Abstract
Background
Despite the known health risks of hypertension, many hypertensive patients still have uncontrolled blood pressure. Clinical inertia, the tendency of physicians not to intensify treatment, is a common barrier in controlling chronic diseases. This trial is aimed at determining the impact of activating patients to ask providers to make changes to their care through tailored feedback.
Methods
Diagnosed hypertensive patients were enrolled in this RCT and randomized to one of two study groups: (1) the intervention condition - Web-based hypertension feedback, based on the individual patient’s self-report of health variables and previous BP measurements, to prompt them to ask questions during their next physician’s visit about hypertension care (2) the control condition- Web-based preventive health feedback, based on the individual’s self-report of receiving preventive care (e.g., pap testing), to prompt them to ask questions during their next physician’s visit about preventive care. The primary outcome of the study is change in blood pressure and change in the percentage of patients in each group with controlled blood pressure.
Conclusion
Five hundred participants were enrolled and baseline characteristics include a mean age of 60.0 years; 57.6% female; and 77.6% white. Overall 37.7% participants had uncontrolled blood pressure; the mean body mass index (BMI) was in the obese range (32.4) and 21.8% had diabetes. By activating patients to become involved in their own care, we believe the addition of the web-based intervention will improve blood pressure control compared to a control group who receive web-based preventive messages unrelated to hypertension.
Keywords: Hypertension, Internet, tailored-feedback, web-based
1. Introduction
Hypertension is a growing global concern affecting an estimated one billion people worldwide with approximately 50–65 million residing in the United States [1–3]. Hypertension is strongly associated with increased risk of cardiovascular disease (CVD), with CVD being the number one cause of death in the US [2, 4]. Clinical trials have shown that blood pressure control has decreased the rate of stroke, myocardial infarction and heart failure [5]. A study using data from the National Health and Nutrition Examination Survey (NHANES) showed that despite these known benefits of blood pressure control, only 50% of diagnosed hypertensive patients in the United States have their blood pressure under control [3].
Engaging patients in their own care (patient activation) is a widely agreed-upon self-management goal for chronic diseases such as hypertension. Positive changes in patient activation can lead to positive self-management behavior changes in patients with chronic conditions [6]. One important way for patients to be involved in their care is to ask questions during physician visits. Kravitz and colleagues observed that standardized patients who asked for a treatment for depression were nearly eight times as likely to receive a prescription for an antidepressant medication as standardized patients who made no request [7]. This is consistent with many studies that report that prompting patients to ask their providers specific questions leads to changes in care [8–12]. Patient prompts have been widely successful in improving preventive care, however no definitive studies have been proven effective in understanding the potential impact on the care of chronic illness [8, 13, 14].
Because approximately three-fourths of North Americans have access to the Internet [15] and 80% of those have sought health information [16], the Internet is a viable channel for a wide variety of health-related interventions. In a meta-analysis of 75 randomized controlled trials, Portnoy and colleagues concluded that computer-delivered interventions can lead to improvements in health-related knowledge as well as modifying health related behaviors [17]. It has also been shown that giving web-based personalized feedback can be efficacious in other chronic diseases, for example in the treatment of problem drinkers [18]. Investigators have created interventions that use the Internet to educate patients and help them self-manage illnesses and modify behaviors [19–21]. However, no interactive website has been identified that enable patients to enter individual information about their condition to learn questions to ask their physician with the goal of improving blood pressure control.
In an article from Science in 2003, Williams, Willard and Snyderman describe the need for novel heath services based on personalized care. If these mechanisms are successful they will provide improved outcomes, affordable payment mechanisms, enhanced patient safety and greater patient involvement in their own care [22]. Given the potential role of the Internet for helping patients to know what to ask their providers, we set out to answer the question: - Would providing a web-based tool help patients learn what questions to ask their physician during a visit help to improve blood pressure control?- Given that Americans increasingly manage aspects of their lives using the Internet, we believe that this question is of great significance in improving hypertension care. If effective, this approach could prove useful for other conditions for which evidence based guidelines exist. This study is the first to give computer-tailored reminders and feedback directly to patients to encourage them to ask their physician about modifications to a patient’s chronic disease management regimen.
2. Target Population
Because a primary objective of the study is to understand the efficacy of the web-based tool among patients with hypertension, participants are required to have regular Internet access. A trade-off inherent to web-based interventions is that the patients who may be in greatest need of an intervention may not have access to the Internet [16]. As of December 2008, the Pew Internet and American Life Project noted that 74% of American adults had access to the Internet at home or work [16]. This rate was lower, however, for African-Americans (64%) and individuals with incomes < $30,000/year (57%), groups who characteristically have the lowest rates of blood pressure control [23]. For example, though the rates of blood pressure control increased for non-Hispanic black men between 1988–2004, the rates of blood pressure control were lower compared to non-Hispanic white men (29.9% v. 36.2%) [23]. This pattern was similar for women and even more striking for Mexican-American men and women.
Our interest in pursuing the Internet as an intervention channel, despite the disparities in control seen in populations with lower Internet access rates, is twofold: 1) the majority of US adults do have Internet access; therefore the majority of US adults with hypertension would have access to this intervention channel; and 2) the Internet can deliver interventions very cost effectively, due to advertising support in a business model that has increasingly proven to be viable for useful websites [24, 25]. Therefore, web-based interventions that are proven to be effective can be easily disseminated, an advantage over other interventions that require more costly interventions, such as nurse case management.
Primary Care Providers (PCPs) whose practices were located within 40 miles of the Penn State Hershey Medical Center (PSHMC) in Central Pennsylvania were recruited. To maximize recruitment of minority patients, Census data (www.census.gov) were used to create a list of zip codes within 40 miles of PSHMC with the highest racial and ethnic minority populations. A list of PCPs within these zip codes was then purchased from a marketing firm (SK&A, Inc.). Recruitment letters were mailed to providers. Study staff members made follow-up phone calls to assess the level of interest of the physicians in having their practice participate in the study. A project director and a project coordinator visited physicians who expressed interest in order to more fully explain the study. Out of the 836 letters that were sent to practices throughout Central Pennsylvania, 15 practices met with Study Project Managers and 7 practices were recruited. The physicians willing to participate then signed a data use agreement to allow the research staff access to their patients’ medical records. Primary care and Internal Medicine Physicians within PSHMC ambulatory clinics were also recruited to participate in this study. Providers outside of the PSHMC system were reimbursed $100 per participant recruited into the study. Providers within the PSHMC system were not financially reimbursed because they were part of the same institution as the study staff. As a research institution, providers within the PSHMC system are expected to aid in clinical trials. Due to the low demand of this study for providers within the PSHMC system it was determined that no burden was placed on providers that would warrant compensation. Because there was very little burden placed on providers either outside or within the PSHMC system we do not expect the differences in compensation to affect providers behaviors.
After recruiting the practice site, the study staff visited the practice to review the charts of patients to determine potential eligibility (TABLE 1). Patients meeting these criteria were mailed letters co-signed by their primary care provider and the study investigator to recruit them for the study. In order to ensure a representative sample of the minority population in the area, recruitment letters were sent from provider locations that were located in areas with high percentages of racial and ethnic minority populations. Patients interested in participating were then encouraged to call the toll-free study number. During a screening phone call, patients were explained the study and assessed for the remaining inclusion and exclusion criteria.
Table 1.
