Abstract
Background
The purpose of this study was to examine rates of traumatic events and PTSD in cocaine dependent cases and a community comparison sample.
Methods
Participants were interviewed as part of the Family Study of Cocaine Dependence. A cross-sectional case-cohort design assessed a total of 918 participants: 459 cocaine dependent cases recruited from chemical dependency treatment and 459 community-based participants. Community-based comparison participants were matched to cocaine dependent cases on year of birth (within 1 year), ethnicity, gender, and neighborhood (zip code). Participants completed a personal interview modeled after the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA).
Results
Compared to community-based individuals, cocaine dependent cases recruited from treatment experienced higher rates of assaultive events including rape or sexual assault in women (58% vs. 33%) and threatened with a weapon in men (75% vs. 52%). Cocaine dependent cases endured significantly more types of trauma than the community-based participants (4.64 vs. 3.08) and PTSD (22.4% and 12.2%). The number of traumatic exposures, witnessing trauma to others, experiencing violent trauma, and being female were predictive of conditional risk of PTSD, even after controlling for cocaine dependence and other demographic factors.
Conclusions
Cocaine dependence is strongly associated with an increased risk of exposure to traumatic events and PTSD and experiencing multiple, violent traumas increases the risk of PTSD, regardless of cocaine dependence. The high prevalence of trauma seen in our community-based participants emphasizes the role of violence in the neighborhood and the connection between drug dependence, trauma exposure, and PTSD.
Keywords: Trauma, PTSD, Cocaine Dependence, Neighborhood
1. Introduction
1.1 Prevalence of trauma & PTSD among drug users
Substance dependence is a serious health problem that is complicated by a greater risk of experiencing violence and developing posttraumatic stress disorder (PTSD). In the National Comorbidity Study, 7.8% of the general population reported lifetime PTSD (Kessler et al., 1995) while in contrast, studies with drug users described much higher rates of trauma and PTSD (Back et al., 2000; Johnson et al., 2003; Johnson et al., 2006; Mills et al., 2005; Mills et al., 2006; Najavits et al., 2003; Reynolds et al., 2005). For example, Johnson et al. (2006) reported in a sample of drug users that 42% experienced a traumatic event and of those who experienced trauma, 44% met criteria for PTSD. Likewise, Mills et al. (2005) studied distressing events in heroin dependent individuals and found that 92% were exposed to trauma and among those, 45% met PTSD criteria.
These examples highlight the conditional risk of PTSD, that is, the rate of PTSD among individuals who have experienced at least one traumatic event, whereas the general population prevalence reported by Kessler et al. (1995) is for all individuals. Cottler et al. (1992) examined rates of trauma and PTSD in the general population and found that alcohol and drug users were almost twice as likely to experience a traumatic event compared to non-users. This study also provides a direct comparison of conditional risk of PTSD, where drug users were three times more likely to meet criteria for PTSD than non-users (Cottler et al., 1992).
There are multiple theories about the relationship between drug use disorders and PTSD. One possible explanation is that drug users engage in risky and criminal behaviors making them more vulnerable to experiencing violent and traumatic events, thus elevating their risk of PTSD (Cottler et al., 1992). Alternatively, the self-medication hypothesis proposes that drugs are used to alleviate symptoms of painful traumatic experiences and PTSD (Brown and Wolfe, 1994; Chilcoat and Breslau, 1998a, b). Many studies indicate that trauma exposure is high in “hard” drug users (i.e., cocaine and opiates) and polysubstance users (Cottler et al., 1992; Johnson et al., 2006; Mills et al., 2005; Mills et al., 2006; Najavits et al., 1998). This may be explained in part by the high risk behaviors associated with the acquisition and use of these drugs, which lends evidence to support the first explanation described above. In the National Household Survey on Drug Abuse, those who used alcohol, cannabis, and cocaine were more likely to commit violent and non-violent crimes compared to those who used alcohol and cannabis only or alcohol only (Harrison and Gfroerer, 1992). Even if a drug user does not personally commit a crime, he or she likely associates with people who do (i.e., drug dealers), which puts them at an increased risk of experiencing violence and victimization.
We know that individuals with substance dependence are at high risk for experiencing traumatic events, but how this compares with the risk for other people living in their same neighborhoods is not as clear. Most studies compare rates of trauma and PTSD among drug users to the general population, which does not take into account the prevalence of violence in different communities. Several studies have examined communities with high rates of drug use (Bell et al., 1998; Kadushin et al., 1998; Petronis & Anthony, 2000). Residents in these neighborhoods deal with factors of social disorganization, poor economic conditions, chronic disease, and traumatic events (Bell et al., 1998). Considering these findings, it is reasonable to assume that individuals from the same community as drug users may also experience elevated rates of distressing events.
The development of PTSD is influenced by a variety of factors including psychopathology, the nature of the event, and the number of prior traumatic events. In a meta-analysis, Ozer et. al (2003) found that both distal factors (e.g., lifetime and family history of psychopathology) and proximal factors to the trauma (e.g., perceived life threat, perceived support) were significant predictors of the development of PTSD, with the latter proximal factors as the strongest predictors. In addition to the proximal factors discussed by Ozer and colleagues (2003), the type of event may also influence the development of PTSD. Evidence suggests that PTSD rates are higher among those who have experienced a violent personal assault (e.g., rape, stabbed, shot) compared to other types of trauma such as learning of trauma to others (Breslau, 2009; Breslau et al., 1998; Breslau et al., 2004; Hapke et al., 2006). In a study of cocaine dependent individuals, Najavits and colleagues found that those with PTSD reported significantly more traumatic events than those without PTSD, indicating a dose-response relationship between number of events and PTSD (Najavits et al., 1998). Other researchers have also noted this relationship; however, the maximum number of traumatic events assessed in most studies was relatively low, ranging from two to six (Breslau et al., 1999; Perkonigg et al., 2000; Suliman et al., 2009). Because drug-using populations have high exposure to traumatic events, it is worthwhile to examine the relationship between number of events and PTSD to understand whether or not the risk of developing PTSD increases with each additional trauma or if there is a ceiling effect.
