessions | |||
| Alliance Itemsb | |||
| Was easy to talk to | 3.74(.49) | 3.86(.54) | 3.91(.42) |
| Was concerned about me | 3.52(.53) | 3.51(.78) | 3.59(.59)d |
| Understood me | 3.50(.55) | 3.64(.64) | 3.77(.53) |
| Asked about my own ideas before presenting his/hers |
3.52(.57) | 3.76(.62) | 3.77(.53) |
| Helped me talk about my own reasons for change | 3.45(.63) | 3.73(.59) | 3.76(.52) |
| Treated me like an equal | 3.64(.48) | 3.89(.49) | 3.88(.52) |
| Respected my ideas about how change can occur | 3.63(.48) | 3.84(.50) | 3.79(.58) |
| Did not push me into something I was not ready for | 3.63(.49) | 3.84(.54) | 3.84(.57) |
| Accepted that I might choose not to change | 3.63(.51) | 3.66(.73) | 3.62(.73) |
| Total | 32.30(3.26)** | 33.81(4.27) | 33.87(3.89) |
| Total Alliance Internal Consistency | .859 | .925 | .908 |
| Satisfaction and Engagementc | |||
| How satisfied were you with the overall session? | 3.46(1.01)** | 4.70(.59) | 4.69(.60) |
| How engaged did you feel? | 3.94(.95)** | 4.65(.60) | 4.57(.76) |
Patient version shown.
4-point scale from 1 = “strongly disagree” to 4 = “strongly agree”.
5-point scale from 1 = “not at all” to 5 = “very”.
For SOs the item was: “Therapist helped me believe I could contribute to changing my SOs drinking if I wanted to”.
difference significant at .005 level.
2.3.2. Patient measures
Patient baseline alcohol use was assessed with a 6-month Graduated Frequency for Alcohol (GF; Greenfield & Rogers, 1999). This measure results in composite indicators of past 6-month alcohol use frequency (number of drinking days) and quantity (number of drinks per drinking day). The smoking Contemplation Ladder (Biener & Abrams, 1991) has been previously modified to assess motivation to change drinking behavior in a hospital-based MI study (Becker, Maio, & Longabaugh, 1996). The single-item measure states, “Each rung of this ladder represents where a person might be in thinking about changing their drinking. Select the number that best represents where you are now.” Item options range from “no thought of changing” (0) to “taking action to change” (10).
2.3.3. SO measures
SO baseline alcohol use was measured with a 6-month GF (Greenfield & Rogers, 1999), resulting in composite measures of past 6 month frequency and quantity. SO relationship type (e.g., spouse or other romantic partner, immediate or extended family member, friend, roommate, or co-worker) and reaction to the patient’s drinking (i.e., left when patient drank, did not accept, neutral, accepted, encouraged) were assessed via patient report using The Important People Instrument (Longabaugh & Zywiak, 1998). For analyses, relationship type was categorized as romantic partner, family, or concerned friend. Report of SO reaction to the patient’s drinking was also categorized as did not accept, neutral, and accepted.
2.4. Data Analysis
Sample characteristics, therapist, patient and SO reports of treatment components were summarized with means, standard deviations, and percentile estimates. To examine differences in process variables by reporter (i.e., therapist, patient, SO) and by treatment condition, paired and independent sample t-tests were conducted. For inferential aims regarding the impact of participants on SOMI sessions, one-way analyses of variance were conducted to compare the impact of romantic partner, family and concerned friend SO types on the patient- and SO-rated within-session processes of interest (i.e., alliance, satisfaction, and engagement). Patient and SO gender were also examined in relation to these outcomes in two independent samples t-tests. Finally, a series of rank order correlations was conducted to test associations between patient drinking and motivation measures, SO drinking and reaction measures, and patient- and SO-rated alliance, satisfaction, and engagement.
3. Results
3.1. Sample characteristics
The treated sample (N = 380) was primarily male (67.6%), had an average age of 33 years (SD = 11.2), and 12.4 years of education (SD = 2.3). The majority were never married (60.5%) and White (70.7%), followed by African American (18.9%). The average baseline AUDIT score was 15.3 (SD = 8.2), and 46% of participants reported drinking alcohol prior to hospital entry. The patients in this sample reported drinking, on average, 97 days (SD = 60.2) in the past 6 months with an average of 9.4 (SD = 6.5) drinks per drinking day. The average reported readiness to change drinking at baseline was 5.7 (SD = 3.7), which corresponds to “I should change someday, but I am not ready”.