Patient inclusion and exclusion criteria.
Inclusion Criteria
|
Exclusion Criteria
|
3. Study Design and Methods
The purpose of this randomized controlled trial (RCT) is to determine whether patient-tailored reminders and feedback will prompt participants to ask questions about their hypertension management during their physician visits and lead to changes in blood pressure control. The intervention was designed to help participants overcome clinical inertia in their care, or the tendency of providers to not make a change to the plan of care for participants who are not at their treatment target [26, 27]. By activating participants to become involved in their own care, the hypothesis is that the addition of the web-based intervention will improve clinical outcomes (% of patients at goal for BP) compared to a control who receives web-based preventive messages unrelated to hypertension. The secondary hypothesis is that providers also will be activated to change behavior (e.g. prompting them to make treatment intensifications) to improve hypertension outcomes.
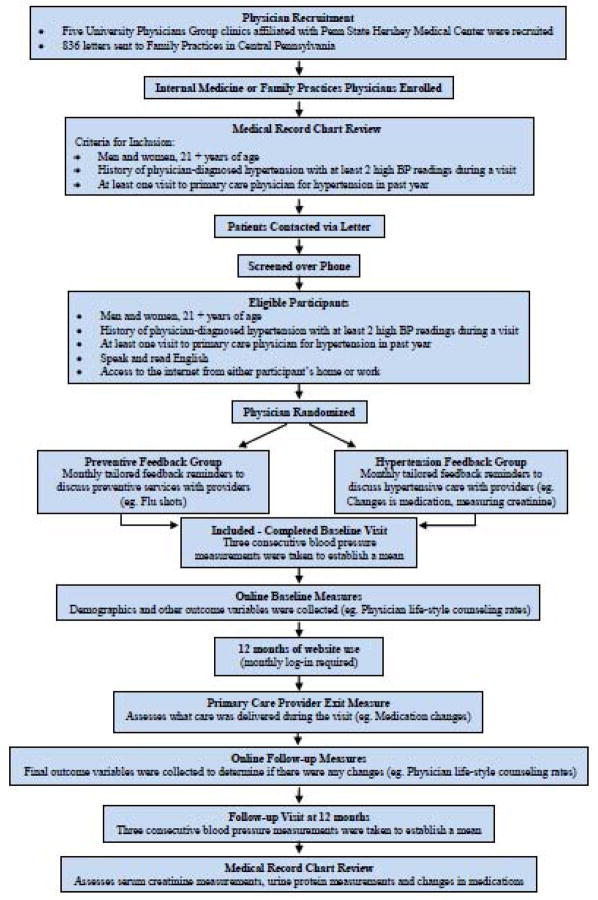
Because the intervention was designed to improve clinical inertia in hypertension care, the provider was the unit of randomization (see FIGURE 1 for flowchart of the study). To be eligible for the study, all physicians were board-certified in internal medicine or family practice, did not have specialty training in nephrology or cardiology, were clinically active (at least 50% of their time spent providing direct primary care) and were not planning to retire in the next two years, listed as retired, part-time or inactive.
Figure 1.
Flowchart of web quality hypertension study.
Randomization by provider did not allow us to fully control the balance of the study groups. Because the number of eligible patients per provider varied from the actual number of participants per provider, the study groups became slightly off-balance. The effects of the differences in study groups were determined to not be statistically significant.
Eligible participants were scheduled for a baseline visit (BLV) at their physician’s office, where their blood pressure was measured and study staff recorded their current prescriptions. After the BLV, they were randomized according to provider to the intervention condition (hypertension feedback) or control condition (preventive feedback). They completed the online baseline measures (OBM), where demographic data were collected. After their first visit with their PCP, participants completed an exit survey to assess what care was delivered during the visit (e.g., medication changes made). At the end of the 12 month period, participants complete follow-up self-reported measures online and a face-to-face follow-up visit (FUV) is scheduled where their blood pressure is assessed as well as their current prescriptions are recorded by study staff.
Research participants are compensated up to $190 in the form of gift cards at several stages throughout the study. At the BLV participants were given $40. When participants complete their PCP exit measures they were mailed $10. Throughout the study participants can earn $5 for each month they use the website for a potential $60. At participant’s FUV they are compensated $80 for visit attendance.
This study was done with full institutional review and approval per Penn State Hershey Medical Center’s Institutional Review Board.
4. Intervention
4.1 Intervention Condition
Intervention condition (IC) participants receive access to the hypertension module of the web-based intervention for 12 months, which include: 1) Web-based hypertension feedback, based on the individual patient’s self-report of health variables, 2) A - Pocket Chart - that patients can print and take to their doctor visits to help them collect important numerical data during that can later be entered into the website, 3) Automated reminders that track the dates of upcoming visits with their PCP, and remind patients to use the website before physician visits. Participants were prompted to enter the date of their next PCP visit every time they completed the online questions. Participants were expected to use the website at least once each month and received reminder emails if 30 days had elapsed since the last time they used the website.
On the website (www.myexpertdoctor.com), patients answer questions about their blood pressure (e.g., last value of systolic and diastolic blood pressure) and their previous hypertension care (e.g., date and value of last creatinine blood test). The patient is then provided with on-screen feedback based on their responses and the current guideline, which also includes questions that they may want to ask their physician to improve their care (e.g., - Can I lower my blood pressure by drinking less alcohol?-). Participants also receive a layperson description of the scientific rationale for the statement, and a link to a reputable external website that validates asking the suggested question. As low health literacy is a known problem in primary care, the feedback messages were written at an average Flesch-Kincaid grade level of 6.1 [28]. While only links that were written for lay audiences were chosen, rather than links for health professionals, we anticipate that these include messages that are hard to understand for some patients. To limit this, we chose links to well-established organizations (e.g., American Heart Association). The on-screen feedback is generated based upon participant responses to the survey questions. The feedback is prioritized, so that the highest priority recommendations appear at the top of the page based upon the JNC7 [2].
The web-based feedback is based on the most recent hypertension guidelines (JNC7) [2]. JNC7 was reviewed for the presence of specific recommendations on hypertension management. Recommendations were ranked based on the strength of the evidence supporting them in addition to the likelihood of impact. For example, while JNC7 recommends checking potassium before initiating therapy, its impact on blood pressure control or on the morbidity from hypertension is likely to be limited [2]. From previous work by our team in studying a similar migraine headache website, it appeared that the efficacy of a recommendation intervention was related to its placement on the webpage, with those placed at the top of the online feedback page being most effective [29]. This is consistent with the - primacy effect -, noted in the communications literature, that items placed first in a message are likely to have the greatest effect [30, 31]. This is also consistent with the time restraints and other competing demands of the physician visit [32, 33]. We assumed, therefore, that patients could only practically ask 1–2 questions during physician visits and expect that these questions will be appropriately addressed. For this reason, the prioritization of recommendations was done so that the highest priority (most widely accepted) recommendations appear at the top of the web page. For example, on the top of the web page we focused the feedback on the target values of systolic and diastolic blood pressure, since these are a consistent focus of recommendations from the JNC7 [2], National Committee for Quality Assurance [34] and a recent national study from RAND [35]. TABLE 2 shows sample recommendations and sample tailored messages.
Table 2.