1.2 Purpose
The purpose and significance of the study lies in the establishment of a community-matched baseline for comparisons. Neither cocaine dependence nor trauma are evenly distributed throughout the country, but rather both cocaine dependence and violence are concentrated in neighborhoods. The aforementioned general population studies provide general prevalence rates of trauma and cocaine dependence; however, they may fail to provide a fair comparison. For example, a cocaine dependent subject who lives in a chaotic and socially distressed neighborhood will be compared to a non-cocaine dependent subject who lives in an affluent community. Though many demographic factors can be controlled for in these analyses such as gender, age, educational attainment and poverty, many unmeasured community factors cannot be adequately taken into account. This study seeks to better study the relationship of trauma and PTSD between cocaine dependent individuals recruited from treatment compared to a community-matched baseline group. This study design provides a matching of unmeasured neighborhood factors.
This study of individuals in treatment for cocaine dependence and individuals from their neighborhoods sought to examine factors related to traumatic events and PTSD. Specifically, this unique design allows us to better estimate how cocaine dependent cases differ from neighborhood comparison participants, as previous studies have not included a community-matched sample. Our hypotheses were that cocaine dependent cases would experience more traumatic events than community-based participants and that the risk of PTSD would be elevated by number of traumatic events experienced. To address these hypotheses, the present analyses assessed (1) the prevalence and predictors of traumatic events in cocaine dependent cases compared to community-based participants and (2) the prevalence of PTSD in cocaine dependent cases compared to community-based participants and (3) the predictors of PTSD including number and type of traumas.
2. Methods
2.1 Sample
Data are from the Family Study of Cocaine Dependence, a cross-sectional case-cohort design which included cocaine dependent index cases and community-based comparison participants. The data collection period was from 2001-2005. The Washington University School of Medicine IRB approved the protocol and written, informed consent was obtained from all participants.
Cocaine dependent cases were recruited from alcohol and drug treatment centers, including publicly and privately funded inpatient and outpatient facilities in the city of St. Louis and surrounding counties in Missouri. Eligible cases met criteria for DSM-IV cocaine dependence, spoke fluent English, and were at least 18 years of age. Because this was initially designed as a family-based study, cocaine dependent cases were also required to have a full sibling within five years of their age who was willing to participate. To increase the number of complete sibling pairs, cocaine dependent cases were interviewed only after their siblings participated. Response rates were calculated among eligible participants only, which excludes individuals who did not have a sibling participate. Of the eligible cocaine dependent cases, 77.1% participated. Non-participation was due to inability to locate a subject after initial contact (58.7%), subject refusal (20.3%) and other miscellaneous reasons (21%).
One to one matching to cocaine dependent cases based on year of birth (within 1 year), gender, ethnicity, and neighborhood (using zip code) was employed to recruit community-based comparison participants. Potential participants were identified through the Missouri Family Registry maintained by Washington University in St. Louis for research purposes. This registry includes all Missouri residents who have a driver’s license or state identification card (i.e., non-drivers). Individuals were sent a letter describing the study, followed by a phone call inviting them to participate. Year of birth, gender, and ethnicity were confirmed during telephone screening. The community-based individuals were also required to have a full sibling within five years of their age who was willing to participate. Eighty percent of screened and eligible community recruited individuals participated. Substance dependence and other psychiatric disorders were not exclusionary criteria for community-based participants.
Community-based participants were matched on all four criteria (i.e., year of birth, gender, ethnicity, and zip code) for 96.5% of cocaine dependent cases. The current analyses included only matched cocaine dependent cases and community-based participants. The total sample comprised 918 participants: 459 cocaine dependent cases and 459 community-based comparison participants. Sibling data were not included in these analyses because the focus of these analyses was on the case-community cohort design rather than familial transmission.
2.2 Assessment
All participants completed the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA) with an expanded assessment of cocaine dependence. When administered by trained interviewers, the SSAGA has good reliability in assessing substance abuse and dependence and other psychiatric disorders (Bucholz et al., 1994; Bucholz et al., 1995). A module from the Diagnostic Interview Schedule for DSM-IV (DIS-IV), a structured assessment that evaluated the presence or absence of psychiatric disorders according to the DSM-IV criteria (American Psychiatric, 2000; Robins et al., 2000) was used to evaluate PTSD. A history of fifteen specific traumatic events were queried including rape or sexual assault, assaultive violence (e.g., shot, stabbed), witnessing trauma to others, and non-violent trauma (e.g., serious accident, sudden death of a loved one). The traumatic events were assessed using closed-ended questions (e.g., Have you ever been raped or sexually assaulted?) with nominal response options (i.e., Yes or No). Participants were asked to select the most distressing event and were subsequently evaluated for symptoms of PTSD. A diagnosis of PTSD was dependent on Criterion A, which required intense fear, helplessness, or horror in association with the most distressing event. Interview data was checked for consistency by a senior editor and entered into a computerized data file. Lifetime psychiatric diagnoses were made by a computer algorithm that analyzed responses to the interview using DSM-IV criteria (American Psychiatric, 2000).
2.3 Analyses
The purpose of the analyses was to compare lifetime prevalence of traumatic events and PTSD between the cocaine dependent cases recruited from treatment and the community-based participants. We also examined lifetime prevalence of PTSD among those who have experienced a traumatic event (i.e., conditional risk for PTSD). Analyses were conducted separately for males and females because of the known gender differences in rates of drug dependence, exposure to violence, and PTSD (Breslau, 2009; Compton et al., 2005; Kandel et al., 1997). The prevalence rate ratio (PRR) was calculated to compare lifetime prevalence between the cases and community-based participants (Rothman and Greenland, 1998; Zocchetti et al., 1995). There was no correction for multiple testing. In addition, regression analyses were performed to assess the predictors of conditional risk for PTSD and number of traumatic events, whereby number of events refers to the 15 different types of events queried. All analyses were performed using the Statistical Package for the Social Sciences (SPSS, 2008).
