Abstract
Using data from a recent randomized clinical trial involving juvenile drug court (JDC), youth marijuana use trajectories and the predictors of treatment non-response were examined. Participants were 118 juvenile offenders meeting diagnostic criteria for substance use disorders assigned to JDC and their families. Urine drug screen results were gathered from weekly court visits for 6 months, and youth reported their marijuana use over 12 months. Semiparametric mixture modeling jointly estimated and classified trajectories of both marijuana use indices. Youth were classified into responder versus non-responder trajectory groups based on both outcomes. Regression analyses examined pretreatment individual, family, and extrafamilial predictors of non-response. Results indicated that youth whose caregivers reported illegal drug use pretreatment were almost 10 times as likely to be classified into the non-responder trajectory group. No other variable significantly distinguished drug use trajectory groups. Findings have implications for the design of interventions to improve JDC outcomes.
Keywords: juvenile drug court, adolescent substance abuse, trajectory outcomes, treatment non-response
1. Introduction
The growing recognition of the need to address substance abuse among adolescent offender populations (Grisso & Underwood, 2004) combined with the success of adult drug courts (General Accountability Office, 2005) has led to the development and proliferation of juvenile drug courts (JDCs), in which drug treatment services are integrated with intensive judicial oversight (Belenko & Logan, 2003). Approximately 500 JDCs are in operation within the U.S. as of June 2009 (Bureau of Justice Assistance Drug Court Clearing House, 2009), which represents an almost 5-fold increase over the number in operation 10 years earlier (Bureau of Justice Assistance Drug Court Clearing House, 2007). The widespread transport of JDCs across the nation has occurred in spite of relatively limited evidence of their effectiveness. Several recent meta-analyses (Aos, Miller, & Drake, 2006; Shaffer, 2006; Wilson, Mitchell, & MacKenzie, 2006), for example, have found that the average effect sizes for the capacity of JDCs to reduce criminal activity is positive, but relatively small. Yet, as reviewers of substance abuse treatment for adolescents have noted (e.g., Waldron & Turner, 2008), outcomes from any given intervention can vary widely.
The overriding purpose of the present study, therefore, is to examine the nature of the variability in JDC outcomes in the hope that findings can be used to inform the development of more effective JDC services. Specifically, this study uses data from a rigorous randomized trial of JDC (Henggeler et al., 2006) that was published after the aforementioned meta-analyses. Findings from this clinical trial showed that JDC was more effective than family court at decreasing adolescent substance use over a 12-month period, with effect sizes considerably higher than those reported in the meta-analyses. As noted by Wilson et al. (2006), substance use outcomes are rarely reported in drug court evaluations in spite of their centrality to drug court and well-documented link with crime (Chassin, 2008).
The design of the study is informed by the small extant literature on the predictors of youth substance use treatment responsiveness. In a conceptually similar study, Waldron, Turner, and Ozechowski (2005) evaluated substance use change trajectories for adolescents receiving one of several substance abuse treatments. The investigators identified four different types of change trajectories for marijuana use over an 18 month period: improvers, slow improvers, relapsers, and resistant. Importantly, 25% of the sample was included in the resistant group -- youth who continued heavy marijuana use without showing any reductions throughout the study period. Another 25% of the youth comprised the relapser group -- youth who demonstrated improvements during the initial 4 months but then deteriorated. Other studies of both adolescents and adults have also identified distinct trajectories of substance use following substance abuse treatment, including trajectories reflecting no improvement (Brown, D'Amico, McCarthy, & Tapert, 2001; Chung, Maisto, Cornelius, & Martin, 2004; Xie, Drake, & McHugo, 2006)
In attempting to understand differential treatment response, investigators have examined a range of predictors. Waldron et al. (2005), for example, found that the improver group was generally low in other antisocial behavior at pretreatment, and that the relapsers were generally high in depression. Consistent with the broader child and adolescent treatment outcome literature (e.g., Reyno & McGrath, 2006; Silverman, Pina, & Viswesvaran, 2008), Williams and Chang (2000) concluded in their review that pre-treatment variables associated with better outcomes following adolescent substance abuse treatment fall within individual, family, and peer domains. Across a range of individual and family based treatments, the most consistent predictors included severity of pretreatment substance use and parent and peer related variables.
In sum, this study aims to identify trajectory groups for substance abusing juvenile offenders participating in JDC. As in the aforementioned studies of differential treatment response, all youth received substance abuse treatment. Unique to the present study, however, all youth were also enrolled in JDC. The increased structure (e.g., weekly court appearances, specified behavioral demands, and consequences for positive and negative behavior) and oversight (e.g., frequent contact with judge, probation officer, and other court personnel) inherent in JDC might lead to different types of drug use trajectories than observed by Waldron et al. (2005). Similarly, in the context of considerable judicial supervision, perhaps predictors of differential treatment response will emerge that have clear implications for improving the effectiveness of JDC. For example, research on adult offenders suggests that drug court services may have increased efficiency if offenders are matched to the level of judicial supervision based on their level of risk (Marlowe, Festinger, Lee, Dugosh, & Benasutti, 2006). Thus, using data from a recent clinical trial of JDC (Henggeler, et al., 2006), the current investigation identifies trajectories of marijuana use among youth participating in drug court and examines factors associated with trajectory groups.
2. Method
2.1. Design and Procedures
As noted, the present study was conducted using data from youth participating in Henggeler et al. (2006). The purpose of the original study was to evaluate the effectiveness of JDC relative to traditional family court services and to determine whether the inclusion of two evidence-based treatments of adolescent substance abuse (multisystemic therapy [MST] and contingency management [CM]) would enhance JDC outcomes. In the original study, youth were randomly assigned to one of four intervention conditions: Family court with usual community substance abuse services (FC), JDC with usual community substance abuse services (DC), JDC with MST (DC/MST), and JDC with MST and CM (DC/MST-CM). Because of the focus on JDC drug use trajectories, youth in the FC condition were excluded from all analyses.
Assessments were conducted with each youth and his or her caregiver at three points in time: within 72 hours of recruitment into the study (pretreatment); 4 months post-recruitment, corresponding to the average end of MST/MST-CM treatment; and 12 months post-recruitment, corresponding to the average end of JDC. Research assistants administered the assessment battery to families in their homes or in detention facilities for youth in juvenile justice custody. Families were paid $75 for each completed assessment as compensation for their time, and all procedures were approved by the university’s institutional review board.
2.2. Participants
Participants were 118 adolescents recruited from the Department of Juvenile Justice (DJJ), which is the public agency responsible for adjudicating and intervening with juvenile offenders in the community where the study took place (Charleston, South Carolina). All youth met Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV; American Psychiatric Association, 1994) diagnostic criteria for alcohol or drug abuse or dependence. Additional inclusion criteria were (a) age of 12–17 years, (b) residence in Charleston County, and (c) residence with at least one parent figure. Adolescents were excluded if they were already involved in substance abuse treatment or if a family member had already received MST treatment. To enhance generalizability, no youth was excluded due to mental health, physical health, or intellectual difficulties. All families of youth who met inclusion criteria were recruited for study participation by a researcher who obtained informed consent and assent, and the recruitment rate was 98%.