The majority (76.6%) of SOs named as the participant’s first choice were recruited into the study. Of all recruited SOs, 41% were romantic partners, 30.3% were friends, and 28.6% were family members. The majority of romantic partner SOs were cohabitating partners (49.3%), followed by non-cohabitating partners (28.2%) and spouses (19.7%). Family members were primarily mothers (38.4%), siblings (29.3%) and daughters (14.1%). Of concerned friends, 92% were identified as friends (not other concerned participants such as roommates or coworkers). Male patients were more likely than female patients to have romantic partner SOs (47.2% vs. 27.9%) and female patients were more likely than male patients to have friend SOs (38.7% vs. 26.4%; χ2(2, 346) = 11.91, p < .005). Overall, SOs drank, on average, 48 days (SD = 58.2) in the past 6 months with an average of 5.2 (SD = 5.2) drinks per drinking day, but SO drinking did not significantly differ by relationship type. Family members were least likely to accept the patient’s drinking compared to romantic partners and friends (F(2, 330) = 4.36, p < .05).
3.2. Therapist, patient and SO views of treatment alliance
Table 1 shows the internal consistency for the Total Alliance composite measure, which was excellent with alpha values ranging from .86 to .95 across therapist, patient, and SO ratings. Ratings of alliance were higher when rated by the patient or SO than when rated by the therapist, and these differences were statistically significant (see Table 1). Patients and SOs also provided significantly higher ratings on session satisfaction and engagement than therapists (see Table 1).
3.3. Treatment components/fidelity by MI and SOMI sessions
Table 2 shows therapist-rated component occurrence varied substantially (47.9% to 98.8%) in these flexibly delivered intervention sessions. While components such as Typical Week, Pros and Cons, Goals and Values, Looking Forward/Looking Back, and Importance and Confidence Rulers occurred most of the time (84.2% to 98.8%), other components (such as Describe the Accident/Injury, Change Plan, and Personalized Feedback) were more variable in occurrence (47.9% to 70.3%). The MI and SOMI sessions did not differ in therapist report of the component occurrence, and patients rated components as equally useful regardless of treatment condition (see Table 2). Finally, SOMI sessions were slightly longer than MI sessions (M = 48.3, SD = 17.2, M = 44.1, SD = 16.3, respectively), but this mean difference was 4.2 minutes, (t(339) = 2.33, p < .05).
Table 2.
Therapist-reported treatment components and patient-rated usefulness by individual and SOMI sessions
| Treatment component itema | Individual MI Therapist report % used (N = 209) |
Individual MI Patient report M(SD) |
SO MI Therapist report % used (N = 171) |
SO MI Patient report M(SD) |
|---|---|---|---|---|
| Describe the accident/injury | 53.6 | 2.57(.59) | 47.9 | 2.46(.63) |
| Describe a typical week of drinking | 95.7 | 2.61(.59) | 98.2 | 2.65(.53) |
| Explored pros of drinking | 97.6 | 2.54(.65) | 98.8 | 2.44(.69) |
| Things SO likes about patient’s drinking | 89.5 | 2.50(.70) | ||
| Explored cons of drinking | 98.1 | 2.78(.47) | 98.8 | 2.75(.49) |
| Things SO doesn’t like about the patient’s drinking | 91.2 | 2.67(.57) | ||
| Used technique of looking forward/looking back | 67.5 | 2.62(.63) | 68.4 | 2.68(.55) |
| Explored patient goals and values | 93.3 | 2.82(.41) | 90.6 | 2.82(.43) |
| How the SO has made positive attempts in the past to help the patient with his/her drinking |
91.2 | 2.47(.67) | ||
| How the patient’s friends and/or family feel about drinking |
91.2 | 2.50(.67) | ||
| Ways in which the SO can help the patient reduce alcohol use |
93.0 | 2.51(.67) | ||
| Provided feedback on drinking norms | 69.4 | 2.62(.57) | 66.7 | 2.60(.54) |
| Provided feedback on consequences of drinking | 68.9 | 2.69(.56) | 67.2 | 2.65(.54) |
| Provided feedback on BAC levels | 70.3 | 2.63(.59) | 65.5 | 2.68(.51) |
| Provided feedback on personal risk factors | 68.9 | 2.62(.60) | 66.1 | 2.68(.52) |
| Used importance and confidence rulers | 84.2 | 2.61(.63) | 87.1 | 2.68(.54) |
| Created change plan | 54.1 | 2.52(.69) | 50.9 | 2.58(.63) |
3-Point; 1 = “not at all useful”, 2 = “somewhat useful”, 3 = “very useful”.