3. Results
3.1 Sample characteristics
Demographic information for both groups is presented in Table 1. By design, all cases were cocaine dependent. Because substance dependence was not an exclusionary criterion for recruitment of community-based participants, 30.1% of community-based participants were dependent on at least one illicit drug and 19% of the community-based sample was cocaine dependent. Cocaine dependent cases recruited from treatment were significantly more likely to be dependent across all the queried substances (e.g., tobacco, alcohol, cocaine, marijuana, etc.) compared to community-based participants. For additional detail about the rates of drug use and dependence in this sample see Bierut et al. (2008). In addition, cocaine dependent cases recruited from treatment centers were significantly more likely to have lower income, be unemployed, have less education, and be currently unmarried compared to the community-based comparison participants.
Table 1. Demographics.
| Cocaine Dependent Cases (N= 459) |
Community-Based Comparisons (N=459) |
|
|---|---|---|
| Sex, % | ||
| Male | 47.1 | 47.1 |
| Female | 52.9 | 52.9 |
| Race, % | ||
| Black | 50.3 | 50.3 |
| White | 49.7 | 49.7 |
| Age, mean (SD), y | 35.9 (8.7) | 36.9 (8.9) |
| Birth cohort, % | ||
| Before 1961 | 30.7 | 30.1 |
| 1961 - 1968 | 34.9 | 34.9 |
| After 1968 | 34.4 | 35.1 |
| Marital status, % * | ||
| Married/Widowed | 13.5 | 39.7 |
| Separated/Divorced | 34.0 | 20.0 |
| Never married | 52.5 | 40.3 |
| Education, % * | ||
| < High School | 26.6 | 8.1 |
| GED / High School | 54.7 | 47.5 |
| Some College | 14.2 | 16.3 |
| College or Higher | 4.5 | 28.1 |
| # years completed, mean (SD) * | 11.7 (2.0) | 13.6 (2.2) |
| Employment, % * | ||
| Full-time | 25.8 | 59.3 |
| Part-time | 11.6 | 13.1 |
| Disabled | 10.7 | 6.5 |
| Unemployed | 44.3 | 11.3 |
| Other ** | 7.6 | 9.8 |
| Income, % * | ||
| < $10,000 | 40.5 | 12.2 |
| $10,000 - $29,999 | 25.9 | 20.0 |
| $30,00 - $49,999 | 11.5 | 24.0 |
| ≥ $50,000 | 13.3 | 40.7 |
| Unknown or refused | 8.7 | 3.1 |
| Lifetime Dependence, % | ||
| Tobacco * | 75.6 | 31.4 |
| Alcohol * | 71.2 | 29.4 |
| Marijuana * | 47.9 | 18.3 |
| Cocaine * | 100.0 | 19.0 |
| Opiates * | 24.2 | 3.7 |
| Other † * | 38.8 | 8.5 |
| Any Dependence | 100.0 | 50.3 |
Significant difference between cases and community comparisons, p < .05
Includes homemaker, student, and retired
Other includes stimulants, sedatives, PCP, hallucinogens, & other drugs
3.2 Comparisons between cases and community-based participants of traumatic events
Compared to the community-based group, cocaine dependent cases recruited from treatment were more likely to experience all queried assaultive and violent events as well as witnessing someone injured or killed (see Table 2). Being raped or sexually assaulted was significantly more common in cocaine dependent women recruited from treatment versus the community-based women (58.4% v. 32.5%, respectively). Both the cocaine dependent men and women recruited from treatment were more likely to experience a serious accident than the community-based participants. In contrast, experiencing non-violent trauma (e.g., natural disaster, being exposed to dangerous materials) and other traumatic events was, in general, similar in cocaine-dependent cases and community-based participants.
Table 2. Lifetime Prevalence of Traumatic Events.
| MEN | Case (n=216) |
Community (n=216) |
PRR (95% CI) | Non-Dep Comm (n=157) |
PRR (95% CI) (compared to cases) |
|---|---|---|---|---|---|
| Rape or Sexual Assault | 11.6 | 8.3 | 1.40 (0.79-2.49) | 6.4 | 1.81 (0.90-3.66) |
| Other Assaultive Violence | 80.6 | 58.8 | 1.37 (1.20-1.56) | 49.7 | 1.62 (1.37-1.92) |
| Threatened with weapon | 75.0 | 52.3 | 1.43 (1.24-1.66) | 42.7 | 1.76 (1.44-2.14) |
| Shot | 19.4 | 8.8 | 2.20 (1.33-3.66) | 3.8 | 5.11 (2.23-11.71) |
| Stabbed | 26.4 | 13.4 | 1.97 (1.31-2.96) | 7.0 | 3.77 (2.05-6.95) |
| Mugged/Robbed | 51.9 | 36.6 | 1.42 (1.14-1.76) | 28.7 | 1.81 (1.37-2.39) |
| Captive/Tortured/Kidnapped | 4.6 | 1.4 | 3.29 (0.92-11.79) | 0.6 | 7.67 (0.89-65.69) |
| Witnessing Trauma to Others | 65.3 | 55.1 | 1.19 (1.02-1.38) | 47.1 | 1.39 (1.14-1.68) |
| Seen Someone Injured | 61.6 | 50.0 | 1.23 (1.04-1.46) | 42.7 | 1.44 (1.17-1.78) |
| Seen Someone Killed | 46.8 | 31.5 | 1.49 (1.17-1.89) | 21.0 | 2.23 (1.59-3.12) |
| Non-violent Trauma | 83.3 | 77.8 | 1.07 (0.98-1.18) | 73.9 | 1.13 (1.01-1.26) |
| Serious Accident | 41.7 | 24.5 | 1.70 (1.28-2.26) | 22.9 | 1.82 (1.31-2.53) |
| Discovered dead body | 21.3 | 14.8 | 1.44 (0.96-2.17) | 11.5 | 1.85 (1.12-3.06) |
| Natural Disaster | 22.7 | 23.1 | 0.98 (0.70-1.39) | 25.5 | 0.89 (0.62-1.28) |
| Dangerous Materials | 7.4 | 7.4 | 1.00 (0.51-1.95) | 8.3 | 0.89 (0.44-1.80) |
| Serious Illness | 7.9 | 3.2 | 2.47 (1.04-5.86) | 2.5 | 3.16 (1.07-9.31) |
| Sudden Death of loved One | 71.8 | 64.8 | 1.11 (0.97-1.26) | 60.5 | 1.19 (1.02-1.38) |
| Other Trauma | 19.0 | 18.5 | 1.03 (0.69-1.52) | 17.2 | 1.10 (0.71-1.72) |
|
| |||||
| Number of traumas, mean (SD) | 4.89 (2.91) | 3.59 (2.64) | F=23.67 (1), p<.001 | 3.01 (2.38) | F=43.99 (1), p<.001 |