Youth averaged 15.2 years of age (SD = 1.06), and 84% were male. Racial representation reflected that of youth in the juvenile justice system in the study site, with 67% African-American, 31% White, and 2% biracial. Only 13% lived with both biological or adoptive parents, 21% lived with a biological parent and another adult caregiver, 49% lived with a single biological or adoptive parent, and 16% lived with other relatives. Socioeconomically, median family income was in the $10,000-$15,000 range, 37.3% of families were receiving financial assistance, and the median educational status of the primary caregivers was 12th grade. The youth averaged 3.6 arrests (SD = 2.5) prior to study entry, and 43% had received mental health or substance abuse treatment previously. Almost all youth (97.5%) met diagnositc criteria for a cannibis use disorder, while 15.3% met criteria for an alcohol use disorder, 4.2% met criteria for a cocaine use disorder; and 16.9% met criteria for two substance use disorders.
The sample size was considered adequate for this preliminary examination based on power analyses. For logistic regression analyses for a single dichotomous predictor variable with the sample proportion in each category of 50/50, the sample size was sufficient for a power of .80 to detect a difference in event rates of approximately 25%. As the proportion becomes less balanced, the detectable difference in event rate increases, for example, approximately 29% for 70/30 and 45% for 90/10. For a single continuous predictor variable, the sample size was sufficient for power of .80 to detect a difference in event rates of approximately 25%.
2.3. Interventions
All youth were enrolled in JDC and, as part of their JDC participation, approximately one-third also received community substance abuse treatment and two-thirds received evidence-based substance abuse treatment. Please see Henggeler et al. (2006) for additional details about the intervention models.
2.3.1. Juvenile Drug Court
All youth were enrolled in and began drug court interventions immediately after study entry. JDC was held initially once per week, and procedures were typical of those provided in JDCs nationally (National Association of Drug Court Professionals, 1997). Prior to each court appearance, urine drug screens were obtained, and the youth, caregiver, and substance abuse counselor reported on the youth’s behavior during the past week. If the youth’s drug screen was dirty or if negative behavior was reported, sanctions could be imposed. Sanctions varied in intensity and ranged from community service to detention. If the youth’s behavior was positive and he or she provided clean drug screens, the judge rewarded the youth with incentives that also varied in level of intensity (e.g., meal at a fast food restaurant, tickets to a sporting event). The participating JDC used a 3-level system to determine how often a youth’s attendance was required at court (i.e., weekly, biweekly, or monthly), with graduation from one level to the next dependent on clean drug screens and acceptable behavior in other areas. The standard duration of JDC was 12 months. In addition, all youth were supervised via probation or parole, which included a minimum of approximately 2 hr of juvenile justice contact per month for approximately 1 year.
2.3.2. Community Substance Abuse Treatment
In addition to JDC, youth in the DC condition received outpatient alcohol and drug abuse services from the local state-funded alcohol and drug treatment facility. Services typically lasted for 12 weeks and included: 1) group treatment sessions focusing on risk reduction, peer influence, conflict resolution, and anger management (1.5 hr, 4 days a week); 2) individual sessions (once per week); and 3) family group therapy (1.5 hr, 2 days per week). In addition, youth concurrently received 6 weeks (once per week) of a group treatment pertaining to drug selling behavior. The theoretical orientations of these services were cognitive-behavioral and systems theory. The interventions were not manual driven, and selection of material was left to the therapists’ discretion. Services were office-based, with little community outreach. Less intensive services were offered if needed following the completion of the 12-week program.
2.3.3. Evidence-Based Substance Abuse Treatment
MST or MST-CM was provided within the context of JDC. MST is a manualized (Henggeler, Schoenwald, Borduin, Rowland, & Cunningham, 2009) evidence-based treatment that targets a comprehensive set of risk factors with individualized interventions. These interventions integrate empirically based clinical techniques (e.g., family therapy, cognitive-behavioral therapy) into a broad-based ecological framework that addresses relevant risk and protective factors across individual, family, peer, school, and neighborhood domains. Interventions focus on promoting behavioral changes in the youth’s natural ecology by empowering caregivers with skills and resources to address difficulties that arise in raising adolescents. Intensive, standardized, and sustained quality assurance protocols are used to maintain fidelity to the treatment model. Services are delivered via a home-based approach, which facilitates high engagement and low dropout rates. Therapists carry low caseloads (4–5 families per clinician), and services are delivered in home, school, and/or neighborhood settings at times convenient to the family. Therapists are available to respond to clinical problems 24 hours a day, 7 days a week.
Youth and families in the MST-CM condition received full MST treatment plus CM (Budney & Higgins, 1998). CM is a behavioral treatment program that involves: 1) frequent urine analysis and a voucher system that rewards clean screens, 2) functional analysis of drug use, and 3) self-management plans for coping with individual triggers based on functional analysis results. Consistent with MST treatment principles, the youth’s caregivers were closely involved in all aspects of CM (e.g., taking urine samples, administering vouchers, and reinforcing youth’s use of self management plans).
2.4. Marijuana Use Outcome Measures
Marijuana was, by far, the most frequently used and abused substance among participants and, consequently, is the focus of this report. In operationalizing marijuana use, the advantages and disadvantages of both self-report and biological indices were considered per the recommendations of Lennox, Dennis, Scott, and Funk (2005). Although any self-report measure is subject to a variety of biases, a self-report instrument assessing the illegal and stigmitized behavior of substance use is likely to be especially vulnerable to bias. Hence, the validity of self-report substance use measures is often questioned. As objective indicators, biological measures are not subject to these biases and are often considered superior to self-report indices. Although the ability of biological indicators to capture substance use among participants who deny or underreport use presents a clear advantage, such indicators are also limited by the indivudal variation their detection window, and thus may not identify people who admit drug use. In light of these strengths and weaknesses and recent evidence of the usefulness of combining information from self-report and biological measures of substance use as opposed to using either measure alone (Lennox, Dennis, Ives, & White, 2006; Lennox et al., 2005), we elected to examine both urine drug screen and self-reported measures and then combine these indices to form the trajectory groupings as described in the results section.
2.4.1. Urine Drug Screens for Cannabis
Urine drug screens were collected weekly (sometimes at random, other times during appointments) by the therapist before each court appearance The minimum detectable level for cannabis is 50 ng/µl, and the sensitivity is 50%. To avoid the possibility of tampering, same-sex therapists observed urine specimen collection and/or sealed water sources and removed all potential contaminants or adulturants from the collection area. Following standard protocols for the JDC, youth with unexcused absences (e.g., runaway, did not show) and youth who missed court because they had been recently placed in detention were counted as having a positive urine screen for cannabis. Likewise, youth with excused absences (e.g., a GED class) were counted as having negative (i.e., clean) drug screens. Whether or not each youth had a positive cannibis screen was determined for each month. Analysis of urine drug screens was limited to the first 6 months of the study because of excessive missing data after that point (e.g., due to the large percentage of youth terminated from the drug court program).