3.4. The effect of SOs on SOMI sessions
Patients in SOMI sessions did not differ in their reported total alliance, satisfaction, or engagement when the SOs were romantic partners, family or friends. Female patients reported higher engagement than males (t(162) = −2.54, p < .05), but not alliance or satisfaction. SO self-reported alliance, satisfaction, and engagement did not differ by relationship type or by SO gender. Among the patient (baseline past 6 month frequency and quantity, pre-session motivation) and SO (baseline past 6 month frequency and quantity, reaction to patient’s drinking) variables examined, the only SO drinking variable associated with patient engagement was SO-reported past 6 month drinking quantity, which had a negative association with patient self-rated engagement (rs = −.23, p < .05). This association suggests that the inclusion of heavier drinking SOs was associated with lower levels of patient engagement. For SO satisfaction and engagement, only patient reported SO acceptance of drinking was significant, and had a negative association with SO engagement (rs = −.19, p < .05). Thus, SOs accepting of patient drinking were less likely to be engaged in SOMI sessions than those that were non-accepting.
4. Discussion
Within this hospital-based sample of high-risk adult alcohol users, MI and SOMI sessions were delivered with a high degree of acceptability and consistency. Therapists perceived slightly lower alliance and patient satisfaction and engagement, but these ratings were consistently positive overall. These analyses suggest it is possible to include a significant other in MI sessions and maintain a high level of patient engagement and satisfaction. Males sought more SO support from romantic partners while females sought support from friends, which is consistent with previous work with treatment seeking samples (Rice & Longabaugh, 1996). However, SO drinking and attitudes toward drinking appeared to be the most important SO characteristics for future research and SOMI implementation. Specifically, SO drinking had a negative association with patient engagement and SOs who were accepting of patient drinking were less likely to feel engaged in sessions than SOs who were unaccepting. Within session outcomes did not differ by the three SO relationship types, but romantic partners had the highest proportion of acceptance of patient drinking. Therefore, the inclusion of an SO in these sessions may be less helpful when the SO themselves are drinkers, or when the SO is supportive of the patient’s drinking, and these indicators may be more important to consider than characteristics such as SO gender or type of SO relationship.
The SOMI sessions were generally well-received. Therapist ratings of the sessions, however, were somewhat lower than participant ratings. Although significantly different, these ratings were qualitatively consistent. It is possible that this reflects different expectations and processes. For example, a therapist may have been somewhat disappointed if the patient did not decide to complete a change plan during the session, while the patient may have felt very satisfied and engaged due to having a nonjudgmental conversation about his/her drinking. Research on training in MI suggests acceptable agreement among trained practitioners and independent raters (Hartzler, Baer, Dunn, Rosengren, & Wells, 2007), but therapists may somewhat undervalue their own skills or therapeutic impact. SOMI sessions were, on average, slightly longer than IMI sessions, but component occurrence and rated usefulness were quite similar. Moreover, previous work shows that both patients in both conditions were equally likely to complete a written Change Plan, which can be considered a proximal marker of commitment (Magill, Apodaca, Barnett, & Monti, 2010). In sum, treatment consistency and acceptability were highly similar in IMI and SOMI conditions.
SO drinking and response to the patient’s drinking had an effect on ratings of session engagement within SOMI. Motivational interviewing is designed to facilitate behavior change among individuals at varying stages of motivational readiness, and our results suggest that this orientation can be extended to those enlisted to be in support of change. The relative brevity of MI is connected to its capitalization on patient intrinsic desires and natural support systems that facilitate behavior change (Miller & Rollnick, 2002). If the natural support system involves other heavy drinkers, involving those individuals in treatment session may be less helpful than including others who are supportive of drinking reduction or cessation. Patient, but not SO gender, was associated with higher self-reported levels of engagement, but further research will need to consider these findings more closely. Specifically, future studies should examine the role of SO support, motivation, and drinking variables in relation to treatment process and patient outcomes, and whether these associations are moderated by gender. This is particularly true for hospital settings where participants may receive opportunistic intervention, and therefore be at varying stages of readiness for change.
Limitations of this study warrant discussion. This work is cross-sectional, conducts secondary analysis, and should be considered exploratory. We intentionally selected SOs that were identified by the participant as being supportive in general, and other inclusion criteria might have resulted in different outcomes. However, the majority of SOs named as the participant’s first choice for involvement were recruited into the study, which indicates that this inclusion criterion might not have created an important selection bias. The fact that such a high proportion of selected SOs were enrolled also supports the disseminability of SO involved MI interventions in opportune hospital settings. Patients were enrolled from two sites in our Trauma Center, but generalizability will be limited to similar settings.