| WOMEN | Case (n=243) |
Community (n=243) |
PRR (95% CI) | Non-Dep Comm (n=215) |
PRR (95% CI) (compared to cases) |
|---|---|---|---|---|---|
| Rape or Sexual Assault | 58.4 | 32.5 | 1.80 (1.46-2.22) | 29.3 | 1.99 (1.58-2.52) |
| Other Assaultive Violence | 65.0 | 36.2 | 1.80 (1.48-2.17) | 32.1 | 2.02 (1.63-2.51) |
| Threatened with weapon | 53.9 | 26.7 | 2.02 (1.59-2.56) | 23.3 | 2.31 (1.77-3.03) |
| Shot | 7.0 | 1.2 | 5.83 (1.70-20.01) | 1.4 | 5.00 (1.49-16.83) |
| Stabbed | 15.2 | 2.9 | 5.24 (2.38-11.53) | 1.4 | 10.86 (3.40-34.71) |
| Mugged/Robbed | 37.4 | 21.4 | 1.75 (1.31-2.34) | 18.1 | 2.07 (1.49-2.87) |
| Captive/Tortured/Kidnapped | 23.5 | 8.2 | 2.87 (1.78-4.62) | 7 | 3.36 (1.96-5.74) |
| Witnessing Trauma to Others | 46.9 | 29.6 | 1.58 (1.25-2.01) | 27.0 | 1.74 (1.34-2.25) |
| Seen Someone Injured | 43.2 | 27.2 | 1.59 (1.24-2.04) | 24.7 | 1.75 (1.33-2.30) |
| Seen Someone Killed | 26.7 | 14.4 | 1.85 (1.28-2.69) | 11.2 | 2.38 (1.55-3.66) |
| Non-violent Trauma | 81.1 | 73.3 | 1.11 (1.00-1.22) | 72.6 | 1.12 (1.01-1.24) |
| Serious Accident | 30.5 | 17.3 | 1.76 (1.26-2.46) | 15.8 | 1.93 (1.34-2.77) |
| Discovered dead body | 16.0 | 7.0 | 2.29 (1.33-3.93) | 5.1 | 3.14 (1.65-5.97) |
| Natural Disaster | 21.4 | 21.0 | 1.02 (0.72-1.44) | 20.0 | 1.07 (0.75-1.53) |
| Dangerous Materials | 2.5 | 1.6 | 1.56 (0.44-5.50) | 1.4 | 1.79 (0.45-7.03) |
| Serious Illness | 11.9 | 4.5 | 2.64 (1.35-5.19) | 3.7 | 3.22 (1.50-6.89) |
| Sudden Death of loved One | 71.6 | 62.6 | 1.14 (1.01-1.30) | 61.9 | 1.16 (1.01-1.32) |
| Other Trauma | 13.2 | 14.0 | 0.94 (0.60-1.48) | 14.4 | 0.92 (0.58-1.45) |
|
| |||||
| Number of traumas, mean (SD) | 4.51 (2.96) | 2.68 (2.25) | F=58.65 (1), p<.001 | 2.44 (2.06) | F=73.54 (1), p<.001 |
“Case” refers to cocaine-dependent individuals recruited from treatment centers; “Community” refers to matched community-based comparisons; “Non-Dep Comm” refers to non-cocaine dependent matched community-based comparisons
Most of the cocaine dependent cases recruited from treatment and community-based participants experienced traumatic events. Ninety-four percent of cocaine dependent cases and 87% of community-based participants experienced at least one distressing event. Furthermore, it was uncommon for participants to suffer only one incident (13.0%). Though both groups were exposed to high rates of traumatic experiences, cocaine dependent cases recruited from treatment endured significantly more distressing events than the community-based participants (4.64 vs. 3.08, respectively, p < .001). Twenty-six percent of cocaine dependent cases from treatment experienced seven or more distinct traumatic events compared to only 11% of community-based comparison participants (p < .001).
By design, participants in the community-based sample were not excluded based on drug dependence and subsequently 19% (n=87) of these individuals met criteria for cocaine dependence. In addition, 71.3% of the cocaine dependent community-based sample (n=62) sought chemical dependency treatment. In part, the high prevalence of traumatic events experienced by the community cohort may be related to these cocaine dependent community participants. To address this, analyses were repeated with the community-based cohort separated into two groups: cocaine dependent and non-cocaine dependent. The cocaine dependent community-based individuals reported traumatic event rates similar to the cocaine dependent individuals recruited from treatment centers and there were no statistically significant differences between the groups. Trauma exposure rates in the non-cocaine dependent community-based participants decreased; however, the comparisons to the cases were similar to those seen before (see Table 2).
We conducted a negative binomial regression to examine predictors of number of traumatic events. Group status (cocaine dependent cases or community-based cohort), gender, ethnicity, education and income were entered as categorical predictors. Group status (β = .385, p < .001), gender (β = .189, p < .001), ethnicity (β = .302, p < .001), and income (β = .142, p < .05) were significant predictors such that cocaine dependent cases, males, African Americans, and lower income participants were associated with a higher number of traumatic events. Analyses were repeated with cocaine dependence as a predictor rather than group status. Cocaine dependence (β = .500, p < .001) and African American ethnicity (β = .260, p <.01) significantly predicted a higher number of events, whereas gender and income were no longer significant.
3.3 Prevalence and Predictors of PTSD
Although participants may have reported exposure to multiple types of trauma, the design of the PTSD assessment module anchored the diagnosis of PTSD to one event that participants reported as their most distressing. Table 3 presents the index traumas that the participants reported as most distressing. The two most commonly reported events were sudden death of a loved one (31.4%) and rape or sexual assault (20.1%).