2.4.2. Self-Reported Marijuana Use
Self-reported substance use was assessed with the Form 90 (Miller, 1991), which is an interview based on time line follow-back methodology. A calendar was first used to highlight important events and then used to record specific quantities and types of substances consumed on each day during the period. This period covered the previous 90 days for each assessment, except for the 4-month assessment, when the period covered every day from the first assessment. The numbers of days of marijuana use was computed for each month over the 12-month study period, except for the time not covered by any assessments (months 5 through 8).
2.5. Predictor Variables
Consistent with the extant literature on differential treatment response for youth, key variables from individual, family, and extrafamilial domains were assessed.
2.5.1. Individual-Level Variables
2.5.1.1. Prestudy marijuana use
The Form 90 was also used to assess the number of days of marijuana use during the 90 days prior to last use before study entry, as pretreatment substance use is a consistent predictor of posttreatment substance use.
2.5.1.2. Arrests
Arrests that occurred before study entry were identified through computerized records maintained by South Carolina DJJ. Because youth as young as 16 years could be charged as adults, adult criminal records were also collected from the South Carolina Law Enforcement Division for youth 16 years of age and older. The range of pretreatment arrests (M = 3.6) was wide (1 to 14) and positively skewed, with fewer and fewer participaints having higher values. To reduce the skeweness and facilitate the examination of associations with other variables, values above 4 were recoded to 4. As such, the prestudy arrest variable has four levels: 1 = one arrest, 2 = two arrests, 3 = three arrests, and 4 = four or more arrests.
2.5.1.3. Anxiety/depression
The Youth Self-Report (YSR; Achenbach, 1990) version of the Child Behavior Checklist was used to obtain youth self-reports of their symptoms. The YSR is one of the best-validated measures of self-reported behavioral functioning for youth aged 11 to 18 years and includes 119 behavior problem items rated on a three-point scale (0 = not true, 1 = somewhat true, 2 = very true). For present purposes, and in light of the aforementioned findings reported by Waldron et al. (2005), the narrow-band anxious/depressed mood T-score was used.
2.5.2. Family-Level Variables
2.5.2.1. Caregiver illegal substance use
Caregivers reported their use of illegal substances on the Personal Experiences Inventory (Winters & Henly, 1989). The PEI is a self-report instrument designed to access alcohol and drug abuse and associated problems. Twelve PEI items that tap the frequency of self-reported substance use for the previous 90 days were used to develop indexes for alcohol, marijuana, and other drug use. Whether or not caregivers endorsed any item pertaining to the use of marijuana or another illegal drug during the 90 days prior to study entry was used to indicate caregiver illegal substance use (0 = no illegal substance use, 1 = some illegal subtance use).
2.5.2.2. Family legal problems
Whether family members other than the youth also had problems with the law was assessed. Specifically, caregiver and youth reports on a family history questionnaire were employed to gather information about whether caregivers, siblings, or other household members had experienced legal problems. First, the name of each of the youth’s siblings, caregivers, and other household members were listed on the family history questionnaire. Youth and primary caregiver were separately asked to indicate whether each of the individuals listed had any history of problems with the law. The family legal problems variable was scored dichotomously, indicating whether or not the item was endorsed by either the caregiver or the youth for any family member (0 = no family members with legal problems, 1 = at least one family member with a legal problem).
2.5.2.3. Parental supervision
Caregiver supervision was measured using four caregiver-report items pertaining to parental knowledge of youth’s whereabouts and activities from the Pittsburgh Youth Study (Loeber, Stouthamer-Loeber, Van Kamen, & Farrington, 1991). A sample item is, “Do your parent(s) know who you are with when you are away from home?” Respondents rated each item using a 3-point rating scale (1 = almost never, 2 = sometimes, 3 = often). Items were summed such that higher scores indicated more parental supervision.
2.5.3. Extrafamilal-Level Variables
2.5.3.1. Peer drug activities
The four-item Peer Drug Activity Scale (Loeber et al. 1991) was used to assess the proportion of the youth’s friends who engaged in various drug related behaviors (e.g., used alcohol, sold drugs) during the previous 90 days. Items were rated using a 5-point scale (from 0 = none of them to 4 = all of them) and were summed so that higher scores indicated higher proportions of friends involved in drug-related activities.
2.5.3.2. School status
Whether or not each youth was in school at study entry was determined by caregiver reported school placement on a demographic questionnaire. Students who had been expelled or had formally dropped out from school without starting any other educational program (e.g., General Education Diploma preparation) were considered not in school. Students who voluntarily did not attend school or whose parents kept them out of school for more than 30 days were also considered not in school. Students who were on school suspension were considered in school. Thus, school status was a dichotomous variable (0 = not in school, 1 = in school).
2.5.3.3. Treatment condition
Whether or not the youth received an evidence-based substance abuse treatment while in JDC was examined. Because Henggeler et al. (2006) found that outcomes for youth in the DC/MST and DC/MST-CM conditions were similar, these two intervention conditions were combined (MST/MST-CM) as the evidence-based condition for all analyses in the present study (0 = community substance abuse treatment, 1 = evidence-based substance abuse treatment).
3. Results
The primary aims of the study were to identify (a) marijuana use trajectories for substance abusing juvenile offenders participating in JDC and (b) pertinent variables associated with the trajectories.
3.1. Identification of Trajectory Groups
Semiparametric growth mixture modeling (SGM) is well-suited for identifying subgroups of individuals with similar substance use trajectories. This data analytic technique avoids ad hoc categorization procedures, which are often biased (Nagin, 1999; 2005), and is more sensitive to the identification of trajectory groups than cluster analysis (Dumenci & Windle, 2001). Like conventional approaches to analyzing individual trajectories, SGM models the relationship between time and an outcome (e.g., marijuana use) using a polynomial function (e.g., linear, quadratic terms). Unlike conventional approaches, however, the coefficients that determine the shape of the trajectory are free to vary across groups. Coefficients derived from the optimal model are used to generate each individual’s predicted probability of membership in each group (i.e., posterior probability), and individuals are identified as belonging to the group based on their maximum posterior probability. A more technical presentation of SGM is available elsewhere (Nagin, 1999; 2005). SGM was implemented in the current study using a customized SAS macro known as Proc Traj (Jones, Nagin, & Roeder, 2001). Proc Traj supports outcome variables that have normal distributions and certain types of non-normal distributions (i.e., logistic and zero-inflated Poisson). Participants with missing observations on the substance use measures were included in the analyses. Proc Traj accommodates such missing data, assuming that missing values are missing completely at random.
