Abstract
Purpose
The beneficial properties of β-glucans have been recognized for centuries. Their proposed mechanisms of action in cancer therapy occur via stimulation of macrophages and priming of innate neutrophil complement receptor 3 (CR3) for eliciting CR3-dependent cellular cytotoxicity of iC3b-opsonized tumor cells. The current study is to investigate whether β-glucan therapy has any impact on anti-tumor adaptive T cell responses.
Experimental Design
We first examined the trafficking of orally administered particulate yeast-derived β-glucan and its interaction with dendritic cells (DCs) that captured tumor materials. Antigen-specific T cells were adoptively transferred into recipient mice to determine whether oral β-glucan therapy induces augmented T cell responses. Lewis lung carcinoma and RAM-S lymphoma models were used to test oral β-glucan therapeutic effect. Further mechanistic studies including tumor-infiltrating T cells and cytokine profiles within the tumor milieu were determined.
Results
Orally administered particulate β-glucan trafficked into spleen and lymph nodes and activated DCs that captured dying tumor cells in vivo, leading to the expansion and activation of antigen-specific CD4 and CD8 T cells. In addition, IFN-γ production of tumor-infiltrating T cells and CTL responses were significantly enhanced upon β-glucan treatment, which ultimately resulted in significantly reduced tumor burden. Moreover, β-glucan-treated tumors had significantly more DC infiltration with the activated phenotype and significant levels of Th1-biased cytokines within the tumor microenvironment.
Conclusions
These data highlight the ability of yeast-derived β-glucan to bridge innate and adaptive anti-tumor immunity and suggest that it can be used as an adjuvant for tumor immunotherapy.
Introduction
Biological response modifiers (BRMs) derived from microbial products have represented important tools for defining mechanisms of host defense, but most BRMs have remained classified as non-specific because their exact mode of action was unknown. β-Glucan BRMs were first reported 45 years ago and have been extensively investigated for both their anti-tumor and anti-infective activity (1–4). Most β-glucan BRMs are derived from yeast, bacteria, barley, or fungi and have a backbone structure of linear β-1,3-linked D-glucose molecules (β-1,3-D-glucan). They also have β-1,6-linked side chains of β1,3-D-glucan of varying sizes that occur at different intervals along the backbone (5). There are at least four β-glucan receptors that have been identified: complement receptor 3 (CR3, CD11b/CD18, Mac-1, αMβ2 integrin) (6); lactosylceramide (7); scavenger receptor (8); and dectin-1 (9–11). In our previous studies, we showed that low molecular weight, soluble β-glucan derived from yeast could bind to CR3 lectin-like domain with high affinity and prime the receptor for subsequent cytotoxic activation of iC3b-coated tumor cells (12, 13). Furthermore, we and other investigators have demonstrated the therapeutic efficacy using combined yeast-derived or barley β-glucan with complement activating anti-tumor mAbs in a variety of murine syngeneic tumor models (14–17) as well as human carcinoma xenograft models (18–23). These studies reaffirm that dual occupancy of CR3 by lectin-like domain ligand β-glucan and inserted domain ligand iC3b is critical for β-glucan-mediated tumor immunotherapy. In addition, yeast-derived β-glucan-mediated tumor immunotherapy utilizes a novel mechanism by which innate immune effector neutrophils are primed to kill iC3b-opsonized tumors cells (16).
While these studies are mainly focused on the role of β-glucans on innate immune cells, recent studies suggest that β-glucans may also possess the regulatory properties on adaptive immune responses. For example, bacterial β-glucan Curdlan stimulates both Th1 and Th17 T cell responses (24) and exhibits a potent adjuvant effect on CD8 T cell priming (25). In addition, Curdlan is capable of converting regulatory T cells (Treg) into Th17 cells using an in vitro culture system (26). Th17 cells have been demonstrated to play a critical role in anti-tumor T cell responses (27–29). In contrast, zymosan β-glucan predominantly stimulates production of anti-inflammatory cytokines such as IL-10 and TGF-β (30). Zymosan in vivo treatment induces regulatory APCs and Ag-specific T cell tolerance. In addition, β-glucan from Candida albicans stimulates human monocyte differentiation into DCs, but these DCs inefficiently polarize naïve T cells (31). These new emerging data are of great importance and suggest a potential regulatory role of β-glucans in eliciting adaptive T cell responses. Thus, it is crucial to determine whether yeast-derived β-glucan treatment in cancer would promote or inhibit anti-tumor T cell responses.
In this study, we evaluated the potential effect of orally administered particulate yeast-derived β-glucan as whole β-glucan particles (WGPs) on adaptive T cell responses. We earlier showed that oral WGPs were taken up by macrophages that transported them to spleen, lymph nodes and bone marrow (BM). Within the marrow, the macrophages processed particulate β-glucan to release small soluble active β-glucan moiety that bound to CR3 of neutrophils for eliciting cytotoxicity of iC3b-opsonized tumor cells (32). Here, we report that WGPs activate DCs that capture tumor materials and that this subsequently leads to augmented Ag-specific CD4 and CD8 T cell responses. Orally administered WGP treatment caused significant tumor regression with enhanced anti-tumor T cell activity and alteration of the tumor microenvironment towards Th1 responses. Therefore, particulate yeast-derived β-glucan links both innate and adaptive immune responses and could serve as a potent adjuvant for effective tumor immunotherapy.
Materials and Methods
Reagents
Highly purified, soluble yeast β-glucan (PGG-Glucan) and particulate β-glucan WGP isolated from the cell wall of Saccharomyces cerevisiae were provided by Biothera (Eagan, MN). The β-glucan preparation contained <0.02% protein, <0.01% mannan, and 1% glucosamine. For some studies, WGPs were labeled with fluorescein dichlorotriazine (DTAF; Molecular Probes-Invitrogen, Carlsbad, CA) as described previously (32). The endotoxin level was 0.06 EU/ml as tested by the Gel-clot method (Associates of Cape Cod, East Falmouth, MA). Fluorochrome-conjugated anti-mouse mAbs including CD3 (17A2), CD4 (GK1.5), CD8(53-6.7), CD11c (N418), Gr-1 (RB6-8C5), CD25 (PC61), CD40 (HM40-3), CD80 (16-10A1), CD86 (GL1), CD49b/pan-NK (DX5α), F4/80 (BM8), MHC II (M5/114.15.2) and mouse Fc block (2.4G2) were purchased from eBiosciences (San Diego, CA).
Ovalbumin (OVA)-transfected Lewis Lung Carcinoma (LLC/OVA) cells
LLC cells were obtained from the American Type Culture Collection (Manassas). LLC cells were infected with pMiT-OVA retrovirus in the presence of 10 μg/ml polybrene after 24 hr pre-treatment with 250 ng tunicamycin (T7765; Sigma-Aldrich, St. Louis, MO). LLC cells that stably expressed high levels of OVA were sorted via MoFlo High Speed Cell Sorter (Dako-Cytomation, Fort Collins, CO). To ensure tumorigenicity, an additional selection was made by in vivo passage of the transfected cells in C57Bl/6 mice. The tumor cell lines with high OVA expression levels and capable of generating s.c. tumors were used for experiments.