Sample recommendations and tailored messages for subjects not adherent to recommendation.
| Recommendation from JNC7 | Message |
|---|---|
| The blood pressure should be controlled to less than 130/80 in patients with diabetes or chronic kidney disease and to less than 140/90 in others. | WHAT CAN YOU DO TO HELP ME LOWER MY BLOOD PRESSURE? Your blood pressure is too high. The goal for your top number is less than 130, and the goal for your bottom number is less than 80. Your current blood pressure of 152 over 94 puts you at risk for stroke, heart attack, and kidney damage. You need to keep BOTH numbers under control. Your doctor can give you one or more medicines, increase the dose of your medicines, or refer you to a blood pressure specialist. Your doctor should keep making changes in your care until your blood pressure numbers get to the goal. |
| Physicians should discuss medication adherence. | WHAT KIND OF ROUTINE WOULD HELP ME TO TAKE MY MEDICINES EACH DAY? From what you’ve told us, you don’t have a routine for taking your medicine. It is very helpful to take your medicines the same way each day. Some people buy a pillbox or use a timer or take their medicine when they brush their teeth. Your doctor may have other helpful ideas. It is important that you find some routine, as it will help you to control your blood pressure. |
| Physicians should address barriers to adherence. | SHOULD A BLOOD PRESSURE MEDICINE BE CHANGED TO ONE THAT DOESN’T BOTHER ME? From what you’ve told us, a blood pressure medicine may be bothering you. It is often hard to know what is causing bothersome symptoms. They may or may not be from a medicine. Your doctor may do one of the following:
|
| Physicians should discuss lifestyle changes. | WHAT LIFESTYLE CHANGES WOULD HELP TO CONTROL MY BLOOD PRESSURE? Lifestyle changes can help people lower their blood pressure. Weight loss, regular exercise and eating less salt, more fruits, vegetables and low-fat dairy products have all been proven to help. You should talk to your doctor about which of these changes may be most helpful for you. |
| Follow-up should be at least each month until blood pressure is controlled. | SHOULD I BE SEEN MORE FREQUENTLY UNTIL MY BLOOD PRESSURE IS CONTROLLED? From what you’ve told us, your blood pressure is not controlled and your next visit is more than 2 months away. You should talk to your doctor about this. You shouldn’t go more than 2 months without seeing your doctor if your blood pressure is not controlled. You may want to call to make an appointment that is sooner than the one that is planned. |
| Serum creatinine and potassium should be monitored regularly. | AM I DUE TO HAVE A BLOOD TEST FOR CREATININE AND POTASSIUM? At least once every year, people with high blood pressure should have a blood test for creatinine and potassium. People with high blood pressure are at high risk for kidney damage. People with more creatinine and potassium in the blood need to have their blood pressure controlled more closely. |
The feedback received by participants is based upon JNC7 guidelines and is tailored specifically to their response to the survey questions [2]. For example, it is recommended that patients have their serum creatinine checked yearly to screen for hypertensive kidney damage. Our intervention will prompt patients to ask their doctor about checking their creatinine level if it has not already been done within the past year. Along with the feedback, participants are provided with a - Pocket Chart - that they can print out at home and bring to their physician visit. This pocket chart will help participants keep track of their latest lab values and blood pressure measurements.
In addition to the feedback that is tailored specifically to hypertension, feedback is provided regarding other confounding conditions, such as obesity and diabetes. For example, if a participant indicates that he/she has not had a blood test for diabetes within the past five years, he/she will be prompted to ask their doctor about whether they should have the test done. Additionally, the feedback suggests participants talk to their doctors as to other lifestyle changes that could lower their blood pressure, such as weight control and getting regular exercise.
The main objective in providing participants with questions to ask their physicians, as opposed to just giving participants specific guidelines to follow, is to encourage patient activation. By prompting participants to ask their physician specific questions, we anticipate that participants will become more engaged in their healthcare and will develop a more open relationship with their physician. One of the primary outcome variables we are analyzing is to determine if there is a difference in quality of care (and the health outcomes) in participants who actively engage their physicians by asking specific questions compared to those who do not.
The intervention was designed to be used before a visit with the physician who provides the patient’s hypertension care. For that reason, it was essential to track the dates of these visits so the patients could be reminded to use the intervention before their visits. We assume that the intervention would be significantly less effective if used long before or following an office visit, as the intervention is designed to - activate - patients to ask specific questions during visits. For that reason, participants in both conditions received monthly email reminders to log into the website for the sole purpose of clarifying the dates of upcoming physician visits. In addition, patients in both conditions receive email reminders to use the site, starting 10 days before their physician visit and repeated twice if the participant has not used the site before the planned visit. This is also critical as the tailored feedback is based on variables that may change (i.e. recent lab or blood pressure values), so using the website just before the physician visit is preferred, in order to have the most accurate feedback. This approach has worked well, with over 90% of patients in the pilot randomized trial for migraines using the website before a physician visit [29].
An important requirement of the intervention is that patients enter a few critical bits of data about their health, such as their latest creatinine value, systolic and diastolic blood pressure values at their last visit. For that reason, we created a wallet-sized - Pocket Chart - to help patients collect test results from their doctor during visits. These values can later be entered into the website, by patients, to create accurate tailored reports. Patients are encouraged to print the - Pocket Chart - and bring it to their doctor visits and ask their physician to record test results, or ask their physician for the test value and record it themselves. Overall, the use of a small - Pocket Chart - will insure that the data that patients enter into the website, and therefore the feedback, will be accurate.
We chose not to give computer-tailored feedback reports to physicians for two main reasons: First, reports given to patients have proven widely effective at improving preventive care [8]. Second, reminders to physicians have not proven consistently effective at improving chronic disease management [14, 36–38].
4.2 Control Condition
The control condition (CC) is identical to the intervention condition (IC), except that the content of the CC intervention was focused on preventive services, rather than hypertension. The content of the questions and feedback on the website focus on non- hypertension-related preventive services (e.g., mammography screening, tetanus immunizations). The control condition participants, therefore also receive the core components of the intervention (Web-based personalized feedback, pocket chart and automated email reminders), but the content area focus on preventive services, rather than hypertension. The control condition, being an active treatment control condition was designed to improve preventive care, but is unlikely to change hypertension care. This control condition design was chosen to limit attrition and control for contact time, which will best enable us to address the specific aims of the study. Many similar studies have used this control group design [39–41]. We considered several different control conditions, including a no treatment control condition and a delayed treatment control condition. As patients with chronic medical conditions, such as hypertension, are less likely to receive preventive services such as mammography [42–44], we have chosen an active treatment control condition that seeks to enhance the delivery of preventive services. In addition, a recent study by Halpern and colleagues noted that physicians may be much more receptive to active- rather than placebo- controlled drug trials [45]. We believe that an active treatment control condition will also limit physicians desire to provide extra interventions to patients who they believe are not getting the active treatment. By limiting the tendency for co-intervention by physicians, the potential effects of the intervention are maintained as well as our ability to recruit and retain physicians and their patients.
5. Study Outcomes
5.1 Primary Outcome
The primary outcome measure is blood pressure control (TABLE 3). Based on this measurement, and the participants - history of diabetes or chronic kidney disease from chart reviews, blood pressure is categorized as - controlled - or - not controlled -. We expect that the intervention group will have a greater percentage of participants with controlled blood pressure than the control group. Hypertension guidelines from the NIH (JNC7) suggest that patients with diabetes or chronic kidney disease should have a blood pressure target of less than 130/80 and all other adults with uncomplicated hypertension should have a blood pressure target of less than 140/90 [2]. If both the systolic and diastolic blood pressure is lower than the respective target, blood pressure is categorized as - controlled -. If either the systolic or diastolic blood pressure is equal to or greater than the target, blood pressure is categorized as - not controlled -. This dichotomous outcome of - controlled-/- not controlled serves as the main outcome measure for the study and is the variable upon which the sample size calculations were performed.