Table 3. Prevalence of Most Distressing Event among subjects with PTSD.
| Rape or Sexual Assault | 20.1 |
| Other Assaultive Violence | 15.0 |
| Threatened with weapon | 3.8 |
| Shot | 3.1 |
| Stabbed | 1.9 |
| Mugged/Robbed | 3.1 |
| Captive/Tortured/Kidnapped | 3.1 |
| Witnessing Trauma to Others | 11.4 |
| Seen Someone Injured | 1.3 |
| Seen Someone Killed | 10.1 |
| Non-violent Trauma | 40.2 |
| Serious Accident | 3.8 |
| Discovered dead body | 4.4 |
| Natural Disaster | 0.6 |
| Dangerous Materials | 0.0 |
| Serious Illness | 0.0 |
| Sudden Death of loved One | 31.4 |
| Other Trauma | 13.2 |
The lifetime prevalence of PTSD for all participants was high (see Table 4). Cocaine dependent cases recruited from treatment were at almost double the risk for PTSD compared to the community-based participants (22.4% and 12.2%, respectively, p < .001). Repeating the analysis after dividing the community-based cohort into those with and without cocaine dependence showed that there were no statistical differences in the lifetime prevalence of PTSD between the cocaine dependent cases recruited from treatment and the cocaine dependent participants recruited from the community. The contrast between the cocaine dependent cases recruited from treatment and the community-based sample without cocaine dependence increased.
Table 4. Lifetime Prevalence of PTSD.
| MEN | Case (n=216) |
Community (n=216) |
PRR (95% CI) | Non-Dep Comm (n=157) |
PRR (95% CI) (compared to cases) |
|---|---|---|---|---|---|
| Overall Rate of PTSD | 16.2 | 9.3 | 1.74 (1.04-2.92) | 7.6 | 2.13 (1.14-3.98) |
| Conditional Rate of PTSD * | 17.2 | 10.6 | 1.62 (1.00-2.64) | 9.0 | 1.91 (1.07-3.40) |
| WOMEN | Case (n=243) |
Community (n=243) |
PRR (95% CI) | Non-Dep Comm (n=215) |
PRR (95% CI) (compared to cases) |
|---|---|---|---|---|---|
| Overall Rate of PTSD | 28.0 | 14.8 | 1.89 (1.32-2.72) | 12.6 | 2.22 (1.48-3.33) |
| Conditional Rate of PTSD ** | 30.4 | 17.1 | 1.78 (1.27-2.49) | 14.8 | 2.05 (1.41-2.98) |
Conditional analysis for men included 203 cases and 189 community-based subjects
Conditional analysis for women included 224 cases and 210 community-based subjects
Because PTSD is a diagnosis based on experiencing a traumatic event, the high prevalence is related to the higher baseline rates of trauma and violence suffered by these participants. When examining the lifetime prevalence of PTSD amongst those who have experienced a traumatic event (i.e., conditional risk of PTSD), the prevalence in both groups increases: cocaine dependent cases 24%, community-based individuals 14%. Of the entire sample, more than 19% reported conditional PTSD. Though men were more likely to be exposed to different types of trauma, women were more likely to meet criteria for conditional risk of PTSD (cases W: 30.2% v. M: 17.2%; community-based W: 17.1% v. M: 10.6%).
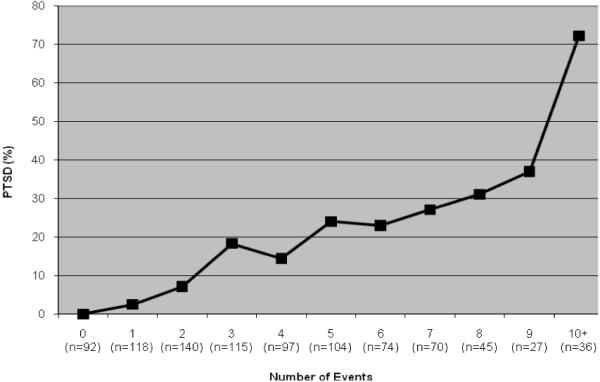
To better understand the increased lifetime prevalence of PTSD and conditional risk of PTSD among the cocaine dependent cases recruited from treatment and the community-based cohort, further analyses were undertaken on predictors of PTSD. Figure 1 displays the percentage of all participants who met criteria for PTSD given the number of traumatic events experienced in their lifetime. There was a stepwise increase in the reporting of a diagnosis of PTSD as the number of traumatic events increase. Surprisingly, even after six and seven distinct traumas, the prevalence of PTSD did not plateau but rather continued to steadily increase. The elevated prevalence of PTSD in this sample may reflect the high number of different types of trauma that this population experienced. To further examine this, a logistic regression analysis was conducted using group status (cases or community-based cohort), gender, ethnicity, education, income, and number of traumatic events as predictors for conditional risk of PTSD. Gender and number of traumatic events were the only significant predictors of PTSD (female gender: OR=2.72, 95%CI: 1.79-4.13; number of traumas: OR=1.39, 95%CI: 1.28-1.50).
Figure 1. Prevalence of Lifetime PTSD by Number of Traumatic Events.
Finally, in addition to number of traumas, we also examined type of trauma as a predictor of the conditional risk of PTSD. We conducted a second logistic regression using the same demographic predictors mentioned above (i.e., group status, gender, ethnicity, education, income) and also included 5 different categories of trauma: rape /sexual assault, other assaultive violence, witnessing trauma to others, non-violent trauma, and other trauma. An individual could report any or all of these different traumatic experiences. In this multivariate analysis, the prediction of PTSD differed by exposure to the different types of traumatic experiences. Those who experienced either sexual assault or other assaultive violence were two and a half times more likely to have PTSD than those who did not experience these types of trauma (see Table 5). Witnessing trauma to others, experiencing other trauma, and being female were also significant predictors of conditional risk of PTSD.