Mice and tumor models
Wildtype (WT) C57BL/6 mice were purchased from National Cancer Institute (Frederick, MD). CD4 and CD8 OVA TCR transgenic (Tg) OT-I and OT-II mice were purchased from Taconic (Germantown, NY). The murine tumor protocols were performed in compliance with all relevant laws and institutional guidelines and were approved by the Institutional Animal Care and Use Committee of the University of Louisville.
For RMA-S-MUC1 tumor model, groups of C57Bl/6 mice received oral WGPs (100 μg, 200 μg, 400 μg, daily), beginning on the day 11 after palpable tumors were formed. Mice were treated for 3 weeks with tumor diameter measurements made with calipers every third day and mice were sacrificed when tumors reached 12 mm in diameter. Mice were observed for tumor-free survival over 100 days. For LLC/OVA tumor model, therapy was initiated 7 days before mice were implanted s.c. with LLC/OVA cells (1×107/mouse). Two groups of C57Bl/6 mice were treated with 200 μl of WGPs (4 mg/ml in saline; total 800 μg) or 200 μl of PBS given every other day using an intragastric gavage needle. Therapy was continuously administered for 3 weeks after palpable tumors were formed. Tumor diameters were measured every third day and mice were sacrificed when tumors reached 15 mm in diameter.
Induction of tumor cell apoptosis and in vivo delivery of dying tumor cells
LLC/OVA cells were cultured with 5 μM staurosporine (Sigma) for 6 h to induce apoptosis. Apoptotic tumor cells were assessed by Annexin V-FITC Apoptosis Detection Kit (BD Biosciences). Cells were labeled with carboxyfluorescein diacetate succinimidyl ester (CFSE) (Molecular Probes) or PKH26 (Sigma) as described previously (33). For in vivo delivery of dying tumor cells, 2 × 107 apoptotic CFSE-labeled LLC/OVA cells were injected i.v. into mice. Mice were sacrificed 2 h following dying tumor cell injection and the splenocytes were stained for CD11c and CD8. In some experiments, mice receiving dying PKH26-labeled LLC/OVA cells were treated with or without orally administered WGPs (400 μg daily) and the splenocytes were prepared and stained with CD11c-allophycocyanin and FITC-conjugated mAbs CD40, CD80, and CD86 and MHC class II or isotype control mAbs.
Bone marrow-derived DCs (BMDCs)
BMDCs were generated as described previously (34). Cultured BMDCs at day 7 were used for experiments. BMDCs were further purified with anti-CD11c-microbeads (Miltenyi Biotec Inc., Auburn, CA). Purity was >90% assessed by flow cytometry.
In vitro and in vivo T cell proliferation assay
For in vitro assay, OT-I (CD8+) or OT-II (CD4+) T cells were purified by microbead separation (Miltenyi) from splenocytes of OT-I or OT-II Tg mice. T cells (1×105) were co-cultured with irradiated (2500 rads) DCs (2×104) and dying LLC/OVA tumor cells (1×105) in the presence or absence of WGP or PGG treatment for 72 h. 3H-thymidine (1.0 μCi/well; ICN, Irvine, CA) was added during the last 16 h of culture. For in vivo assay, OT-I or OT-II T cells were labeled with 10 μM CFSE for 10 min at 37°C as previously described (35). T cells (1 × 106/mouse) were adoptively transferred into mice treated with or without oral WGPs. One-day later, mice were injected with apoptotic LLC/OVA cells. Recipient mice were continuously treated with WGPs for 5 days and the turnover of T cells was examined by flow cytometry.
In vivo cytotoxicity assay
For preparation of target cells, splenocytes from naïve C57BL/6 mice were labeled with CFSE at 5 μM (CSFEhigh) or 0.5 μM (CFSElow). The CSFEhigh population was pulsed with 10 μg/ml of OVA SIINFEKL peptide for 4 h. Equal numbers of OVA peptide-pulsed CSFEhigh and no-peptide-pulsed CSFElow cells were mixed and adoptively transferred into LLC/OVA tumor-bearing mice treated with or without WGPs. Naïve mice without tumors were used as controls. After 24 h, spleen cells were harvested and killing activity was assessed using flow cytometry. Percent killing was determined by CFSE+ gate after normalizing each sample to controls by the formula [1-(ratioexperimental/ratiocontrol)×100] where ratio=%CSFEhigh/% CSFElow.
Quantitative real-time PCR (qRT-PCR)
Tumor samples were treated with TRIzol reagent (Invitrogen) and total RNA was isolated and reverse-transcribed with TaqMan Reverse Transcription Reagents (Applied Biosystems, Foster City, CA). The indicated cytokine mRNA levels were quantified by qRT-PCR amplification using the BIO-RAD (Hercules, CA) MyiQ single color RT-PCR detection system. Briefly, cDNA was amplified in a 25 μl reaction mixture containing 12.5 μl of SYBR Green PCR supermix (BIO-RAD), 100 ng of cDNA template, and selected primers (200 nM) using the recommended cycling conditions (denaturation at 95°C for 10 min followed by 40 cycles of 95°C for 15 sec and 63°C for 1 min). The primer sequences, designed with Primer Express software (Applied Biosystems) were summarized in the supplementary Table I.
Immunofluorescence and immunohistochemistry staining
C57BL/6 mice were orally gavaged daily for 8 days with 2 mg DTAF-WGPs and then sacrificed. Fresh spleen and inguinal lymph nodes were embedded in Tissue-Tek® optimal cutting temperature (OCT) compound 4853 (Electron Microscopy Science, Hatfield, PA). Cryosections (7 μm) were fixed in ice-cold acetone and air-dried. Sections were stained with the biotinylated rat anti-mouse CD11c (eBioscience) at 4°C overnight. After three washes with PBS, sections were incubated with steptavidin-Alexa 594 (Molecular Probes) and then imaged on a Leica TCS SP5 confocal microscope system with an HC PL APO 20x/0,7 CS (air) objective (Leica Microsystems Inc., Exton, PA).
For tumor sample immunohistochemistry staining, tumor sections were first blocked with avidin/biotin blocking kit (Vector Laboratories, Burlingame, CA) and then stained with the biotinylated rat anti-mouse CD11c mAbs. After three washes with PBS, sections were incubated with the steptavidin-HRP secondary Ab (Thermo Scientific, Rockford, IL). Slides were rinsed in PBS and then incubated with the 3-amino-9-ethylcarbazole (AEC) substrate solution (Vector Laboratories). Slides were then counterstained with hematoxylin and mounted with Clear-Mount mounting medium (Electron Microscopy Science).
