Abstract
Background
Conservative treatment was long recommended for midclavicular fractures because of the excellent results that were reported in the 1960’s and 70’s. Recently, however, the rucksack bandage has received competition from surgical treatment. The spectrum of operations ranges from classic plate osteosynthesis to intramedullary techniques and angle-stable implants.
Methods
We present and evaluate the current treatment options on the basis of a selective review of the literature.
Results
Recent studies have confirmed some long-held concepts and refuted others. The risk of non-union after conservative treatment was previously reported as 1% to 2% but has turned out to be much higher in selected subgroups such as in patients with severe displacement, female patients, and patients of advanced age. Furthermore, new implants and techniques have made surgery safer and more likely to result in bony union.
Conclusion
In any case of midclavicular fracture, the type of fracture should be precisely analyzed and an individual treatment strategy should be developed in view of the patient’s particular situation. Current studies show with a high level of evidence (level 1) that patients with dislocated fractures benefit from surgery.
Midclavicular fractures heal without the doctor, with the doctor, and despite the doctor!” Although this maxim never found its way unto the scientific literature it held sway for many years, with the result that very few patients underwent surgery. Particularly in the past 10 years, however, surgical treatment options have gained increasing importance, with the result that closer attention is being paid to this “trivial” injury. This interest has culminated in the publication of several studies with high levels of evidence. In this review we set out to examine the old maxim in light of recent findings. On the basis of a selective survey of the literature, particular consideration is accorded to recent studies with high evidence levels.
Epidemiology
Midclavicular fracture is one of the most common injuries of the skeleton, representing 3% to 5% of all fractures and 45% of shoulder injuries (1, 2, e1). The annual incidence of midclavicular fracture in Europe is 64 per 100 000 population (e1). Breaks of the shaft form 70% to 80% of all clavicular fractures; lateral fractures contribute 15% to 30%, and medial fractures, at 3%, are relatively rare. Open clavicular fracture is an absolute rarity, found in only 0.1% to 1% of cases. The rate of midclavicular fractures is more than twice as high in men as in women. The peak incidence occurs in the third decade of life. About 10% of patients have significant accompanying injuries, most frequently vertebral fractures, other shoulder girdle injuries, or broken ribs (e2).
Mechanism of injury
Most midclavicular fractures in young adults are incurred during sports or in vehicle accidents, while falls are typically responsible in children and older adults. Recent biomechanical studies have shown that apart from direct blows to the clavicular shaft, the fractures are caused more by the impact of blunt trauma on the acromion, resulting in flexion of the clavicle between the acromioclavicular and sternoclavicular joints, than by falls onto the outstretched hand (1, 3, 4, e2).
Diagnosis
Detection of isolated midclavicular fractures generally poses no problems, because when questioned the patients report typical symptoms and their complaints can be readily localized. In slim individuals the malposition caused by the fracture can often be recognized immediately. Diagnosis may not be so easy in unconscious or polytraumatized patients, especially when other injuries take priority in the initial assessment. Nevertheless, midclavicular fracture is not one of the classic overlooked fractures, because it is readily diagnosed on the obligatory chest radiograph in such patients.
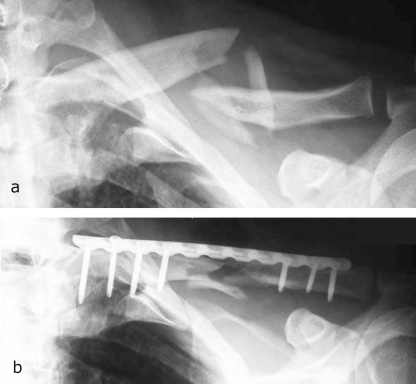
Examination of vascular, motor, and sensory function is followed by diagnostic radiology. Regardless of whether the fracture was identified on initial pyhysical examination or discovered incidentally on imaging, the clavicle should ideally be X-rayed in two projections: anteroposterior with the arm hanging down, and 45° craniocaudal. The fracture can then be correctly classified, the treatment indications determined, and the patient advised correspondingly. Recent studies clearly show that viewing midclavicular fracture as a trivial injury that almost always heals without complications and requires neither individualized diagnosis and treatment nor close monitoring of the outcome leads to an increased rate of non-union. An important part is played by underestimation of the displacement of the fragments on the anteroposterior radiograph (Figure 1) (5– 11).
Figure1.
