Abstract
The purpose of this experiment was to conduct a dismantling study of cognitive processing therapy in which the full protocol was compared with its constituent components—cognitive therapy only (CPT-C) and written accounts (WA)—for the treatment of posttraumatic stress disorder (PTSD) and comorbid symptoms. The intent-to-treat (ITT) sample included 150 adult women with PTSD who were randomized into 1 of the 3 conditions. Each condition consisted of 2 hr of therapy per week for 6 weeks; blind assessments were conducted before treatment, 2 weeks following the last session, and 6 months following treatment. Measures of PTSD and depression were collected weekly to examine the course of recovery during treatment as well as before and after treatment. Secondary measures assessed anxiety, anger, shame, guilt, and dysfunctional cognitions. Independent ratings of adherence and competence were also conducted. Analyses with the ITT sample and with study completers indicate that patients in all 3 treatments improved substantially on PTSD and depression, the primary measures, and improved on other indices of adjustment. However, there were significant group differences in symptom reduction during the course of treatment whereby the CPT-C condition reported greater improvement in PTSD than the WA condition.
Keywords: cognitive processing therapy, posttraumatic stress disorder, interpersonal violence, cognitive behavioral therapy
There are two primary mechanisms of change thought to under-lie efficacious treatment of posttraumatic stress disorder (PTSD): (1) Improvement occurs through emotional processing of the trauma memory by way of repeated exposure, and/or (2) improvement occurs because the meaning of the event changes (Brewin, Dalgleish, & Joseph, 1996; Ehlers & Clark, 2000; Foa & Jaycox, 1999; Keane & Barlow, 2002; Resick, 2001b). Consistent with such theories, most therapies that have been developed and tested for PTSD have tended to include repeated in vivo and/or imaginal exposure, some type of cognitive intervention, or a combination of exposure and cognitive therapy. Such approaches have accumulated empirical support in the treatment of PTSD (Bryant, Moulds, Guthrie, Dang, & Nixon, 2003; Ehlers et al., 2003; Foa et al., 1999, 2005; Foa, Rothbaum, Riggs, & Murdock, 1991; Marks, Lovell, Noshirvani, Livanou, & Thrasher, 1998; Resick, Nishith, Weaver, Astin, & Feuer, 2002; Schnurr et al., 2007).
Nonetheless, the outcomes of such approaches leave room for improvement, with approximately 20%–50% of treatment completers continuing to be diagnosed with PTSD after treatment (Resick et al., 2002; Schnurr et al., 2007). In response, researchers have begun to examine the effects of various treatment components, in which components are examined singly and in combination, or a new component is added to an existing protocol (Bryant et al., 2003; Foa et al., 2005; Marks et al., 1998; Paunovic & Öst, 2001). Published results thus far have been mixed. Marks et al. (1998) compared exposure, cognitive restructuring (CR), the combination, and a relaxation training control condition. The combination of the two active components was no more efficacious in treating PTSD than exposure or CR alone, although all three exposure and cognitive interventions were more efficacious than relaxation training. Paunovic and Öst (2001) conducted a study with a small sample comparing exposure with a combination of exposure, CR, and breathing retraining and found no differences between the treatments. Foa et al. (2005) compared prolonged exposure (PE) with PE plus CR and also found no improvement with the combination. In contrast, Bryant et al. (2003) compared exposure with exposure plus CR and found that the combination was more efficacious than exposure alone.
There are several possible explanations for the discrepancy in outcomes across these studies. One is that the sample sizes were not large enough to detect the rather small effects expected between active interventions (Schnurr, 2007). Another possible explanation is that the CR that was offered may have been different across the studies. It appears that Foa et al.’s (2005) and Paunovic and Öst’s (2001) CR was more present-focused with an emphasis on current fear cognitions, and Marks et al.’s (1998) and Bryant et al.’s (2003) studies may have used a more trauma-focused cognitive intervention. However, more problematic is the very nature of additive studies themselves.
When one develops a therapy protocol with particular session length and number of sessions that is considered optimal for that protocol and then attempts to add components in an additive study, the combination treatment typically suffers because the original components must be condensed to accommodate the new component. The combination treatment may not be delivered in an optimal manner because not enough time is spent on either component to reach a therapeutic dose. For example, in Foa et al.’s (1999) study comparing PE, stress inoculation training (SIT), and the combination of SIT and PE (SIT/PE), 56% of the PE group was evaluated to have good end state functioning compared with 36% of the SIT/PE group. In Foa et al.’s (2005) study comparing PE with the combined PE/CR condition, they found that the pre- to posttreatment effect sizes (ESs) were a standard deviation less for the combined condition than the PE only condition. Clearly, even an efficacious intervention, such as exposure therapy, is diminished when less session time is spent on exposure to accommodate the addition of SIT or CR.
Further, the temporal ordering of the therapeutic components in an additive study could also detract from the overall efficacy of the intervention beyond the abbreviation of the components in an additive design. For example, if one were to add CR or SIT after exposure has just been completed, it could have diminishing returns compared with having those components precede the exposure. To truly test an additive design, one would have to counter-balance the temporal ordering of the components in addition to the amount of actual time spent on each element.
An alternative approach to the additive study is the dismantling study. In a dismantling design, the components of a treatment are examined separately and in combination to disentangle the relative utility of various components. For example, in the 1970s, many studies were designed to examine individual components of systematic desensitization for simple phobias until it was concluded that neither the relaxation nor the hierarchical presentation of feared stimuli were required beyond exposure for a therapeutic effect. The dismantling approach has two distinct advantages relative to the additive approach. First, as treatment components are administered as stand-alone treatment packages, there is no need to condense any one component. Second, the temporal ordering of treatment components is no longer problematic; the full treatment package can be administered as it was originally designed.
Nonetheless, dismantling studies pose their own unique challenges and may have potential drawbacks. Because components are pulled out and expanded to fill time, they must stand as viable therapies on their own. To equate time spent in treatment across conditions, a client will receive more of a given component than he or she would if the full treatment package had been administered. Treatment components may also be changed in ways that increase or decrease therapist– client time together. Additionally, it may not be possible to dismantle a treatment such that there are no overlapping procedures across conditions. For example, a cognitive intervention may also contain at least minimal exposure elements because discussing trauma-related cognitions almost certainly necessitates talking about the trauma. Furthermore, when clients talk about reactions to the exposure therapy, such discussion could be construed as a cognitive intervention. Such threats to internal validity may have the effect of influencing the interpretation of the results.
Cognitive processing therapy (CPT) for PTSD was originally developed with both cognitive therapy and written trauma accounts. Both components were initially incorporated into the 12-session protocol, so neither component would have to be shortened or condensed in a dismantling study. Thus, with CPT, it is possible to conduct a dismantling study to determine whether both components are essential and contribute to successful outcomes.
CPT was first tested with rape victims in a group format (Resick & Schnicke, 1992), followed by a clinical trial in which individually administered CPT was compared with PE and a wait-list control group (Resick et al., 2002). The results of that trial showed no statistical differences between CPT and PE on the primary outcome variables of PTSD and depressive symptoms. There were, however, small to medium ES differences favoring CPT on those measures. A statistical effect did emerge between conditions on guilt cognitions, with large ES differences favoring CPT over PE. Both treatments resulted in markedly improved symptoms compared with the waiting list condition, which did not improve. Chard (2005) tested a group and individual adaptation of CPT for adult survivors of child sexual abuse compared with a waiting list control and found CPT to be very efficacious in reducing PTSD and other comorbid symptoms. Recently, CPT was tested in a randomized trial with military veterans and was also found efficacious (Monson et al., 2006). Similarly, in community settings, CPT was found to be effective with incarcerated adolescents (Ahrens & Rexford, 2002) and refugees, even when delivered through an interpreter (Schulz, Resick, Huber, & Griffin, 2006).
In the traditional administration of CPT, the cognitive component is predominant, with the trauma account element consisting of two sessions that include writing about the worst traumatic event, reading it back to the therapist, and processing emotions. Clients are also asked to read the account at home between sessions on a daily basis. There is built-in latitude within the CPT protocol to assign clients further written accounts (WAs) at home if helpful. The therapist then uses Socratic questioning to challenge the clients’ erroneous conclusions about the event. The development of the dismantling design included changing CPT to the cognitive therapy only (CPT-C) condition, which required the elimination of the two exposure sessions and a greater focus on Socratic questioning. Developing the WA condition of the dismantling design was more challenging because one must expand the therapy to fill 12 hrs of writing, reading the WAs back to the therapist, and conducting emotion-focused non-CR processing with the therapist. We accomplished this by having the participants write their accounts during part of the session and having the reading of accounts and support work during the other half. Piloting indicated that we could not accomplish this with 1-hr sessions because participants could not typically write their account in only 30 min. We used PE as a guide to the therapy structure and configured the WAs to be implemented faithfully to CPT but also as close as possible to the way PE was implemented in the previous trial comparing CPT and PE (Resick et al., 2002) with 2-hr sessions after the first two introductory 1-hr sessions.
The primary purpose of this study was to examine the components of CPT, singly and compared with the full protocol. We hypothesized that the original CPT protocol would be more efficacious than either component—CPT-C or WA—administered alone, although we also planned to compare CPT-C with WA to determine whether either single component was superior to the other. The design of the study, which included assessment of PTSD and depressive symptoms throughout therapy, as well as before and after, allowed for a powerful examination of change across conditions and time.
Using data from Resick et al.’s (2002) clinical trial comparing CPT with PE and a waiting list condition, Nishith, Resick, and Griffin (2002) conducted curve estimation techniques and found that PTSD scores during treatment were quadratic rather than linear. In other words, PTSD scores tended to increase slightly before decreasing. Thus, a secondary purpose of this study was to examine patterns of change to determine whether those findings are replicated and to determine when change occurs during the course of treatment. Finally, in this study we aimed to expand the investigation of the effects of the three therapy conditions on a range of comorbid symptoms known to be associated with posttrauma functioning. The relationships among treatment and depression, anger, anxiety, and cognitions (including guilt, shame, and other dysfunctional cognitions) were also examined.