Graphing and statistical analysis of data
Data from each experiment were entered into Prism 4.0 (GraphPad Software, San Diego, CA) to generate bar graphs or graphs of tumor regression and to determine the significance of differences between data sets. Student T-test was used to compare differences between each dataset.
Results
Orally administered particulate β-glucan WGPs directly interact with DCs in situ and stimulate DCs that phagocytose apoptotic tumor cells for maturation
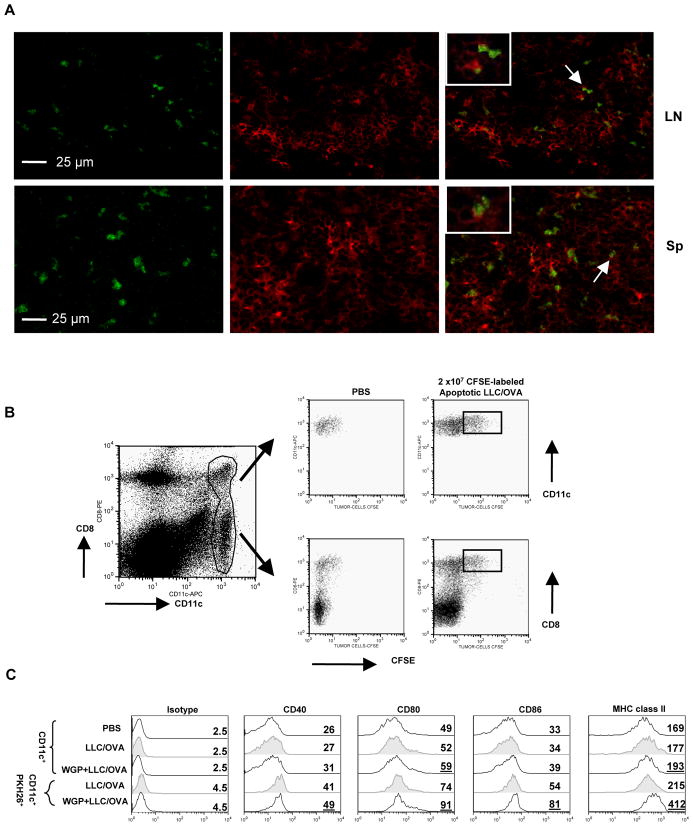
Previous studies have shown that orally administered particulate β-glucan WGPs are captured predominantly by macrophages or mucosal M cells that transport them to the BM, spleen, and lymph nodes (32). To determine whether oral WGP would directly interact with DCs, mice were fed orally with DTAF-labeled WGPs. Fluorescence microscopy revealed that WGPs were readily seen in both spleen and lymph nodes (Figure 1A). Co-localization study demonstrated that WGPs directly interacted with CD11c+ DCs and some of the WGP particles were phagocytosed by DCs.
Figure 1. Oral WGPs migrate to the spleen and lymph node and interact with DCs.
(A) Mice were fed orally with DTAF-WGPs (green). Spleen (Sp) and inguinal lymph nodes (LN) were cryosectioned and stained with anti-CD11c mAb (red). (B) Mice were injected with 2 ×107 CFSE-labeled apoptotic LLC/OVA tumor cells or PBS. At 2 h after injection, spleen cells were harvested and stained with mAbs against CD11c and CD8α. Data show that DCs uptaking CFSE-positive apoptotic tumor cells are CD8α+. Cells were gated on CD11c+ population. (C) Groups of mice (n=5) were treated with WGPs daily for 7 days (400 μg/mouse). Fluorescein dye PKH26-labeled apoptotic LLC/OVA tumor cells (2 × 107/mouse) were injected i.v. into C57Bl/6 mice. Five hours later, mice were sacrificed and spleen cells were isolated and stained with mAbs against CD11c, CD40, CD80, CD86, MHC class II, and relevant isotype controls. Cells were gated on CD11c+populations or CD11c+ and PKH26+ populations. Data show that co-stimulatory CD40, CD80, CD86, and MHC class II molecules are significantly upregulated in DCs capturing tumor materials after WGP treatment. Numbers represent mean fluorescent intensity (MFI).
We next determined whether DCs could take up the apoptotic tumor cells and interact with orally administered WGPs. Apoptotic LLC/OVA tumor cells were labeled with CFSE and then injected i.v. into mice. We followed the uptake of CFSE-labeled apoptotic tumor cells in vivo by lymph node or splenic DCs. As shown in Figure 1B, CFSE-labeled apoptotic tumor cells were predominantly phagocytosed by splenic CD11c+DCs. Consistent with previous finding (33), only the CD8α+CD11c+ DC subset from spleen endocytosed the injected CFSE-labeled dying tumor cells. In experiments not depicted, we found that few CFSE-labeled tumor cells were taken up by other CD11c− fractions of spleen, which were marked for CD11b+ macrophages.
To determine whether orally fed WGPs stimulate DC activation in vivo, groups of mice injected with fluorescein dye PKH26-labeled apoptotic LLC/OVA tumor cells i.v. were treated with or without orally administered WGPs. Splenic DCs were analyzed by flow cytometry for the expression of a number of cell surface molecules. As indicated in Figure 1C, injection of apoptotic tumor cells alone had little effect on the phenotype of the total CD11c positive population with respect to the PBS control. In addition, the expression levels of surface markers on total DCs were marginally upregulated in total CD11c+DCs in the presence of WGP treatment (Figure 1C, third row). Strikingly, with WGP treatment, surface markers such as co-stimulatory CD80, CD86, and MHC class II molecules were significantly upregulated in DCs that had captured apoptotic tumor cells, revealed by examining cells positive for CD11c and PKH26 (Figure 1C, compare fourth and fifth row). Therefore, the oral administration of WGPs allows DCs that capture tumor materials to activate in vivo.