Technique for X-ray of the clavicle
anteroposterior projection with the patient supine (day of injury)
anteroposterior projection with the patient in sitting position and the arm hanging down (2 days after injury)
Unless there are complex injuries, such as vascular or neural trauma, a correctly conducted standard X-ray examination renders further diagnostic imaging—computed tomography, magnetic resonance imaging, or angiography—unnecessary.
Classification
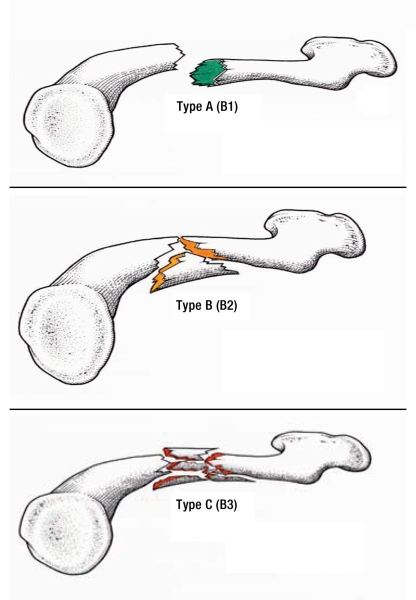
The OTA (Orthopaedic Trauma Association) classification of midclavicular fractures (figure 2) has been adopted internationally. It distinguishes:
Figure 2.
Classification of midclavicular fractures according to the Orthopaedic Trauma Association (OTA) 1996 (2007). Illustration: Josef Ribbers, Cologne
Treatment
Conservative and various surgical procedures are available. To advise the patient correctly and determine which form of treatment is indicated, it is first necessary to explain the individual techniques, complete with their advantages and disadvantages.
Conservative treatment
If conservative treatment is indicated, administration of analgesics is accompanied by immobilization of the injured side by means of a rucksack bandage or sling. Reduction of the fragments is not indicated, as no bandage has the potential to maintain the result of reduction long term (5, 14, e3).
The success of treatment can be monitored clinically by following the developments in the pain situation and in arm mobility. Many patients can raise the arm to a horizontal position after 3 weeks. Callus formation becomes radiologically detectable no less than 6 weeks after injury. By this time the patient should have regained almost the full range of motion and be practically free of pain. Sports in which unusual loads are placed on the shoulder can be resumed after 12 weeks. Physiotherapy is not obligatory. Manual lymph drainage is indicated in the initial phase, and sessions of assisted (3rd week) and active (6th week) exercise treatment are indicated in the case of massive swelling and extreme limitation of motion.
Complications—Different authors have found that up to 50% of patients treated with a rucksack bandage can show an increasing degree of displacement (5, e3). This occurs almost routinely because of the caudal tension exerted by the weight of the arm on the lateral fragment, while the medial fragment is held in cranial position by the sternocleidomastoid muscle.
Excessive tightening of the rucksack bandage often causes significant complications, ranging from cutaneous maceration in the axilla (33% in the study by Jubel et al. in 2005 [5]) through brachial paresthesia (“pins and needles”) (33%) and massive swelling (55%) to deep brachial vein thromboses (1, 5). Moreover, the rucksack bandage has practically no effect in the supine position, because the shoulders inevitably fall forward. For these reasons the rucksack bandage should essentially be viewed as a means of reducing pain; based on current knowledge, routine “retightening” is not recommended.
Painful instability or persistence of crepitations beyond 3 to 4 weeks points to defective bony healing. Failure to detect callus after 12 weeks is a sure sign of delayed healing, which in our experience culminates in non-union in over 50% of cases.
Surgical treatment
The following operative procedures are used:
Classic compression plate osteosynthesis
Minimally invasive plate osteosynthesis (MIPO) with angle-stable implants
Minimally invasive elastic stable intramedullary nailing (ESIN)
Classic compression plate osteosynthesis—In the classic technique a 10- to 14-cm-long incision is made to provide access to the clavicle. The fragments are anatomically reduced, and if indicated lag screws are inserted to hold them in place. A 6- to 10-hole small-fragment LCDC (limited contact dynamic compression) plate is then applied (e4, e5). Alternatively a reconstruction plate may be used (e6). Smaller plates, such as the one-third tubular plate, have proved too weak. Postoperatively the shoulder can be mobilized to the extent permitted by pain; immobilization for 4 to 5 days may be required.