Method
Participants
Participants were recruited broadly throughout the St. Louis metropolitan area through referrals from victim assistance agencies, community therapists, flyers, newspaper advertisements, and word of mouth. Exclusion criteria from the trial included illiteracy, current psychosis, suicidal intent, or dependence upon drugs or alcohol. In addition, participants could not be in a currently abusive relationship or being stalked. Participants were included if they had experienced sexual or physical assault in childhood or adulthood and met criteria for PTSD at the time of the initial assessment, were at least 3 months posttrauma (no upper limit), and if on medication, were stabilized. Women with current substance dependence were included if/when they had been abstinent for 6 months. Those with substance abuse were permitted to participate if they agreed to desist in usage during the period of treatment. Following telephone screening, potential participants were invited to be assessed for possible participation, at which time they discussed and signed informed consent for participation. This study was conducted in compliance with the University of Missouri Institutional Review Board.
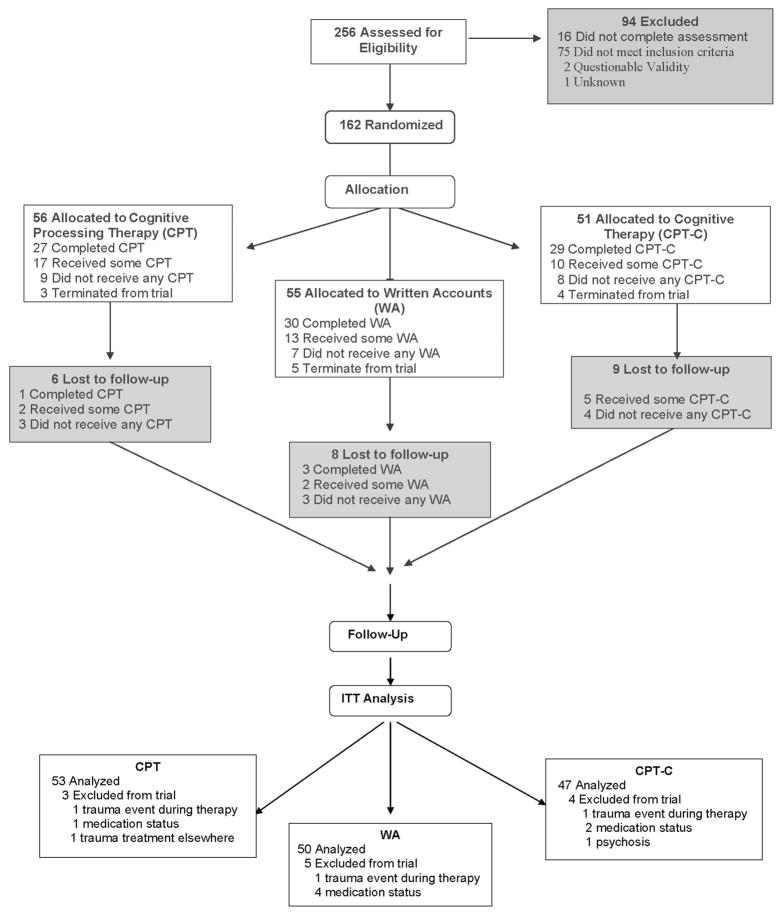
A total of 256 women were assessed for possible participation (see Figure 1) by assessors who were blind to group assignment. The most common reasons for exclusion from the study (n = 94) were not meeting the criteria for PTSD (n = 28), current substance dependence (n = 12), medication instability (n = 11), and current abuse or stalking (7). Sixteen women failed to complete the initial assessment. Of 162 women randomized into the trial, 12 were terminated from the study, by design, for meeting exclusion criteria subsequent to new violence (women had to be at least 3 months posttrauma), changes in medication, or psychosis. Among them, 1 WA participant was terminated from the trial when the therapist stopped the protocol because of increased suicidal ideation. These terminations were evenly distributed across groups. Therefore, the intent-to-treat (ITT) sample included 150 women. There was one other unrelated adverse event during the trial.
Figure 1.
Flowchart of participants through the trial. ITT = intent-to-treat.
Randomization was largely successful with regard to demographics of the sample and symptoms at the pretreatment assessment. In the ITT sample, there were no significant differences in demographics among the three groups except for income. Overall, the women were an average of 35.4 years of age (SD = 12.4) and had 13.8 years of education (SD = 2.8; 52% had partial college or technical training). Only 20% (30 of 150) of the women were married or cohabiting. The sample was 62% White (93 of 150), 34% African-American (51 of 150), and 4% were from other racial groups (5 of 150). A total of 3% described themselves as Hispanic. The average length of time since the index event (the event deemed worst and the initial focus of treatment) was 14.6 years (SD = 14.4; Mdn = 10.4), with a range from 3.3 months to 58.3 years. There was a significant difference in income levels, χ2(10, N = 146) = 26.7, p =.003, with the CPT group having significantly lower income than the other two conditions. In the CPT group, 79% of the women had total household income less than $20,000 per year compared with 42% of the women in WA and 46% of the women in CPT-C. There were, however, no differences among the groups in the number of hours worked per week (M = 19.43, SD = 20.2). With regard to current medication, 41% of the sample was on psychotropic medication, which did not differ across groups.
The three groups did not differ by their trauma histories or index events, although there was a trend ( p =.06) for the CPT group to report more adult victimization frequency. This was a multiply victimized sample. Of the sample, 6% had only adult sexual assault or adult physical assault. Another 3% had only child sexual abuse. However, 84% of the sample endorsed adult physical assault, 80.7% endorsed adult sexual victimization, 78% reported child sexual abuse (60% penetrative sexual abuse), and 60.7% reported experiencing domestic violence. When asked about the total number of childhood victimization events, 47.3% reported more than 10, and 46.6% reported more than 10 adulthood incidents. For the assessment of PTSD and initial treatment focus, participants were asked to identify a worst event, which was designated as the index event. Of the ITT participants, 38% identified child sexual assault as the index event; 31.1% chose adult sexual assault, 23.3% chose adult physical assault, and 7.3% chose child physical assault.
Of the women in the ITT sample, 24 never returned for the first session of therapy, 40 received partial therapy, of whom, 5 women received partial treatment because the allocated 12-week therapy time limit expired. Of those who started treatment and did not run out of time (they may have finished if given more time), 34% of CPT, 26% of WA, and 22% of CPT-C participants dropped out of therapy. There were 127 women who completed at least one of the posttreatment assessments regardless of treatment participation (15% study dropout). There were 86 women who completed all therapy sessions, of whom, 4 did not return for follow-up. There were no significant differences between treatment groups on these treatment status categories. There were, however, differences in demographics among treatment status groups. There was a significant race effect on treatment completion, χ2(4, N = 150) = 15.55, p = .004. Only 37.3% (19 of 51) of the African American women completed all therapy sessions, 35.3% (18 of 51) completed some sessions, and 27.5% (14 of 51) attended no sessions. This compared with 66.7% (62 of 93), 23.7% (22 of 93), and 9.7% (9 of 93), respectively, of Caucasian women, and 83% (5 of 6) who completed and 16.7% (1 of 6) who did not attend any sessions who were listed as “other” (Asian, Native American, Pacific Islander). There were also differences in treatment completion based on household income, χ2(10, N = 146) = 25.79, p = .004. Of those who did not attend any therapy, 69.6% (16 of 23) earned less than $20,000 per year, and none had incomes above $50,000 per year. Of those who received some therapy, 75.7% (28 of 37) fell into the under $20,000 per year category, and 10.8% (4/37) had household income of more than $50,000 per year. Of the participants who completed the full course of therapy, 44.2% (38 of 86) earned under $20,000 household income per year, whereas 18.6% (16 of 86) fell into the over $50,000 per year category. In sum, although this was largely a low income sample, lowest income participants were less likely to complete the full course of therapy. There were no differences in treatment status based on marital/cohabitation status, age, years of education, number of crimes in childhood, number of crime events in adulthood, or number of crime events in the previous 6 months.
As per the inclusion criterion, all participants met the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM–IV; American Psychiatric Association, 1994) criteria for PTSD at the initial interview. At pretreatment, using the SCID modules for MDD, panic disorder, and substance abuse, there were no significant differences between groups on these disorders. Of the total sample, 50% (75 of 150) met the criteria for MDD, 1 woman met the criteria for alcohol abuse, 2 were inadvertently admitted with alcohol or drug dependence,1 and 2% had cannabis abuse, but there was no other substance abuse or dependence. At pretreatment, 20% of the women also met criteria for panic disorder. There were no differences between groups on any of the symptom measures at pretreatment.
Instruments
Interviews
Clinician-Administered PTSD Scale (CAPS; Blake et al., 1990, 1995)
The CAPS can be used to assess DSM–IV PTSD diagnosis and PTSD symptom severity. For each symptom, a clinician rates two separate dimensions, frequency and intensity, on a scale ranging from 0 (never) to 4 (daily or almost daily), and from 0 (none) to 4 (extreme), respectively. Items rated with a frequency of one or higher and an intensity of two or higher were considered diagnosable symptoms (Blake et al., 1995). Symptom severity was determined by the sum of frequency and intensity ratings. CAPS diagnoses and symptom severity scores have demonstrated reliability and validity (Weathers, Keane, & Davidson, 2001). Cronbach’s alpha on CAPS total score for this study was .91.
Structured Clinical Interview for DSM–IV Axis I Disorders—Patient Edition (SCID; First, Gibbon, Spitzer, & Williams, 1996)
The SCID is a semistructured interview designed to assess the presence of DSM–IV Axis I disorders. In this study, we assessed panic disorder, major depressive disorder (MDD), and substance abuse/dependence. The psychotic screen of the SCID was used for exclusion purposes. Median interrater and test–retest reliability for the diagnostic modules used in this study are described in Zanarini et al. (2000).
