Summary
Aim
To describe our experience using extracorporeal cardiopulmonary resuscitation (ECPR) in resuscitating children with refractory cardiac arrest in the intensive care unit (ICU) and to describe hospital survival and neurologic outcomes after ECPR.
Methods
A retrospective chart review of a consecutive case series of patients requiring ECPR from 2001–2006 at Arkansas Children’s Hospital. Data from medical records was abstracted and reviewed. Primary study outcomes were survival to hospital discharge and neurological outcome at hospital discharge.
Results
During the 6-year study period, ECPR was deployed 34 times in 32 patients. 24 deployments (73%) resulted in survival to hospital discharge. Twenty eight deployments (82%) were for underlying cardiac disease, 3 for neonatal non cardiac (NICU) patients and 3 for pediatric non-cardiac (PICU) patients. On multivariate logistic regression analysis, only serum ALT (p value = 0.043; OR-1.6; 95% confidence interval-1.014–2.527) was significantly associated with risk of death prior to hospital discharge. Blood Lactate at 24 hours post ECPR showed a trend towards significance (p value-0.059; OR-1.27; 95% confidence interval-0.991–1.627). The Hosmer-Lemeshow tests (p value = 0.178) suggested a good fit for the model. Neurological evaluation of the survivors revealed that there was no change in PCPC scores from a baseline of 1–2 in 18/24 (75%) survivors.
Conclusions
ECPR can be used successfully to resuscitate children following refractory cardiac arrest in the ICU, and grossly intact neurologic outcomes can be achieved in a majority of cases.
Keywords: cardiopulmonary resuscitation, ECMO, pediatric, outcomes
Introduction
Since closed-chest cardiac massage was introduced, cardiopulmonary resuscitation (CPR) has been widely instituted for cardiac arrest (1, 2). Several reports have demonstrated only a higher rate (63% to 70%) of return of spontaneous circulation (ROSC) after CPR (3–5), with much lower survival-to-discharge rates (10% to 27%) for cardiac arrests in children (1, 3–5). More recently, a four-year review of the National Registry of Cardiopulmonary Resuscitation revealed a rate of survival-to-discharge of 27% for pediatric in-hospital cardiac arrest, with 65% of survivors having a good neurologic outcome (5). For those patients requiring prolonged resuscitation the outcomes are even more dismal (1,6–8).
Due to the low survival rates after prolonged CPR, more aggressive methods have been suggested to improve its success (9, 10). Recently, institution of extracorporeal life support (ECLS) has been proposed for selected cases of cardiac arrest when conventional CPR fails. Case series from many institutions have reported reasonable success with extracorporeal CPR (ECPR) in terms of both short-term survival and neurologic outcome (7,11–33). This study represents our institutional experience with ECPR instituted during active chest compressions following in-hospital pediatric cardiac arrest. We hypothesized that ECPR is effective in resuscitating children with refractory cardiac arrests in the ICU and is often associated with good neurologic outcomes.
Material and methods
A retrospective chart review, approved by the Institutional Review Board of University of Arkansas for Medical Sciences was performed. The study population included all patients (0 to 20 years of age) admitted to Arkansas Children’s Hospital who were resuscitated from cardiac arrest during active chest compressions by means of veno-arterial ECLS between January 2001 and March 2006. Patients were identified through a review of the institutional ECLS database and the institutional CPR database. This time period was chosen as it represents the time period between the full implementation of the American Heart Association 2000 CPR guidelines (9) to the full implementation of the American Heart Association 2005 CPR guidelines (10) at our institution.
For this study, “cardiac arrest” was defined as any patient requiring external chest compressions or internal cardiac massage for ≥ 60 seconds because of a profound low cardiac output state, which is consistent with the operational definition of cardiac arrest from the American Heart Association National Registry of CPR (10). We included in the analysis only children who underwent active chest compressions or internal cardiac massage at the time of ECLS cannulation. Patients who were placed on ECLS after ROSC were excluded.
ECPR is initiated at our institution when the ECPR team is activated via STAT notification process to initiate call for ECLS to aid CPR. The team consists of a cardiothoracic surgeon, ECLS specialist/ perfusionist, intensive care specialist and nursing staff familiar with initiation and management of a patient on ECLS. Conventional CPR was managed by fellow or faculty neonatologists, intensivists, or cardiologists, depending on the location of the patient. During the study period, an ECLS coordinator was in-house 24/7 if other patients were being supported with ECLS at the time. Otherwise, an ECLS coordinator was on-call 24/7 and immediately available to return to the hospital. A pre-assembled and/or primed backup circuit was available at all times. The surgical team was responsible for cannulation, while the nursing and medical physician team were focused on conducting CPR and monitoring the patient during the cannulation process. Cannulation sites utilized included thoracic (for cardiac patients with recent sternotomy) or cervical/ groin cannulation. In patients with left ventricular dysfunction, consideration was given after ECLS cannulation to early decompression of the left atrium and ventricle which, if necessary, was accomplished by atrial septostomy or a transthoracic left atrial cannula placement (15).