Table 3.
Primary and Secondary Outcomes with Collection Schedule
| Outcome | Measurement | Data Sources | Collection Schedule | ||||
|---|---|---|---|---|---|---|---|
| BLV | Months 1–12 | PCP | FUV | Chart Review | |||
| Primary | |||||||
| Change in diastolic, systolic, and mean blood pressure | Recorded blood pressure values taken by research coordinators blinded to randomization scheme | Cardinal Health Adult L & XL | X | X | |||
| Percent with controlled blood pressure | Recorded blood pressure values taken by research coordinators blinded to randomization scheme | Cardinal Health Adult L & XL | X | X | |||
| Secondary | |||||||
| Urine protein levels testing in previous 12 months | Chart Review; Self-report online survey | Medical Record review; Self-reported data by participants through online survey | X | X | X | ||
| Serum creatinine testing in previous 12 months | Chart Review; Self-report online survey | Medical Record review; Self-reported data by participants through online survey | X | X | X | ||
| Lifestyle counseling in previous12 months | Self-report online survey based on JNC7 guidelines* | Self-reported data by participants through online survey | X | X | |||
| Medication Intensiification | Prescriptions given by primary care physician | Self-report at BLV and FUV | X | X | |||
| Fidelity Measures | |||||||
| Utilization of the website | Percent of participants who used the website on a monthly basis | Monitoring of participant log-in on website | X | X | |||
| Study visit attendance | Percent of participants who attended the two study visits | Attendance of study visits | X | X | |||
7th Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure: JNC Express. 2003, U.S. Department of Health and Human Services: Bethesda, MD.
At the BLVs and FUVs, blood pressure is measured according to a standardized protocol [46–48]. Dr. Bonita Falkner, a co-author on the recommendations from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research [47] oversaw the blood pressure measurement protocol and the training of research staff in the measurement of blood pressure. Trained personnel measured blood pressure after the participant rested for at least five minutes in the seated position. Using a blood pressure cuff that was appropriately sized to the participant’s upper arm, blood pressure was measured by auscultation. Three separate blood pressure measurements were taken to establish a mean value that was used as the blood pressure value for each participant.
5.2 Secondary Outcomes
After each visit with the participant’s PCP, the participant receives an email with a link to complete a brief online survey, the PCP Exit Measures. This survey asks about topics that may have been discussed during the visit (eg. Did you discuss what can be done to lower your blood pressure? Did your physician recommend you that you start taking and new medications for your hypertension?). Questions are also asked about the ways in which the website was used before and during the visit. For example, we ask participants whether or not the website content was printed and brought to the physician visit.
The main secondary outcomes of the study are processes of care that indicate a higher level of quality of care, as recommended in evidence-based guidelines [2]. The list of these quality-oriented processes of care includes: 1) serum creatinine measurement; 2) urine protein measurement; 3) counseling about lifestyle changes (e.g., salt restriction, weight loss); and 4) medication intensifications. These outcomes is measured by chart review and questionnaires filled out during Online Baseline Measures and Online Follow-up Measures. Specific recommendations regarding these processes of care for patients with hypertension are made in the JNC7 [2]. Our goal for these measures is to determine the impact of the intervention on the quality of care, other than blood pressure control, as the website makes recommendations that are specific to these quality-oriented processes of care. For example, JNC7 recommends measuring serum creatinine at least once each year [2], so the website has been designed to ask patients to enter the date of the last time these tests were performed. Participants who have not had the tests in the past year are then encouraged to talk to their physician about having them done. From the chart reviews, we will then be able to compare the percentage of participants in each condition who have had their urine protein and serum creatinine measured in the previous year. We hypothesize that participants in the IC condition will be significantly more adherent to these processes of care than will patients in the CC.
As a part of the outcome analysis, the fidelity measures are analyzed by passive tracking of website use. Each login by participants is recorded, as well as the duration of each login, the number of pages viewed, and the number of times that participants receive the computer-tailored feedback. The active part of the intervention is the computer-tailored feedback, thus representing the - dose - of the intervention. Dose will be measured as a proportion of participants that use the website on a monthly basis, expressed as a percentage. We hypothesize that participants with higher levels of intervention fidelity will be positively related to changes in blood pressure.
6. Statistical Analysis
6.1 Sample Size
In the current study, we are powered to detect an effect size that translates to a Relative Risk of 1.5 (60%/40%). We chose this conservative effect size to: 1) address possible differences in demographics (e.g., Internet access and health insurance) between our sample and other previous studies; 2) address possible differences in efficacy between interventions to increase preventive services and studies such as ours that seeks to change chronic disease management practices; and 3) have the power to detect a clinically significant effect. Given the well-documented morbidity and mortality from uncontrolled hypertension, a 20% difference between groups is highly clinically significant.
Using formulas developed by Cohen (1988)[49], our calculations indicate that 12 practices per treatment group (24 total) with at least 200 patients per treatment group (400 total) need to be available for analysis at 12 months to give us the power to see a significant difference between conditions in the percentage of patients with controlled hypertension (60% v. 40%). Assuming a 12-month follow-up rate of 90% for practices and 80% for participants within each remaining practice, we recruited 13 practices per treatment group (26 practices total) and 500 total participants.
6.2 Statistical Analysis Plan
Initially, the two randomized groups will be compared on important demographic and other baseline variables to ensure successful randomization. If groups are determined to be different on some measures, we will make them statistically equivalent by including those theoretically meaningful confounders as covariates in subsequent analyses. T-tests, ANOVA and/or chi-square tests of independence comparing those who complete the study with those lost to follow-up will be performed on baseline demographic variables and blood pressure control at baseline to identify potential differential dropout. These comparisons ensure equality of intervention and comparison groups after accounting for study attrition. For the primary outcome, we will apply intention to treat principles (ITT) [50] whereby two sets of analyses will be conducted. First, all available data will be included in one set of analyses. Second, participants lost to follow-up will be conservatively assumed to have not achieved blood pressure control thresholds. Similar findings between both approaches would increase confidence in the results overall.
Data analysis will focus on the primary hypothesis that participants in the IC condition will have a significantly greater blood pressure control rate at 12 months, as compared to CC participants. There are a number of ways that this outcome can be analyzed, such as using aggregate techniques (e.g. chi-square, t-tests) to analyze group differences in rates, but there are a number of considerations that make the logistic model the most tenable option. It is possible that the groups may have differences at baseline in potential confounders (e.g. socio-economic status, hypertension severity) that may contribute to group differences in the 12 month event rate between the two conditions. It is for these reasons that we will examine the primary outcome using the logistic regression model, which will be estimated using the generalized estimating equations (GEE) approach of Zeger and Liang (1986) [51]. We will first include the main effects of intervention assignment (IC vs. PC), and then introduce person-level covariates in a stepwise fashion. Finally, interaction terms will be included to test for potential modifying effects of covariates on treatment response.