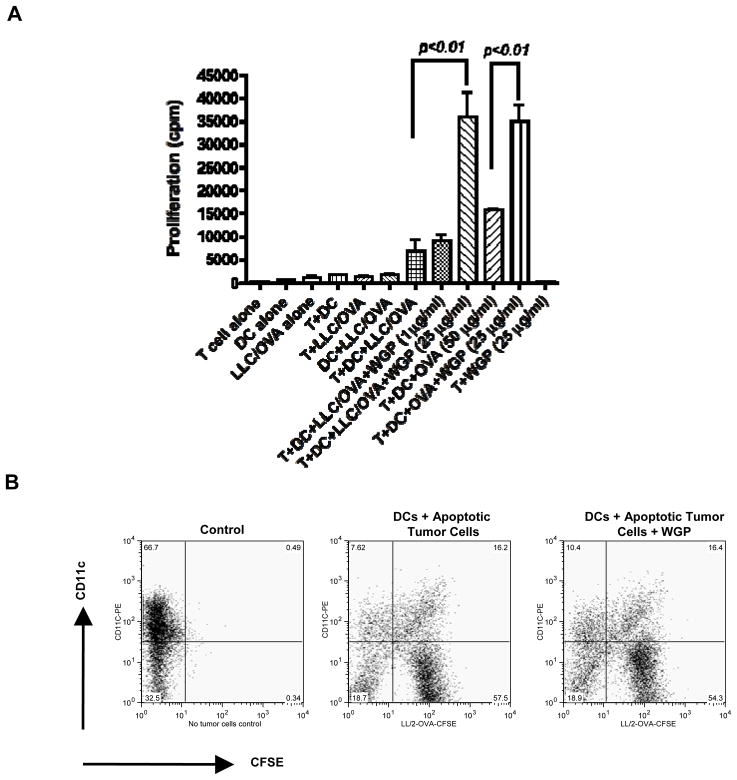
WGP treatment induces enhanced Ag-specific CD4 and CD8 T cell responses
To determine if enhanced Ag-specific T cell responses would be induced by delivery of dying tumor cells to DCs upon WGP treatment, we first co-cultured DCs in vitro with apoptotic LLC/OVA tumor cells and OVA CD4 or CD8 T cells in the presence or absence of WGP treatment. WGP treatment significantly augmented OVA Tg CD4 T cell proliferation in vitro (Figure 2A). Similarly, CD8 T cell proliferation was also significantly increased (data not shown). However, WGPs did not have direct effect on T cell proliferation. To examine the possibility that WGP treatment could enhance the uptake of dying tumor cells by DCs, DCs were co-cultured with apoptotic tumor cells in the presence or absence of WGPs. As shown in Figure 2B, WGPs did not enhance DC-mediated phagocytosis of apoptotic tumor cells in vitro.
Figure 2. WGPs significantly increase Ag-specific T cell proliferation in vitro but do not enhance DC-mediated apoptotic tumor cell phagocytotosis.
(A) BMDCs were co-cultured with apoptotic LLC/OVA tumor cells and purified CD4 OVA Tg T cells in the presence or absence of varying amounts of WGPs. DCs with CD4 Tg T cells in the presence of OVA Ag (50 μg/ml) with or without WGPs were used as positive controls. (B) CFSE-labeled apoptotic LLC/OVA cells were co-cultured with BMDCs in the presence or absence WGPs in vitro for 24 hrs. Cells were then analyzed by flow cytometry.
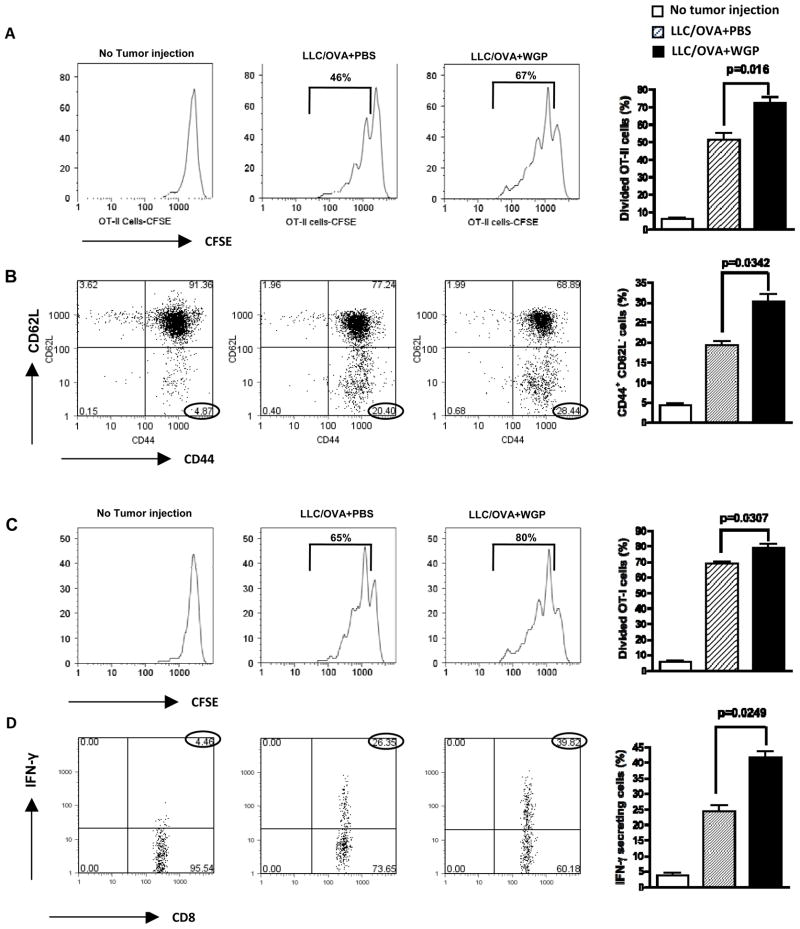
We next examined whether orally administered WGPs enhance Ag-specific T cell responses in vivo. Groups of mice were injected with apoptotic LLC/OVA tumor cells and CFSE-labeled OVA TCR Tg CD4 T cells (OT-II) were adoptively transferred. As depicted in Figure 3A, augmented CD4 T cell proliferation was induced in response to WGP treatment. In addition, the number of activation/memory phenotypes of CD4 T cells as defined as CD44highCD62Llow was significantly increased in WGP-treated mice (Figure 3B). Similarly, OVA CD8 T cell proliferation was also augmented upon WGP treatment (Figure 3C). Furthermore, the number of IFN-γ-producing CD8 T cells was significantly increased in WGP-treated mice (Figure 3D). These data strongly suggest that particulate β-glucan WGP treatment leads to augmented Ag-specific CD4 and CD8 T cell responses both in vitro and in vivo.
Figure 3. Enhanced Ag-specific T cell responses upon oral WGP in vivo treatment.
(A) Groups of mice (n=3) treated with or without WGPs (400 μg/daily/mouse for 7 days) were injected i.v. with or without apoptotic LLC/OVA tumor cells. After 24 h, mice were adoptively transferred with CFSE-labeled OT-II CD4 T cells. Mice were continuously treated with or without WGPs for 5 days and sacrificed. Splenocytes were examined by flow cytometry. Cells were gated on CFSE positive cells. Percentage indicates proliferated cells. (B) Splenocytes were stained with mAbs against CD44 and CD62L. Cells were gated on CFSE positive populations. (C) Groups of mice (n=3) treated with or without WGPs were injected with or without apoptotic LLC/OVA tumor cells. After 24 h, mice were adoptively transferred with CFSE-labeled OT-I CD8 T cells. Mice were continuously treated with or without WGPs for 5 days and sacrificed. Splenocytes were examined by flow cytometry. Cells were gated on CFSE positive cells. Percentage indicates proliferated cells. (D) Splenocytes were restimulated with OVA (50 μg/ml) for 24 h and then stained for intracellular IFN-γ production. Cells were gated on CD8+ T cells.