The management approach of these study patients once placed successfully on ECMO remained uniform during the study period. It consisted of initiation of moderate hypothermia (~34°C) for at least 24 hours. We maintain normal blood pressure for age by adjusting flow on pump and minimizing inotrope/ vasopressor doses. Normal blood gas parameters are maintained by adjusting sweep flow and FiO2 delivery via the oxygenator membrane. All patients were placed on “rest” ventilatory support with a low rate (<10 breath/minute), high PEEP (8–15 cmH2O) and low inspired oxygen concentration (< 0.4). Blood gas parameters were normalized by adjusting sweep flow and FiO2 delivery via the ECMO membrane. Serum glucose is maintained between 100–150 mg/dl by using insulin infusions judiciously. Anticoagulation with unfractionated heparin is while on ECMO is titrated to maintain activated clotting times between 160 to 220 seconds. Patients are adequately sedated once neurological activity is detected using benzodiazepines and opioids. Steroids are not given routinely before or after initiation of ECMO.
The medical record of each subject was reviewed for demographic information, medical history, primary diagnosis, duration of mechanical ventilation prior to ECLS cannulation, inotropes/ vasopressor prior to ECPR, duration of conventional CPR before ECLS, rhythm prior to ECPR, need for defibrillation, duration of ECLS support, and survival to hospital discharge. Additional clinical variables collected were highest serum lactate, serum lactate level at 24 hours after initiation of ECLS, lowest arterial pH, renal function parameters (blood urea nitrogen, creatinine, need for renal replacement therapy), evidence of hepatic injury (aspartate aminotransferase (AST) and alanine aminotransferase (ALT), and hematological parameters (WBC count) We treated each resuscitation event separately and included all ECPR events in our analysis, except where otherwise noted.
We also reviewed medical records to ascertain whether the child had a meaningful neurologic impairment at the time of hospital discharge and on subsequent follow-up. Admission and discharge Pediatric Cerebral Performance Category and Pediatric Overall Performance Category (16) were assigned in surviving children through retrospective chart review. Not every patient had a formal pediatric neurology consultation during hospitalization.
The primary outcome measure, survival to hospital discharge, is reported as recommended by the Utstein reporting template (10). One patient had two separate ECPR deployments in two separate hospitalizations. For the purposes of the study these were counted as two separate survivals to hospital discharge events thus giving us a denominator of 33 patients. Univariate and multivariate logistic regression analysis was carried out to identify risk factors for death prior to discharge.
Statistics
Continuous variables are presented as median (range) whereas categorical variables are presented as percentages. Statistical analysis was performed in three steps: univariate analysis was first used to examine the relationship between the categorical and continuous variables and the primary outcome variable using the Wald test. From the univariate analysis, all variables at a p value ≤ 0.20 in the univariate analysis were entered for multivariate analysis. Stepwise logistic regression with forward selection was used to build parsimonious models for each outcome. Those variables that did not retain statistical significance on multivariate analysis were removed from the model. When the final model was identified, several additional analyses where performed wherein the factors that had not been retained in the model were reevaluated for inclusion. Results are presented as odds ratios (OR) with 95% confidence interval (CI). Due to collinearity between age and weight only one of the variables (age) was included in the multivariate analysis. The values for serum AST were log transformed to stabilize variance and normalize the distribution. The model’s goodness-of-fit was evaluated using the Hosmer-Lemeshow chi square test and the discrimination of the model was assessed using the area under the receiver operating curve. A p value of ≤ 0.05 was considered to be statistically significant. All analyses were performed using Stata statistical software, version 10, (StataCorp LP, College Station, Texas).