Standardized Trauma Interview
The standardized trauma interview was adapted from Resick, Jordan, Girelli, Hutter, and Marhoeder-Dvorak’s (1988) treatment study and includes both investigator-generated and standardized questionnaires. In this study, it was used to assess demographic characteristics, including trauma history. Child sexual abuse was assessed with the Sexual Abuse Exposure Questionnaire (SAEQ; Rowan, Foy, Rodriguez, & Ryan, 1994). The SAEQ is a retrospective self-report measure of childhood sexual abuse. This study utilized the 10-item overall exposure portion of the questionnaire, in which respondents identify whether they experienced each of 10 sexual abuse events. Affirmative answers are summed to determine an overall exposure score. The overall exposure portion of the SAEQ has demonstrated reliability and validity in a treatment-seeking sample, including 2-week test–retest reliability ranging from .73 to .93 and statistically significant relationships with PTSD diagnoses and symptom severity (Rowan et al., 1994). The Physical Punishment Scale of the Assessing Environments-III (AE-III-PP; Berger, Knutson, Mehm, & Perkins, 1988) was used to assess childhood physical abuse victimization. The AE-III-PP examines the experience of punishment during childhood (before age 16 years) with 12 true or false items. Punitive behaviors in the AE-III-PP range from mild (e.g., spanked) to physically damaging (e.g., severely beaten). A total score is computed by summing the positively endorsed items, with a higher score reflecting more physical abuse experiences. The AE-III-PP has demonstrated reliability and validity, including acceptable test–retest reliability over a 2-month period and score differences between groups with and without verified physical abuse (Berger et al., 1988; Feindler, Rathus, & Silver, 2003). The 12-item Physical Assault Scale of the Revised Conflict Tactics Scales (Straus, 1979) was used to assess adult physical assault victimization. Participants reported the frequency of each abusive behavior experienced from current partners during the past year and previous partners during the last year of the relationship on a scale ranging from 0 (never) to 6 (more than 20 times). The Physical Assault Scale has demonstrated reliability and validity, including internal consistency of .86 and expected relationships between the scale and measures of related experiences, such as psychological abuse (Straus, Hamby, Boney-McCoy, & Sugarman, 1996). Additional investigator-generated items were used to further assess history of adult trauma. These items have no demonstrated psychometric properties.
Interrater reliability on structured interviews
We established interrater reliability for diagnostic interviews with new diagnostic interviewers by using training tapes and having more experienced faculty interviewers supervise and rate initial live interviews. After reliability had been established (100% diagnostic reliability and high item reliability), all diagnostic interviewers had audiotapes reviewed by senior project staff on a random ongoing basis to ensure that there was no drift in diagnostic decisions. Weekly individual and group meetings were held throughout the project to discuss diagnostic conceptualizations and to reconcile conflicting diagnostic decisions.
A random sample of 31 tapes was selected for evaluation of interrater reliability for the CAPS. Categorical diagnostic analyses revealed that the kappa coefficient for the overall PTSD diagnosis was 1.00 with 100% agreement. Kappa values and percentages of agreement for each of the three clusters of PTSD symptoms were as follows: reexperiencing (κ = .87; 90% agreement), avoidance (κ = .72; 77% agreement), and arousal (κ = .69; 77% agreement).
A random sample of 40 tapes was selected for evaluation of diagnostic reliability on the SCID. The SCID was administered to assess current diagnoses of MDD, alcohol dependence and substance dependence, and panic disorder. Kappa values and percentages were obtained for MDD (κ = .80; 90% agreement), alcohol and substance dependence (all κs = 1.00; 100% agreement), and panic disorder (κ = .75; 92% agreement).
Self-Report Scales
Beck Depression Inventory—II (BDI–II; Beck, Steer, & Brown, 1996)
The BDI–II contains 21-items assessing depressive symptoms corresponding to the DSM–IV criteria for MDD. The BDI–II has demonstrated reliability and validity in a heterogeneous out-patient sample (Beck et al., 1996). Coefficient alpha for this study was .91.
The Experience of Shame Scale (ESS; Andrews, Qian, & Valentine, 2002)
The ESS is a 25-item questionnaire that assesses characterological, behavioral, and bodily shame over the past month. Participants rate each item on a scale ranging from 1 (not at all) to 4 (very much), with higher scores indicating greater shame. The ESS has demonstrated reliability and validity, including internal consistency reliability of .92 for the total score and construct validity as demonstrated by the questionnaire’s relationship with an alternate measure of shame (Andrews et al., 2002). Coefficient alpha for this study was .96.
The Personal Beliefs and Reactions Scale (PBRS; Mechanic & Resick, 1999)
The PBRS examines trauma-related beliefs. The PBRS is a 50-item measure that assesses disruptions in beliefs concerning self-blame, safety, trust, control, esteem, and intimacy. Only total score was used here. Each item is rated on a scale ranging from 1 (not true at all) to 6 (completely true). Higher scores on the PBRS reflect less distorted cognitions. Previous research with the PBRS has indicated that cognitions change with successful treatment (Owens, Pike, & Chard, 2001). Mechanic and Resick (1999) found acceptable internal consistency with subscale alpha coefficients ranging from .62 to .81. Test–retest reliability was .81. Concurrent validity was also demonstrated. Coefficient alpha for total score in the study was .90
Posttraumatic Diagnostic Scale (PDS; Foa, 1995)
The PDS is a 49-item self-report measure that assesses trauma history and all DSM–IV criteria for the diagnosis of PTSD. Respondents rate the frequency of each symptom item on a scale ranging from 0 to 3, with higher scores indicating greater frequency of symptoms. The PDS has demonstrated reliability and validity with a heterogeneous trauma group (Foa, Cashman, Jaycox, & Perry, 1997). Coefficient alpha for this study was .88.
State-Trait Anger Expression Inventory (STAXI; Speilberger & Sydeman, 1994)
The STAXI is a 44-item measure that assesses several components of anger. In the current study, we examined anger suppression (“Anger In”) and aggressive anger expression (“Anger Out”). The anger components examined in this study have demonstrated reliability and validity, including internal consistency reliability ranging from .73 to .84 and a theoretically consistent factor structure (Speilberger, Sydeman, Owen, & Marsh, 1999). In this study, coefficient alpha for Anger In was .79 and for Anger Out was .81.
State-Trait Anxiety Inventory (STAI; Speilberger, 1970)
The STAI is a 40-item measure that assesses state and trait anxiety. The STAI has demonstrated reliability and validity (Spielberger et al., 1999). For this study, coefficient alphas were .95 for state anxiety and .92 for trait anxiety.
Therapeutic Outcome Questionnaire
This questionnaire (Foa et al., 1991), an adaptation of Borkovec and Nau’s (1972) scale, measures the perceived credibility of each active treatment. Toward this end, there were four brief questions asked at the first session after the therapy had been explained At posttreatment, the questions were asked again querying the perception of the client regarding the success of the intervention in reducing symptoms.
Trauma-Related Guilt Inventory (TRGI; Kubany et al., 1996)
The TRGI is a 32-item questionnaire that assesses several components of trauma-related guilt. Items are scored on a 5-point scale ranging from 1 (never/not at all true) to 5 (always/extremely true). In this study, we examined Guilt Cognitions that consists of 22 items. The Guilt Cognitions subscale has demonstrated reliability and validity, including internal consistency reliability of .86 and moderate correlations with PTSD and depression symptoms in a trauma sample (Kubany et al., 1996). In this study, Cronbach’s alpha was .89.
Therapists and Training
Therapists included eight women with master’s degrees or doctorates in clinical psychology and training in cognitive behavior therapy. Client assignments were balanced so each therapist conducted approximately equal numbers of therapy cases in each condition. After the therapists read the treatment manuals, there was a 1-day training workshop for each condition conducted by Patricia A. Resick or a senior staff member. Additionally, the therapists watched clinical training tapes of the therapy being conducted and then conducted therapy on 2 clients in each of the conditions as pilot participants prior to conducting therapy with the study sample. Throughout the study, all sessions were videotaped and therapy was closely supervised by the primary investigator and project directors with weekly group supervision sessions to ensure competence and adherence to the protocols.
Treatment Adherence and Competence
Independent raters, all trained in CPT and provided with the CPT, CPT-C, and WA manuals, who were not otherwise involved in the project, conducted assessments of treatment adherence and therapist competence. All therapy sessions were videotaped and were available for random selection for rating. We conducted ratings using rating forms developed for this project that included sections on unique and essential elements specific to each session, essential but not unique elements, acceptable but not necessary elements, and proscribed elements for each therapy (Nishith & Resick, 1994, 2000; Weaver & Nishith, 2000). The number of items potentially rated for each session and across the three therapies varied depending upon the goals and specifics of the protocol for each therapy, but generally there were 3–10 unique and essential items for each session (63–69 items total), 8 essential but not unique elements, and 3–5 proscribed elements. For adherence, the element was scored whether or not it occurred, whereas for competence, a rating was made on a 7-point scale ranging from 1 ( poor) to 7 (excellent), with satisfactory at the midpoint. Because sessions were drawn randomly from only a portion of possible clients, the sample sizes for any given session were too small to analyze meaningfully across groups. There was only one item that the three fidelity ratings had in common for every client rated, an overall rating of the therapist’s skill across the sessions that were rated for that client, ranging from 1 ( poor) to 7 (excellent), with satisfactory at the midpoint. The rest of the ratings were aggregated across sessions within type of therapy.
Adherence and competence ratings were conducted on 29 clients from the ITT sample for whom up to three randomly chosen sessions were rated as available. In other words, a rater viewed up to three randomly selected sessions for each of the randomly selected clients who had completed at least one session. Of the 1,031 total therapy sessions, 89 were rated, and 12 of the sessions were double-rated for reliability. The number of different sessions rated for each therapy included 30 for CPT, 29 for WA, and 30 for CPT-C.