Minimally invasive plate osteosynthesis (MIPO) with angle-stable implants—The MIPO procedure is distinguished from classic compression plate osteosynthesis by the choice of implants and the technique used. In contrast to the conventional plate, both the screw heads and the holes in the plate are threaded. Insertion of a screw results in an angle-stable connection between screw and plate, yielding much higher stability than with a classic plate. Furthermore, the construction no longer requires maximal friction between implant and bone. This is advantageous in the presence of poor bone structure (osteoporosis) and has a less adverse effect on the periosteal circulation.
The logical development of this tissue-sparing technique is minimally invasive application (15). The plate is inserted through a small incision and positioned percutaneously. The individual screws can than be inserted via accessory incisions that can be created as required. Exact anatomic reconstruction of the individual fragments is often impossible—but also unnecessary, provided the length, axis, and rotation of the clavicle are restored correctly (figure 3).
Figure 3.
Minimally invasive plate osteosynthesis
Before operation
After operation
Complications of plate osteosynthesis—Apart from incorrect choice of implant and inadequate reduction and screw anchoring, the essential complications of plate osteosynthesis are implant failure (loosening, breakage) and refracture after implant removal, which altogether occur in around 10% of cases (16, 17). These problems are more frequent in classic plate osteosynthesis, which tends to compromise the supply of blood to the bone because of the extensive bony exposure and the compression of plate to bone. If technical and biological problems coexist, then a greatly increased risk of non-union must be assumed. If revision becomes necessary, resection of the pseudarthrosis and cancellous bone grafting may have to be followed by insertion of a stronger plate in a different position.
Minimally invasive elastic stable intramedullary nailing (ESIN)—The ESIN method traces its roots back to the early work of Lambotte in 1907 (cited in [e7]). In 1998, with reference to publications by Prévot, Jubel and Rehm suggested the use of an elastic titanium nail (18, 19). From the biomechanical point of view intramedullary application is ideal, because the central position of the intramedullary nail avoids the problem of the ever-changing tension side.
The patient is positioned flat on the X-ray table; intraoperative imaging in two projections must be possible. The ventral cortex is opened via a small incision lateral to the sternoclavicular joint and the titanium nail is inserted. The nail is advanced to the fracture site and then, following (closed or open) reduction, driven into the lateral fragment. After sufficient engagement of the lateral fragment, the nail can be shortened so that its end lies under the skin (19, 20) (figure 4).
Figure 4.
Elastic stable intramedullary nailing
Before operation
After operation
Following
implant removal 8 months later
Postoperatively the patient may move the arm actively to the extent permitted by pain, but not going above horizontal. Depending on fracture type, the patient regains a complete range of motion after 3 to 6 weeks. The nail can be removed after 6 to 12 months.
Complications—While plate osteosynthesis can, in principal, be used in all types of midclavicular fractures, ESIN is restricted to fractures of types A and B. The reason is that the nail does not possess length stability in all circumstances: In type C fractures, where by definition there is no cortical support, “telescoping” of the fracture may occur over a period of time. This results in secondary shortening and thus to failure of the technique (21).
Fresh type A fractures (less than 10 days old) can frequently be reduced in closed technique and elegantly treated by ESIN. Older and type B fractures require open reduction in about 50% of cases. Additional fragments can be reduced with the help of strong suture material. Type B fractures without a sufficiently extensive area of contact between the principal fragments are unsuitable for ESIN and must be treated with plate osteosynthesis.
In addition to inaccurate determination of the indications, problems may be caused by imprecise choice of entry site; selection of the wrong (too thin) implant (rule of thumb: diameter 2.5 mm for women, 3 mm for men), resulting in secondary displacement; and insufficient shortening of the sternal end of the nail, leading to skin irritation. Lateral nail perforation may also occur if the surgeon drives the nail in too forcefully or fails to consult the image intensifier properly.
Recommendations
Surgical treatment is indisputably indicated in the following situations (e8, e9):
-
Damage to vessels and/or nerves (1% to 2%)
Open fractures or imminent perforation of the skin (1% to 2%)
Painful non-union (3% to 5%)
Further undisputed (albeit rare) indications are (e8, e9):
“Floating shoulder,” i.e., simultaneous injury of clavicle and scapula
Clavicular fracture in polytraumatized patients who also have injuries of the lower limbs (in order to permit mobilization)
Bilateral clavicular fracture
Clavicular fracture with ipsilateral fracture of multiple ribs
Multiple fractures of the upper extremity.