The identification of substance use trajectory groups proceeded in two steps. First, models were estimated separately for the urine cannabis and self-report marijuana use outcomes. The optimal number of groups for each outcome was determined by testing models with progressively more groups and comparing fit. The Bayesian information criterion (BIC) was used to evaluate fit, with larger (i.e., less negative) values indicating better fit (Nagin, 1999; 2005). The BIC is a function of a model’s maximum likelihood and favors parsimony (i.e., models with fewer groups). Both the Bayes Factor and the probability that each model was correct were calculated based on the BIC procedures outlined in Nagin (2005). If one model is compared to a second, a large Bayes factor (B12 ≥ 10) provides strong evidence favoring the first model, and a small Bayes factor (B12 ≤ .10) provides strong evidence favoring the second model. For the probability that a model is correct, higher values are favorable, with values of 1.0 indicative of 100% probability that the model is correct. Once the optimal number of groups was identified, nonsignificant higher order parameter estimates were removed and the model was re-estimated. The average posterior probability of membership in each group for those participants assigned to that group was examined to evaluate model adequacy. Values above 0.7 for all groups are considered acceptable (Nagin, 2005).
In the second step, trajectory groups for both measures of marijuana use were jointly estimated in a single model. Specifically, data from both self reports and urine drug screens were used to compute the trajectories for each outcome. The dual model analyzes trajectories of two distinct, but related outcomes, whether they evolve over the same time period or not (Nagin, 2005; Nagin & Tremblay, 1999). Models estimated using the joint trajectory analysis may differ somewhat from those estimated separately because the joint analysis uses information derived from both outcomes in model estimation. This approach was appropriate because we planned to look at the outcomes in a combined fashion. This joint analysis built upon the separate models identified in the first step.
3.1.1. Trajectory Groups for Urine Cannabis Screens
Analysis of urine drug screen results required the use of logistic modeling techniques, as the variable was dichotomous (i.e., 0 = negative screen, 1 = positive screen). Two-, three-, four- and five-group models were estimated. Models were initially estimated with intercept, linear, and quadratic coefficients to describe trajectories in each group. Results indicated that the BIC values decreased for two (BIC = −331.19) to three (BIC = −341.89), four (BIC = −353.21) and five (BIC = −361.46) group models, suggesting that the two-group model was optimal. The Bayes factor for the comparison of each model with the model with one less group was high in all cases (two-group vs. three-group Bayes factor = 6.57E+07; three-group vs. four-group Bayes factor = 1366.49; four-group vs. five-group Bayes factor =156.02), indicating that the model with the smaller number of groups was superior in each comparison. Analyses to determine the probability that each model was correct revealed that the probability that the two-group model was correct was high (probability = 1.00) and the probability that each of the other models was correct was low (all probabilities = 0.00). Thus, the two-group model was retained. Nonsignificant higher order parameter estimates were removed from the two-group model (one at a time) and the model was re-estimated. The average posterior probabilities of membership in each group for those participants assigned to that group were very high for group 1 (M = .93, SD = .14, range = .50 to 1.0) and group 2 (M = .91, SD = .15, range = .51 to 1.0), suggesting that the model corresponds well to the data.
3.1.2. Trajectory Groups for Self-Reported Marijuana Use
Because days of use had a high proportion of zero values, as is frequently the case with count variables, models assuming a normal distribution could not be employed. Thus, the zero-inflated Poisson (ZIP) model appropriate for count data (Atkins & Gallop, 2007) was used. To account for the gap in the months during which self-reported use data were not collected, time was coded to reflect the month beginning at month 0 (0, 1, 2, 3, 9, 10, 11). Two-, three-, four- and five-group models were estimated. Models were initially estimated with intercept, linear, quadratic, and cubic coefficients to describe trajectories in each group. Results indicated that the BIC values increased (became less negative) for two (BIC = −1152.17) to three (BIC = −1081.67) groups. The four- and five-group models did not converge. The Bayes factor reflecting the comparison of the three-group model to the two-group model was extremely low (Bayes factor = 0.00), indicating that the three-group model was superior to the two-group model. Further, comparison to determine the probability that each model was correct revealed that the probability that the two-group model was correct was low (probability = 0.00) and the probability that the three-group model was correct was high (probability = 1.00). Thus, the three-group model was retained. Nonsignificant higher order parameter estimates were removed from the three-group model (one at a time), and the model was re-estimated. The average posterior probabilities of membership in each group for those participants assigned to that group were very high for group 1 (M = .98, SD = .05, range = .74 to 1.0), group 2 (M = .94, SD = .11, range = .62 to 1.0), and group 3 (M = 1.0, SD = .0002, range = 1.0 to 1.0), suggesting that the model corresponds to the data well. The very high average posterior probabilities for both cannabis screens and self-reported marijuana use models suggest that group assignment uncertainty would not be a problem for subsequent analyses involving group membership. Nevertheless, the limitations of using group membership derived from these models is noted in the discussion section.
3.1.3. Joint Marijuana Use Trajectory Analyses
Dual trajectory models were estimated in which trajectories for urine cannabis screens and self-reported marijuana use were jointly estimated, based on the trajectory models retained for each individual outcome. Parameter estimates for each of these outcomes are presented separately in Table 1 and Table 2, and findings are presented accordingly.
Table 1.
Trajectory Groups for Urine Cannabis Screens
| Parameter Estimates |
||||
|---|---|---|---|---|
| Group Name | Intercept | Linear | Quadratic | % |
| Improver | 2.62*** | −2.50*** | .29*** | 57.6 |
| Resistant | 3.02*** | −.31* | 42.4 | |
Note. Only parameters retained in the final model are presented.
p < .05.
p < .01.
p < .001.
Table 2.
Trajectory Groups for Self-Reported Marijuana Use
| Parameter Estimates |
|||||
|---|---|---|---|---|---|
| Group Name | Intercept | Linear | Quadratic | Cubic | % |
| Abstinent | .05 | 74.6 | |||
| Modest User | 1.85*** | −.096 | −.01* | 16.1 | |
| Relapser | 3.15*** | .24*** | .04** | −.001* | 9.3 |
Note. Only parameters retained in the final model are presented.
p < .05.
p < .01.
p < .001.