Regarding adherence to CPT, 90% of unique and essential elements were included in all sessions, and there were no violations of the protocols regarding proscribed elements. There was 97% agreement between the raters across all items and sessions. For unique and essential elements on WA adherence, there was 80% adherence to the protocol across all sessions, and for proscribed elements, there were two violations on proscribed elements. There was 85% agreement between the raters across all items. The lower nonadherence in this condition was primarily due to one therapist, but the elements that were omitted were minor items. The CPT-C adherence for unique and essential elements was 90% adherence to the protocol across all sessions, and there were no protocol violations on proscribed elements. There was 100% agreement between the raters across all items.
The competence of the therapists was rated on all of the unique and essential components for each session rated, and an overall therapist skill rating was given for the three sessions that were rated for a client. For CPT (198 items), 80% of the unique and essential component items were rated as satisfactory or better, and 100% of the sessions were rated satisfactory or better on overall therapist skill. For WA (274 items), 83% of the unique and essential components and 93% of the tapes on overall therapist skill were rated satisfactory or better. For CPT-C (164 items), 83% of unique and essential items and 100% of the tapes on overall therapist skill were rated satisfactory or better. The differences in overall therapist skill across the three therapies were not statistically significant.
Design and Treatment Overview
In accordance with the dismantling design of the study, participants were randomly assigned to CPT, CPT-C, or WA. The treatments were scheduled to be completed within 6 weeks and were equated for amount of therapy time (i.e., 12 hr), but they were delivered slightly differently. CPT and CPT-C consisted of 12 sessions, each 60 min in length, conducted two times per week. WA had, in the 1st week, two separate 60-min sessions; thereafter, the sessions were 2 hr in length and held once a week, for a total of seven sessions. An upper limit for therapy completion was established to maintain the integrity of the protocols; if participants did not complete the treatment within 12 weeks, treatment was terminated, and they were assessed 2 weeks later regardless of the amount of treatment they had received.
Following a brief telephone screen, potential participants were scheduled for assessment. Prior to assessment, potential participants signed consent to participate in the study, understanding they would not continue to participate in the treatment portion of the study if they met the exclusion criteria or did not meet the inclusion criteria. After assessments were conducted and participants were accepted into treatment, they were randomly assigned to one of the three treatments by the data manager (the investigators and assessors were blind as to assignment and assessors continued to be blind to condition throughout the trial). Posttreatment assessments were conducted 2 weeks after the conclusion of treatment (or, if a participant stopped treatment prior to the prescribed number of sessions, 2 weeks after treatment would have ended) and 6 months after the end of treatment. Data collection occurred between October 2000 and August 2005.
CPT
CPT followed the manual as written by Resick and Schnicke (1993), but updated by Resick (2001a) to include more generic wording on all of the forms. CPT is a highly structured protocol in which the client learns the skill of recognizing and challenging dysfunctional cognitions, first about the worst traumatic event and then later with regard to the meaning of the events for current beliefs about self and others. Session 1 begins with education about PTSD, an overview of and rationale for treatment, and an assignment to write an impact statement about the meaning of the index event to the client. After reading and discussing the meaning of the event (Session 2), clients are introduced to identification of and relationship between events, thoughts, and emotions. At the end of Session 3, clients are assigned to write a detailed account of the most traumatic event. Clients are encouraged to experience their emotions as they write their account and read it back to themselves daily. Unlike the WA condition described below, clients do not record discomfort levels. The client reads the account to the therapist in Session 4, and the remainder of the session focuses on cognitive therapy with Socratic questions regarding self-blame and other distortions regarding the event. At the close of Session 4, clients are instructed to rewrite the account as homework. The account is again processed during Session 5. Writing about a second trauma may occur after Session 5, but the focus of therapy shifts to teaching clients to challenge and change their beliefs about the meaning of the event and the implications of the trauma for their lives.
Clients are first taught to challenge a single thought by asking themselves a series of questions. They are then taught to identify problematic patterns of thinking that have become a style of responding. From that point, beginning with Session 7, clients begin to use more advanced worksheets that incorporate the earlier worksheets and that ask the clients to develop and practice alternative, more balanced self-statements. From Sessions 7 to 12, clients are also asked to focus on one theme each week to correct any overgeneralized beliefs related to that theme: safety, trust, power/control, esteem, and intimacy. At Session 11, clients are also asked to rewrite their impact statements to reflect their current beliefs, which are then used in the final session to evaluate gains made in treatment and areas on which the client wishes to continue working.
CPT-C
The CPT-C protocol was identical to full CPT except for the exclusion of the WA component. At Session 3, instead of being assigned the account to write, participants were assigned to complete event–thought– emotion (A–B–C) worksheets again for homework. At Session 4, they moved on to challenging questions. The work of Session 7 was divided into two sessions so that the total number of sessions and hours of treatment equaled 12.
WA
The configuration for WA was developed to maintain integrity for the spirit of that component of the protocol. In CPT, the participants write their accounts at home, using as much time as needed and then read it back to the therapist in session, which takes only a few minutes. However, to ensure that the participants spent some minimal amount of time writing in this study and to ensure that they had 12 hrs in sessions, we asked participants in WA to write in-session. The WA protocol expanded upon the exposure component of CPT such that the first two 1-hr sessions were comprised of overview of treatment and education regarding PTSD and instruction regarding subjective units of distress (SUDS) anchoring as well as assault script construction. In the remaining five sessions, participants were oriented for the first 15 min of the session with homework review and discussion of the upcoming writing assignment. They were stationed alone in a room for 45–60 min and asked to write about their worst trauma. The participants were asked to give a SUDS rating at the beginning and end of the writing period and to rate the peak emotions during the writing session.
At the end of the writing period, the therapist returned to the room and asked the participant to read her trauma account aloud. After this was completed, the therapist elicited the client’s responses regarding emotions, reviewed what she had learned from the assignment, and discussed which details had been added or overlooked. The therapists were allowed to make nondirective, supportive comments and occasional educational statements, but they were not allowed to engage in any cognitive therapy or challenges to the client’s dysfunctional statements. They could direct the clients to write specific portions of the account in more detail over the sessions (focusing in on “hotspots”) or move to other traumatic events if they had made good progress with the worst traumatic event. For homework, clients were asked to finish writing their accounts if they were not able to complete them during the session time. They were also asked to read their account to themselves everyday between sessions and to record their SUDS ratings. The SUDS ratings were used to identify hotspots and areas that needed further attention or to determine when to go on to other traumas.
Analysis Plan
The primary analyses of the study were conducted with the ITT (in which we continued to assess dropouts if possible). The results were analyzed three different ways for comparison purposes. Diagnostic interviews were compared by chi-square analyses with last observation carried forward for missing data at any of the follow-ups. Because the PDS and BDI–II were also collected weekly during treatment, we analyzed them—along with pre-, post- and follow-up scores (yielding nine data points)—using linear mixed-effects regression with maximum likelihood estimation (SAS PROC MIXED). Omnibus results are reported followed by planned comparisons to determine when change happens for each group and differences between groups during and after treatment. Regarding power, with the current study sample size, for repeated measures in the main analyses on PDS and BDI–II within each condition of study, we have 80% power to detect an ES of 0.46; for comparison between any two conditions, we have 80% power to detect an ES of 0.57; and for a general three-group comparison, we have 80% power to detect an ES of 0.26.
Symptom severity measures, for which we had only three data points (pretreatment, posttreatment, and 6-month follow-up), were analyzed separately with hierarchical linear modeling (HLM), which estimates missing values. Hierarchical linear and nonlinear modeling software (HLM 6.0; Scientific Software International) does not provide omnibus tests for statistical models. The analyses included the CAPS and other supplementary measures of emotions and cognitions. Women who completed all treatment sessions were analyzed separately. ESs of treatment status groups (ITT, complete therapy, partial therapy, and no therapy) are also presented.
Results
Perceived Credibility of Interventions
At pretreatment there were no differences between the three treatment conditions on the total score on the Therapeutic Outcome Questionnaire. At posttreatment there were also no significant differences between groups.
Linear Mixed-Effects Regression Analyses on PDS and BDI–II
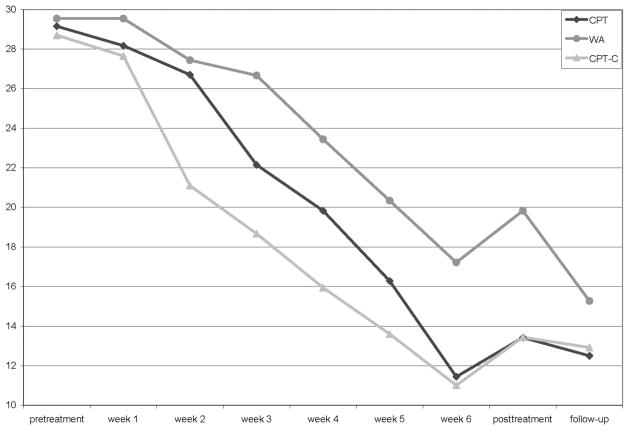
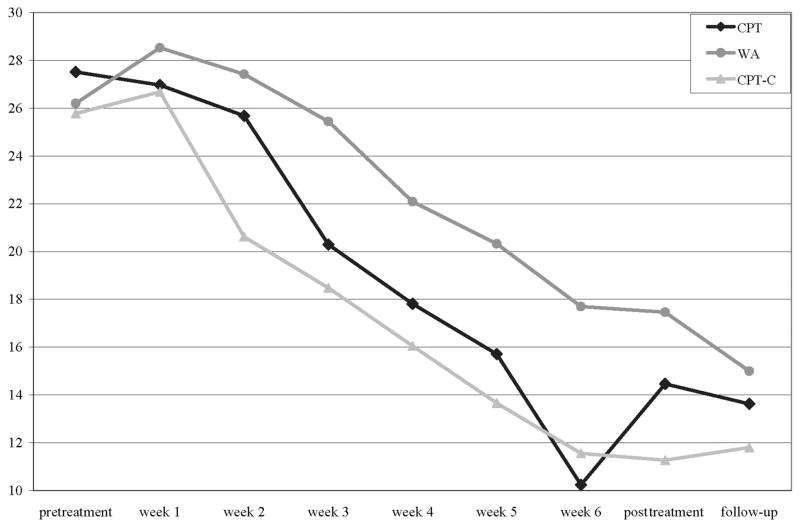
The PDS and BDI–II were collected weekly, as well as at pretreatment, 2 weeks posttreatment, and follow-up (see Table 1 for ITT sample; means and standard deviations of treatment completers can be requested from Patricia A. Resick). We analyzed the nine time periods three times with linear mixed-effects regression using maximum likelihood estimation, with exact dates of assessment, by weeks, and with time as a categorical variable. Because the results were very similar, the more parsimonious categorical presentation is included here (see Figures 2 and 3). A quadratic function also did not provide an advantage over the linear fit. There was a significant group effect for PDS, F(2, 183) = 4.5, p = .01, and BDI–II, F(2, 179) = 3.1, p = .05, indicating that overall the three groups differed. There was also a significant negative slope over time for PDS, F(1, 147) = 155.0, p = .0001, and BDI–II, F(1, 147) = 77.3, p = .0001. There was not a significant interaction between time and group in the linear categorical model. Because income differed between groups, it was included in another mixed model but did not change the results.