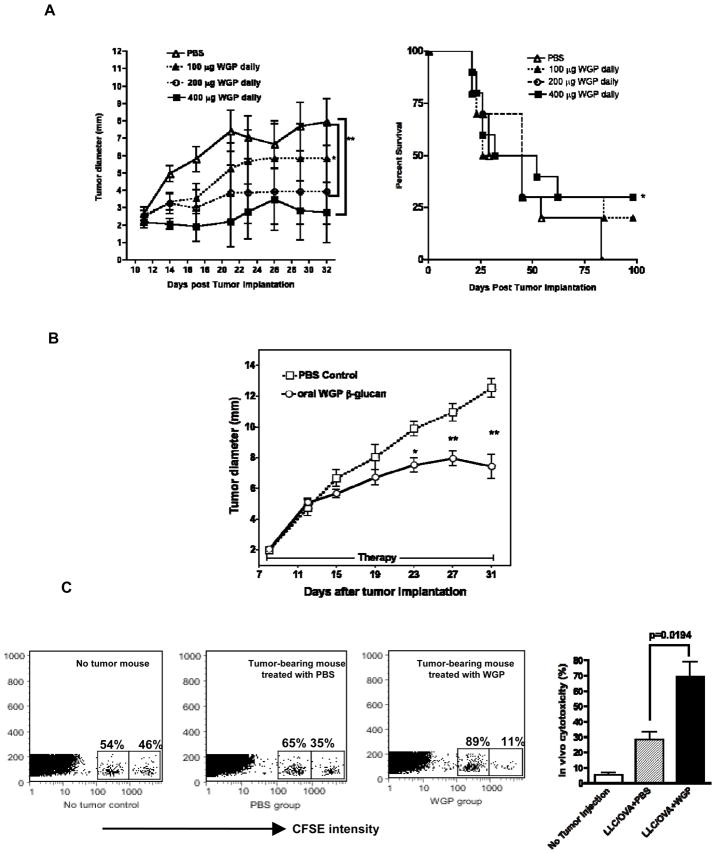
WGP treatment in vivo significantly delays tumor progression with increased CD8-mediated cytotoxic activity
Our previous studies have demonstrated that WGP in combination with anti-tumor mAbs exhibited enhanced therapeutic efficacy (32, 36). To examine whether WGP treatment alone without exogenously administered anti-tumor mAbs would have any therapeutic efficacy, we first used RAM-S-MUC1 lymphoma model. Groups of mice were given oral WGP treatment at different doses. WGP treatment with three different doses all caused delayed tumor growth compared to saline treatment. Significance was observed when tumor-bearing mice received 200 μg and 400 μg WGP daily treatment. More importantly, WGP treatment with 400 μg daily dose also achieved significant prolonged survival (Figure 4A).
Figure 4. WGP treatment significantly reduces tumor burden and prolongs survival with increased CD8 T cell killing activity.
(A) Groups of mice (n=10) were implanted s.c. with RMA-S-MUC1, and after 11 days, to allow tumor formation, were treated with oral WGPs at different does (100 μg, 200 μg, 400 μg, daily) for 3 weeks. Tumor-free survival was also monitored. Points, mean; bars, SE. *p<0.05, **p<0.01. (B) Groups of mice (n=12) were implanted s.c with LLC/OVA tumor cells. After palpable tumors formed, mice were treated with or without orally administered WGPs for three weeks. Tumor diameters were recorded at the indicated time. *p<0.05, **p<0.01. Points, mean; bars, SE. (B) Tumor-bearing mice with LLC/OVA (n=3) treated with or without WGPs for three wks were adoptively transferred with OVA Class I peptide loaded CFSEhigh splenocytes with unloaded CFSElow splenocytes. Mice were sacrificed after 24 hrs and CFSE+ cells were gated and analyzed by flow cytometry. Data show that tumor-bearing mice treated with WGPs have the highest cytotoxicity against target cells compared to PBS treated or naïve mice.
To further confirm the therapeutic benefit provided by WGPs in other tumor models, groups of mice were implanted with LLC/OVA tumor cells. As shown in Figure 4B, tumor-bearing mice treated with WGPs exhibited a significantly smaller tumor burden as compared to those treated with saline at day 23, day 27, and day 31 after tumor implantation. Further studies revealed that depletion of both CD4 and CD8 T cells completely abrogated WGP-mediated therapeutic efficacy (data not shown). Next, CD8 T cell killing activity was evaluated in tumor-bearing mice treated with or without WGPs. As shown in Figure 4C, mice without tumors had minimal killing activity. Mice with tumors but with PBS control treatment had approximately 30% killing activity. Strikingly, tumor-bearing mice treated with oral WGP treatment had over 70% killing activity. These data suggest that WGP treatment can significantly delay tumor progression, presumably via activating anti-tumor adaptive T cell responses.
WGP treatment in vivo significantly enhances tumor-infiltrating IFN-γ-producing T cells and DC infiltration within tumors and modulates the cytokine secretion profile
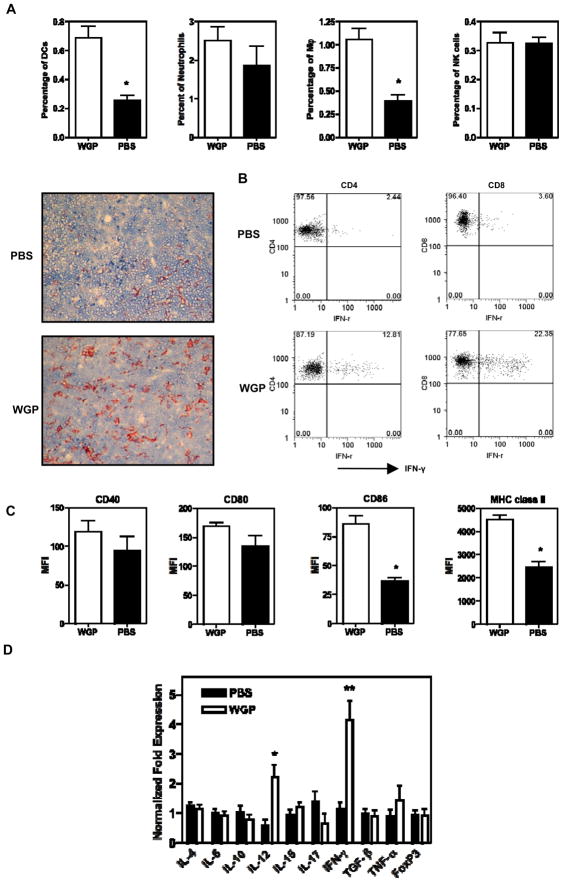
It is becoming clear that tumors can actively subvert the immune system through a variety of immune suppressive mechanisms within the tumor microenvironment (37, 38). To determine whether WGP treatment had any impact on the tumor microenvironment, we examined the types of infiltrating cells and cytokine profiles within the LLC/OVA tumors. Tumors from mice treated with or without orally administered WGPs were excised and live cells were stained with different mAbs including CD4, CD8, Gr-1 (granulocytes), F4/80 (macrophages), CD11c (DC), and NK 1.1 (NK cells). The number of tumor-infiltrating CD4, CD8, granulocytes, and NK cells was not significantly altered upon WGP treatment (Figure 5A and data not shown). However, tumor-infiltrating CD4 and CD8 T cells secreted abundant IFN-γ upon OVA stimulation in WGP-treated mice compared to those in PBS-treated mice (Figure 5B). In addition, the number of tumor-infiltrating DCs and macrophages was significantly increased upon WGP treatment (Figures 5A). More importantly, CD86 and MHC class II expression levels were significantly increased on tumor-infiltrating DCs after WGP treatment in vivo (Figure 5C). Similar results were observed in tumor-infiltrating macrophages (data not shown).