Results
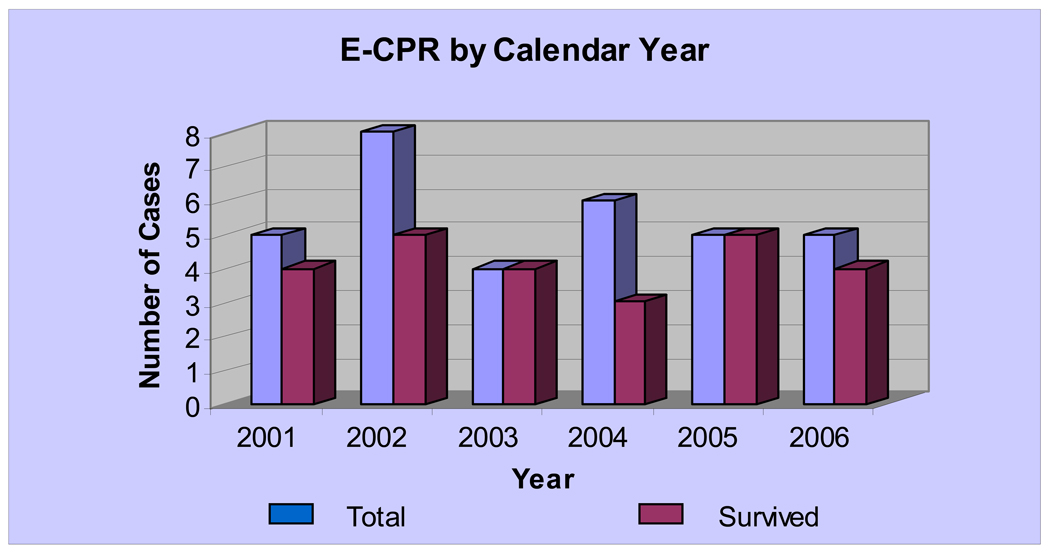
During the 6-year study interval, 329 in-hospital cardiac arrests occurred at our institution. Figure 1 shows the yearly distribution of ECPR events and survival to discharge over the study period. Four additional patients required ECLS after an episode of CPR, with cannulation for ECLS occurring after ROSC. These four patients were excluded from the study. None of these four patients survived to hospital discharge.
Figure 1.
Distribution of ECPR cases and survival by calendar year
During the study period 32 patients underwent 34 ECLS deployments. Surgical cannulation occurred in these patients during active external chest compressions or internal cardiac massage. One patient underwent two ECLS deployments for ECPR during the same hospitalization but did not survive to hospital discharge. Another patient required ECPR twice during two separate hospitalizations. This patient survived to hospital discharge from both events. For analyzing the primary outcome data this patient was counted twice.
Twenty eight deployments (82%) were for underlying cardiac disease, 3 for neonatal non-cardiac (Neonatal ICU) patients and 3 for pediatric non-cardiac (Pediatric ICU) patients (Table 1). Overall, 24 patients requiring 33 ECLS deployments (73%) survived to hospital discharge.
Table 1.
Differences between survivors and non-survivors and univariate analysis of variables associated with death prior to hospital discharge in patients requiring ECPR
| Variables (All) | Non-survivor | Survivor | Odds ratio | P value | 95% CI | |
|---|---|---|---|---|---|---|
| Age (months)¶ | 6 (0.66–150) | 1.55 (0–168) | 1.01 | 0.205 | 0.995 – 1.025 | |
| Male Gender | 5 | 16 | 0.63 | 0.556 | 0.131 – 2.989 | |
| Weight (kilograms)¶ | 8 (3–65) | 3.9 (2.14–66.7) | 1.03 | 0.205 | 0.984 – 1.075 | |
| Type of patient: | 2.11* | 0.526* | 0.211 – 21.01* | |||
| CVICU | 8 | 20 | ||||
| NICU | 0 | 3 | ||||
| PICU | 1 | 2 | ||||
| Post-cardiac surgery | 4 | 13 | 0.42 | 0.293 | 0.085 – 2.099 | |
| Pre-ECPR lactate (mmol/L)¶ | 2 (0.7–13.7) | 2 (1.1–28.7) | 1.02 | 0.80 | 0.866 – 1.169 | |
| Prior CPR events before episode requiring ECPR | 3 | 7 | 1.21 | 0.23 | 0.235 – 6.271 | |
| CPR Variables | ||||||
| Timing of ECPRa | 4 | 11 | 1.12 | 0.50 | 0.856 –3.573 | |
| Duration of pre-ECLS CPR (minutes)¶ | 60 (20–76) | 43 (15–142) | 1.01 | 0.70 | 0.979 – 1.044 | |
| Closed vs. open chest ECLS Cannulation | 9 | 15 | 0.21 | 0.17 | 0.022 – 1.951 | |
| Initial rhythm at CPR (VF/VT vs. Others)b | 3 | 19/4 | 1.90 | 0.459 | 0.347 – 10.40 | |
| Defibrillation/ cardioversion performed | 3 | 7 | 0.81 | 0.821 | 0.130 – 5.028 | |
| Prolonged CPR (> 60 minutes) | 5 | 5 | 4.75 | 0.063 | 0.919 – 24.55 | |
| Post ECPR Variables | ||||||
| Serum bilurubin (direct), highest¶ | 1.3 (0.1–6.9) | 0.7 (0.1–11.5) | 1.05 | 0.690 | 0.813 – 1.365 | |
| Serum alanine aminotransferase, highest¶ | 200 | 69 (21–927) | 1.53 | 0.032 | 1.037 – 2.260 | |
| Blood urea nitrogen, highest¶ | 37 (9–77) | 27 (13–65) | 1.02 | 0.334 | 0.977 – 1.070 | |
| Serum creatinine, highest¶ | 0.7 (0.5–2.7) | 0.7 (0.5–2.9) | 1.40 | 0.532 | 0.489 – 3.993 | |
| WBC count, highest | 9.73 (6.1–18.8) | 7.13 (2.7–17.4) | 1.08 | 0.338 | 0.924 – 1.260 | |
| pH ≤ 7.2 | 8 | 14 | 5.71 | 0.126 | 0.613 – 53.23 | |
| Duration of ECMO (hours)¶ | 59 (7–905) | 122 (41–816) | 1.00 | 0.65 | 0.997 – 1.004 | |