Table 1.
CPT, WA, and CPT-C Means, Standard Deviations, and Sample Sizes Over Time on the Posttraumatic Diagnostic Scale (PDS) and Beck Depression Inventory—II (BDI–II) With the ITT Sample
| Instrument | CPT |
WA |
CPT-C |
||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | n | M | SD | n | M | SD | n | |
| PDS | |||||||||
| Pretreatment | 29.15 | 9.54 | 53 | 29.35 | 9.72 | 48 | 28.48 | 9.51 | 46 |
| Week 1 | 28.03 | 9.72 | 48 | 29.40 | 9.67 | 40 | 28.22 | 10.42 | 36 |
| Week 2 | 26.67 | 10.25 | 36 | 26.94 | 9.61 | 36 | 21.32 | 9.37 | 34 |
| Week 3 | 21.33 | 10.03 | 33 | 26.37 | 10.15 | 35 | 18.53 | 10.95 | 32 |
| Week 4 | 18.28 | 8.42 | 29 | 22.84 | 11.82 | 31 | 15.56 | 11.92 | 32 |
| Week 5 | 14.46 | 7.58 | 28 | 18.43 | 13.15 | 30 | 12.35 | 10.65 | 31 |
| Week 6 | 9.19 | 9.89 | 27 | 14.47 | 14.53 | 30 | 10.21 | 9.74 | 29 |
| Posttreatment | 13.98 | 11.77 | 42 | 18.79 | 15.09 | 38 | 12.89 | 12.06 | 38 |
| 6-month follow-up | 12.11 | 11.94 | 44 | 14.62 | 12.57 | 39 | 12.22 | 11.42 | 36 |
| BDI–II | |||||||||
| Pretreatment | 27.51 | 11.75 | 53 | 26.31 | 10.99 | 48 | 25.72 | 11.33 | 46 |
| Week 1 | 28.15 | 11.53 | 39 | 27.58 | 10.23 | 40 | 26.82 | 10.74 | 34 |
| Week 2 | 26.64 | 11.76 | 36 | 26.11 | 10.45 | 36 | 19.97 | 10.77 | 33 |
| Week 3 | 20.39 | 11.35 | 33 | 24.40 | 13.28 | 35 | 17.78 | 13.20 | 32 |
| Week 4 | 17.34 | 11.57 | 29 | 20.77 | 13.02 | 31 | 15.13 | 12.24 | 32 |
| Week 5 | 15.03 | 11.29 | 29 | 18.47 | 15.88 | 30 | 12.10 | 11.95 | 31 |
| Week 6 | 10.26 | 9.89 | 27 | 15.40 | 15.27 | 30 | 10.31 | 11.25 | 29 |
| Posttreatment | 14.37 | 13.83 | 43 | 15.95 | 14.10 | 38 | 10.50 | 11.69 | 38 |
| 6-month follow-up | 13.16 | 13.19 | 44 | 14.21 | 14.59 | 38 | 10.78 | 13.29 | 36 |
Note. CPT = cognitive processing therapy; WA = written accounts; CPT-C = cognitive therapy only; ITT = intent-to-treat
Figure 2.
Posttraumatic Diagnostic Scale with categorical assessment interval of cognitive processing therapy (CPT), written accounts (WA), and cognitive therapy only (CPT-C).
Figure 3.
Beck Depression Inventory—2 with categorical assessment interval of cognitive processing therapy (CPT), written accounts (WA), and cognitive therapy only (CPT-C).
Comparisons at each session (least square means based on the mixed model) are depicted in Table 2 with alpha fixed at .01. CPT did not differ from CPT-C on the PDS or BDI–II. CPT differed from WA only at posttreatment on the PDS, although there was a trend at Week 6 of therapy on the PDS. CPT-C differed from WA at most assessments during treatment on the PDS, and there were trends throughout treatment on the BDI. The groups did not differ at the pretreatment and 6-month follow-up assessments.
Table 2.
Comparison of Treatment Conditions by Sessions During Treatment: Intent-to-Treat Sample
| Variable | PDS |
BDI–II |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CPT vs.WA |
CPT vs. CPT-C |
WA vs. CPT-C |
CPT vs. WA |
CPT vs. CPT-C |
WA vs. CPT-C |
|||||||
| DLSM | p | DLSM | p | DLSM | p | DLSM | p | DLSM | p | DLSM | p | |
| Pretreatment | −0.39 | .86 | 0.45 | .84 | 0.84 | .71 | 1.31 | .60 | 1.74 | .49 | 0.43 | .87 |
| Week 1 | −1.37 | .56 | 0.52 | .83 | 1.88 | .03 | −1.56 | .56 | 0.29 | .92 | 1.85 | .50 |
| Week 2 | −0.74 | .76 | 5.60 | .03 | 6.34 | .01 | −1.74 | .53 | 5.06 | .08 | 6.81 | .02 |
| Week 3 | −4.52 | .08 | 3.48 | .18 | 8.00 | .00 | −5.15 | .08 | 1.81 | .54 | 6.96 | .02 |
| Week 4 | −3.62 | .18 | 3.89 | .15 | 7.50 | .01 | −4.27 | .16 | 1.76 | .56 | 6.03 | .05 |
| Week 5 | −4.07 | .13 | 2.67 | .32 | 6.74 | .01 | −4.61 | .13 | 2.06 | .50 | 6.67 | .03 |
| Week 6 | −5.78 | .03 | 0.43 | .87 | 6.21 | .02 | −7.46 | .01 | −1.32 | .66 | 6.14 | .04 |
| Posttreatment | −6.41 | .01 | −0.02 | .99 | 6.39 | .01 | −2.99 | .27 | 3.19 | .25 | 6.19 | .03 |
| 6-month follow-up | −2.76 | .25 | −0.41 | .87 | 2.35 | .35 | −1.37 | .61 | 1.82 | .51 | 3.19 | .26 |
Note. Positive numbers indicate that the therapy listed first had worse outcomes (higher Posttraumatic Diagnostic Scale [PDS] or Beck Depression Inventory—II [BDI–II] scores) at that assessment. If the difference between the least square means between the two types of treatment is negative, then the first therapy listed had lower scores (better outcomes). Significance was set at p = .01. CPT = cognitive processing therapy; WA = written accounts; CPT-C = cognitive therapy only; DLSM = differences of least square means.
Regarding when significant change occurs during treatment, we conducted multiple paired t tests, comparing PDS and BDI–II at each week against baseline scores for each group with Tukey–Kramer adjustment for multiple testing. On the PDS, there was significant improvement by Week 2 in the CPT-C group ( p = .001), by Week 3 in the CPT group ( p = .02), and at Week 5 for the WA group ( p = .005; refer to Figure 2). On the BDI–II, there was significant improvement at Week 3 for the CPT-C group ( p = .006), at Week 4 for the CPT group ( p = .005), and at Week 6 for the WA group ( p = .04; refer to Figure 3).
To examine the effects of therapy according to treatment status, we use Table 3 to display Hedges’ g over time, used here to adjust for small sample sizes (Hedges, 1982), on the PDS and BDI–II on the basis of the least square means for four different samples with the formula , using the total ITT sample (n = 150), treatment completers (n = 86), those who received partial therapy (n = 40), and those who received no therapy but just assessments (n = 24). There were large ESs over time for the ITT and completer samples, medium ESs for the partially treated samples, and small ESs for those who only participated in assessments but attended no therapy.2
Table 3.
Effect Sizes (Hedges’ g) Over Time on the PDS and BDI–II: CPT, WA, and CPT-C
| Treatment type | Intent-to-treat (n = 150) |
Completers (n = 86) |
Partial treatment (n = 40) |
Not treated (n = 24) |
||||
|---|---|---|---|---|---|---|---|---|
| Post | 6 months | Post | 6 months | Post | 6 months | Post | 6 months | |
| PDS | ||||||||
| CPT | 1.1 | 1.2 | 0.9 | 0.8 | 0.7 | 0.7 | 0.0 | 0.3 |
| WA | 0.7 | 1.0 | 0.7 | 0.9 | 0.2 | 0.4 | 0.2 | 0.4 |
| CPT-C | 1.1 | 1.1 | 0.9 | 0.9 | 0.5 | 0.5 | 0.3 | 0.4 |
| BDI–II | ||||||||
| CPT | 1.0 | 1.2 | 1.0 | 1.1 | 0.7 | 0.5 | 0.0 | 0.1 |
| WA | 0.7 | 1.0 | 0.7 | 0.8 | 0.2 | 0.4 | 0.0 | 0.4 |
| CPT-C | 1.2 | 1.3 | 1.2 | 1.1 | 0.5 | 0.4 | 0.1 | 0.4 |
Note. PDS = Posttraumatic Diagnostic Scale; BDI–II = Beck Depression Inventory—II; CPT = cognitive processing therapy; WA = written accounts; CPT-C = cognitive therapy only.