Equally, there is consensus that minimally displaced midclavicular fractures should be treated conservatively. Traditionally, conservative therapy was also the treatment of choice for fractures with a greater degree of displacement. This approach was based essentially on statistics from the 1960’s showing a low rate of non-union (<1%), a higher proportion of malunions after conventional plate osteosynthesis (Rowe et al.: 0.8% vs. 3.7%; Neer et al.: 0.1% vs. 4.6%), and high patient satisfaction (2, 22). It should be borne in mind, however, that these studies included children and adolescents.
Following the introduction of new techniques (ESIN, plate fixation), the past 10 years have seen a number of studies whose results have revived the debate whether midclavicular fractures should be treated by conservative or surgical means.
The study published by Robinson et al. was based on prospective observation of 868 consecutive patients with conservative treatment of a midclavicular fracture. Clinical and radiological follow-up examinations were conducted 6, 12, and 24 weeks after injury. The cumulative risk of non-union after 24 weeks was 4.5% (10). Brinker et al. used these data to calculate the likelihood of non-union in various subpopulations and found very high rates for displaced and/or multifragmentary fractures (table 1) (9).
Table 1. Probability of non-union of midclavicular fractures 24 weeks after injury in women and men: findings in 868 conservatively treated fractures (from Brinker [9]).
| Displaced (%) | Multifragmentary (%) | Displaced and multifragmentary (%) | Neither displaced nor multifragmentary (%) | |||||
| Age (years) | Women | Men | Women | Men | Women | Men | Women | Men |
| 25 | 19 | 8 | 7 | 3 | 33 | 20 | 3 | <1 |
| 35 | 20 | 11 | 8 | 4 | 35 | 21 | 4 | <1 |
| 45 | 25 | 14 | 10 | 5 | 37 | 25 | 5 | 1 |
| 55 | 28 | 18 | 12 | 6 | 42 | 29 | 6 | 2 |
| 65 | 33 | 20 | 18 | 7 | 47 | 33 | 7 | 3 |
In a meta-analysis published in 2005, Zlowodzi et al. determined a 5.9% rate of non-union in 1145 conservatively treated fractures. A subanalysis revealed a rate of 15.1% for displaced fractures. Significantly better results were achieved in such cases by plate osteosynthesis (2.2%) and ESIN (2%). One limitation reported by the authors of this meta-analysis was the excessively low EBM (evidence-based medicine) level: of the 22 studies evaluated, only five yielded level-1 or -2 evidence (8).
We carried out a prospective, comparative, non-randomized study in which it was shown that patients treated by ESIN had significantly better objective and subjective results than a comparable, conservatively treated group over a period of 12 months (5).
With regard to evidence-based recommendations, two prospective randomized studies with level-1 evidence have been published to date.
A Canadian multicenter study (2007) compared conservative treatment with conventional plate osteosynthesis in 132 patients with displaced fractures. The surgical option proved advantageous in terms of functional outcome, rate of malunion, and healing time (7).
In 2008, Smekal et al. published the results of a randomized controlled clinical study comparing ESIN and conservative treatment in 60 patients (30 in each group) with displaced midclavicular fractures. Displacement was defined as the absence of cortical contact between the principal fragments.
After 24 weeks, bony consolidation had not been attained in 30% of the conservatively treated and in 3.3% of the surgically treated patients. After 32 weeks, all surgically managed clavicles had healed, while three conservatively treated patients (10%) displayed symptomatic non-union. The functional outcome after 6 months and 2 years was significantly better in the surgically treated patients than in those who were managed conservatively (21).
Besides the problem of non-union, attention also needs to be paid to healing of the clavicle in the wrong position. We investigated the influence of shortening on the functional outcome, regardless of the method of treatment (23). In line with Smekal’s results, we found that the functional outcome depended on the extent of shortening. Patients with malposition resulting in shortening of more than 1.75 cm had scores similar to those of patients with painful non-union.
Two reviews were recently added to the Cochrane Library database, one comparing the operative methods for treatment of fracture or non-union, the other comparing different forms of conservative management (24, 25). Both of these reviews determined a very low level of evidence, because of the poor quality of the studies they embraced. The studies cited above were not included in these reviews because they compared surgical and conservative treatment.