| Blood Lactate at 24 hours post ECPR¶ | 3.2 (1.2–24) | 2.55 (0.6–7.7) | 1.27 | 0.108 | 0.948 – 1.712 | |
| Renal Replacement Rx on ECMO | 3 | 4 | 3.50 | 0.182 | 0.556 – 22.03 | |
daytime (7 am –7 pm) shift vs. other shift
VF= ventricular fibrillation, VT=ventricular tachycardia
median (range)
cardiac diagnosis vs. others
Log transformed for calculating odds ratio
Among those with cardiac disease, 20 (71%) patients with cardiac disease survived to hospital discharge (Table 1). Two of these cardiac patients required ECPR for intractable arrhythmia, 12 patients had cyanotic congenital heart disease and the rest had acyanotic heart disease.
A minority of the study patients had non-cardiac primary diagnoses. All 3 neonatal ICU patients and 2/3 (67%) pediatric ICU patients requiring ECPR survived to hospital discharge. The primary diagnoses of the three PICU patients were succinylcholine-related malignant hyperthermia (survived), toxic shock syndrome (survived), and septic shock with underlying developmental delay (died). Two of the 3 neonatal ICU survivors suffered cardiac arrest related to septic shock, and 1 had meconium aspiration syndrome with persistent pulmonary hypertension leading to cardiac arrest. Five out of 10 patients (50%) who received prolonged chest compressions (> 60 minutes duration) prior to ECMO deployment survived to hospital discharge.
Table 1 also shows the comparison between survivors (to hospital discharge) and non-survivors of ECPR for other variables. Table 2 depicts the univariate analyses of variables impacting death prior to hospital discharge for patients undergoing ECPR. All variables at a p value of < 0.2 on the univariate analysis (age in months, blood Lactate at 24 hours post ECPR, a pH of ≤7.2, need for renal replacement therapy, duration of CPR for > 60 minutes, serum ALT) were included in the stepwise multivariate logistic regression model.
Table 2.
Multivariate analysis of variables associated with death prior to hospital discharge in patients requiring ECPR
| Variables | Odds Ratio | p value | 95% Confidence Interval |
|---|---|---|---|
| Serum AST | 1.60 | 0.043 | 1.015 2.527 |
| Blood Lactate at 24 hours post-ECPR | 1.27 | 0.059 | 0.991 1.627 |
On multivariate logistic regression analysis, only serum ALT (p value = 0.043; OR- 1.6; 95% confidence interval-1.014–2.527) was significantly associated with risk of death prior to hospital discharge. Blood Lactate at 24 hours post ECPR showed a trend towards significance (p value-0.059; OR-1.27; 95% confidence interval-0.991–1.627). A Hosmer-Lemeshow χ2 p-value of 0.178 suggested a good fit for the model.
The multivariate model showed a sensitivity of 66.7%, specificity of 100%, a positive predictive value of 100% and a negative predictive value of 88.89%. The receiver-operating curve a measure of discrimination of the model yielded an area under the curve of 0.81.
The Pediatric Cerebral Performance Score (PCPC) and the Pediatric Overall Performance Score (POPC) were used to evaluate gross neurological outcomes in the survivors. 75% (18/24) survivors had no change in PCPC and POPC scores from a baseline (1–2) at discharge. Of the 24 survivors, subsequent post-discharge follow-up was available for 19 patients (79%). Mean duration of follow-up was 31.5 months (range 1–72 months). The PCPC and POPC scores were unchanged from those at the time of discharge for the cohort where follow-up after discharge was available.
