Abstract
Simultaneous bilateral quadriceps tendon rupture is a rare injury. We report the case of bilateral quadriceps tendon rupture sustained with minimal force while refereeing a football game. The injury was suspected to be associated with statin use as the patient had no other identifiable risk factors. The diagnosis was confirmed using bedside ultrasound.
INTRODUCTION
Simultaneous bilateral quadriceps tendon rupture is a rare injury. As of 2009, only 70 cases have been reported in the English literature. Although rare, most cases have been associated with chronic metabolic disturbances or inflammatory diseases in patients over the age of 50.1 Iatrogenic causes of bilateral quadriceps rupture, including steroid and flouroquinolone use, have also been identified in the literature.2–6 Although HMG-CoA reductase inhibitor (statin)-associated musculoskeletal complaints have been reported, few have involved tendon rupture.7–11 We present a case of simultaneous bilateral quadriceps tendon rupture in which the only identifiable risk factor was statin use. The diagnosis was confirmed using bedside ultrasound.
CASE REPORT
A 56-year-old African-American male presented to the emergency department (ED) complaining of what he described as “torn muscles to the right and left knee.” The patient stated that he was refereeing a football game and, while running, suddenly felt his right knee buckle. As he was falling to the ground, he also felt a pop in the left knee. The patient described severe pain to both knees and was unable to ambulate.
At the time of examination in the ED, the patient denied pain at rest, numbness or tingling. The patient did report swelling around the knees, particularly at the superior aspect.
The patient’s past medical history was remarkable only for hyperlipidemia, for which he had been taking atorvastatin (lipitor), 20 mg once daily, for about three years. He stated he had stopped the medication three weeks prior to the injury and denied previously being on any other cholesterol-lowering agent. He denied other past medical history, specifically renal problems, hypertension, metabolic problems, joint diseases, previous orthopedic injuries or other chronic illnesses. He also denied other medication use, including steroids, herbal supplements or fluoroquinolones in the preceding six months. Furthermore, he denied previous musculoskeletal problems prior to or during treatment with atorvastatin. His past surgical, family and social histories were all unremarkable.
On physical exam, the patient was an athletic-appearing male who looked younger than his stated age, sitting up on the stretcher in no acute distress. Vital signs revealed a blood pressure of 149/75, but were otherwise within normal limits. All portions of the exam were unremarkable except for the musculoskeletal exam. Observation revealed swelling to both knees, left greater than right, without ecchymosis, skin lacerations or open fractures. He had visible defects superior to the patella bilaterally. There was tenderness to palpation of both distal quadriceps tendons. The thigh and leg compartments were soft. There was full passive range of motion of both knees with pain, but active range of motion was severely limited. The patient was unable to straight-leg-raise due to complete absence of knee extension bilaterally. There was full active range of motion of both ankles and 5/5 strength when tested. He was neurovascularly intact.
Anterior-posterior and lateral radiographs of the right and left knees showed a thickening of the quadriceps tendon with pre-patellar bursitis on the left and normal findings on the right.
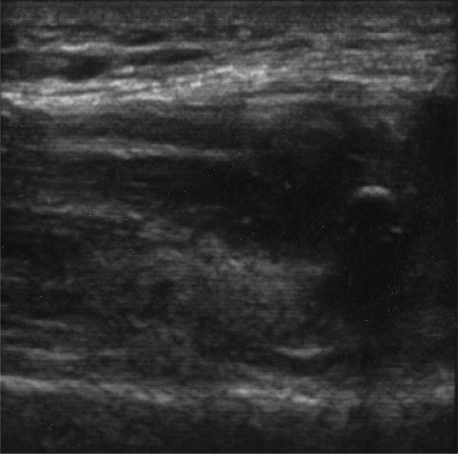
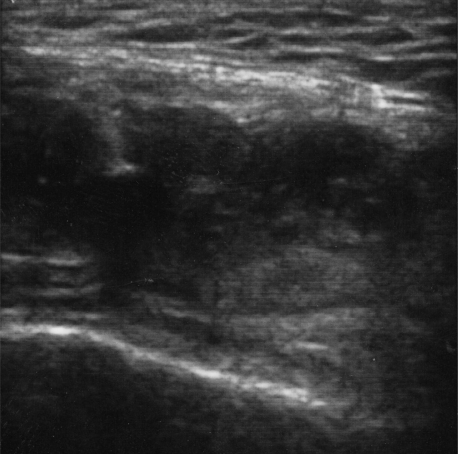
Bedside ultrasound was performed for confirmation of suspected bilateral quadriceps tendon rupture. A linear probe was used to scan the patient bilaterally revealing complete disruption of both quadriceps tendons with anechoic fluid collections noted superiorly, representing hematomas. Both sides appeared similar on ultrasound, verifying the diagnosis of bilateral spontaneous quadriceps tendon ruptures (Figure 1 and Figure 2).