Figure 5. WGP treatment significantly increases IFN-producing T cells and DC infiltration within the tumors and drives Th1 cytokine production in the tumor microenvironment.
(A) LLC/OVA tumor specimens (n=5) from WGP-treated or untreated mice were prepared for single cell suspensions. Tumor infiltrating cells were assessed by flow cytometry. Data indicate that oral WGP treatment in vivo significantly increases DC and macrophage infiltration within the tumors. Tumor samples were cryosectioned for immunohistochemistry staining with anti-CD11c mAb, which shows brown staining. Magnification ×200. The sections shown in this figure are representative tumor sections of 10 total tumor specimens. (B) Single cells from tumors treated with or without WGPs were re-stimulated with OVA (50 μg/ml) for overnight and then performed surface staining with mAbs against CD4 or CD8 and intracellular IFN-γ staining. Cells were gated on CD4+ or CD8+ T cell populations. (C) Single cell suspensions were stained with mAbs against CD11c, CD40, CD80, CD86, and MHC class II. Cells were gated on a CD11c+ population. *P<0.05. (D) RNAs from tumor specimens treated with or without WGPs (5 tumors per group) were extracted and reverse-transcribed for RT-PCR for the indicated cytokines and transcriptional factor FoxP3. *p<0.05; **p<0.01.
Next, we examined whether cytokine profiles in the tumor milieu would be altered with or without WGP treatment. To this end, LLC tumors from WGP-treated or un-treated mice were excised and RNAs were extracted for RT-PCR. As shown in Figure 5D, the levels of IL-4, IL-6, IL-10, IL-15, IL-17, TGF-β, TNF-α, and Foxp3 were not significantly changed. Strikingly, IL-12 and IFN-γ mRNAs were both significantly increased within the tumor milieu after WGP treatment. These data suggest that WGPs are able to modulate the tumor microenvironment towards Th1 responses.
Discussion
Over a century ago, Sir William B. Coley observed spontaneous tumor regression in some patients afflicted simultaneously with bacterial infection (39). Coley’s toxins, a mixture of heat-killed bacteria, were hypothesized to be effective to induce tumor regression. In recent decades, it was discovered that bacteria contain conserved pathogen-associated molecular patterns (PAMPs) that stimulate immune responses (40). β-Glucans are major components of the cell wall of various fungi or bacteria and can be recognized as PAMPs by the mammalian innate immune system. Their mechanism of action in cancer therapy occurs mainly via priming innate effector neutrophil CR3 to induce cytotoxicity of iC3b-opsonized tumor cells (41). Combined yeast-derived β-glucan with anti-tumor mAb therapy is currently approved by the FDA for its clinical investigation in Phase I/II trials (42). However, recent studies have suggested that β-glucans also have a critical role in regulating T cell responses (24, 30). Thus, the goal of the current study was to investigate the possible interplays between β-glucan therapy and anti-tumor T cell responses.
Previously, we showed that orally administered WGPs could be captured by gastrointestinal macrophages that trafficked into the BM, lymph node, and spleen (32). This property was recently used by other investigators to effectively deliver proinflammatory cytokine silencing genes in mouse macrophages via engineering of glucan-encapsulated short interfering (si)RNA particles (43). In this study, we found that orally administered WGPs trafficked into spleen and lymph nodes and directly interacted with DCs. More importantly, WGPs stimulated splenic DCs that captured tumor materials to up-regulate surface accessory molecules, which are critical for T cell activation. Although it is surprising that WGPs only induce DC activation when these DCs have captured apoptotic tumor cells, it is possible that the DCs that interact with WGPs are also the ones that preferentially capture tumor cells. It is worth noting that DCs that captured tumor material had upregulated surface accessory molecules even without WGP stimulation (data not shown). However, WGP treatment further activated these DCs that had captured apoptotic tumor cells (Figure 1c). Regardless, WGP in vivo treatment subsequently leads to the augmented Ag-specific CD4+ and CD8+ T cell responses. This is demonstrated by two systems. Using the OVA-specific T cell adoptive transfer approach, we showed that WGP treatment could stimulate Ag-specific CD4 and CD8 T cell expansion and activation. In the LLC/OVA tumor model, we further demonstrated that augmented anti-tumor CD4 and CD8 T cell responses were elicited in WGP-treated tumor-bearing mice, thus leading to the reduced tumor burden.
Interestingly, yeast zymosan β-glucan stimulates DCs to secrete abundant IL-10 but little IL-6 and IL-12, thus inducing immune tolerance (30, 44). In contrast, the current study demonstrates that particulate yeast-derived β-glucan WGPs stimulate IL-12 and IFN-γ production within the tumor microenvironment and significantly promote anti-tumor Th1 responses. These observed differences in DC cytokine profiles and subsequent T cell responses could be attributed to the differential compositions of zymosan vs. WGPs as we suggested previously (45). Zymosan is an insoluble cell wall preparation and composes fewer β-glucans (12- to 14%). WGPs although purified from the same strain of yeast, S. cerevisiae, contain significantly more β-glucan (>85%). We found that in vitro WGPs predominantly trigger DCs to secrete IL-12 and TNF-α, but low amounts of IL-6 and IL-10, and that they significantly upregulate co-stimulatory molecules and MHC class II (supplemental Figure). These observations reaffirm the notion that different compositions of β-glucan preparations could lead to distinct biological outcomes.