Of the 32 patients in the study, 31 had imaging of the head (ultrasound in 25 patients, CT scan in 10 patients, and MRI in 18 patients) performed during the hospitalization. Among the 9 patients who did not have either a head CT scan or MRI, 8 had a normal head ultrasound. Among the 4 patients who had a head CT scan but no head MRI performed, 3 head CT scans were normal and 1 showed evidence of brain uncal herniation. Among those who died, 1 had no head imaging performed, 1 had diffuse cerebral edema, and 1 had brain uncal herniation on head CT scan, and 6 had normal head imaging. Among the survivors, 7 had normal head ultrasound and no other imaging studies, 5 had severe brain injury noted, and another 4 had milder lesions (very small areas of infarction in the left frontal lobe in 2 patients, subdural fluid collection, a 2-mm lacunar defect in the left globus pallidus) on head MRI’s.
Table 3 provides details of the patients who were found to have more than 2 points change in POPC/ PCPC scores. Of the 5 children who received >60 minutes of chest compressions before ECPR, 2 (40%) survived without gross neurologic injury.
Table 3.
Diagnostic details of patients requiring ECPR with worse neurological outcomes
| No. | Diagnosis | CPR/ lowest pH |
PCPC Pre arrest |
POPC Pre arrest |
PCPC Post arrest |
POPC Post arrest |
|---|---|---|---|---|---|---|
| 1 | Malignant hyperthermia ventricular fibrillation |
142 min; pH 6.7 |
2 | 2 | 5 | 5 |
| 2 | Hetrotaxy, AVC, TAPVR, PS, PHTN | 56 min. pH6.5 |
1 | 1 | 4 | 4 |
| 3 | Hetrotaxy, transitional AVC, Low cardiac output |
60 min. pH 7.17 |
1 | 1 | 4 | 4 |
| 4 | Neonatal COA with cardiogenic shock | 40 min pH 6.8 |
1 | 1 | 4 | 4 |
| 5 | TA; BTS; lung lobe resection, poor LV function, heart transplant PHTN |
40 min; pH 7.18 |
1 | 1 | 2 | 3 (hemiparesis) |
| 6 | Repaired Tetrology pulmonary atresia; arrest in out of state community hospital; mobile ECLS |
>75 min; pH 6.7 |
1 | 1 | 4 | 4 |
PCPC=Pediatric cerebral performance score; POPC= Pediatric overall performance score; AVC=atrioventricular canal; TAPVR= total anomalous pulmonary venous return; PS= pulmonary stenosis; PHTN= pulmonary hypertension; COA= coarctation of aorta; TA= tricusid atresia; BTS=Blalock-Taussig shunt
Discussion
This series of patients resuscitated with ECPR both supports and complements prior single-institution reports (7,11–13). Table 4 shows other published pediatric series of ECPR patients (17) and their reported outcomes. As in previous studies, patients with cardiac disease were more likely to survive to hospital discharge after ECPR deployment than patients with other disease processes. Also similar to previous studies (7,13), survival to hospital discharge was not significantly associated with duration of CPR prior to institution of ECMO support. The primary difference between this case series and previous series lies in its higher-than-expected survival rate. While some very small series of cardiac patients supported with ECPR have demonstrated 80–100% survival 5,18), the larger and likely more representative series that have been published have reported hospital survival outcomes in the range of 30 – 50%.
Table 4.
Summary of previous studies on ECPR
| Author, year | Patient population | Successful cannulation (n) |
Survival to discharge; n (%) |
Duration of CPR in minutes median (range) or mean +/− SD |
|---|---|---|---|---|
| Huang 200829 | Mixed¶ | 27 | 11 (41) | Survivors 45 (25–50); Non-survivors 60 (37– 81) |
| Chan 200831 | Cardiac: ELSO Registry* | 492 | 208 (42) | Not reported |
| Thiagarajan 200712 | ELSO Registry* | 695 | 261(38) | Not reported |
| Ghez 200730 | Cardiac | 14 | 8 (57) | 44+/− 27 minutes (10–110 minutes) |
| Alsoufi 200713 | Mixed¶ | 80 | 27 (34) | Outcome: Favorable-46 (14–95);Unfavorable-41 (19–110) |
| MacLaren 200725 | Septic shock | 18 | 10 (55) | Not reported |
| Thourani 200628 | Cardiac | 15 | 11(73%) | 54 (4–127) |
| Allan 200632 | Cardiac | 19 | 15 (79) | 29 (20– 57) |
| De Mos 200622 | Mixed¶ | 5 | 2 (40) | All: 31–77; Survivors: 35–48 |
| Cengiz 200520 | ELSO Registry* | 161 | 64 (40) | Not reported |
| Shah 200527 | Cardiac | 27 | 9 (33) | Not reported |
| Morris 200426 | Mixed¶ | 64 | 21 (33) | Survivors: 50 (5–105); Non-survivors: 46 (15–90) |
| Hamrick 200323 | Cardiac# | 12 | 1 (8) | Not reported |
| Aharon 200118 | Cardiac# | 10 | 8 (80) | 42 (5–110) |
| Parra 20005 | Cardiac | 4 | 4 (100) | 16 (12–20) |
| Posner 200024 | ER | 2 | 1 (50) | 50, 90 |
| Duncan 199814 | Cardiac | 11 | 7 (64) | 55 (20–103) |
| del Nido 199621 | Cardiac# | 11 | 6 (55) | 65 +/− 9 |
| Dalton 199319 | Cardiac | 11 | 6 (55) | 42 (42–110) |
post-cardiotomy only
ELSO Registry
includes cardiac and non-cardiac patients
A recently published meta-analysis of extracorporeal membrane oxygenation use in children after cardiac arrest examined 288 children supported with ECPR (included 98 previously unpublished cases) (33). Overall survival to hospital discharge was 114/288 (39.6%). Interestingly, this meta-analysis included some patients for whom ECLS was initiated after ROSC and reported only 176/251 (70%) patients in whom ECLS was instituted concurrently with CPR, as was the case for all of the patients in our current series. Outcome data for patients cannulated for ECPR during active chest compressions is not separately reported in this meta-analysis, and presumably the overall survival rate includes some patients who received ECLS after ROSC. Regardless, the rate of survival to hospital discharge in our series (73%) compares favorably with the published literature.