Table 5. Multivariate Logistic Regression: Predictors of Conditional PTSD.
| OR | 95% CI | |
|---|---|---|
| Male | 0.53* | 0.33-0.86 |
| Female | 1.00 | |
|
| ||
| Case | 1.10 | 0.70-1.75 |
| Community | 1.00 | |
|
| ||
| African-American | 1.22 | 0.79-1.90 |
| European-American | 1.00 | |
|
| ||
| Education | ||
| < High School | 2.16 | 0.98-4.79 |
| High School | 1.55 | .072-3.34 |
| Some College | 1.54 | 0.66-3.59 |
| 4 year College | 1.00 | |
|
| ||
| Income | ||
| <10,000 | 0.92 | 0.48-1.78 |
| 10,000-29,999 | 1.14 | 0.62-2.12 |
| 30,000-49,999 | 0.93 | 0.48-1.80 |
| > 50,000 | 1.00 | |
|
| ||
| Rape or Sexual Assault | 2.87** | 1.83-4.51 |
| 1.00 | ||
|
| ||
| Other Assaultive Violence | 2.59** | 1.53-4.38 |
| 1.00 | ||
|
| ||
| Witnessing Trauma to Others |
1.78* | 1.15-2.76 |
| 1.00 | ||
|
| ||
| Non-violent Trauma | 1.94 | 0.95-3.95 |
| 1.00 | ||
|
| ||
| Other Trauma | 1.78* | 1.10-2.88 |
| 1.00 | ||
Statistically significant difference, p < 0.05
p<0.001.
4. Discussion
This study is unique in its use of a case-cohort sampling design. Cases were cocaine dependent participants recruited from chemical dependency treatment settings and this group was compared to a cohort recruited from the same community. We examined the types of traumatic events and risk of PTSD after experiencing a traumatic event (conditional risk of PTSD) in cocaine dependent cases and community-based cohort. Overall, the pattern of traumatic events in this study is consistent with previous reports (Breslau et al., 1998; Kessler et al., 1995). What differs is the magnitude of the violence and traumatic events experienced by both cocaine dependent cases recruited from treatment and individuals in the community-based cohort.
First, cocaine dependent cases recruited in chemical dependency treatment centers reported experiencing alarmingly high rates of violent and traumatic events. Nearly 94% of cocaine dependent cases recruited in treatment endured at least one traumatic event. Fifty-eight percent of female cocaine dependent cases recruited in treatment reported being raped or sexually assaulted, 54% had been threatened with a weapon, and nearly 27% witnessed someone being killed. Of the male cocaine dependent cases recruited in treatment, 75% were threatened with a weapon, 19% had been shot, and almost 47% witnessed someone being killed. These high levels of traumatic events are greater than noted in previous studies on drug users (Breslau et al., 1998; Cottler et al., 2001; Johnson et al., 2003; Johnson et al., 2006; Wasserman et al., 1997). One reason for this may be that we had strict inclusion criteria that participants were both cocaine dependent and in treatment. In addition, the high prevalence of trauma in this sample supports evidence that dependence of “hard” drugs, like cocaine, is associated with an increased risk of trauma exposure. We do not know the timing of cocaine dependence and trauma nor can we assume causality. However, what is clear is that cocaine dependence and exposure to traumatic events are strongly correlated.
Secondly, compared to other population studies, the community-based comparison participants experienced highly elevated rates of traumatic events (Breslau et al., 1998; Kessler et al., 1995; Koenen et al., 2002; Tjaden, 2006). The community-based participants were recruited from the same zip codes where cocaine dependent index cases lived and matched based on year of birth, gender, and ethnicity. Eighty-seven percent of the men and women recruited from the community suffered at least one traumatic event, which is similar to the 1996 Detroit Area Survey of Trauma, but almost double that reported in the National Comorbidity Survey (Breslau et al., 1998; Kessler et al., 1995). Although the overall prevalence of traumatic events was similar to the Detroit Area Survey of Trauma, our community-based comparison participants experienced much higher levels of assault and violent events (Breslau et al., 1998). For example, Breslau et al. (1998) reported that 5.4% of respondents were raped and 6.2% were sexually assaulted, whereas 21% of our community sample reported being raped/sexually assaulted.
In the current study, drug use and dependence were not exclusionary criteria and community-based participants were recruited regardless of substance dependence. This is a unique study design and its purpose is to allow us to better compare cocaine dependent cases with individuals from their communities. Large scale nationally representative studies can compare cocaine dependent participants and non-dependent individuals; however, comparisons of participants within neighborhoods are not possible. By contrasting participants from the same neighborhoods, we may reduce or eliminate the influence of unmeasured neighborhood environmental features on the relationship between cocaine dependence, traumatic events, and PTSD.
In our community-based group, we found high lifetime prevalence of substance dependent individuals living in the same area where the cocaine dependent cases recruited from treatment live. Subsequently, 19% of our community-based participants were cocaine dependent. Even after excluding these individuals from analyses, we found that trauma and PTSD rates in the community-based group dropped slightly, but remained higher than rates reported in previous studies. This has important implications for the community as a whole. Other community members who do not use drugs are being exposed to violence such as shootings and robberies, which may increase their risk of developing PTSD. Our study highlights not only the high rates of trauma and PTSD in cocaine dependent individuals but also the high prevalence of violence in their neighborhoods.
This study yields additional evidence for the increased risk of PTSD associated with drug dependence. Other investigators have noted rates of lifetime PTSD among substance abusers ranging from 20% to 52% (Back et al., 2000; Johnson et al., 2006; Reynolds et al., 2005; Wasserman et al., 1997). Our current study shows 24% of the individuals recruited from treatment with cocaine dependence who experienced a traumatic event met criteria for PTSD. This high prevalence is a function of the number and violent nature of traumatic events experienced by these individuals. Najavits and colleagues (1998) reported individuals with PTSD endorsing significantly more traumatic experiences than those without PTSD and our study confirms this finding. Further, evidence suggests that experiencing assaultive violence such as being raped, stabbed, or shot, is associated with higher rates of PTSD (Breslau et al., 2004; Hapke et al., 2006). Thus, the cumulative violent experiences of cocaine dependent cases are likely contributing to a higher prevalence of PTSD and possibly other psychological disorders. This has important treatment implications for treating those with comorbid PTSD and substance dependence. In addition to treating both disorders simultaneously, treatment may be more effective if patients were educated about the relationship between drug use and interpersonal violence, as described by Hien et al. (2010).