It is becoming clear that the tumor microenvironment plays a critical role in tumor immunotherapy, as tumors can actively subvert the immune system to establish an immune suppressive environment (37, 38). Therefore, the main challenge of tumor immunotherapy is to modulate the suppressive tumor microenvironment to favor the elicitation of strong anti-tumor immune responses. We demonstrated that particulate β-glucan WGPs modulate the tumor microenvironment towards Th1 responses via actively recruiting DCs into the tumor milieu and further activating them. The activated tumor-infiltrating DCs elicit augmented anti-tumor CD4 and CD8 T cell responses evidenced by the fact that tumor-infiltrating T cells produce abundant IFN-γ. However, it is unknown how WGP treatment engenders more DC infiltration within tumors. It is possible that WGPs may mobilize DC precursors from the BM. Indeed, previous studies have demonstrated that β-glucan is capable of mobilizing hematopoietic stem/progenitor cells from the BM niche to the periphery (46, 47). It is also possible that DC trafficking into tumors is regulated by different subset of T cells. A recent study demonstrated that Th17 cells promote DC infiltration into lung cancer tissues (27).
Our previous study demonstrated that orally administered WGP β-glucan synergizes with anti-tumor mAbs to induce significant tumor regression and achieve long-term tumor-free survival (32). These effects were ascribed to the in vivo CR3 priming of effector neutrophils because their therapeutic efficacy was significantly decreased in CR3-deficient mice. However, WGP treatment only showed significant long-term tumor free survival with respect to untreated or mAb-treated animals in RAM-S-MUC1 tumor model and this efficacy is independent of CR3 (32), which is consistent with our current findings. Based on the current results, we speculate that this effect is due to the activation of anti-tumor T cell responses elicited by WGPs. Thus, combined therapy with β-glucan WGPs not only elicits neutrophil-mediated CR3-dependent cytotoxicity but also stimulates anti-tumor T cell responses to provide a more effective means of eliminating tumors and develop a long-term tumor-specific T cell immunity that prevents tumor recurrence.
Statement of Translational Relevance.
Combined yeast-derived β-glucan with anti-tumor mAb therapy is currently approved by the FDA for its clinical investigation in Phase I/II trials. The mechanism of action of β-glucan in cancer therapy occurs mainly via priming innate effector neutrophil CR3 to induce cytotoxicity of iC3b-opsonized tumor cells. The current study demonstrated that yeast-derived particulate β-glucan exhibited potent adjuvant effect on promoting anti-tumor T cell responses. The findings will not only advance our understanding of the action mode of β-glucan but also have potential for direct clinical utilization by enhancing the effect of cancer immunotherapy.
Supplementary Material
Acknowledgments
Grant support: This work was supported by NIH/NCI RO1 CA86412, RO1CA150947, and Kentucky Lung Cancer Research Program.
References
- 1.Diller IC, Mankowski ZT, Fisher ME. The effect of yeast polysaccharides on mouse tumors. Cancer Res. 1963;23:201–8. [PubMed] [Google Scholar]
- 2.Di Luzio NR, Williams DL, McNamee RB, Edwards BF, Kitahama A. Comparative tumor-inhibitory and anti-bacterial activity of soluble and particulate glucan. Int J Cancer. 1979;24:773–9. doi: 10.1002/ijc.2910240613. [DOI] [PubMed] [Google Scholar]
- 3.Hunter JT, Meltzer MS, Ribi E, Fidler IJ, Hanna MG, Jr, Zbar B, et al. Glucan: attempts to demonstrate therapeutic activity against five syngeneic tumors in guinea pigs and mice. J Natl Cancer Inst. 1978;60:419–24. doi: 10.1093/jnci/60.2.419. [DOI] [PubMed] [Google Scholar]
- 4.Lavigne LM, O’Brien XM, Kim M, Janowski JW, Albina JE, Reichner JS. Integrin engagement mediates the human polymorphonuclear leukocyte response to a fungal pathogen-associated molecular pattern. J Immunol. 2007;178:7276–82. doi: 10.4049/jimmunol.178.11.7276. [DOI] [PubMed] [Google Scholar]
- 5.Ensley HE, Tobias B, Pretus HA, McNamee RB, Jones EL, Browder IW, et al. NMR spectral analysis of a water-insoluble (1-->3)-beta-D-glucan isolated from Saccharomyces cerevisiae. Carbohydr Res. 1994;258:307–11. doi: 10.1016/0008-6215(94)84098-9. [DOI] [PubMed] [Google Scholar]
- 6.Ross GD. Regulation of the adhesion versus cytotoxic functions of the Mac-1/CR3/alphaMbeta2-integrin glycoprotein. Crit Rev Immunol. 2000;20:197–222. [PubMed] [Google Scholar]
- 7.Zimmerman JW, Lindermuth J, Fish PA, Palace GP, Stevenson TT, DeMong DE. A novel carbohydrate-glycosphingolipid interaction between a beta-(1–3)-glucan immunomodulator, PGG-glucan, and lactosylceramide of human leukocytes. J Biol Chem. 1998;273:22014–20. doi: 10.1074/jbc.273.34.22014. [DOI] [PubMed] [Google Scholar]
- 8.Rice PJ, Kelley JL, Kogan G, Ensley HE, Kalbfleisch JH, Browder IW, et al. Human monocyte scavenger receptors are pattern recognition receptors for (1-->3)-beta-D-glucans. J Leukoc Biol. 2002;72:140–6. [PubMed] [Google Scholar]
- 9.Brown GD, Gordon S. Immune recognition. A new receptor for beta-glucans. Nature. 2001;413:36–7. doi: 10.1038/35092620. [DOI] [PubMed] [Google Scholar]
- 10.Brown GD, Herre J, Williams DL, Willment JA, Marshall AS, Gordon S. Dectin-1 mediates the biological effects of beta-glucans. J Exp Med. 2003;197:1119–24. doi: 10.1084/jem.20021890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gantner BN, Simmons RM, Canavera SJ, Akira S, Underhill DM. Collaborative induction of inflammatory responses by dectin-1 and Toll-like receptor 2. J Exp Med. 2003;197:1107–17. doi: 10.1084/jem.20021787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thornton BP, Vetvicka V, Pitman M, Goldman RC, Ross GD. Analysis of the sugar specificity and molecular location of the beta-glucan-binding lectin site of complement receptor type 3 (CD11b/CD18) J Immunol. 1996;156:1235–46. [PubMed] [Google Scholar]
- 13.Xia Y, Vetvicka V, Yan J, Hanikyrova M, Mayadas T, Ross GD. The beta-glucan-binding lectin site of mouse CR3 (CD11b/CD18) and its function in generating a primed state of the receptor that mediates cytotoxic activation in response to iC3b-opsonized target cells. J Immunol. 1999;162:2281–90. [PubMed] [Google Scholar]