Unfortunately, the factors behind such an encouraging survival rate are not clear from the current data and remain somewhat speculative. In our report serum ALT was identified as the only significant risk factor for death prior to hospital discharge. This likely simply represents a greater degree of end-organ injury in the non-survivors. It stands to reason that more rapid deployment of extracorporeal support during a cardiac arrest may be associated with improved perfusion and better neurologic and survival outcomes. However, as previously noted, neither this series nor others noted statistically different duration of CPR between survivors and non-survivors. Additionally, the range of pre-ECLS CPR duration for patients in this series does not differ appreciably from times reported in other series from other institutions.
All of the patients reported in this series suffered cardiac arrest in either the cardiovascular ICU, pediatric ICU or the neonatal ICU of a major children’s hospital. The cardiac arrest was managed by either a cardiac intensivist or a fellow or attending pediatric intensivist or neonatologist who was immediately available. Pediatric cardiovascular surgeons were available for cannulation for ECPR either immediately or within a very short time (< 30 minutes in almost all cases). ECLS staff also was available to the patient in-house in almost all cases reported. In 2007, after the current analysis, our institution adopted a standard of ECLS coordinators being available in-house on a continuous basis. It is possible that all of these factors contributed both to rapid provision of expert CPR and rapid provision of extracorporeal support, both of which may have enhanced outcomes. However, it should be noted that these circumstances do not differ appreciably from those reported by Alsoufi and colleagues from Toronto (13), yet overall survival in his large series of predominantly cardiac patients was 34%.
As in other reported series (29), neurologic outcome in our series was quite encouraging, particularly considering that the alternative neurologic outcome, were ECPR not provided, is death. 18/24 (75%) of survivors had no change from baseline in PCPC or POPC scores.
Study Limitations
As a retrospective non-randomized study this analysis has limitations. Due to small sample size the study is subject to selection or ascertainment bias despite having included consecutive patients during the study period in the study with a definitive primary outcome. Despite our multivariate analysis results, the factors behind such an encouraging survival rate in our study cohort are not clear from the current data and remain speculative. Even though we have neurological outcome data at the time of hospital discharge, unfortunately, detailed neurologic examination, neurodevelopmental evaluation, and detailed neuro-imaging studies were not uniformly available for reporting in our current series as has been the case in other series. Despite the availability of ECPR in all areas within our institution, all ECPR events in this occurred in the ICU’s - a controlled and monitored set-up, and predominantly included patients with cardiac pathology. This study is limited to answer if these superior outcomes can be replicated in other in-patient areas of the hospital and in cohorts where patients without primary cardiac disease make up the majority of the cohort. Such detailed evaluation is a goal of our program and should be a focus on any multi-center evaluation of ECPR.
Conclusions
In conclusion, ECLS instituted for selected refractory pediatric in-hospital cardiac arrest patients is feasible and effective. Based on our experience, we suggest that ECPR be more widely considered as an emergency resuscitative tool. Many questions regarding this use of ECLS technology remain to be answered, including the patient populations most likely to benefit, technical and system factors associated with best outcomes, and detailed neurodevelopmental follow-up. The recent meta-analysis published by Tajik suggests that ECPR may have a “value added” for hospital survival of 12–23% (33). However, given that ECPR is currently utilized for refractory cardiac arrest, it is not unreasonable to view each survivor as a 100% improvement in outcome. It is our hope that experienced ECMO centers will more readily consider use of this technology and that multi-institutional studies will address the questions noted above.
Acknowledgments
Financial Disclosure:
Supported in part by NIHCHD grant support -5 U10 HD050009
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
None of the authors have any conflict of interest that could inappropriately influence (bias) this work.