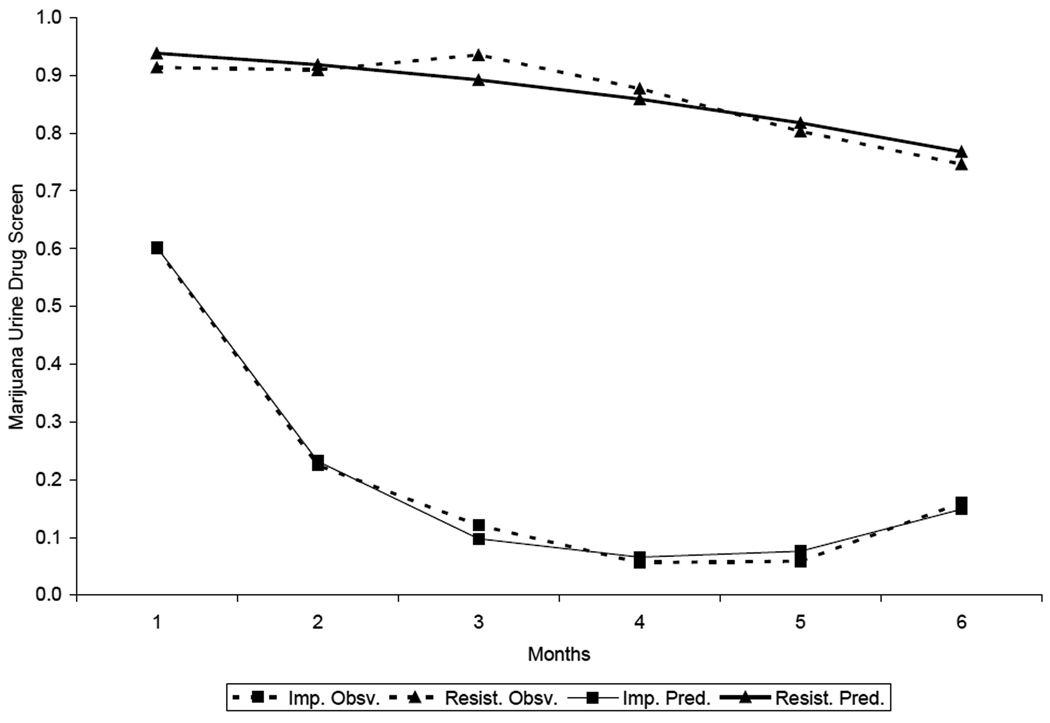
3.1.3.1 Urine cannabis screens
The two groups identified from the urine drug screen data are depicted in Figure 1 and, following the nomenclature of Waldron et al. (2005), are described as resistant and improvers. The resistant group comprised 42.4% of the sample and was characterized by a gentle negative linear slope, indicating that the percentage of positive screens gradually decreased over time. Importantly, even with this decrease, 74% of youth assigned to this group had at least one positive screen at the end of the 6-month period. The improver group comprised 57.6% of the sample. Participants in this group evidenced a dramatic decline in the probability of positive screens during the first months, and maintained a relatively low likelihood of positive screens through the remainder of the 6-month period.
Figure 1.
Observed and predicted trajectories for urine cannabis screen results. Imp = Improvers, Resist. = Resistant, Obsv. = Observed, Pred. = Predicted.
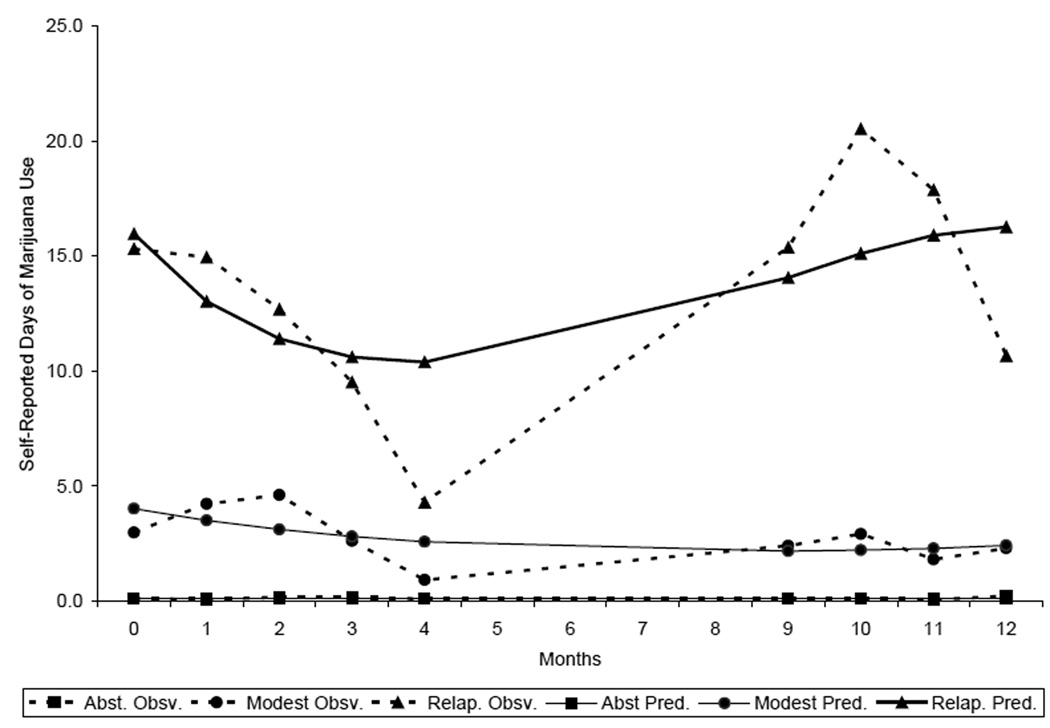
3.1.3.2. Self-reported marijuana use
The three groups identified based on the adolescent self-reports of marijuana use are depicted in Figure 2 and are labeled abstinent, modest users, and relapsers. Almost three-quarters (74.6%) of youth were assigned to the abstinent group in which members reported virtually no use of marijuana throughout the 12-month period. The modest user group comprised 16.1% of the sample and evidenced a barely perceptible U-shaped trend in self-reported use – averaging about 3 days of reported marijuana use per month. The relapser group, comprising 9.3% of the sample, demonstrated a gradual decrease in self-reported use during the first 4 months of JDC, which coincided with the most intensive substance abuse treatment efforts. Subsequently, however, their self-reported marijuana use increased to pretreatment levels.
Figure 2.
Observed and predicted trajectories for self-reported marijuana use. Abst. = Abstinent, Modest = Modest Users, Relaps. = Relapsers, Obsv. = Observed, Pred. = Predicted.
3.1.3.3. Overlap between urine screen and self-reported trajectory groups
Substantive discrepancies between the trajectory models based on biological versus self-report indices were observed. Just over half of the sample evidenced low levels of use by both measures, being classified as abstinent by self reports and as improvers by urine screens (n = 60, 50.8%). Almost one quarter were also categorized as abstinent based on self reports, but in contrast, were categorized as resistant by urine screens (n = 28, 23.7%). Other youth categorized as resistant based on urine screens evidenced consistent self-reports, being classified as either modest users (n = 18, 15.3%) or relapsers (n = 4, 3.4%). The remaining youths evidenced discrepant trajectories, being classified as improvers based on urine screens, but considered either modest users (n = 1, 0.8%) or relapsers (n = 7, 5.9%) based on self reports.