Conclusion
The debate on treatment options for midclavicular fractures is currently centered on the question of whether displaced fractures should primarily be managed surgically, and if so which implant should be selected. The results of the studies published to date do not yield a conclusive answer to this question. Moreover, it remains to be precisely analyzed which patients benefit from operative treatment. However, the literature findings already clearly show that treatment should be tailored to the situation of each individual patient. The patient should be informed in detail of the options available and the potential benefits and risks of each approach (table 2). Both conservative and surgical treatment require painstaking diagnostic investigation, analysis of indications, treatment and aftercare in order to achieve the best possible results. In the light of current knowledge, midclavicular fracture can no longer be considered a trivial injury.
Table 2. Advantages and disadvantages of conservative and surgical treatment of midclavicular fractures.
| Treatment | Advantages | Disadvantages |
| Conservative |
|
|
| Surgical |
|
|
Key Messages.
Precise X-ray positioning of the clavicle in two projections is essential for correct analysis of the fracture type.
No adequate long-term reduction of a displaced midclavicular fracture can be achieved with a rucksack bandage or other such aid.
Patients with a displaced midclavicular fracture benefit from surgical treatment.
Simple midclavicular fractures can be managed very elegantly and with high stability by means of an intramedullary titanium nail.
Complex midclavicular fractures can be treated surgically by insertion of a bridging angle-stable plate.
Acknowledgments
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
Professor Andermahr has received honoraria from Synthes GmbH (Umkirch) for serving as a consultant.
The remaining authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Nordqvist A, Petersson CJ, Redlund-Johnell I. Mid-clavicle fractures in adults: end result study after conservative treatment. J Orthop Trauma. 1998;12:572–576. doi: 10.1097/00005131-199811000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res. 1968;58:29–42. [PubMed] [Google Scholar]
- 3.Stanley D, Trowbridge EA, Norris SH. The mechanism of clavicular fracture. A clinical and biomechanical analysis. J Bone Joint Surg Br. 1988;70:461–464. doi: 10.1302/0301-620X.70B3.3372571. [DOI] [PubMed] [Google Scholar]
- 4.Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1998;80:476–484. doi: 10.1302/0301-620x.80b3.8079. [DOI] [PubMed] [Google Scholar]
- 5.Jubel A, Andermahr J, Prokop A, Lee JI, Schiffer G, Rehm KE. Treatment of mid-clavicular fractures in adults. Early results after rucksack bandage or elastic stable intramedullary nailing. Unfallchirurg. 2005;108:707–714. doi: 10.1007/s00113-005-0970-8. [DOI] [PubMed] [Google Scholar]
- 6.Jubel A, Andermahr J, Schiffer G, Rehm KE. Technique of intramedullary osteosynthesis of the clavicle with elastic titanium nails. Unfallchirurg. 2002;105:511–516. doi: 10.1007/s00113-001-0386-z. [DOI] [PubMed] [Google Scholar]
- 7.Society COT. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89:1–10. doi: 10.2106/JBJS.F.00020. [DOI] [PubMed] [Google Scholar]
- 8.Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005;19:504–507. doi: 10.1097/01.bot.0000172287.44278.ef. [DOI] [PubMed] [Google Scholar]
- 9.Brinker MR, Edwards TB, O’Connor DP. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2005;87:676–677. doi: 10.2106/00004623-200503000-00034. [DOI] [PubMed] [Google Scholar]
- 10.Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2004;86-A:1359–1365. doi: 10.2106/00004623-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79:537–539. doi: 10.1302/0301-620x.79b4.7529. [DOI] [PubMed] [Google Scholar]
- 12.Classification OTACfCa. Fracture and dislocation compendium. J Orthop Trauma. 1996;10(Suppl 1 v-ix):1–154. [PubMed] [Google Scholar]
- 13.Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21:S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 14.Petracic B. Efficiency of a rucksack bandage in the treatment of clavicle fractures. Unfallchirurgie. 1983;9:41–43. [PubMed] [Google Scholar]