References
- 1.Schindler MB, Bohn D, Cox PN, et al. Outcome of out-of-hospital cardiac or respiratory arrest in children. N Engl J Med. 1996;335:1473–1479. doi: 10.1056/NEJM199611143352001. [DOI] [PubMed] [Google Scholar]
- 2.Slonim AD, Patel KM, Ruttimann UE, Pollack MM. Cardiopulmonary resuscitation in pediatric intensive care units. Crit Care Med. 1997;25:1951–1955. doi: 10.1097/00003246-199712000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Reis AG, Nadkarni V, Perondi MB, et al. A prospective investigation into the epidemiology of in-hospital pediatric cardiopulmonary resuscitation using the international Utstein reporting style. Pediatrics. 2002;109:200–209. doi: 10.1542/peds.109.2.200. [DOI] [PubMed] [Google Scholar]
- 4.Suominen P, Olkkola KT, Voipio V, et al. Utstein style reporting of in-hospital pediatric cardiopulmonary resuscitation. Resuscitation. 2000;45:17–25. doi: 10.1016/s0300-9572(00)00167-2. [DOI] [PubMed] [Google Scholar]
- 5.Nadkarni VM, Larkin GL, Peberdy MA, et al. National Registry of Cardiopulmonary Resuscitation Investigators. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;4(295):50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 6.Zaritsky A, Nadkarni VM, Getson P, et al. CPR in children. Ann Emerg Med. 1987;16:1107–1111. doi: 10.1016/s0196-0644(87)80465-1. [DOI] [PubMed] [Google Scholar]
- 7.Morris MC, Wernovsky G, Nadkarni VM. Survival outcomes after extracorporeal cardiopulmonary resuscitation instituted during active chest compressions following refractory in-hospital pediatric cardiac arrest. Pediatr Crit Care Med. 2004;5:440–446. doi: 10.1097/01.pcc.0000137356.58150.2e. [DOI] [PubMed] [Google Scholar]
- 8.Nichols DG, Kettrick RG, Swedlow DB, et al. Factors influencing outcome of cardiopulmonary resuscitation in children. Pediatr Emerg Care. 1986;2:1–5. doi: 10.1097/00006565-198603000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Pediatric Advanced Life Support Circulation. 2000;102:I-291–I-342. [Google Scholar]
- 10.2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112:IV-1–IV-203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 11.Chen YS, Lin JW, Yu HY, et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet. 2008;16(372):554–561. doi: 10.1016/S0140-6736(08)60958-7. [DOI] [PubMed] [Google Scholar]
- 12.Thiagarajan RR, Laussen PC, Rycus PT, et al. Extracorporeal membrane oxygenation to aid cardiopulmonary resuscitation in infants and children. Circulation. 2007;116:1693–1700. doi: 10.1161/CIRCULATIONAHA.106.680678. [DOI] [PubMed] [Google Scholar]
- 13.Alsoufi B, Al-Radi OO, Nazer RI, et al. Survival outcomes after rescue extracorporeal cardiopulmonary resuscitation in pediatric patients with refractory cardiac arrest. J Thorac Cardiovasc Surg. 2007;134:952–959. doi: 10.1016/j.jtcvs.2007.05.054. [DOI] [PubMed] [Google Scholar]
- 14.Duncan BW, Ibrahim AE, Hraska V, et al. Use of rapid-deployment extracorporeal membrane oxygenation for the resuscitation of pediatric patients with heart disease after cardiac arrest. J Thorac Cardiovasc Surg. 1998;116:305–311. doi: 10.1016/s0022-5223(98)70131-x. [DOI] [PubMed] [Google Scholar]
- 15.Seib PM, Faulkner SC, Erickson CC, et al. Blade and balloon atrial septostomy for left heart decompression in patients with severe ventricular dysfunction on extracorporeal membrane oxygenation. Cathet Cardiovasc Intervent. 1999;46:179–186. doi: 10.1002/(SICI)1522-726X(199902)46:2<179::AID-CCD13>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 16.Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr. 1992;121:68–74. doi: 10.1016/s0022-3476(05)82544-2. [DOI] [PubMed] [Google Scholar]
- 17.Fiser RT, Morris MC. Extracorporeal cardiopulmonary resuscitation in refractory pediatric cardiac arrest. Pediatr Clin North Am. 2008;55:929–941. doi: 10.1016/j.pcl.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 18.Aharon AS, Drinkwater DC, Jr, Churchwell KB, et al. Extracorporeal membrane oxygenation in children after repair of congenital cardiac lesions. Ann Thorac Surg. 2001;72:2095–2101. doi: 10.1016/s0003-4975(01)03209-x. [DOI] [PubMed] [Google Scholar]