3.2. Prediction of Drug Trajectory Groups
As previously discussed, to obtain as valid an assessment of treatment response as possible, the results for biological and self-report indices were combined to create a single variable with two levels: responders and non-responders. Youth assigned to both improver (urine drug screens) and abstinent (self reports) groups were classified as responders (n = 60). On the other hand, youth assigned to the resistant (urine drug screens), modest use, or relapse groups (self-reports) were classified as non-responders (n = 58). Accordingly, youths whose trajectories evidenced modest or high levels of use by either self-report or urine screen measures were considered to be non-responders. Such procedures are consistent with those used by the developers of SPGM, who also assigned individuals into groups based on their combined membership determined by two trajectories for subsequent analyses (e.g., Côté, Vaillancourt, Barker, Nagin, & Tremblay, 2007; Fontaine, 2008).
Logistic regression analysis was used to explore the factors associated with membership in the responder versus non-responder groups. Demographic characteristics (i.e., youth gender, age, and ethnicity), youth pretreatment severity of problem behavior (i.e., self-reported marijuana use, arrests, depression/anxiety), family functioning (i.e., caregiver illegal drug use, family problems with the law, parental supervision), school status, peer drug activity, and evidence-based treatment condition were all examined as predictors. Participants with missing data on any of the predictors were excluded from the logistic regression analysis, resulting in the loss of one participant for this part of the analysis. Findings are presented in Table 3. Parental illegal substance use was the only predictor variable associated with significantly increased likelihood of classification into the non-responder group (β = 1.06, p = .02). Youth whose parents admitted to having used an illegal drug during the 3 months prior to study entry were more than nine times as likely than counterparts whose parents did not report illegal drug use to show no or little reduction in their marijuana use following enrollment in JDC (OR = 9.5). As a point of illustration, 84.6% of youth whose parents admitted to using illegal drugs were categorized as nonresponders. In contrast, 45.2% of youth whose parents did not admit to using illegal substances were classified as nonresponders.
Table 3.
Logistic Regression Predicting Membership in Treatment Responder versus Non-responder Groups
| 95% Wald Confidence Limits |
||||
|---|---|---|---|---|
| Variable | Lower | Upper | ||
| B | Odds ratio | bound | bound | |
| Ethnic minority | .22 | 1.25 | 0.45 | 3.50 |
| Female | .22 | 1,25 | 0.39 | 4.03 |
| Age | .07 | 1.07 | 0.73 | 1.56 |
| Pretreatment self-reported marijuana use | −.01 | .99 | 0.98 | 1.01 |
| Pretreatment arrests | .15 | 1.16 | 0.79 | 1.70 |
| Anxiety/depression | .06 | 1.06 | 0.98 | 1.15 |
| Caregiver illegal substance use | 1.13 * | 9.50 | 1.60 | 56.58 |
| Family legal problems | .04 | 1.08 | 0.49 | 2.34 |
| Parental supervision | .58 | 1.79 | 0.56 | 5.69 |
| Peer drug activities | .15 | .1.17 | 0.68 | 2.02 |
| School status | .52 | 1.69 | 0.68 | 4.18 |
| Treatment condition | −.16 | .73 | 0.31 | 1.68 |
p < .05.
4. Discussion
Based on analysis of longitudinal marijuana use data from a recent effectiveness trial (Henggeler et al., 2006), the present study examined youth variability in treatment responsiveness and the predictors of intervention failure following enrollment in JDC. With 97.5% of youth meeting diagnostic criteria for marijuana use or dependence at time of enrollment, urine drug screens for cannabis and self-reports for marijuana use served as key outcomes. Rigorous statistical modeling techniques identified two distinct groups of youth. The first group, comprising 51% of the sample, showed substantial declines in marijuana use over 12 months. Specifically, most youth in this group (80–85%) began testing negative for marijuana early in their course of JDC involvement and sustained their low rates of marijuana use throughout follow-up. Accordingly, these youth were considered “responders” to JDC interventions. In contrast, the second group of youth comprised 49% of the sample and can be considered “non-responders.” These youth sustained high rates (90%) of positive urine tests for cannabis throughout their first 6 months following JDC enrollment and reported using marijuana an average of 10 or more days per month by the end of the 12-month period.
The finding that a substantial portion of JDC participants did not show reductions in drug use following interventions is consistent with other research examining outcomes following substance abuse treatment for adolescents. For example, in a study of 120 adolescents receiving evidence-based outpatient treatments for marijuana abuse or dependence (Waldron, Slesnick, Brody, Turner, & Peterson, 2001), Waldron et al. (2005) reported that 25% of youth showed no improvements over 15 months post-intervention and that another 25% of youth showed initial improvements but then relapsed. On the other hand, the percentages of non-responders are even higher (e.g., 62%-75%; Brown et al., 2001; Williams & Chang, 2000) in adolescent substance abuse treatment studies that did not use evidence-based services. Thus, the fact that 51% of youth in the present study were successful in substantially reducing or eliminating their marijuana use suggests that JDC substance use outcomes are at least comparable to those obtained for other evidence-based intervention models, especially when one considers the additional challenges presented by the co-occurrence of criminal behavior among the present participants.
In the hope of informing efforts to enhance JDC outcomes, key demographic, and individual-, family-, and extrafamilial-level predictors of responder versus non-responder status were evaluated. In contrast with expectations, only one variable emerged as a significant predictor of treatment non-response, and that variable had a substantive effect. Youth whose caregivers (the vast majority of whom were biological or adoptive parents) reported using an illegal drug at the baseline assessment were more than nine times as likely to be classified as treatment non-responders. Caregiver illicit substance use was more detrimental to youth 12-month outcomes than the severity of the youth’s own substance use or arrest history at intake, or than any of the other well established risk factors examined here. Although parental drug use has long been identified as an important risk factor for adolescent substance abuse (Brook, Brook, & Pahl, 2006), the centrality of this variable for failure in JDC is noteworthy.
Several explanations for the deleterious impact of caregiver drug use on youth responsiveness to JDC seem viable. First and foremost, caregivers who use drugs model this behavior for their youth, either tacitly or directly indicating that drug use is normative and acceptable, and that quitting is challenging or unnecessary. Similarly and second, youth with drug using caregivers likely have more direct access to drugs (e.g., if caregivers use in front of the youth or bring drugs into the home) and to people who use drugs (e.g., parents’ friends) than do youth whose parents do not use illegal substances. In the absence of clear and unambiguous caregiver support for youth abstinence, JDC interventions will likely have difficulty counteracting the positive drug messages that youth receive at home and convincing youth that drug use has negative long-term consequences. Third, caregivers who use drugs are often less competent in their parenting (Berg-Nielsen, Vikan, & Dahl, 2002; Chassin, Curran, Hussong, & Colder, 1996), providing less monitoring of youth behavior and implementing consequences for appropriate (e.g., school attendance) and inappropriate (e.g., drug use, school suspension) behavior less consistently than parents who are not affected by drug use. Finally, caregivers who use drugs might be less engaged in JDC interventions, avoiding their child’s court appearances or treatment sessions due to fear that their own use will be detected. Such disengagement might limit the services that the youth receives and indicate to the youth that compliance with JDC mandates is not important.