- 15.Andermahr J, Faymonville C, Rehm KE, Jubel A. Percutaneous plate osteosynthesis for clavicular fractures, Initial description. Unfallchirurg. 2008;111:43–45. doi: 10.1007/s00113-007-1304-9. [DOI] [PubMed] [Google Scholar]
- 16.Kuner EH, Schlickewei W, Mydla F. Surgical therapy of clavicular fractures, indications, technic, results. Hefte Unfallheilkd. 1982;160:76–83. [PubMed] [Google Scholar]
- 17.Poigenfurst J, Reiler T, Fischer W. Plating of fresh clavicular fractures. Experience with 60 operations. Unfallchirurgie. 1988;14:26–37. [PubMed] [Google Scholar]
- 18.Jubel A, Prokop A, Kress J, Rehm KE. Die elastische stabile Marknagelung der Klavikulafraktur im mittleren Drittel. Hefte zu „Der Unfallchirurg“. 1998:738–739. [Google Scholar]
- 19.Rehm KE, Andermahr J, Jubel A. Die intramedulläre Osteosynthese der Klavikula mit einem elastischen Titannagel. Oper Orthop Traumatol. 2004;16:365–379. [Google Scholar]
- 20.Jubel A, Andermahr J, Schiffer G, Tsironis K, Rehm KE. Elastic stable intramedullary nailing of midclavicular fractures with a titanium nail. Clin Orthop Relat Res. 2003:279–285. doi: 10.1097/00003086-200303000-00037. [DOI] [PubMed] [Google Scholar]
- 21.Smekal V, Irenberger A, Struve P, Wambacher M, Krappinger D, Kralinger FS. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures-a randomized, controlled, clinical trial. J Orthop Trauma. 2009;23:106–112. doi: 10.1097/BOT.0b013e318190cf88. [DOI] [PubMed] [Google Scholar]
- 22.Neer CS. Nonunion of the clavicle. JAMA. 1960;172:1006–1011. doi: 10.1001/jama.1960.03020100014003. [DOI] [PubMed] [Google Scholar]
- 23.Jubel A, Andermahr J, Faymonville C, Binnebosel M, Prokop A, Rehm KE. Reconstruction of shoulder-girdle symmetry after midclavicular fractures. Stable, elastic intramedullary pinning versus rucksack bandage. Chirurg. 2002;73:978–981. doi: 10.1007/s00104-002-0544-z. [DOI] [PubMed] [Google Scholar]
- 24.Lenza M, Belloti JC, Andriolo RB, Gomes Dos Santos JBF, aloppa F. Conservative interventions for treating middle third clavicle fractures in adolescents and adults. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD007121.pub2. CD007121. [DOI] [PubMed] [Google Scholar]
- 25.Lenza M, Belloti JC, Gomes Dos Santos JB, Matsumoto MH, Faloppa F. Surgical interventions for treating acute fractures or non-union of the middle third of the clavicle. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD007428.pub2. CD00742. [DOI] [PubMed] [Google Scholar]
- e1.Nordqvist A, Petersson CJ. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994;300:127–132. [PubMed] [Google Scholar]
- e2.Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002;11:452–456. doi: 10.1067/mse.2002.126613. [DOI] [PubMed] [Google Scholar]
- e3.Mullick S. Treatment of mid-clavicular fractures. Lancet. 1967 [Google Scholar]
- e4.Ali Khan MA, Lucas HK. Plating of fractures of the middle third of the clavicle. Injury. 1978;9:263–267. doi: 10.1016/s0020-1383(77)80041-7. [DOI] [PubMed] [Google Scholar]
- e5.Allgower M, Perren S, Matter P. A new plate for internal fixation—the dynamic compression plate (DCP) Injury. 1970;2:40–47. doi: 10.1016/s0020-1383(70)80111-5. [DOI] [PubMed] [Google Scholar]
- e6.Kremer K, Lierse W, Platzer W, Schreiber HW, Weller S. Plattenosteosynthese der Klavikula. In: Kremer K, Lierse W, Platzer W, Schreiber HW, Weller S, editors. Chirurgische Operationslehre. Stuttgart, New York: Georg Thieme Verlag; 1994. pp. 25–27. [Google Scholar]
- e7.Diez HG, Schmittenbecher PP, Illing P. München, Wien, Baltimore: Urban & Schwarzenberg; 1997. Historische Betrachtung der intramedullären Osteosynthese. [Google Scholar]
- e8.Geel CW. Scapula and clavicle: AO principles of fracture management. In: Colton CL, Fernandez Dell´Oca A, Holz U, Kellam JF, Ochsner PE, editors. Stuttgart, New York: Thieme; 2000. pp. 261–262. [Google Scholar]
- e9.Weise K. Schultergürtel und Schultergelenk: Frakturen. Chirurgie. In: Hirner A, Weise K, editors. Schnitt für Schnitt. Stuttgart, New York: Thieme-Verlag; 2004. 277 pp. [Google Scholar]