7. Results
Baseline data has been collected on demographics as well as primary and secondary outcome variables. These data were then compared between treatment study groups. Because the blind on the study has not been lifted, the treatment and control groups have not been identified; therefore the groups were arbitrarily named Study A and Study B.
7.1 Enrollment
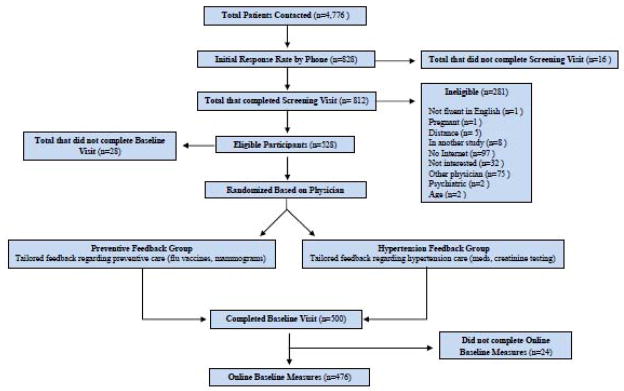
Five University Physicians Group clinics associated with Hershey Medical Center and 836 Family Practices were contacted to enroll in our study. Of the physicians contacted, 54 responded and agreed to participate (FIGURE 3).
After a medical record chart review, patients of enrolled physicians with a diagnosis of hypertension were sent letters recruiting them to participate in the study (n = 4,776) with 828 patients responding, of which 812 were screened for eligibility. Eligible participants (n = 528) were scheduled for a baseline visit (n = 500), where three consecutive blood pressures were measured, and they were enrolled in the study. Following the visit, the majority (95.2%) of participants (n = 476) logged onto the website and competed the Online Baseline Measures (OBM). From the 476 participants who completed the baseline measures questionnaire, demographic data as well as baseline secondary outcome data were collected.
7.2 Demographics
TABLE 4 reports the baseline characteristics as well as baseline data for outcome variables. As self-reported from the OBM (n = 476), the demographics of age, gender, race, ethnicity, education, and income were determined to have no significant difference between treatment study groups (p>0.05). However there was a significant difference between treatment study groups with regards to participants that are employed for wages, 51.7% in Study A and 36.1% in Study B (p=.001), which will be adjusted for in the final analysis. A noteworthy finding is the high rate of participants that completed four or more year of college (42.4%), while only 45% of participants are employed for wages. When evaluating the general health measures of BMI, smoking, and diabetes there was no significant difference between treatment study groups (p>0.05). It was also found that only 1.0% of participants enrolled in the study were uninsured, this is much lower than the US Census Bureau 2008 national average of 15.5% [52]. It was also found that the mean BMI was 32.4, indicating that the majority of participants are above their ideal weight. In fact, 83.2% of the participants in the study had a BMI in the category of overweight or obese with respect to the World Health Organizations classification of weight according to BMI. In addition, 21.8% were diagnosed with diabetes, demonstrating that this is generally an unhealthy population. Apart from employment status, there is no significant difference in demographics between study groups.
Table 4.
Baseline characteristics and outcome variables.
| Characteristic | Total (n=500) | Study A (n=282) | Study B (n=218) | p- value* |
|---|---|---|---|---|
| Age, mean (SD) | 60.0 (11.7) | 59.1 (12.0) | 61.1(11.2) | 0.069 |
| Gender, female, % | 57.6 | 58.5 | 56.4 | 0.639 |
| Race, White, % | 77.6 | 79.1 | 75.7 | 0.367 |
| Ethnicity, Hispanic, % | 2.6 | 3.5 | 1.4 | 0.131 |
| Education, College 4+ years, % | 42.4 | 41.7 | 43.4 | 0.707 |
| Income, < $50,000, % | 49.3 | 49.0 | 49.7 | 0.878 |
| Employed for Wages, % | 45.0 | 51.7 | 36.1 | 0.001 |
| BMI, mean (SD) | 32.4 (7.4) | 32.1 (7.3) | 32.8 (7.5) | 0.326 |
| Smoking, % | 8.6 | 7.7 | 9.8 | 0.440 |
| Diabetes, % | 21.8 | 22.5 | 21.0 | 0.408 |
| Systolic BP, mean (SD) | 132.6 (15.0) | 132.7 (14.9) | 132.4 (15.2) | 0.835 |
| Diastolic BP, mean (SD) | 75.5 (11.0) | 75.7 (11.1) | 75.2 (10.8) | 0.624 |
| Systolic BP control, % | 65.3 | 67.8 | 61.9 | 0.183 |
| Diastolic BP control, % | 86.4 | 86.3 | 86.6 | 0.916 |
| Overall BP control, % | 62.3 | 64.1 | 59.9 | 0.355 |
| Health, Very Good/Excellent, % | 33.6 | 32.5 | 35.1 | 0.545 |
| Number of BP medications, mean (SD) | 1.62 (1.0) | 1.52 (1.0) | 1.75 (1.1) | 0.017 |
| Internet use for health, ≥ once/month, % | 20.9 | 20.4 | 21.6 | 0.746 |
| Used Internet before a physician visit, % | 47.7 | 51.7 | 42.4 | 0.079 |
p-value from F test for continuous outcomes and Pearson Chi-squared test for categorical outcomes
7.3 Baseline outcome data
The primary outcome data collected at the baseline visit yielded an overall mean systolic blood pressure of 132.6 and a mean diastolic of 75.5 (TABLE 4). Using the JNC7 recommendations for blood pressure control, only 62.3% of participants were found to have their blood pressure under control. There was no significant difference in any of the blood pressure measures (mean systolic BP, p=0.84, mean diastolic BP, p=0.62, systolic BP control, p=0.18, diastolic BP control, p=0.92, overall BP control, p=0.36) found between treatment study groups.
Two of the secondary outcomes are based upon self-report of last serum creatinine and urine protein. Only 33.3% of participants were able report on these values in their OBM. It was therefore determined that self report of these statistics is not a reliable measure, therefore these outcomes will be assessed using data taken from the 12 month Chart Review.
As part of the OBM, the baseline lifestyle counseling rates were evaluated (TABLE 5). By definition all participants in the study were diagnosed with hypertension, however it was observed that only 53.4% of participants were advised to change their eating habits in the past year and only 55.3% were advised to be more physically active. It is also interesting to note that only 51.1% of participants were advised to lose weight while only 11.8% of participants had a BMI in the normal range.
Table 5.
Baseline lifestyle counseling rates.
| Within the past 12 months, has a doctor, nurse, or other health professional advised you to: | Total, % | Study A | Study B | p-value |
|---|---|---|---|---|
| (1) Eat fewer high fat or high cholesterol foods? | 53.6 | 52.0 | 55.6 | 0.364 |
| (2) Eat more fruits and vegetables? | 53.2 | 52.4 | 54.1 | 0.469 |
| (3) Lose weight? | 51.1 | 49.1 | 53.7 | 0.299 |
| (4) Be more physically active? | 55.3 | 55.4 | 55.1 | 0.516 |
| (5) Quit smoking? | 11.1 | 9.6 | 13.2 | 0.237 |
| (6) Drink less alcohol? | 6.7 | 7.0 | 6.3 | 0.497 |
As part of a secondary analysis, the change in number of blood pressure medications will be evaluated. It was observed that the mean number of blood pressure medications that participants took was 1.6, this number is consistent with the baseline mean of 1.6 medications taken in a separate 2008 hypertension intervention RCT done by Green et al.[53]. However, there was a significant (p=0.017) difference in the mean number of blood pressure medications between treatment study groups, and this will be adjusted for in the final analysis.