The fact that caregiver illegal drug use is highly associated with youth non-responsiveness to JDC suggests that, to optimize effectiveness, JDC programs should have the capacity to address family problems that impede the success of participants. Consistent with this view, Hills, Shufelt, and Cocozza (2009) recently noted that the lack of family involvement in JDCs is a major contributor to treatment failure and that effective family interventions are one of the most frequent needs among JDC programs. Clearly, youth whose caregivers use illegal drugs are likely to have considerable family treatment needs including interventions to address parental drug use, improve parental monitoring and discipline skills, and reduce family conflict. It is noteworthy that in the present case, where two-thirds of the families received MST -- a well-validated family-based treatment -- the important role of caregiver drug use still emerged. Indeed, for the past decade we have been conducting treatment development studies that aim to integrate evidence-based adult substance abuse treatments for substance abusing caregivers into MST programs (Schaeffer, Saldana, Rowland, Henggeler, & Swenson, 2008; Swenson et al., 2009). Although some progress has been made, the present findings clearly demonstrate the importance of this aim for treating substance abusing youth in the juvenile justice system. Irrespective of the availability of evidence-based family treatments (Waldron & Turner, 2008), however, JDCs often possess the leverage to address caregiver drug abuse as a barrier to treatment success for youth in JDCs. Juvenile drug court personnel, especially treatment providers and the drug court coordinator, should be prepared to identify and address any barrier to successful outcomes for juvenile drug court participants.
4.1. Limitations
Several study limitations should be noted. First, youth outcomes resulting from JDC interventions were examined over the course of only 12 months, which corresponds to the typical length of JDC involvement. Some of the youth identified as non-responders in the present study might actually be “late responders,” showing benefits after their involvement in JDC has ended. Studies with longer-term follow-up periods are needed to explore this possibility. Second, urine drug screen data were not used for months 7 to12 due to high rates of missingness, and self-report data were not collected for months 5 to 9. These gaps might have influenced results in unknown ways. Third, a large confidence interval was observed around the effect of parent illegal substance use on youth responder group membership. As such, findings should be considered tentative until replicated. Fourth, other potential predictors of youth responsiveness to JDC interventions (e.g., attendance to court or treatment sessions, duration of treatment services) were not explored in the present study and might be a focus of future research. Finally, although the approach of assigning group membership based on the combined information derived from the joint analysis of two trajectories has been utilized by leaders in group-based trajectory analysis (e.g., Côté et al., 2007, Fontaine et al., 2008), it is not without limitations. Specifically, the models and group memberships derived from trajectory analyses are approximations of reality. Distinct groups of trajectories do not literally exist in the population, and consequently, group membership is probabilistic, not certain (Nagin, 2005). Although the average posterity probabilities of assignment were high for all groups in the current study (means ranged from .91 to 1.00), some uncertainty remains. Hence, the findings should be interpreted accordingly.
4.2. Conclusion
The present study contributes to the growing empirical base demonstrating the effectiveness of JDC and responds to the call within the adolescent treatment literature for a better understanding of the factors that predict positive outcomes for youth receiving substance abuse interventions (Waldron & Turner, 2008). The findings suggest that the percentage of youth who are successful following JDC interventions is comparable to those found for other empirically-supported treatments for adolescent substance abuse and is superior to the success rates reported in the literature for interventions that are not evidence-based. Most importantly, the findings also suggest that obtaining successful outcomes in JDC will be difficult in cases where the youth’s caregiver is using an illicit drug and that JDC programs might consider the integration of services to address caregiver illegal drug use as a contributing factor to youth antisocial behavior.
Acknowledgements
This manuscript was supported by grants R01AA122202 from the National Institute on Alcoholism and Alcohol Abuse and SAMHSA/Center for Substance Abuse Treatment, and R01DA13066 from the National Institute on Drug Abuse.
We greatly appreciate the support of Judge Charlie Segars Andrews, Judge Joyclin Cates, and Julius Scott, Drug Court Coordinator, of the Charleston Juvenile Drug Court for this project.
The first author is a board member and stockholder of MST Services, LLC, the Medical University of South Carolina-licensed organization that provides training in MST.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM. Manual for the Youth Self-Report and 1991 Profile. Burlington: University of Vermont, Department of Psychiatry; 1990. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Aos S, Miller M, Drake E. Evidence-based public policy options to reduce future prison construction, criminal justice costs, and crime rates. Olympia: Washington State Institute for Public Policy; 2006. [Google Scholar]
- Atkins DC, Gallop RJ. Rethinking how family researchers model infrequent outcomes: A tutorial on count regression and zero-inflated models. Journal of Family Psychology. 2007;21(4):726–735. doi: 10.1037/0893-3200.21.4.726. [DOI] [PubMed] [Google Scholar]
- Belenko S, Logan TK. Delivering more effective treatment to adolescents: Improving the juvenile drug court model. Journal of Substance Abuse Treatment. 2003;25(3):189–211. doi: 10.1016/s0740-5472(03)00123-5. [DOI] [PubMed] [Google Scholar]
- Berg-Nielsen ST, Vikan A, Dahl AA. Parenting related to child and parental psychopathology: A descriptive review of the literature. Clinical Child Psychology and Psychiatry. 2002;7:529–552. [Google Scholar]
- Brook JS, Brook DW, Pahl K. The developmental context for adolescent substance abuse intervention. In: Liddle HA, Rowe CL, editors. Adolescent substance abuse: Research and clinical advances. New York: Cambridge University Press; 2006. pp. 25–51. [Google Scholar]
- Brown SA, D'Amico EJ, McCarthy DM, Tapert SF. Four-year outcomes from adolescent alcohol and drug treatment. Journal of Studies on Alcohol. 2001;62(3):381–388. doi: 10.15288/jsa.2001.62.381. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Higgins ST. Rockville, MD: National Institute on Drug Abuse; A community reinforcment plus vouchers approach: Treating cocaine addiction. 1998 (NIH Publication No. 98-4309)
- Bureau of Justice Assistance Drug Court Clearing House. Drug court activity update. 2007 Available from http://www1.spa.american.edu/justice/documents/1956.pdf.
- Bureau of Justice Assistance Drug Court Clearing House. Summary of juvenile/family drug court activity by state and county. 2009 Available from http://www1.spa.american.edu/justice/documents/2153.pdf.