Diagnostic Interviews
On the CAPS interview for the assessment of PTSD, all participants were positive for PTSD at pretreatment. For the ITT sample at posttreatment, with last observation carried forward for missing data, there was a trend for a difference between groups, χ2(2, N = 150) = 5.6, p = .06, with 45.3% of the CPT, 58.0% of the WA, and 34.0% of the CPT-C group meeting PTSD diagnostic criteria. At the 6-month follow-up, there were no significant differences in diagnostic status among the groups, with 39.6% (CPT), 44.0% (WA), and 38.3% (CPT-C) meeting criteria for PTSD, respectively. Also with last observation carried forward, for treatment completers there were no differences between treatment groups at any time point. On the CAPS at posttreatment, 29.6% of CPT, 36.7% of WA, and 20.7% of CPT-C participants continued to meet the criteria for PTSD. At the 6-month follow-up, 25.9% of CPT, 26.7% of WA, and 20.7% of CPT-C participants still met criteria for PTSD.
On the SCID interview, 50% of the women in the ITT sample were diagnosed with current MDD at pretreatment, and there were no significant differences between groups. At posttreatment and 6-month follow-up, there were also no significant differences between groups, with 24.0% of the entire sample meeting criteria at posttreatment and 20.7% at the 6-month follow-up. On panic disorder, 13.3% of the entire sample met criteria at pretreatment, 12% at posttreatment, and 12.7% at the 6-month follow-up, with no differences between groups at any time point.
Like the ITT sample, 51.2% of the treatment completers were diagnosed with current major depression (MDD) at pretreatment, whereas 16.3% continued to meet criteria for MDD at posttreatment, and 12.8% continued to meet criteria for MDD at the 6-month follow-up. For panic disorder, 21.2% met criteria at pretreatment, 11.6% at posttreatment, and 7.0% at the 6-month follow-up. There were no differences between groups on these measures.
CAPS Severity
Raw means and standard deviations for each group at each assessment for the ITT sample are listed in Table 4 (data on completers are available from Patricia A. Resick), and ESs are listed in Table 5 for the CAPS and secondary analyses of the study. Analyses were conducted on pre-, post-, and 6-month follow-up scores by HLM. First, both WA and CPT-C were compared with CPT, and then WA and CPT-C were compared with each other. In each case, CAPS scores decreased significantly over time but did not differ between groups for both the ITT and completer samples. On ITT analyses with HLM, CAPS decreased 36.1 points on average from baseline ( p < .001) among those receiving CPT, 31.9 points ( p < .001) among those receiving WA, and 40.8 points ( p < .001) among those in the CPT-C group. On the completer analyses (all ps < .001), CPT group decreased 37.7 points, WA group decreased 36.5 points, and CPT-C decreased 42.1 points on the CAPS.
Table 4.
CPT, WA, and CPT-C Means, Standard Deviations, and Sample Sizes Over Time on Supplementary Measures
| Measure | Treatment type | Pretreatment |
Posttreatment |
Follow-up (6 months) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | n | M | SD | n | M | SD | n | ||
| CAPS | CPT | 70.19 | 15.50 | 53 | 34.74 | 27.62 | 42 | 31.96 | 28.46 | 45 |
| WA | 70.38 | 18.65 | 50 | 44.76 | 31.55 | 38 | 35.90 | 27.09 | 40 | |
| CPT-C | 73.87 | 21.04 | 47 | 31.32 | 37.00 | 37 | 31.03 | 27.57 | 36 | |
| STAI–State | CPT | 50.67 | 12.90 | 52 | 38.36 | 12.70 | 42 | 39.30 | 14.15 | 43 |
| WA | 51.30 | 12.82 | 50 | 42.31 | 14.21 | 36 | 37.92 | 14.17 | 38 | |
| CPT-C | 50.85 | 12.82 | 47 | 35.11 | 13.62 | 38 | 36.00 | 15.03 | 36 | |
| STAI–Trait | CPT | 55.87 | 10.18 | 52 | 45.05 | 12.96 | 42 | 43.50 | 12.68 | 44 |
| WA | 56.48 | 9.95 | 50 | 46.23 | 15.42 | 35 | 43.39 | 13.02 | 38 | |
| CPT-C | 53.13 | 10.90 | 47 | 38.53 | 11.62 | 38 | 38.86 | 12.44 | 36 | |
| STAXI–Anger In | CPT | 18.67 | 4.45 | 52 | 15.69 | 3.28 | 42 | 16.55 | 4.67 | 44 |
| WA | 20.58 | 4.48 | 50 | 17.58 | 4.66 | 36 | 15.89 | 5.18 | 38 | |
| CPT-C | 18.60 | 4.34 | 47 | 15.18 | 4.14 | 38 | 15.81 | 5.06 | 36 | |
| STAXI–Anger Out | CPT | 14.87 | 3.58 | 52 | 14.40 | 3.40 | 42 | 14.23 | 3.13 | 44 |
| WA | 15.22 | 4.27 | 50 | 15.08 | 4.13 | 36 | 14.63 | 3.37 | 38 | |
| CPT-C | 14.66 | 4.26 | 47 | 13.95 | 2.59 | 38 | 13.69 | 3.86 | 36 | |
| PBRS | CPT | 159.37 | 38.50 | 52 | 213.26 | 49.92 | 42 | 217.39 | 43.96 | 44 |
| WA | 154.82 | 36.27 | 50 | 188.22 | 49.93 | 36 | 205.92 | 46.57 | 38 | |
| CPT-C | 161.45 | 39.53 | 47 | 225.21 | 40.54 | 38 | 216.50 | 48.78 | 36 | |
| ESS | CPT | 58.79 | 16.45 | 52 | 49.48 | 17.87 | 42 | 47.36 | 16.14 | 44 |
| WA | 61.00 | 19.96 | 50 | 54.09 | 20.42 | 35 | 46.71 | 15.26 | 38 | |
| CPT-C | 57.72 | 17.64 | 47 | 46.16 | 15.28 | 38 | 46.97 | 15.15 | 36 | |
| TRGI–Guilt Cognitions | CPT | 1.64 | 0.89 | 52 | 0.94 | 0.73 | 42 | 0.95 | 0.80 | 44 |
| WA | 1.81 | 0.50 | 50 | 1.13 | 0.70 | 36 | 1.09 | 0.71 | 38 | |
| CPT-C | 1.71 | 0.90 | 47 | 0.79 | 0.62 | 38 | 0.96 | 0.73 | 36 | |
Note. CPT = cognitive processing therapy; WA = written accounts; CPT-C = cognitive therapy only; CAPS = Clinician-Administered Posttraumatic Stress Disorder Scale; STAI–State = State-Trait Anxiety Inventory—State Scale; STAI–Trait = State-Trait Anxiety Inventory—Trait Scale; STAXI–Anger In = State-Trait Anger Expression Inventory—Anger Suppression Scale; STAXI–Anger Out = State-Trait Anger Expression Inventory—Anger Expression Scale; PBRS = Personal Beliefs and Reactions Scale; ESS = Experience of Shame Scale; TRGI–Guilt Cognitions = Trauma-Related Guilt Inventory—Guilt Cognitions subscale.
Table 5.
Cohen’s d Effect Sizes for Slopes Over Time: CPT, WA, and CPT-C on CAPS and Supplementary Measures for Intent-to-Treat (ITT) and Treatment Completers
| Measure | CPT |
WA |
CPT-C |
|||
|---|---|---|---|---|---|---|
| ITT | Completers | ITT | Completers | ITT | Completers | |
| CAPS | −1.68 | −2.03 | −1.54 | −1.98 | −1.82 | −2.18 |
| STAI–State | −0.93 | −0.85 | −0.92 | −1.00 | −1.05 | −1.08 |
| STAI–Trait | −1.10 | −1.20 | −1.10 | −1.25 | −1.21 | −1.38 |
| STAXI–Anger In | −0.56 | −0.72 | −0.97 | −0.97 | −0.63 | −0.76 |
| STAXI–Anger Out | −0.23 | −0.34 | −0.21 | −0.37 | −0.34 | −0.40 |
| PBRS | 1.44 | 1.71 | 1.28 | 1.61 | 1.44 | 1.72 |
| ESS | −0.94 | −0.82 | −1.02 | −0.96 | −0.92 | −0.97 |
| TRGI–Guilt Cognitions | −1.08 | −1.15 | −1.06 | −1.12 | −1.19 | −1.26 |
Note. CPT = cognitive processing therapy; WA = written accounts; CPT-C = cognitive therapy only; CAPS = Clinician-Administered Posttraumatic Stress Disorder Scale; STAI–State = State-Trait Anxiety Inventory—State Scale; STAI–Trait = State-Trait Anxiety Inventory—Trait Scale; STAXI–Anger In = State-Trait Anger Expression Inventory—Anger Suppression Scale; STAXI–Anger Out = State-Trait Anger Expression Inventory—Anger Expression Scale; PBRS = Personal Beliefs and Reactions Scale; ESS = Experience of Shame Scale; TRGI–Guilt Cognitions = Trauma-Related Guilt Inventory—Guilt Cognitions subscale.
Supplementary Measures
Also using HLM with estimates of missing data across the three time points, we examined the following measures: Anger In and Anger Out from the STAXI, State and Trait Anxiety from the STAI, ESS total, Guilt Cognitions from the TRGI, and PBRS. With one exception, all groups decreased significantly, and the three groups did not differ on either the ITT or completer samples. The exception was Anger Out, which did not change significantly over time in any of the groups but was also not elevated to clinical levels at pretreatment (Speilberger & Sydeman, 1994).
Discussion
Both components of CPT as well as the full protocol were successful in treating PTSD and other secondary symptoms in this highly traumatized and chronic sample, as evidenced by the large decreases in PTSD and depression symptoms. The results of the trial were quite similar to other trials of cognitive behavioral treatments for PTSD, with large improvements realized over the 6 weeks of treatment and maintained throughout the follow-up period. Participants improved, across conditions, not only on PTSD symptoms but also on depression, anxiety, anger, guilt, shame, and cognitive distortions. Although there was no waiting list control group in this study, there have been ample studies of chronic PTSD that indicate little change over time without active intervention (Resick, Monson, & Gutner, 2007). On the previous randomized controlled trial comparing CPT with PE, Nishith et al. (2002) examined the pattern of change during treatment and found that total PTSD scores showed a quadratic pattern in which symptoms worsened before improving in treatment. This study did not replicate those findings, and the linear fit was equal to the quadratic fit.