8. Discussion
This study is a randomized controlled trial that compares a web-based intervention designed to assist in the treatment of hypertension. Participants are able to enter their individual health information into the website and receive personalized feedback designed to facilitate communication with their physician regarding hypertension management. The two arms of the study are: (1) IC - feedback tailored specific for hypertension management and (2) CC - feedback on general preventive health management. The hypertension intervention being investigated relies on the use of web-based computer delivered personalized feedback to provide self-management support. It also helps in decision making by providing participants with specific questions to ask their physician to improve hypertension outcomes. The web-based component of the intervention incorporates technology and clinical information systems to manage the chronic condition of hypertension. Our intervention is designed to increase patient activation, encouraging patients to be self advocates for their own health. The feedback they receive from the website is designed to give them specific questions to ask their primary care physician regarding hypertension care. It is predicted that not only will these specific questions open the lines of communication, but will also increase the likelihood that patients are receiving care with accordance to the most current guidelines.
8.1 Strengths
The strengths of this study include the demonstrated health needs of the study population and the potential public health benefit of a web-based tool to improve health outcomes in hypertensive patients. The study population as a whole is representative of those for whom the intervention will be most useful. Overall racial minorities included in the study were greater than what is typical for Pennsylvania at large, with 22.4% being minority in the study population and 14.5% minority in Pennsylvania [54]. However because minorities are at a higher risk for developing hypertension and have poorer blood pressure control [55], this over-representation of minorities in our geographical area allows us to better model the actual population of individuals with hypertension.
This web-based intervention will be most helpful for those who are unhealthy; it is predicted to improve their hypertension control and therefore their overall health. Only 62.3% of the study population had their hypertension under control, over one fifth are currently being treated for diabetes and the majority are overweight or obese. The JNC7 recommends lifestyle modifications as first line therapy, stating, - Adoption of healthy lifestyles by all persons is critical for the prevention of high BP and is an indispensable part of the management of those with hypertension- [2]. With so many of the participants being overweight, it is expected that physicians are counseling their patients on lifestyle modifications. In a study using data taken from the 2005 Behavior Risk Factor Surveillance System (BRFSS) it was observed that 75.8% of patients were given exercise counseling for management of their hypertension [56]. This is greater than the 55.3% found to be given exercise counseling in our population. Also from the BRFSS, it was determined that of those given lifestyle counseling for hypertension, 82.1% reported making changes in eating habits and 72.5% made changes in exercise habits[57], demonstrating lifestyle counseling does lead to changes in habits. This supports the need for an intervention, such as the one being studied, in this population.
With approximately three fourths of the North American population having access to the Internet [15], there is a large potential for web-based interventions to reach those in need. Almost 60% of Internet users report using the Internet for health related searches for themselves in the past year [58]. Health information technology has the potential to increase savings, increase safety, and lead to better health [59, 60]. It has been shown that web-based blood pressure monitoring and communication can be effective in improving blood pressure control, demonstrating the feasibility of a web-based intervention improving blood pressure control [53]. Our goal is to expand this concept further by testing the hypothesis that utilization of an interactive web-based tool to help participants know what questions to ask during their visit will lead to improved blood pressure control.
An additional strength of the study is the use of an active treatment control group where participants are treated identically except that the content of the questions and feedback focus on non-hypertension related preventive services. This control condition design was chosen to limit participant attrition and control for contact time, which will best enable us to address the specific aims of the study. An active treatment control condition was chosen to enhance the delivery of preventive services. As patients with a chronic medical condition, participants still receive useful medical advice and prompts to ask their physicians.
8.2 Limitations
Limitations of this study include restriction to patients with access to the Internet, randomization of treatment groups by provider and minor differences in demographics. The Pew Internet and American Life Tracking Survey, in November-December 2008 observed that only 57% of US adults with a household income of < $30,000 had access to the Internet, compared to 94% for US adults with a household income of at least $75,000 [16]. Internet access also varies between rural (63%), urban (71%) and suburban (74%) populations. These differences are also observed between non-Hispanic whites (77%), non-Hispanic blacks (64%) and Hispanic adults (58%) [16]. It is therefore possible that individuals with chronic illness who are most in need of care and whose control of the illness is worse are at greatest risk of not having access to web-based interventions. With that said, a growing majority of individuals do have access to the Internet, and the ease with which web-based interventions can be accessed makes the Internet a potentially fruitful medium for interventions designed to improve chronic illness care.
A second limitation of the study was randomization by provider. Randomization by provider made recruiting difficult. We were not able to recruit patients from the Pennsylvania population as a whole, providers first had to be recruited before we could screen and contact their patients, adding an additional step in the process of recruitment. Because some providers had more patients than others enrolled in the study, this left an unequal number of participants in each intervention study group (Study A, n= 282 and Study B, n=218). Another problem is that a single provider may have an unequally large number of patients enrolled in the study allowing for the potential of the habits of an individual provider to affect the data.
A third limitation of the study is the minor differences in the population between treatment study groups and the general population. In particular, only 1.0% of our population was uninsured, which is dramatically lower than the national average of 15.5% [52]. The Institute of Medicine found that uninsured adults in the US have less access to recommended care, receive poorer quality of care and experience worse health outcomes than do insured adults [61]. This uninsured group was underrepresented in our study. Another difference found in our population was the high rate of participants who attended 4 or more years of college (42.2%), compared to 24.4% of the US population [55]. Yet it was also found that only 45.0% of participants were employed for wages, below the US national average of 63.9% [53]. We believe this high rate of college graduates and low employment rate is explained by the advanced age of our population, many of the participants being retired. With age being a known risk factor for hypertension and only a limited fraction of the elderly receiving adequate therapy [62], these results are expected and reflect that we have accurately targeted the population in need.
An additional potential limitation of the study concerns compensation of the participants. Although paying participants to use the website may limit the ability to make real-world inferences, participant compensation is widely accepted to improve participant recruitment, participation and retention. Our goal is to prove that use of the web-site can lead to better outcomes in hypertension control and we believe that compensating participants for their participation will not affect the outcomes being measured.
In summary, evidence exists that controlled hypertension reduces the risk of cardiovascular complications, and that generally patients can control their blood pressure through proper self-management. The primary goal of the study is to determine whether a web-based intervention that provides questions to ask their providers will help participants improve their hypertension. The intervention addresses important questions in patient activation, provider inertia, and hypertension control via the Internet. This intervention could also be adapted to other chronic diseases through other randomized, controlled interventions.
Figure 2.
CONSORT of patients through recruitment, randomization and baseline visits.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jeffrey Thiboutot, Email: jthiboutot@hmc.psu.edu.
Heather Stuckey, Email: hstuckey@hmc.psu.edu.
Donna Kephart, Email: dkephart@hes.hmc.psu.edu.
William Curry, Email: wjc8@psu.edu.
Bonita Falkner, Email: bonita.falkner@jefferson.edu.
Christopher Sciamanna, Email: cns10@psu.edu.