This study indicates that involving a concerned other in an opportunistic brief intervention for alcohol is acceptable and perceived as useful. Patients will often be accompanied to the hospital Emergency Department or Trauma Center by a concerned other, and the present work suggests that SO-involved brief MIs are an acceptable and disseminable approach. Additional work on the impact of SO characteristics is needed to inform providers of the degree of latitude in implementing opportune brief intervention with hospital patients, and SOs, that may present with a range of alcohol risk and motivation to change. Specifically, future studies should examine the role of SO support, motivation, and drinking variables in relation to MI process and outcomes.
Acknowledgement
Preparation of this manuscript was supported by the National Institute on Alcohol Abuse and Alcoholism by grant number AA009892-11A1 (R01; Monti), by a Department of Veterans Affairs Senior Career Scientist Award to P. Monti. It was also supported by training grant T32 AA07459 awarded to Molly Magill and Nadine Mastroleo. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Apodaca TR, Gogineni A, Barnett NP, Monti PM. Project ACT Motivational Interviewing Therapist Manual. 2006. [available upon request from the first author] [Google Scholar]
- Apodaca TR, Longabaugh R. Mechanisms of action in motivational interviewing: A review of the evidence. Addiction. 2009;104:705–715. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett NP, Murphy JG, Colby SM, Monti PM. Efficacy of counselor vs. computer-delivered intervention with mandated college students. Addictive Behaviors. 2007;32(11):2529–2548. doi: 10.1016/j.addbeh.2007.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker B, Maio RF, Longabaugh R. One for the road: Current concepts and Controversies in alcohol intoxication and injury; Presented at the annual meeting of the Society for Academic Emergency Medicine; Denver, CO. 1996. [Google Scholar]
- Biener L, Abrams DB. The Contemplation Ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychology. 1991;10:360–365. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Two brief alcohol interventions for mandated college students. Psychology of Addictive Behaviors. 2005;19(3):296–302. doi: 10.1037/0893-164X.19.3.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke BL, Arkowitz H, Dunn C. The efficacy of motivational interviewing and its adaptations. In: Miller WR, Rollnick S, editors. Motivational interviewing: Preparing people to change addictive behavior. 2nd Ed. New York: Guilford Press; 2002. [Google Scholar]
- Carroll KM, Connors GJ, Cooney NL, DiClemente CC, Donovan DM, Kadden RR, et al. Internal validity of Project MATCH treatments: Discriminability and integrity. Journal of Consulting and Clinical Psychology. 1998;66:290–303. doi: 10.1037//0022-006x.66.2.290. [DOI] [PubMed] [Google Scholar]
- Cordova JV, Zepeda Warren L, Gee CB. Motivational interviewing as an intervention for at-risk couples. Journal of Marital and Family Therapy. 2001;27:315–326. doi: 10.1111/j.1752-0606.2001.tb00327.x. [DOI] [PubMed] [Google Scholar]
- Edwards ME, Steinglass P. Family therapy treatment outcomes for alcoholism. Journal of Marital and Family Therapy Special Issue: The effectiveness of marital and family therapy. 1995;21:475–509. [Google Scholar]
- Fernandez-Pol B, Bluestone H, Missouri C, Morales G, Mizruchi JS. Drinking patterns of inner-city Black Americans and Puerto Ricans. Journal of Studies on Alcohol. 1986;47:156–160. doi: 10.15288/jsa.1986.47.156. [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Rogers JD. Who drinks most of the alcohol in the U.S.? The policy implications. Journal of Studies on Alcohol. 1999;60:78–89. doi: 10.15288/jsa.1999.60.78. [DOI] [PubMed] [Google Scholar]
- Hartzler B, Baer JS, Dunn C, Rosengren DB, Wells E. What is seen through the looking glass: The impact of training on practitioner self-rating of motivational interviewing skills. Behavioural and Cognitive Psychotherapy. 2007;35(4):431–445. [Google Scholar]
- Havard A, Shakeshaft A, Sanson-Fisher R. Systematic review and meta-analysis of strategies targeting alcohol problems in emergency departments: Interventions reduce alcohol-related injuries. Addiction. 2008;103:368–376. doi: 10.1111/j.1360-0443.2007.02072.x. [DOI] [PubMed] [Google Scholar]