Figure 1.
Sagittal view of right quadriceps tendon rupture
Figure 2.
Transverse view of right quadriceps tendon rupture
Following an orthopedic surgery consult in the ED, the patient was discharged with bilateral knee immobilizers, pain medication and outpatient surgery appointment. Six days later, intraoperative examination confirmed bilateral complete quadriceps tendon ruptures at the osseotendinous junction, and open repair was performed.
The patient was admitted for two days for pain control. While in the hospital the patient was found to be hypertensive and was started on metoprolol, 50 mg by mouth twice daily. According to the patient, the hypertension was likely secondary to pain because his primary doctor stopped the antihypertensive medication after which he had no problems with blood pressure control.
Once pain control was achieved with oral medications, the patient was discharged to a rehab facility for further care, where he remained for four days before discharged home. Instructions upon hospital discharge were to weight-bear as tolerated on both legs as long as the knee immobilizers were in place. Range-of-motion was gradually increased over the next four weeks.
Four months postoperatively the patient continued to be followed in the orthopedic clinic and had achieved 95 degrees of knee flexion bilaterally. However, the patient continued to suffer knee stiffness and was unable to ambulate four months following operative repair.
Investigation into possible causes of the patient’s bilateral quadriceps tendon ruptures identified only oral statin administration as a suspected risk factor. Laboratory analysis revealed a normal comprehensive metabolic panel with a creatinine of 1.1 and normal serum calcium.
DICUSSION
We report a rare case of bilateral quadriceps tendon rupture associated with statin use. We performed a review of the English language literature using the National Library of Medicine and National Institutes of Health database and identified only 70 cases. The first case of bilateral quadriceps tendon rupture was reported by Steiner and Palmer in 1949.12 The majority of bilateral quadriceps tendon rupture have occurred in men over 50, and in those with risk factors such as obesity, diabetes mellitus, chronic renal failure and hyperparathyroidism.1,13–18 Of the reported cases in our review, none were clearly associated with statin use.
Although there are no reported cases of bilateral quadriceps tendon rupture associated with statin use, these cholesterol-lowering agents have been reported to be associated with the development of musculoskeletal complaints, including tendonitis and unilateral tendon rupture.7–10 For example, in a study of 96 patients with tendonitis or tendon rupture believed to be associated with statin use, 14 ruptures involved the quadriceps tendon but none were bilateral.10 Although unproven, several case reports suggest an association between tendon injury and statin therapy.11,19 In addition, several tendinopathies have been reported involving a statin combined with ezetimibe, another cholesterol-lowering agent.20–21 A recent case-control study examining the association between statins and tendon rupture found no significant association compared with control groups.22 Thus the association of statin use and tendon rupture remains ill-defined.
There are several hypotheses that attempt to explain the association of statin use with tendon injury. The exact cause remains unresolved, but a combination of suppressive effects on matrix metalloproteinase activity and prostaglandin E2 activity is thought to play a major role.20,23–24 These enzymes are active in the remodeling process in tendons, but when disrupted could potentially lead to tendon weakening or even rupture.
Multiple large clinical trials have demonstrated the efficacy of statins as cholesterol-lowering agents and in their ability to decrease the risk of myocardial infarctions, angina and revascularization procedures in patients with coronary artery disease.25–29 Knowledge of the cases of tendon injury that do occur and the classes of patients that may be more at risk for developing certain adverse reactions could allow for prevention in some individuals.