References
- 1.Harsha D, Bray G. Weight Loss and Blood Pressure Control. Hypertension: Journal of the American Heart Association. 2008:1420–1425. doi: 10.1161/HYPERTENSIONAHA.107.094011. Published Online. [DOI] [PubMed] [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, Cushman WD, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ the National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 3.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010 May 26;303(20):2043–50. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 4.Rosamond W, Flegal K, Friday G, et al. for the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics -2007 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69–e171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 5.Neal B, MacMahon S, Chapman N. Effects of ACE inhibitors, calcium antagonists, and other blood pressure- lowering drugs. Lancet. 2000;356:1955–1964. doi: 10.1016/s0140-6736(00)03307-9. [DOI] [PubMed] [Google Scholar]
- 6.Hibbard JH, Mahoney ER, Stock R, Tusler M. Do increases in patient activation result in improved self-management behaviors? Health Serv Res. 2007 Aug;42(4):1443–63. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kravitz RL, Epstein RM, Feldman MD, Franz CE, Azari R, Wilkes MS, et al. Influence of Patients’ Requests for Direct-to-Consumer Advertised Antidepressants: A Randomized Controlled Trial. Jama. 2005 Apr 27;293(16):1995–2002. doi: 10.1001/jama.293.16.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stone EG, Morton SC, Hulscher ME, Maglione MA, Roth EA, Grimshaw JM, et al. Interventions that increase use of adult immunization and cancer screening services: a meta-analysis. Ann Intern Med. 2002;136(9):641–51. doi: 10.7326/0003-4819-136-9-200205070-00006. [DOI] [PubMed] [Google Scholar]
- 9.Ornstein SM, Garr DR, Jenkins RG, Rust PF, Arnon A. Computer-generated physician and patient reminders. Tools to improve population adherence to selected preventive services. J Fam Pract. 1991;32(1):82–90. [PubMed] [Google Scholar]
- 10.Turner BJ, Day SC, Borenstein B. A controlled trial to improve delivery of preventive care: physician or patient reminders? J Gen Intern Med. 1989;4(5):403–9. doi: 10.1007/BF02599691. [DOI] [PubMed] [Google Scholar]
- 11.Becker DM, Gomez EB, Kaiser DL, Yoshihasi A, Hodge RH. Improving preventive care at a medical clinic: how can the patient help? Am J Prev Med. 1989;5(6):353–9. [PubMed] [Google Scholar]
- 12.Rosser WW, Hutchison BG, McDowell I, Newell C. Use of reminders to increase compliance with tetanus booster vaccination. Cmaj. 1992;146(6):911–7. [PMC free article] [PubMed] [Google Scholar]
- 13.Leveille SG, Huang A, Tsai SB, Allen M, Weingart SN, Iezzoni LI. Health coaching via an internet portal for primary care patients with chronic conditions: a randomized controlled trial. Med Care. 2009 Jan;47(1):41–7. doi: 10.1097/MLR.0b013e3181844dd0. [DOI] [PubMed] [Google Scholar]
- 14.Grol R. Improving the quality of medical care: building bridges among professional pride, payer profit, and patient satisfaction. Jama. 2001;286(20):2578–85. doi: 10.1001/jama.286.20.2578. [DOI] [PubMed] [Google Scholar]
- 15.Internet World Stats. [accessed 2010 Feb 22];World Internet Users and Population Stats. 2009 URL: http://www.internetworldstats.com/stats.htm.
- 16.Horrigan JB. Home Broadband Adoption 2008. Washington: Pew Internet and American Life Project; 2008. [Google Scholar]
- 17.Portnoy DB, Scott-Sheldon LAJ, Johnson BT, Carey M. Computer-delivered interventions for health promotion and behavioral risk reduction: a meta-analysis of 75 randomized controlled trials, 1988–2007. Prev Med. 2008;47(1):3–16. doi: 10.1016/j.ypmed.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cunningham JA, Wild TC, Cordingley J, Van Mierlo T, Humphreys K. Twelve-month follow-up results from a randomized controlled trial of a brief personalized feedback intervention for problem drinkers. Alcohol Alcohol. 2010 Feb; doi: 10.1093/alcalc/agq009. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krishna S, Francisco BD, Balas EA, Konig P, Graff GR, Madsen RW. Internet-enabled interactive multimedia asthma education program: a randomized trial. Pediatrics. 2003 Mar;111(3):503–10. doi: 10.1542/peds.111.3.503. [DOI] [PubMed] [Google Scholar]
- 20.Van der Meer V, van Stel HF, Detmar SB, Otten W, Sterk PJ, Sont JK. Internet-based self-management offers an opportunity to achieve better asthma control in adolescents. Chest. 2007 Jul;132(1):112–9. doi: 10.1378/chest.06-2787. [DOI] [PubMed] [Google Scholar]
- 21.Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Arch Intern Med. 2006 Aug 14–28;166(15):1620–5. doi: 10.1001/archinte.166.15.1620. [DOI] [PubMed] [Google Scholar]
- 22.Williams RS, Willard HF, Snyderman R. Personalized health planning. Science. 2003 Apr 25;300(5619):549. doi: 10.1126/science.300.5619.549. [DOI] [PubMed] [Google Scholar]
- 23.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008 Nov;52(5):818–27. doi: 10.1161/HYPERTENSIONAHA.108.113357. Epub 2008 Oct 13. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell D. A Small Empire Built on Cuddly and Fuzzy Branches Out From the Web. The New York Times; 2008. Aug 20, [Google Scholar]
- 25.Miller CC. Woman to Woman, Online. The New York Times; 2008. Aug 13, [Google Scholar]
- 26.Berlowitz DR, Ash AS, Glickman M, Friedman RH, Pogach LM, Nelson AL, Wong AT. Developing a quality measure for clinical inertia in diabetes care. Health Serv Res. 2005 Dec;40(6 Pt 1):1836–53. doi: 10.1111/j.1475-6773.2005.00436.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berlowitz DR, Ash AS, Hickey EC, Friedman RH, Glickman M, Kader B, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998 Dec 31;339(27):1957–63. doi: 10.1056/NEJM199812313392701. [DOI] [PubMed] [Google Scholar]
- 28.Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005 Nov-Dec;3(6):514–22. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sciamanna CN, Nicholson RA, Lofland JH, Manocchia M, Mui S, Hartmann CW. Effects of a website designed to improve the management of migraines. Headache. 2006 January;46:92–100. doi: 10.1111/j.1526-4610.2006.00312.x. [DOI] [PubMed] [Google Scholar]
- 30.Page MP, Norris D. The primacy model: a new model of immediate serial recall. Psychol Rev. 1998 Oct;105(4):761–81. doi: 10.1037/0033-295x.105.4.761-781. [DOI] [PubMed] [Google Scholar]
- 31.Brooks BM. Primacy and recency in primed free association and associative cued recall. Psychon Bull Rev. 1999 Sep;6(3):479–85. doi: 10.3758/bf03210838. [DOI] [PubMed] [Google Scholar]
- 32.Nutting PA, Rost K, Smith J, Werner JJ, Elliot C. Competing demands from physical problems: effect on initiating and completing depression care over 6 months. Arch Fam Med. 2000 Nov-Dec;9(10):1059–64. doi: 10.1001/archfami.9.10.1059. [DOI] [PubMed] [Google Scholar]