Although cocaine dependent cases had a higher prevalence of PTSD, it is important to note that the community-based participants also had alarmingly high rates compared to the general population. Among individuals who experienced any traumatic event, 14% of our community-based participants reported PTSD compared to 7 - 9% reported in other population-based studies (Breslau et al., 1998; Breslau et al., 2004; Hapke et al., 2006; Kessler et al., 1995). Because our community-based participants experienced a high number of traumatic events, particularly violent events, it makes sense that they would also have elevated prevalence of PTSD. It is also possible that other neighborhood or community level factors (e.g., social support) could influence the risk of PTSD after experiencing trauma; however, these variables were not directly measured in our study.
There are several limitations to be considered. First, this represents recruitment from a single metropolitan area. Second, it is important to note that this is a case-cohort study, not a case-control study. The purpose of the community-based cohort is not necessarily to compare dependent and non-dependent individuals, but rather to compare cocaine dependent cases recruited from treatment centers with people in their own neighborhoods. Thirdly, data are not available on how many times each subject experienced a traumatic event and subsequently we cannot determine if a reported traumatic event was a single incident versus a series of events (e.g., rape vs. ongoing sexual abuse). In addition, some traumatic events, such as domestic violence, were not directly queried using the standardized assessment. Also, PTSD rates may have been underestimated, given current debate on the inclusion of criterion A in PTSD diagnoses (Kilpatrick et al., 2009). Finally, since the assessment was not designed to examine the temporal order of trauma exposure and drug use, it is unclear whether traumatic events occurred before or after the development of substance dependence. Additionally, data are not available on whether traumatic events occurred during the use of cocaine or other substances.
In summary, individuals in treatment for cocaine dependence have experienced a high level of violent traumatic events and many report a lifetime history of PTSD. The neighbors of cocaine dependent cases also have an elevated risk for experiencing traumatic events which in turn elevated their risk for PTSD. Experiencing multiple, violent traumas increases the risk of PTSD, regardless of cocaine dependence. The high prevalence of trauma seen in our community-based participants emphasizes the role of violence in the neighborhood and the connections among drug dependence, trauma exposure, and PTSD. Drug dependent individuals who return to the same communities with a high baseline rate of cocaine dependence and violence after treatment may be more likely to relapse, which perpetuates the cycle of violence and drugs. Further, drug dependence is not only problematic for the user, but may also increase the risk of trauma exposure in individuals who live in the same neighborhoods. Recognition of high rates of violence and assault experienced by individuals in treatment for cocaine dependence and members from their communities are needed to better inform health plans and public policies for the prevention, reduction, and treatment of cocaine dependence and the consequences of exposure to traumatic and violent events.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric, A. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Back S, Dansky BS, Coffey SF, Saladin ME, Sonne S, Brady KT. Cocaine dependence with and without post-traumatic stress disorder: a comparison of substance use, trauma history and psychiatric comorbidityAm. J Addict. 2000;9:51–62. doi: 10.1080/10550490050172227. [DOI] [PubMed] [Google Scholar]
- Bell DC, Carlson JW, Richard AJ. The social ecology of drug use: a factor analysis of an urban environment. Subst Use Misuse. 1998;33:2201–2217. doi: 10.3109/10826089809056255. [DOI] [PubMed] [Google Scholar]
- Bierut LB, Strickland JR, Thompson JR, Afful SE, Cottler LB. Drug use and dependence in cocaine dependent subjects, community-based individuals, and their siblings. Drug Alcohol Depend. 2008;95:14–22. doi: 10.1016/j.drugalcdep.2007.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma Violence Abus. 2009;10:198–210. doi: 10.1177/1524838009334448. [DOI] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry. 1999;156:902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Breslau N, Wilcox HC, Storr CL, Lucia VC, Anthony JC. Trauma exposure and posttraumatic stress disorder: a study of youths in urban America. J Urban Health. 2004;81:530–544. doi: 10.1093/jurban/jth138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown P, Wolfe J. Substance abuse and post-traumatic stress disorder comorbidity. Drug Alcohol Depend. 1994;35:51–59. doi: 10.1016/0376-8716(94)90110-4. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, Jr., Reich T, Schmidt I, Schuckit MA. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. J Stud Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Hesselbrock VM, Shayka JJ, Nurnberger JI, Jr., Schuckit MA, Schmidt I, Reich T. Reliability of individual diagnostic criterion items for psychoactive substance dependence and the impact on diagnosis. J Stud Alcohol. 1995;56:500–505. doi: 10.15288/jsa.1995.56.500. [DOI] [PubMed] [Google Scholar]
- Chilcoat HD, Breslau N. Investigations of causal pathways between PTSD and drug use disorders. Addict Behav. 1998a;23:827–840. doi: 10.1016/s0306-4603(98)00069-0. [DOI] [PubMed] [Google Scholar]