Contrary to predictions, the combination of cognitive therapy and WAs did not improve upon the results of either component. Moreover, in the primary analyses examining the PDS and BDI–II across the course of therapy, the CPT-C group had significantly lower PDS scores than the WA condition. The CPT condition did not differ from CPT-C or WA. This is not to say that WA did not do well, just that CPT-C performed better.
In comparing WA with two other studies of PE that had similar definitions of ITT (people were randomized into the trial prior to the first session and included in analyses even if they received no therapy), both Resick et al. (2002) and Schnurr et al. (2007) had very similar effects to WA, even though PE included in vivo as well as imaginal exposure, whereas WA only included WAs. In those studies, the PE groups had ITT pretreatment to posttreatment ESs of 1.2 (Resick et al., 2002) and 0.80 (Schnurr et al., 2007). In Resick et al.’s study, 53% of the PE participants were negative for PTSD at posttreatment, and in Schnurr et al.’s study, 41% were negative at posttreatment. In this study, the ITT pretreatment to posttreatment ES for WA was 0.7 (1.0 at the 6-month follow-up), and 42% lost their PTSD diagnosis. Repeated WAs may be an effective alternative to imaginal exposure.
Limitations of the study include a focus only on interpersonal violence and the inclusion of only female participants. Nonetheless, the study included participants with traumas occurring throughout the lifespan and complex trauma histories, which represents typical clients seen in clinical practice. Future research will be needed to replicate these findings with other forms of trauma as well as with male participants.
Another limitation is the limited power that three time points (pretreatment, posttreatment, and follow-up) provide to detect differences between three active treatments for a sample size of 150. Unfortunately, short of multisite studies, larger sample sizes are difficult to obtain, and assessment of a range of measures repeatedly during treatment can become an undue burden to the participants. The primary findings of the analyses with the PDS and BDI–II may represent a more accurate picture of the results because of the greater number of data points available for analysis. A third limitation of the study was the need to alter the WA component such that it was no longer identical in structure to the component that exists in CPT; the expansion to a full protocol that could stand alone may have made this condition less viable as a dismantling comparison. In contrast, the comparison between CPT and CPT-C presented a more effective dismantling comparison because the WAs could be eliminated from the full protocol without fundamentally altering the structure of the cognitive therapy.
Although findings of this dismantling study as well as the examination of change trajectories need to be replicated, there are several tentative conclusions that can be drawn. First, consistent with prior studies, participants improved on PTSD and depression across all three conditions. On the two measures of PTSD and depression that were available throughout the course of treatment and follow-up, CPT-C proved to be more effective and more efficient than repeatedly writing and reading accounts. Participants improved on most of the supplementary measures of symptoms and functioning included in this study, whether assessed by standardized assessor interviews or self-report scales across the three conditions. The sole exception was Anger Out, which either did not change because it was not problematic to begin with in this sample or because for victims of interpersonal violence, anger at the perpetrator is appropriate and would not have been targeted for change by the therapists. In a recent meta-analysis examining the relationship between anger and PTSD, Orth and Wieland (2006) found that Anger Out was less associated with PTSD (ES = 0.29) than Anger In (ES = 0.53).
Although Foa et al.’s (2005) study, which added CR to PE, concluded that CR did not add to the effectiveness of PE, there also appears to be no distinct advantage in including extended exposures of the traumatic memory in CPT. This finding is consistent with the findings of Bryant et al. (2003), Foa et al. (1991, 1999, Marks et al. (1998), and Tarrier et al. (1999), who found that exposure was no more effective than cognitive therapy or stress inoculation in treating PTSD. Perhaps the more interesting question in the future will be to determine whether there are particular types of PTSD clients or particular comorbidity patterns that will benefit better from one type of treatment or the other or whether there are important mediators of treatment change that could be targeted. Examination of predictors of treatment outcome might pick up more subtle patterns of response that are washed out in the straight head-to-head comparisons. Future research should also focus on the efficiency of various treatments and when change is most likely to occur.
This study joins the growing body of research that has found cognitive therapy alone to be at least as effective as exposure in the treatment of PTSD (Ehlers et al., 2003; Marks et al., 1998; Paunovic & Öst, 2001; Tarrier et al., 1999; Tarrier & Sommerfield, 2004). Nevertheless, on the basis of just one dismantling study, we would not recommend eliminating the WA component from the CPT protocol in all cases. Some may need to reconstruct the event and/or access emotions that have been particularly avoided. However, for those clients who are unwilling to undergo exposure-based treatments or only have a few sessions to attend treatment, cognitive therapy may be the treatment of choice. CPT was originally developed as a group treatment (Resick & Schnicke, 1992, 1993). Implementing the cognitive-only version of the protocol may eliminate the problems that are sometimes encountered trying to implement exposure treatment in a group format.
The comparison of ESs in different treatment status conditions indicates that there does appear to be a dose-response relationship in amount of therapy one receives. The assessments themselves may have had a small effect because of the repeated questioning about symptoms and thoughts about the traumatic events, as well as script generation and psychophysiological assessment (not reported here) in a warm supportive environment. Partial therapy had a moderate effect, and completing the full course of treatment had large effects. Notably, not completing the full course of treatment was also associated with being low income and African American. Although beyond the scope of the present article, attention to race, income, and the barriers/facilitators of engaging in treatment should be the focus of future research, and race will be examined in depth in a separate article from this study.
This was the first study to examine a WA protocol that was set up to parallel prolonged imaginal exposure, with writing assignments focusing on the worst traumatic event, reading and processing the account with the therapist, and homework to reread the traumatic event daily. The fact that this protocol was also successful in reducing symptoms has potential for use by therapists who are less skilled in cognitive therapy or when therapist access is limited, such as in rural areas or when the need is great, such as in postdisaster environments. Although this modality requires further testing, therapists could possibly assign writing and discuss the account with the client over the telephone, redirect the focus to specific parts of the account that were omitted, provide support for completing assignments, and so forth without the level of skill that may be needed for cognitive interventions. Lange et al. (2003) have developed an Internet-based therapy, Interapy, which shares some similarities to WA, with written exposures, appears to be very promising.
Theoretically, this study supports the idea that alteration in the meaning of the traumatic event may be an active mechanism of change and that systematic and extensive exposure to the trauma memory may not be a necessary condition of treatment. Most theories of PTSD recovery propose that repeated exposure to the trauma memory is needed for habituation of a fear response, to facilitate restructuring of unhelpful fear appraisals, or to activate situationally accessible memories (Brewin et al., 1996; Cahill & Foa, 2007; Foa & Kozak, 1986). It is possible that a cognitive therapy that focuses not only on current cognitions and appraisals of future danger but also on the traumatic events themselves, along with a broader array of associated cognitions, may be able to promote change more directly. This trauma focus also addresses not just fear but also sadness, anger, shame, and guilt, which Dalgleish (2004) has pointed out are retrospective emotions (looking back at the trauma rather than fear, which is more current and future oriented) and therefore less amenable to change through repetitious exposure. An important topic for future research will be the examination of mediators of change in treatment.
It has been assumed that repeated activation of fear is necessary for change in PTSD treatment but that assumption has only been tested with exposure-based treatments (Foa, Riggs, Massie, & Yarczower, 1995; Pitman, Orr, Altman, & Longpre, 1996). In this study, we did not examine whether the CPT-C group experienced the same level of emotional activation (although emotions were certainly encouraged) as the two interventions that included WAs, which explicitly evoked emotional engagement and imagery. Future researchers should examine further whether fear engagement is actually needed and whether, or to what extent, intervening with trauma-related cognitions directly without ensuring emotional activation is sufficient for improvement in symptoms. If high levels of fear activation and emotional processing are not needed for symptom reduction, then there may be a more direct route to symptom improvement through change in cognitions, potentially resulting in shorter or more palatable treatments that can be implemented in group as well as individual settings.
Acknowledgments
This work was supported by National Institute of Mental Health Grant 2-R01-MH51509 awarded to Patricia A. Resick at the University of Missouri—St. Louis. We thank all of the therapists, assessors, research assistants, and fidelity raters who worked on this project, as well as the participants who were willing to share their experiences and receive therapy in the context of a research project. Special thanks to Jaimie Gradus for her work on data analysis for this project.
Footnotes
One participant was admitted through assessor error and 1 participant because she did not admit it until her participation ended. Both were discovered after analyses were underway or completed; they are both included in the analyses.
To assist with the interpretation of ESs, Cohen (1988) has proposed a set of qualitative descriptors to accompany individual ESs. Demarcation between descriptors is meant to be approximate rather than absolute in nature. Small ESs are operationally defined as .2; medium ESs as .5, and large ESs as .8 (Cohen, 1988).
Contributor Information
Patricia A. Resick, Women’s Health Sciences Division, National Center for PTSD, Veterans Affairs Boston Healthcare System, and Departments of Psychiatry and Psychology, Boston University
Mary O’Brien Uhlmansiek, Human Research Protection Office, Washington University School of Medicine.
Gretchen A. Clum, Department of Community Health Sciences, Tulane University School of Public Health and Tropical Medicine
Tara E. Galovski, Center for Trauma Recovery and Department of Psychology, University of Missouri—St. Louis
Christine D. Scher, Department of Psychology, California State University, Fullerton
Yinong Young-Xu, Executive Division, National Center for PTSD, Veterans Affairs Medical Center, White River Junction, Vermont.