- 33.Parchman ML, Romero RL, Pugh JA. Encounters by patients with type 2 diabetes--complex and demanding: an observational study. Ann Fam Med. 2006 Jan-Feb;4(1):40–5. doi: 10.1370/afm.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.The State of Health Care Quality 2003: Industry Trends and Analysis. Washington, DC: National Committee for Quality Assurance; 2003. [Google Scholar]
- 35.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003 Jun 26;348(26):2635–45. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 36.Murray MD, Harris LE, Overhage JM, Zhou XH, Eckert GJ, Smith FE, et al. Failure of computerized treatment suggestions to improve health outcomes of outpatients with uncomplicated hypertension: results of a randomized controlled trial. Pharmacotherapy. 2004 Mar;24(3):324–37. doi: 10.1592/phco.24.4.324.33173. [DOI] [PubMed] [Google Scholar]
- 37.Rollman BL, Hanusa BH, Gilbert T, Lowe HJ, Kapoor WN, Schulberg HC. The electronic medical record. Arch Intern Med. 2001;161(2):189–97. doi: 10.1001/archinte.161.2.189. [DOI] [PubMed] [Google Scholar]
- 38.Tierney WM, Overhage JM, Murray MD, Harris LE, Zhou XH, Eckert GJ, et al. Effects of computerized guidelines for managing heart disease in primary care. J Gen Intern Med. 2003 Dec;18(12):967–76. doi: 10.1111/j.1525-1497.2003.30635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Flay BR, Graumlich S, Segawa E, Burns JL, Holliday MY. Effects of 2 prevention programs on high-risk behaviors among African American youth: a randomized trial. Arch Pediatr Adolesc Med. 2004 Apr;158(4):377–84. doi: 10.1001/archpedi.158.4.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nelson ME, Layne JE, Bernstein MJ, Nuernberger A, Castaneda C, Kaliton D, et al. The effects of multidimensional home-based exercise on functional performance in elderly people. J Gerontol A Biol Sci Med Sci. 2004 Feb;59(2):154–60. doi: 10.1093/gerona/59.2.m154. [DOI] [PubMed] [Google Scholar]
- 41.Broderick JE, Stone AA, Smyth JM, Kaell AT. The feasibility and effectiveness of an expressive writing intervention for rheumatoid arthritis via home-based videotaped instructions. Ann Behav Med. 2004 Feb;27(1):50–9. doi: 10.1207/s15324796abm2701_7. [DOI] [PubMed] [Google Scholar]
- 42.Fontana SA, Baumann LC, Helberg C, Love RR. The delivery of preventive services in primary care practices according to chronic disease status. Am J Public Health. 1997;87(7):1190–6. doi: 10.2105/ajph.87.7.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beckman TJ, Cuddihy RM, Scheitel SM, Naessens JM, Killian JM, Pankratz VS. Screening mammogram utilization in women with diabetes. Diabetes Care. 2001 Dec;24(12):2049–53. doi: 10.2337/diacare.24.12.2049. [DOI] [PubMed] [Google Scholar]
- 44.Bell RA, Shelton BJ, Paskett ED. Colorectal cancer screening in North Carolina: associations with diabetes mellitus and demographic and health characteristics. Prev Med. 2001 Feb;32(2):163–7. doi: 10.1006/pmed.2000.0785. [DOI] [PubMed] [Google Scholar]
- 45.Halpern SD, Ubel PA, Berlin JA, Townsend RR, Asch DA. Physicians’ Preferences for Active-controlled versus Placebo-controlled Trials of New Antihypertensive Drugs. J Gen Intern Med. 2002;17(9):689–95. doi: 10.1046/j.1525-1497.2002.11024.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.National High Blood Pressure Education Program/(NHBPEP)/National Heart, Lung, and Blood Institute (NHLBI) and American Heart Association (AHA) Working Group Meeting on Blood Pressure Measurement. Bethesday, Maryland: National Institutes of Health; 2002. Apr 19, [Google Scholar]
- 47.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005 Jan;45(1):142–61. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- 48.Beevers G, Lip GY, O’Brien E. ABC of hypertension: Blood pressure measurement. Part II-conventional sphygmomanometry: technique of auscultatory blood pressure measurement. Bmj. 2001;322(7293):1043–1047. doi: 10.1136/bmj.322.7293.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cohen J. Statistical Power Analysis for the Behavioral Sciences. New Jersey: Lawrence Erlbaum Ass; 1988. [Google Scholar]
- 50.Little R, Yau L. Intent-to-treat analysis for longitudinal studies with drop-outs. Biometrics. 1996 Dec;52(4):1324–33. [PubMed] [Google Scholar]
- 51.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986 Mar;42(1):121–30. [PubMed] [Google Scholar]
- 52.DeNavas-Walt C, Proctor B, Smith J. US Census Bureau, Current Population Reports, P60-236, Income, Poverty, and Health Insurance Coverage in the United States: 2008. U.S. Government Printing Office; Washington, DC: 2009. [Google Scholar]
- 53.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008 Jun;299(24):2857–2867. doi: 10.1001/jama.299.24.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.U.S. Census Bureau. PHC-2-1, United States Summary. Washington, DC: 2003. 2000 Census of Population and Housing, Summary Social Economic, and Housing Characteristics. [Google Scholar]
- 55.Rehman SU, Hutchison FN, Hendrix K, Okonofua EC, Egan BM. Ethnic differences in blood pressure control among men at Veterans Affairs clinics and other health care sites. Arch Intern Med. 2005 May;165(9):1041–7. doi: 10.1001/archinte.165.9.1041. [DOI] [PubMed] [Google Scholar]
- 56.Carlson SA, Maynard LM, Fulton JE, Hootman JM, Yoon PW. Physical activity advice to manage chronic conditions for adults with arthritis or hypertension, 2007. Prev Med. 2009 Aug-Sep;49(2–3):209–12. doi: 10.1016/j.ypmed.2009.06.017. Epub 2009 Jun 30. [DOI] [PubMed] [Google Scholar]
- 57.Viera AJ, Kshirsagar AV, Hinderliter AL. Lifestyle modifications to lower or control high blood pressure: is advice associated with action? The behavioral risk factor surveillance survey. J Clin Hypertens (Greenwich) 2008 Feb;10(2):105–11. doi: 10.1111/j.1751-7176.2008.07577.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Atkinson N, Saperstein S, Pleis J. Using the internet for health-related activites: findings from a national probability Sample. J Med Internet Res. 2009;11(1):e4. doi: 10.2196/jmir.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hillestad R, Bigelow J, Bower A, Girosi F, Meili R, Scoville R, Taylor R. Can Electronic Medical Record Systems Transform Healthcare? An Assessment of Potential Health Benefits, Savings, and Costs,-Health Aff (Millwood) 2005 Sep-Oct;24(5):1124–6. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 60.Taylor R, Bower A, Girosi F, Bigelow J, Fonkych K, Hillestad R. Promoting Health Information Technology: Is There a Case for More-Aggressive Government Action? Health Aff (Millwood) 2005 Sep-Oct;24(5):1234–45. doi: 10.1377/hlthaff.24.5.1234. [DOI] [PubMed] [Google Scholar]
- 61.Institute of Medicine (IOM) Care without Coverage: Too Little, Too Late. National Academy Press; Washington, D. C: 2002. [Google Scholar]
- 62.Casiglia E, Tikhonoff V, Pessina AC. Hypertension in the elderly and the very old. Expert Rev Cardiovasc Ther. 2009 Jun;7(6):659–65. doi: 10.1586/erc.09.17. [DOI] [PubMed] [Google Scholar]