- 19.Dalton HJ, Siewers RD, Fuhrman BP, et al. Extracorporeal membrane oxygenation for cardiac rescue in children with severe myocardial dysfunction. Crit Care Med. 1993;21:1020–1028. doi: 10.1097/00003246-199307000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Cengiz P, Seidel K, Rycus PT, et al. Central nervous system complications during pediatric extracorporeal life support: incidence and risk factors. Crit Care Med. 2005;33:2817–2824. doi: 10.1097/01.ccm.0000189940.70617.c3. [DOI] [PubMed] [Google Scholar]
- 21.del Nido PJ, Dalton HJ, Thompson AE, Siewers RD. Extracorporeal membrane oxygenator rescue in children during cardiac arrest after cardiac surgery. Circulation. 1992;86:II300–II304. [PubMed] [Google Scholar]
- 22.de Mos N, van Litsenburg RR, McCrindle B, et al. Pediatric in-intensive-care-unit cardiac arrest: incidence, survival, and predictive factors. Crit Care Med. 2006;34:1209–1215. doi: 10.1097/01.CCM.0000208440.66756.C2. [DOI] [PubMed] [Google Scholar]
- 23.Hamrick SEG, Gremmels DB, Keet CA, et al. Neurodevelopmental outcome of infants supported with extracorporeal membrane oxygenation after cardiac surgery. Pediatrics. 2003;111:e671–e675. doi: 10.1542/peds.111.6.e671. [DOI] [PubMed] [Google Scholar]
- 24.Posner JC, Osterhoudt KC, Mollen CJ, et al. Extracorporeal membrane oxygenation as a resuscitative measure in the pediatric emergency department. Pediatr Emerg Care. 2000;16:413–415. doi: 10.1097/00006565-200012000-00008. [DOI] [PubMed] [Google Scholar]
- 25.MacLaren G, Warwick B, Best D, et al. Extracorporeal membrane oxygenation for refractory septic shock in children: one institution’s experience. Pediatr Crit Care Med. 2007;8:447–451. doi: 10.1097/01.PCC.0000282155.25974.8F. [DOI] [PubMed] [Google Scholar]
- 26.Morris M, Wernovsky G, Helfaer M, et al. Survival outcomes following extracorporeal cardiopulmonary resuscitation from in-hospital pediatric cardiac arrest. Pediatr Crit Care Med. 2004;5:440–446. doi: 10.1097/01.pcc.0000137356.58150.2e. [DOI] [PubMed] [Google Scholar]
- 27.Shah SA, Shankar V, Churchwell KB, et al. Clinical outcomes of 84 children with congenitalheart disease managed with extracorporeal membrane oxygenation after cardiac surgery. ASAIO J. 2005;51:504–507. doi: 10.1097/01.mat.0000171595.67127.74. [DOI] [PubMed] [Google Scholar]
- 28.Thourani VH, Kirshbom PM, Kanter KR, et al. Venoarterial extracorporeal membrane oxygenation (VA-ECMO) in pediatric cardiac support. Ann Thorac Surg. 2006;82:138–144. doi: 10.1016/j.athoracsur.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 29.Huang SC, Wu ET, Chen YS, et al. Extracorporeal membrane oxygenation rescue for cardiopulmonary resuscitation in pediatric patients. Crit Care Med. 2008;36:1607–1613. doi: 10.1097/CCM.0b013e318170b82b. [DOI] [PubMed] [Google Scholar]
- 30.Ghez O, Fouilloux V, Charpentier A, et al. Absence of rapid deployment extracorporeal membrane oxygenation (ECMO) team does not preclude resuscitation ecmo in pediatric cardiac patients with good results. ASAIO J. 2007;53:692–695. doi: 10.1097/MAT.0b013e318151412f. [DOI] [PubMed] [Google Scholar]
- 31.Chan T, Thiagarajan RR, Frank D, Bratton SL. Survival after extracorporeal cardiopulmonary resuscitation in infants and children with heart disease. J Thorac Cardiovasc Surg. 2008;136:984–992. doi: 10.1016/j.jtcvs.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 32.Allan CK, Thiagarajan RR, Armsby LR, et al. Emergent use of extracorporeal membrane oxygenation during pediatric cardiac catheterization. Pediatr Crit Care Med. 2006;7:212–219. doi: 10.1097/01.PCC.0000200964.88206.B0. [DOI] [PubMed] [Google Scholar]
- 33.Tajik M, Cardarelli MG. Extracorporeal membrane oxygenation after cardiac arrest in children: what do we know? Eur J Cardiothorac Surg. 2008;33:409–417. doi: 10.1016/j.ejcts.2007.12.018. [DOI] [PubMed] [Google Scholar]