References
- Ahrens J, Rexford L. Cognitive processing therapy for incarcerated adolescents with PTSD. Journal of Aggression, Maltreatment, and Trauma. 2002;6:201–216. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Andrews B, Qian M, Valentine JD. Predicting depressive symptoms with a new measure of shame: The Experience of Shame Scale. British Journal of Clinical Psychology. 2002;41:29–42. doi: 10.1348/014466502163778. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Berger AM, Knutson JF, Mehm JG, Perkins KA. The self-report of punitive childhood experiences of young adults and adolescents. Child Abuse and Neglect. 1988;12:251–262. doi: 10.1016/0145-2134(88)90033-6. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Klauminzer G, Charney DS, et al. A clinician rating scale for assessing current and lifetime PTSD: The CAPS-1. The Behavior Therapist. 1990;18:187–188. [Google Scholar]
- Borkovec TD, Nau SD. Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry. 1972;3:257–260. [Google Scholar]
- Brewin CR, Dalgleish T, Joseph S. A dual representation theory of posttraumatic stress disorder. Psychological Review. 1996;103(4):670–686. doi: 10.1037/0033-295x.103.4.670. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Moulds ML, Guthrie RM, Dang ST, Nixon RDV. Imaginal exposure alone and imaginal exposure with cognitive restructuring in treatment of posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2003;71(4):706–712. doi: 10.1037/0022-006x.71.4.706. [DOI] [PubMed] [Google Scholar]
- Cahill SP, Foa EB. Psychological theories of PTSD. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and practice. New York: Guilford Press; 2007. pp. 57–77. [Google Scholar]
- Chard KM. An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2005;73:965–971. doi: 10.1037/0022-006X.73.5.965. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Dalgleish T. Cognitive approaches to posttraumatic stress disorder: The evolution of multirepresentational theorizing. Psychological Bulletin. 2004;130(2):228–260. doi: 10.1037/0033-2909.130.2.228. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38(4):319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M, Herbert C, Mayou R. A randomized controlled trial of cognitive therapy, a self-help booklet, and repeated assessments as early interventions for posttraumatic stress disorder. Archives of General Psychiatry. 2003;60:1024–1032. doi: 10.1001/archpsyc.60.10.1024. [DOI] [PubMed] [Google Scholar]
- Feindler EL, Rathus JH, Silver LB. Assessment of family violence: A handbook for researchers and practitioners. Washington, DC: American Psychological Association; 2003. [Google Scholar]
- First M, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM–IV (SCID) New York: New York State Psychiatric Institute, Biometrics Research Department; 1996. [Google Scholar]
- Foa EB. Posttraumatic Stress Diagnostic Scale (manual) Minneapolis, MN: National Computer Systems; 1995. [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9(4):445–451. [Google Scholar]
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology. 1999;67(2):194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Cahill SE, Rauch SAM, Riggs DS, Feeny NC, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73(5):953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Jaycox LH. Cognitive-behavioral theory and treatment of posttraumatic stress disorder. In: Spiegel ID, editor. Efficacy and cost-effectiveness of psychotherapy. Washington, DC: American Psychiatric Association; 1999. pp. 23–61. [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Massie ED, Yarczower M. The impact of fear activation and anger on the efficacy of exposure treatment for posttraumatic stress disorder. Behavior Therapy. 1995;26(3):487–499. [Google Scholar]
- Foa EB, Rothbaum B, Riggs D, Murdock T. Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59:715–723. doi: 10.1037//0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- Hedges LV. Estimation of effect size from a series of independent experiments. Psychological Bulletin. 1982;97:490–499. [Google Scholar]
- Keane TM, Barlow DH. Posttraumatic stress disorder. In: Barlow DH, editor. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York: Guilford Press; 2002. pp. 418–453. [Google Scholar]
- Kubany ES, Haynes SN, Abueg FR, Manke FP, Brennan JM, Stahura C. Development and validation of the Trauma-Related Guilt Inventory (TRGI) Psychological Assessment. 1996;8(4):428–444. [Google Scholar]
- Lange A, Rietdijk D, Hudcovicova M, van de Ven J, Schrieken B, Emmelkamp PM. Interapy: A controlled randomized trial of the standardized treatment of posttraumatic stress through the Internet. Journal of Consulting and Clinical Psychology. 2003;71(5):901–909. doi: 10.1037/0022-006X.71.5.901. [DOI] [PubMed] [Google Scholar]
- Marks I, Lovell K, Noshirvani H, Livanou M, Thrasher S. Treatment of posttraumatic stress disorder by exposure and/or cognitive restructuring: A controlled study. Archives of General Psychiatry. 1998;55:317–325. doi: 10.1001/archpsyc.55.4.317. [DOI] [PubMed] [Google Scholar]
- Mechanic MB, Resick PA. Unpublished manuscript. University of Missouri; St. Louis: 1999. The Personal Beliefs and Reactions Scale: Assessing rape related cognitions. [Google Scholar]
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2006;74(5):898–907. doi: 10.1037/0022-006X.74.5.898. [DOI] [PubMed] [Google Scholar]
- Nishith P, Resick PA. Unpublished instrument. University of Missouri; St. Louis: 1994. Cognitive Processing Therapy (CPT): Therapist adherence and competence protocol. [Google Scholar]
- Nishith P, Resick PA. Unpublished instrument. University of Missouri; St. Louis: 2000. Cognitive Processing Therapy (CPT)—Cognitive Therapy Version (CPT-C): Therapist adherence and competence protocol. [Google Scholar]
- Nishith P, Resick PA, Griffin MG. Pattern of change in prolonged exposure and cognitive-processing therapy for female rape victims with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2002;70(4):880–886. doi: 10.1037//0022-006x.70.4.880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orth U, Wieland E. Anger, hostility, and posttraumatic stress disorder in trauma-exposed adults: A meta-analysis. Journal of Consulting and Clinical Psychology. 2006;74(4):698–706. doi: 10.1037/0022-006X.74.4.698. [DOI] [PubMed] [Google Scholar]
- Owens GP, Pike JL, Chard KM. Treatment effects of cognitive processing therapy on cognitive distortions of female child sexual abuse survivors. Behavior Therapy. 2001;32(3):413–424. [Google Scholar]
- Paunovic N, Öst LG. Cognitive-behavior therapy versus exposure therapy in the treatment of PTSD in refugees. Behaviour Research and Therapy. 2001;39:1183–1197. doi: 10.1016/s0005-7967(00)00093-0. [DOI] [PubMed] [Google Scholar]
- Pitman RK, Orr SP, Altman B, Longpre RE. Emotional processing and outcome of imaginal flooding therapy in Vietnam veterans with chronic posttraumatic stress disorder. Comprehensive Psychiatry. 1996;37(6):409–418. doi: 10.1016/s0010-440x(96)90024-3. [DOI] [PubMed] [Google Scholar]
- Resick PA. Unpublished instrument. University of Missouri; St. Louis: 2001a. Cognitive Processing Therapy: Generic manual. [Google Scholar]
- Resick PA. Stress and trauma. 1. Hove, United Kingdom: Psychology Press; 2001b. [Google Scholar]
- Resick PA, Jordan CG, Girelli SA, Hutter CK, Marhoeder-Dvorak S. A comparative outcome study of behavioral group therapy for sexual assault victims. Behavior Therapy. 1988;19:385–401. [Google Scholar]
- Resick PA, Monson CM, Gutner C. Psychosocial treatments for PTSD. In: Friedman MJ, Keane TM, Resick PA, editors. PTSD: Science and practice—A comprehensive handbook. New York: Guilford Press; 2007. pp. 330–358. [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive processing therapy, prolonged exposure, and a waiting condition for the treatment of posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology. 1992;60:748–756. doi: 10.1037//0022-006x.60.5.748. [DOI] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for rape victims: A treatment manual. Newbury Park, CA: Sage; 1993. [Google Scholar]
- Rowan AB, Foy DW, Rodriguez N, Ryan S. Posttraumatic stress disorder in a clinical sample of adults sexually abused as children. Child Abuse and Neglect. 1994;18(1):51–61. doi: 10.1016/0145-2134(94)90095-7. [DOI] [PubMed] [Google Scholar]
- Schnurr PP. The rocks and hard places in psychotherapy outcome research. Journal of Traumatic Stress. 2007;20:779–792. doi: 10.1002/jts.20292. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea T, Chow BK, et al. Cognitive-behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. Journal of the American Medical Association. 2007;297:820–830. doi: 10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- Schulz PM, Resick PA, Huber LC, Griffin MG. The effectiveness of cognitive processing therapy for PTSD with refugees in a community setting. Cognitive and Behavioral Practice. 2006;13:322–331. [Google Scholar]
- Speilberger CD. STAI: Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- Speilberger CD, Sydeman SJ. State-Trait Anxiety Inventory and State-Trait Anger Expression Inventory. In: Maruish ME, editor. The use of psychological testing for treatment planning and outcome assessment. Hillsdale, NJ: Erlbaum; 1994. pp. 292–321. [Google Scholar]
- Spielberger CD, Sydeman SJ, Owen AE, Marsh BJ. Measuring anxiety and anger with State-Trait Anxiety Inventory (STAI) and State-Trait Anger Expression Inventory (STAXI) In: Maruish ME, editor. The use of psychological tests for treatment planning and outcome assessment. 2. Hillsdale, NJ: Erlbaum; 1999. pp. 993–1022. [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The Conflict Tactics (CT) Scales. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scale (cts2) Journal of Family Issues. 1996;17:283–316. [Google Scholar]
- Tarrier N, Pilgrim H, Sommerfield C, Faragher B, Reynolds M, Graham E, et al. A randomized trial of cognitive therapy and imaginal exposure in the treatment of chronic posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1999;67(1):13–21. doi: 10.1037//0022-006x.67.1.13. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Sommerfield C. Treatment of chronic PTSD by cognitive therapy and exposure: 5-year follow-up. Behavior Therapy. 2004;35:231–246. [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician--Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13(3):132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weaver T, Nishith P. Unpublished instrument. University of Missouri; St. Louis: 2000. Written Account Therapy (WA): Therapist adherence and competence protocol. [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, et al. The collaborative longitudinal personality disorders study: Reliability of Axis I and Axis II diagnoses. Journal of Personality Disorders. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]