As the prevalence of obesity and type II diabetes mellitus increases in the United States, many Americans are being treated for hyperlipidemia with statins. It is possible that statin-associated tendinopathy and tendon rupture will become more frequent, and physicians should be aware of the possible relationship between statin therapy and tendon rupture when treating their patients with cholesterol-lowering medications.
Footnotes
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES:
- 1.Shah MK. Simultaneous bilateral rupture of quadriceps tendons: analysis of risk factors and associations. South Med J. 2002;95:860–6. [PubMed] [Google Scholar]
- 2.Liow RY, Tavares S. Bilateral rupture of the quadriceps tendon associated with anabolic steroid use. Br J Sports Med. 1995;29:77–9. doi: 10.1136/bjsm.29.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilkinson S, Houpt JB, Pritzker KP, Goldhar JN, Gross AE. Avulsion of the quadriceps tendons in a patient with an unusual deforming arthritis and varied skin lesions. J Rheumatol. 1981;8:983–8. [PubMed] [Google Scholar]
- 4.Karistinos A, Paulos LE. “Ciprofloxacin-induced” bilateral rectus femoris tendon rupture. Clin J Sport Med. 2007;17:406–7. doi: 10.1097/JSM.0b013e31814c3e69. [DOI] [PubMed] [Google Scholar]
- 5.Gottschalk AW, Bachman JW. Death following bilateral complete Achilles tendon rupture in a patient on flouroquinolone therapy: a case report. J Med Case Reports. 2009;3:1. doi: 10.1186/1752-1947-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khalig Y, Zhanel GG. Flouroquinolone-associated tendinopathy: a critical review of the literature. Clin Infect Dis. 2003;36:1404–10. doi: 10.1086/375078. [DOI] [PubMed] [Google Scholar]
- 7.Nichols GA, Koro CE. Does statin therapy initiation increase the risk for myopathy? An observational study of 32,225 diabetic and nondiabetic patients. Clin Ther. 2007;29:1761–70. doi: 10.1016/j.clinthera.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 8.Molokhia M, McKeique P, Curcin V, Majeed A. Statin induced myopathy and myalgia: time trend analysis and comparison of risk associated with statin class from 1991–2006. PLos One. 2008;3:e2522. doi: 10.1371/journal.pone.0002522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thompson PD, Clarkson P, Karas RH. Statin-associated myopathy. JAMA. 2003;289:1681–90. doi: 10.1001/jama.289.13.1681. [DOI] [PubMed] [Google Scholar]
- 10.Marie I, Delafenetre H, Massy N, Thuillez C, Noblet C. Tendinous disorders attributed to statins: a study on ninety-six spontaneous reports in the period 1990–2005 and review of the literature. Arthritis Rheum. 2008;59:367–72. doi: 10.1002/art.23309. [DOI] [PubMed] [Google Scholar]
- 11.Chazerain P, Hayem G, Hamza S, Best C, Ziza JM. Four cases of tendinopathy in patients on statin therapy. Joint Bone Spine. 2001;68:430–3. doi: 10.1016/s1297-319x(01)00300-1. [DOI] [PubMed] [Google Scholar]
- 12.Steiner CA, Palmer LH. Simultaneous bilateral rupture of the quadriceps tendon. Am J Surg. 1949;78:752–5. doi: 10.1016/0002-9610(49)90317-7. [DOI] [PubMed] [Google Scholar]
- 13.Neubauer T, Wagner M, Potschka T, Riedl M. Bilateral simultaneous rupture of the quadriceps tendon: a diagnostic pitfall? Report of 3 cases and meta-analysis of the literature. Knee Surg Sports Traumatol Arthrosc. 2007;15:43–53. doi: 10.1007/s00167-006-0133-7. [DOI] [PubMed] [Google Scholar]
- 14.Provelegios S, Markakis P, Cambouroglou G, Choumis G, Dounis E. Bilateral, spontaneous and simultaneous rupture of the quadriceps tendon in chronic renal failure and secondary hyperparathyroidism. Report of 5 cases. Arch Anat Cytol Pathol. 1991;39:228–32. [PubMed] [Google Scholar]