- Chilcoat HD, Breslau N. Posttraumatic stress disorder and drug disorders: testing causal pathways. Arch of Gen Psychiatry. 1998b;55:913–917. doi: 10.1001/archpsyc.55.10.913. [DOI] [PubMed] [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2005;66:677–685. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- Cottler L, Nishith P, Compton W.r. Gender differences in risk factors for trauma exposure and post-traumatic stress disorder among inner-city drug abusers in and out of treatment. Compr Psychiatry. 2001;42:111–117. doi: 10.1053/comp.2001.21219. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Compton WM, 3rd, Mager D, Spitznagel EL, Janca A. Posttraumatic stress disorder among substance users from the general population. Am J Psychiatry. 1992;149:664–670. doi: 10.1176/ajp.149.5.664. [DOI] [PubMed] [Google Scholar]
- Hapke U, Schumann A, Rumpf HJ, John U, Meyer C. Post-traumatic stress disorder: the role of trauma, pre-existing psychiatric disorders, and gender. Eur Arch Psychiatry Clin Neurosci. 2006;256:299–306. doi: 10.1007/s00406-006-0654-6. [DOI] [PubMed] [Google Scholar]
- Harrison L, Gfroerer J. The intersection of drug use and criminal behavior: Results from the National Household Survey on Drug Abuse. Crime and Delinquency. 1992;34:422–443. [Google Scholar]
- Hien DA, Jiang H, Campbell ANC, Hu M, Miele GM, Cohen LR, Bringham GS, Capstick C, Kulaga A, Robinson J, Suarez-Morales L, Nunes EV. Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analyses from a randomized clinical trial in NIDA’s Clinical Trials Networks. Am J Psychiatry. 2010;167:95–101. doi: 10.1176/appi.ajp.2009.09091261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SD, Cunningham-Williams RM, Cottler LB. A tripartite of HIV-risk for African American women: the intersection of drug use, violence, and depression. Drug Alcohol Depend. 2003;70:169–175. doi: 10.1016/s0376-8716(02)00345-9. [DOI] [PubMed] [Google Scholar]
- Johnson SD, Striley C, Cottler LB. The association of substance use disorders with trauma exposure and PTSD among African American drug users. Addict Behav. 2006;31:2063–2073. doi: 10.1016/j.addbeh.2006.02.007. [DOI] [PubMed] [Google Scholar]
- Kadushin C, Reber E, Saxe L, Livert D. The substance use system: social and neighborhood environments associated with substance use and misuse. Subst Use Misuse. 1998;33:1681–1710. doi: 10.3109/10826089809058950. [DOI] [PubMed] [Google Scholar]
- Kandel D, Chen K, Warner LA, Kessler RC, Grant B. Prevalence and demographic correlates of symptoms of last year dependence on alcohol, nicotine, marijuana and cocaine in the U.S. population. Drug Alcohol Depend. 1997;44:11–29. doi: 10.1016/s0376-8716(96)01315-4. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kilpatrick D, Resnick H, Acierno R. Should PTSD Criterion A be retained? J Trauma Stress. 2009;22:374–383. doi: 10.1002/jts.20436. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Harley R, Lyons MJ, Wolfe J, Simpson JC, Goldberg J, Eisen SA, Tsuang M. A twin registry study of familial and individual risk factors for trauma exposure and posttraumatic stress disorder. J Nerv Ment Dis. 2002;190:209–218. doi: 10.1097/00005053-200204000-00001. [DOI] [PubMed] [Google Scholar]
- Mills K, Lynskey M, Teesson M, Ross J, Darke S. Post-traumatic stress disorder among people with heroin dependence in the Australian treatment outcome study (ATOS): prevalence and correlates. Drug Alcohol Depend. 2005;77:243–249. doi: 10.1016/j.drugalcdep.2004.08.016. [DOI] [PubMed] [Google Scholar]
- Mills KL, Teesson M, Ross J, Peters L. Trauma, PTSD, and substance use disorders: findings from the Australian National Survey of Mental Health and Well-Being. Am J Psychiatry. 2006;163:652–658. doi: 10.1176/ajp.2006.163.4.652. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Gastfriend DR, Barber JP, Reif S, Muenz LR, Blaine J, Frank A, Crits-Christoph P, Thase M, Weiss RD. Cocaine dependence with and without PTSD among subjects in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Am J Psychiatry. 1998;155:214–219. doi: 10.1176/ajp.155.2.214. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Runkel R, Neuner C, Frank AF, Thase ME, Crits-Christoph P, Blaine J. Rates and symptoms of PTSD among cocaine-dependent patients. J Stud Alcohol. 2003;64:601–606. doi: 10.15288/jsa.2003.64.601. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Perkonigg A, Kessler RC, Storz S, Wittchen HU. Traumatic events and post-traumatic stress disorder in the community: prevalence, risk factors and comorbidity. Acta Psychiatr Scand. 2000;101:46–59. doi: 10.1034/j.1600-0447.2000.101001046.x. [DOI] [PubMed] [Google Scholar]
- Petronis KR, Anthony JC. Perceived risk of cocaine use and experience with cocaine: do they cluster within US neighborhoods and cities? Drug Alcohol Depend. 2000;57:183–192. doi: 10.1016/s0376-8716(99)00047-2. [DOI] [PubMed] [Google Scholar]
- Reynolds M, Mezey G, Chapman M, Wheeler M, Drummond C, Baldacchino A. Co-morbid post-traumatic stress disorder in a substance misusing clinical population. Drug Alcohol Depend. 2005;77:251–258. doi: 10.1016/j.drugalcdep.2004.08.017. [DOI] [PubMed] [Google Scholar]
- Robins LN, Cottler LB, Bucholz KK, Compton WM, North CS, Rourke KM. [Accessed on May 26, 2010];Diagnostic Interview Schedule for the DSM-IV (DIS-IV) 2000 http://epi.wustl.edu/dis/dishome.htm.
- Rothman KJ, Greenland S. Modern Epidemiology. Lippincott-Raven; Philadelphia: 1998. [Google Scholar]
- SPSS for Windows, Rel. 16.0.2. SPSS Inc.; Chicago: 2008. [Google Scholar]
- Suliman S, Mkabile S, Fincham D, Ahmed R, Stein D, Seedat S. Cumulative effect of multiple trauma on symptoms of posttraumatic stress disorder, anxiety, and depression in adolescents. Compr Psychiatry. 2009;50:121–127. doi: 10.1016/j.comppsych.2008.06.006. [DOI] [PubMed] [Google Scholar]
- Tjaden PTN. US Department of Justice, National Institute of Justice; 2006. Extent, Nature, and Consequences of Rape Victimization: Findings from the National Violence Against Women Survey. [Google Scholar]
- Wasserman DA, Havassy BE, Boles SM. Traumatic events and post-traumatic stress disorder in cocaine users entering private treatment. Drug Alcohol Depend. 1997;46:1–8. doi: 10.1016/s0376-8716(97)00048-3. [DOI] [PubMed] [Google Scholar]
- Zocchetti C, Consonni D, Bertazzi PA. Estimation of prevalence rate ratios from cross-sectional data. Int J Epidemiol. 1995;24:1064–1067. doi: 10.1093/ije/24.5.1064. [DOI] [PubMed] [Google Scholar]