- Chassin L. Juvenile justice and substance use. The Future of Children. 2008;18(2):165–183. doi: 10.1353/foc.0.0017. [DOI] [PubMed] [Google Scholar]
- Chassin L, Curran PJ, Hussong AM, Colder CR. The relation of parent alcoholism to adolescent substance use: A longitudinal follow-up study. Journal of Abnormal Psychology. 1996;105:70–80. doi: 10.1037//0021-843x.105.1.70. [DOI] [PubMed] [Google Scholar]
- Chung T, Maisto SA, Cornelius JR, Martin CS. Adolescents’ alcohol and drug use trajectories in the year following treatment. Journal of Studies on Alcohol. 2004;65(1):105–114. doi: 10.15288/jsa.2004.65.105. [DOI] [PubMed] [Google Scholar]
- Côté SM, Vaillancourt T, Barker ED, Nagin DS, Tremblay R. The joint development of physical and indirect aggression: Predictors of continuity and change during childhood. Development and Psychopathology. 2007;19:37–55. doi: 10.1017/S0954579407070034. [DOI] [PubMed] [Google Scholar]
- Dumenci L, Windle M. Cluster analysis as a method of recovering types of intraindividual growth trajectories: A Monte Carlo study. Multivariate Behavioral Research. 2001;36(4):501–522. doi: 10.1207/S15327906MBR3604_02. [DOI] [PubMed] [Google Scholar]
- Fontaine N, Carbonneau R, Barker ED, Vitaro F, Hébert MC, Côté SM, Nagin DS, et al. Girls hyperactivity and physical aggression during childhood and adjustment problems in early adulthood: A 15-year longitudinal study. Archives of General Psychiatry. 2008;65:320–328. doi: 10.1001/archgenpsychiatry.2007.41. [DOI] [PubMed] [Google Scholar]
- General Accountability Office. Washington, DC: US Government Accountability Office; Adult drug courts: Evidence indicates recidivism reductions and mixed results for other outcomes. 2005 (No. GAO-05-219)
- Grisso T, Underwood LA. Screening and assessing mental health and substance use disorders among youth in the juvenile justice system: A resource guide for practitioners. Washington, DC: Office of Juvenile Justice and Delinquency Prevention; 2004. (No. NCJ 204956) [Google Scholar]
- Henggeler SW, Halliday-Boykins CA, Cunningham PB, Randall J, Shapiro SB, Chapman JE. Juvenile drug court: Enhancing outcomes by integrating evidence-based treatments. Journal of Consulting and Clinical Psychology. 2006;74(1):42–54. doi: 10.1037/0022-006X.74.1.42. [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Schoenwald SK, Borduin CM, Rowland MD, Cunningham PB. Multisystemic therapy for antisocial behavior in children and adolescents. 2nd ed. New York: Guilford Press; 2009. [Google Scholar]
- Hills H, Shufelt JL, Cocozza JJ. Delmar, NY: National Center for Mental Health and Juvenile Justice; Evidence-based practice recommendations for juvenile drug courts. 2009
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods & Research. 2001;29:374–393. [Google Scholar]
- Lennox R, Dennis ML, Ives M, White MK. The construct and predictive validity of different approaches to combining urine and self-reported drug use measures among older adolescents after substance abuse treatment. The American Journal on Addictions. 2006;15(1):92–101. doi: 10.1080/10550490601006089. [DOI] [PubMed] [Google Scholar]
- Lennox R, Dennis ML, Scott CK, Funk R. Combining psychometric and biometric measures of substance use. Drug and Alcohol Dependence. 2005;83:95–103. doi: 10.1016/j.drugalcdep.2005.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R, Stouthamer-Loeber M, Van Kamen W, Farrington DP. Initiation, escalation, and desistence in juvenile offending and their correlates. The Journal of Law and Criminology. 1991;82(1):36–81. [Google Scholar]
- Marlowe DB, Festinger DS, Lee PA, Dugosh KL, Benasutti KM. Matching judicial supervision to clients’ risk status in drug court. Crime and Delinquency. 2006;52(1):52–76. doi: 10.1177/0011128705281746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR. Washington, DC: National Institute on Alcohol and Alcoholism; Form 90: Structured Assessment for Drinking and Related Behaviors. 1991
- Nagin DS. Analyzing developmental trajectories: A semiparametric, group-based approach. Psychological Methods. 1999;4(2):139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Group-based modeling of development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Nagin D, Tremblay RE. Trajectories of boys' physical aggression, opposition, and hyperactivity on the path to physically violent and nonviolent juvenile delinquency. Child Development. 1999;70(5):1181–1196. doi: 10.1111/1467-8624.00086. [DOI] [PubMed] [Google Scholar]
- National Association of Drug Court Professionals, Drug Court Standards Committee. Washington, D.C: Drug Courts Program Office, Office of Justice Programs, U.S. Department of Justice; Defining drug courts: The key components. 1997
- Reyno SM, McGrath PJ. Predictors of parent training efficacy for child externalizing behavior problems -- a meta-analytic review. Journal of Child Psychology and Psychiatry. 2006;47(1):99–111. doi: 10.1111/j.1469-7610.2005.01544.x. [DOI] [PubMed] [Google Scholar]
- Schaeffer CM, Saldana L, Rowland MD, Henggeler SW, Swenson CC. New initiatives in improving youth and family outcomes by importing evidence-based practices. Journal of Child & Adolescent Substance Abuse. 2008;17:27–45. [Google Scholar]
- Shaffer DK. Reconsidering drug court effectiveness: A meta-analytic review. University of Cincinnati; 2006. Unpublished doctoral dissertation. [Google Scholar]
- Silverman WK, Pina AA, Viswesvaran C. Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):105–130. doi: 10.1080/15374410701817907. [DOI] [PubMed] [Google Scholar]
- Swenson CC, Schaeffer CM, Tuerk E, Henggeler SW, Tuten M, Panzarella P, Foley T, Lau C, Remmele L, Cannata E, Guillorn A. Adapting multisystemic therapy for co-occurring child maltreatment and parental substance abuse: The Building Stronger Families project. Journal of Emotional and Behavioral Disorders. 2009;17:3–8. [Google Scholar]
- Waldron HB, Slesnick N, Brody JL, Turner CW, Peterson TR. Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. Journal of Consulting and Clinical Psychology. 2001;69(5):802. [PubMed] [Google Scholar]
- Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):238–261. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- Waldron HB, Turner CW, Ozechowski TJ. Profiles of drug use behavior change for adolescents in treatment. Addictive Behaviors. 2005;30(9):1775–1796. doi: 10.1016/j.addbeh.2005.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams RJ, Chang SY. A comprehensive and comparative review of adolescent substance abuse treatment outcome. Clinical Psychology: Science and Practice. 2000;7(2):138–166. [Google Scholar]
- Wilson DB, Mitchell O, Mackenzie DL. A systematic review of drug court effects on recidivism. Journal of Experimental Criminology. 2006;2(4):459–487. [Google Scholar]
- Winters KC, Henly G. The Personal Experiences Inventory. Los Angeles: Western Psychological Services; 1989. [Google Scholar]
- Xie H, Drake R, McHugo G. Are there distinctive trajectory groups in substance abuse remission over 10 years? An application of the group-based modeling approach. Administration and Policy in Mental Health and Mental Health Services Research. 2006;33(4):423–432. doi: 10.1007/s10488-006-0048-0. [DOI] [PubMed] [Google Scholar]