- Havassy BE, Hall SM, Wasserman DA. Social support and relapse: Commonalities among alcoholics, opiate users and cigarette smokers. Addictive Behaviors. 1991;16:235–246. doi: 10.1016/0306-4603(91)90016-b. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Minugh PA, Nirenberg TD, Clifford PR, Becker B, Woolard R. Injury as a motivator to reduce drinking. Academy of Emergency Medicine. 1995;2:817–825. doi: 10.1111/j.1553-2712.1995.tb03278.x. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Woolard RE, Nirenberg TD, Minugh AP, Becker B, Clifford PR, Carty K, Sparadeo F, Gogineni A. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. Journal of Studies on Alcohol. 2001;62:806–816. doi: 10.15288/jsa.2001.62.806. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Zweben A, Locastro JS, Miller WR. Origins, issues and options in the development of the combined behavioral intervention. Journal of Studies on Alcohol, Suppl. 2005;15:179–187. doi: 10.15288/jsas.2005.s15.179. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Zywiak W. Important People Instrument. Providence, RI: Brown University; 1998. Center for Alcohol and Addiction Studies. 02912 (available by request from the first author) [Google Scholar]
- Magill M, Apodaca TR, Barnett NP, Monti PM. The route to change: Within-session predictors of change plan completion in a motivational interview. Journal of Substance Abuse Treatment. 2010;38(3):299–305. doi: 10.1016/j.jsat.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrady BS. To have but one true friend: Implications for practice of research on alcohol use disorders and social networks. Psychology of Addictive Behaviors. 2004;18:113–121. doi: 10.1037/0893-164X.18.2.113. [DOI] [PubMed] [Google Scholar]
- Meyers RJ, Apodaca TR, Flicker SM, Slesnick N. Evidence-based approaches for the treatment of substance abusers by involving family member. The Family Journal: Counseling and Therapy for Couples and Families. 2002;10:281–288. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York: Guilford; 2002. [Google Scholar]
- Miller WR, Yahne CE, Tonigan JS. Motivational interviewing in drug abuse services: A randomized trial. Journal of Consulting and Clinical Psychology. 2003;71(4):754–763. doi: 10.1037/0022-006x.71.4.754. [DOI] [PubMed] [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Washington, DC: Government Printing Office; Motivational Enhancement Therapy Manual: A clinical research guide for therapists treatment individuals with alcohol abuse and dependence. NIAAA Project MATCH Monograph Series. 1992;Vol. 2 [Publication No. (ADM) 92-1894)]
- Mohr CD, Averna S, Kenny DA, DelBoca FK. “Getting by (or getting high) with a little help from my friends”: An examination of adult alcoholics’ friendships. Journal of Studies on Alcohol. 2001;62:637–645. doi: 10.15288/jsa.2001.62.637. [DOI] [PubMed] [Google Scholar]
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, Woolard R, Lewander W. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Hendrickson SML, Miller WR. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005;28(1):19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Miller WR, Hendrickson SML. How Does Motivational Interviewing Work? Therapist Interpersonal Skill Predicts Client Involvement Within Motivational Interviewing Sessions. Journal of Consulting and Clinical Psychology. 2005;73(4):590–598. doi: 10.1037/0022-006X.73.4.590. [DOI] [PubMed] [Google Scholar]
- O'Farrell TJ. Treating alcohol problems: Marital and family interventions. New York: Guilford; 1993. [Google Scholar]
- O'Farrell TJ, Fals-Stewart W. Alcohol abuse. Journal of Marital and Family Therapy. 2003;29(1):121–146. doi: 10.1111/j.1752-0606.2003.tb00387.x. [DOI] [PubMed] [Google Scholar]
- Rice C, Longabaugh R. Measuring general social support in alcoholic patients: Short forms for perceived social support. Psychology of Addictive Behaviors. 1996;10(2):104–114. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schermer CR, Moyers TB, Miller WR, Bloomfield LA. Trauma center brief interventions for alcohol disorders decrease subsequent driving under the influence arrests. The Journal of Trauma: Injury, Infection, and Critical Care. 2006;60:29–34. doi: 10.1097/01.ta.0000199420.12322.5d. [DOI] [PubMed] [Google Scholar]
- Wood MD, Fairlie AM, Fernandez AC, Borsari B, Capone C, Laforge R, et al. Brief motivational and parent interventions for college students: A randomized factorial study. Journal of Consulting and Clinical Psychology. 2010;78:349–361. doi: 10.1037/a0019166. [DOI] [PMC free article] [PubMed] [Google Scholar]