- 15.Kim YH, Shafi M, Lee YS, Kim JY, Kim WY, Han CW. Spontaneous and simultaneous rupture of both quadriceps tendons in a patient with chronic renal failure. A case studied by MRI both preoperatively and postoperatively. Knee Surg Sports Traumatol Arthrosc. 2006;14:55–9. doi: 10.1007/s00167-005-0626-9. [DOI] [PubMed] [Google Scholar]
- 16.Kaar TK, O’brien M, Murray P, Mullan GB. Bilateral quadriceps tendon rupture: a case report. Ir J Med Sci. 1993;162:502. doi: 10.1007/BF03022583. [DOI] [PubMed] [Google Scholar]
- 17.De Franco P, Varghese J, Brown WW, Bastani B. Secondary hyperparathyroidism, and not beta 2-microglobulin amyloid, as a cause of spontaneous tendon rupture in patients on chronic hemodialysis. Am J Kidney Dis. 1994;24:951–5. doi: 10.1016/s0272-6386(12)81067-5. [DOI] [PubMed] [Google Scholar]
- 18.Preston FS. Bilateral rupture of quadriceps tendons. Br Med J. 1967;1:364. doi: 10.1136/bmj.1.5536.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Movahed MR, Samsamsharaiat SA. Reproducible tendinitis-like symptoms related to statin therapy. J Clin Rheumatol. 2006;12:320–1. doi: 10.1097/01.rhu.0000250239.01489.3a. [DOI] [PubMed] [Google Scholar]
- 20.Pullatt RC, Gadarla MR, Karas RH, Alsheikh-Ali AA, Thompson PD. Tendon rupture associated with simvastatin/ezetimibe therapy. Am J Cardiol. 2007;100:152–3. doi: 10.1016/j.amjcard.2007.02.068. [DOI] [PubMed] [Google Scholar]
- 21.Fux R, Morike K, Gundel UF, Hartmann R, Gleiter CH. Ezetimibe and statin-associated myopathy. Ann Intern Med. 2004;140:671–2. doi: 10.7326/0003-4819-140-8-200404200-00034. [DOI] [PubMed] [Google Scholar]
- 22.Beri A, Dwamena FC, Dwamena BA. Association between statin therapy and tendon rupture: a case-control study. J Cardiovasc Pharmacol. 2009;53:401–4. doi: 10.1097/FJC.0b013e3181a0ce8b. [DOI] [PubMed] [Google Scholar]
- 23.Magra M, Maffulli N. Molecular events in tendinopathy: a role for metalloproteases. Foot Ankle Clin. 2005;10:267–77. doi: 10.1016/j.fcl.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 24.Riley GP, Curry V, DeGroot J, van El B, Verzijl N, Hazleman BL, Bank RA. Matrix metalloproteinase activities and their relationship with collagen remodeling in tendon pathology. Matrix Biol. 2002;21:185–195. doi: 10.1016/s0945-053x(01)00196-2. [DOI] [PubMed] [Google Scholar]
- 25.Bestehorn HP, Rensing UF, Roskamm H, Betz P, Benesch L, Schemeitat K, et al. The effect of simvastatin on progression of coronary artery disease: The multicenter coronary intervention study (CIS) Eur Heart J. 1997;18:226–34. doi: 10.1093/oxfordjournals.eurheartj.a015224. [DOI] [PubMed] [Google Scholar]
- 26.Downs JR, Clearfield M, Weis S, Whitney E, Shapiro DR, Beere PA, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of the AFCAPS/TexCAPS. JAMA. 1998;279:1615–22. doi: 10.1001/jama.279.20.1615. [DOI] [PubMed] [Google Scholar]
- 27.Heart Protection Study Collaborative Group MRC/BHF heart protection study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomized placebo-controlled trial. Lancet. 2002;360:7–22. [Google Scholar]
- 28.Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomized controlled trial. Lancet. 2002;360:1623–30. doi: 10.1016/s0140-6736(02)11600-x. [DOI] [PubMed] [Google Scholar]
- 29.Van Boven AJ, Jukema JW, Zwinderman AH, Crijins HJ, Lie KI, Bruschkle AV. Reduction of transient myocardial ischemia with pravastatin in addition to the conventional treatment in patients with angina pectoris. Circulation. 1996;94:1503–5. doi: 10.1161/01.cir.94.7.1503. [DOI] [PubMed] [Google Scholar]