- 14.Yan J, Vetvicka V, Xia Y, Coxon A, Carroll MC, Mayadas TN, et al. Beta-glucan, a “specific” biologic response modifier that uses antibodies to target tumors for cytotoxic recognition by leukocyte complement receptor type 3 (CD11b/CD18) J Immunol. 1999;163:3045–52. [PubMed] [Google Scholar]
- 15.Hong F, Hansen RD, Yan J, Allendorf DJ, Baran JT, Ostroff GR, et al. Beta-glucan functions as an adjuvant for monoclonal antibody immunotherapy by recruiting tumoricidal granulocytes as killer cells. Cancer Res. 2003;63:9023–31. [PubMed] [Google Scholar]
- 16.Allendorf DJ, Yan J, Ross GD, Hansen RD, Baran JT, Subbarao K, et al. C5a-Mediated Leukotriene B4-Amplified Neutrophil Chemotaxis Is Essential in Tumor Immunotherapy Facilitated by Anti-Tumor Monoclonal Antibody and {beta}-Glucan. J Immunol. 2005;174:7050–6. doi: 10.4049/jimmunol.174.11.7050. [DOI] [PubMed] [Google Scholar]
- 17.Li B, Allendorf DJ, Hansen R, Marroquin J, Ding C, Cramer DE, et al. Yeast beta-glucan amplifies phagocyte killing of iC3b-opsonized tumor cells via complement receptor 3-Syk-phosphatidylinositol 3-kinase pathway. J Immunol. 2006;177:1661–9. doi: 10.4049/jimmunol.177.3.1661. [DOI] [PubMed] [Google Scholar]
- 18.Modak S, Koehne G, Vickers A, O’Reilly RJ, Cheung NK. Rituximab therapy of lymphoma is enhanced by orally administered (1-->3),(1-->4)-D-beta-glucan. Leuk Res. 2005;29:679–83. doi: 10.1016/j.leukres.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 19.Salvador C, Li B, Hansen R, Cramer DE, Kong M, Yan J. Yeast-Derived {beta}-Glucan Augments the Therapeutic Efficacy Mediated by Anti-Vascular Endothelial Growth Factor Monoclonal Antibody in Human Carcinoma Xenograft Models. Clin Cancer Res. 2008;14:1239–47. doi: 10.1158/1078-0432.CCR-07-1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhong W, Hansen R, Li B, Cai Y, Salvador C, Moore GD, et al. Effect of yeast-derived beta-glucan in conjunction with bevacizumab for the treatment of human lung adenocarcinoma in subcutaneous and orthotopic xenograft models. J Immunother. 2009;32:703–12. doi: 10.1097/CJI.0b013e3181ad3fcf. [DOI] [PubMed] [Google Scholar]
- 21.Li B, Allendorf DJ, Hansen R, Marroquin J, Cramer DE, Harris CL, et al. Combined yeast {beta}-glucan and antitumor monoclonal antibody therapy requires C5a-mediated neutrophil chemotaxis via regulation of decay-accelerating factor CD55. Cancer Res. 2007;67:7421–30. doi: 10.1158/0008-5472.CAN-07-1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheung NK, Modak S. Oral (1-->3),(1-->4)-beta-D-glucan synergizes with antiganglioside GD2 monoclonal antibody 3F8 in the therapy of neuroblastoma. Clin Cancer Res. 2002;8:1217–23. [PubMed] [Google Scholar]
- 23.Cheung NK, Modak S, Vickers A, Knuckles B. Orally administered beta-glucans enhance anti-tumor effects of monoclonal antibodies. Cancer Immunol Immunother. 2002;51:557–64. doi: 10.1007/s00262-002-0321-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.LeibundGut-Landmann S, Gross O, Robinson MJ, Osorio F, Slack EC, Tsoni SV, et al. Syk- and CARD9-dependent coupling of innate immunity to the induction of T helper cells that produce interleukin 17. Nat Immunol. 2007;8:630–8. doi: 10.1038/ni1460. [DOI] [PubMed] [Google Scholar]
- 25.Leibundgut-Landmann S, Osorio F, Brown GD, Reis e Sousa C. Stimulation of dendritic cells via the dectin-1/Syk pathway allows priming of cytotoxic T-cell responses. Blood. 2008;112:4971–80. doi: 10.1182/blood-2008-05-158469. [DOI] [PubMed] [Google Scholar]
- 26.Osorio F, LeibundGut-Landmann S, Lochner M, Lahl K, Sparwasser T, Eberl G, et al. DC activated via dectin-1 convert Treg into IL-17 producers. Eur J Immunol. 2008;38:3274–81. doi: 10.1002/eji.200838950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martin-Orozco N, Muranski P, Chung Y, Yang XO, Yamazaki T, Lu S, et al. T helper 17 cells promote cytotoxic T cell activation in tumor immunity. Immunity. 2009;31:787–98. doi: 10.1016/j.immuni.2009.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kryczek I, Banerjee M, Cheng P, Vatan L, Szeliga W, Wei S, et al. Phenotype, distribution, generation, and functional and clinical relevance of Th17 cells in the human tumor environments. Blood. 2009;114:1141–9. doi: 10.1182/blood-2009-03-208249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kryczek I, Wei S, Szeliga W, Vatan L, Zou W. Endogenous IL-17 contributes to reduced tumor growth and metastasis. Blood. 2009;114:357–9. doi: 10.1182/blood-2008-09-177360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dillon S, Agrawal S, Banerjee K, Letterio J, Denning TL, Oswald-Richter K, et al. Yeast zymosan, a stimulus for TLR2 and dectin-1, induces regulatory antigen-presenting cells and immunological tolerance. J Clin Invest. 2006;116:916–28. doi: 10.1172/JCI27203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nisini R, Torosantucci A, Romagnoli G, Chiani P, Donati S, Gagliardi MC, et al. {beta}-Glucan of Candida albicans cell wall causes the subversion of human monocyte differentiation into dendritic cells. J Leukoc Biol. 2007 doi: 10.1189/jlb.0307160. [DOI] [PubMed] [Google Scholar]
- 32.Hong F, Yan J, Baran JT, Allendorf DJ, Hansen RD, Ostroff GR, et al. Mechanism by which orally administered beta-1,3-glucans enhance the tumoricidal activity of antitumor monoclonal antibodies in murine tumor models. J Immunol. 2004;173:797–806. doi: 10.4049/jimmunol.173.2.797. [DOI] [PubMed] [Google Scholar]
- 33.Liu K, Idoyaga J, Charalambous A, Fujii S, Bonito A, Mordoh J, et al. Innate NKT lymphocytes confer superior adaptive immunity via tumor-capturing dendritic cells. J Exp Med. 2005;202:1507–16. doi: 10.1084/jem.20050956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ding C, Cai Y, Marroquin J, Ildstad ST, Yan J. Plasmacytoid dendritic cells regulate autoreactive B cell activation via soluble factors and in a cell-to-cell contact manner. J Immunol. 2009;183:7140–9. doi: 10.4049/jimmunol.0901175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ding C, Wang L, Marroquin J, Yan J. Targeting of antigens to B cells augments antigen-specific T-cell responses and breaks immune tolerance to tumor-associated antigen MUC1. Blood. 2008;112:2817–25. doi: 10.1182/blood-2008-05-157396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yan J, Allendorf DJ, Brandley B. Yeast whole glucan particle (WGP) beta-glucan in conjunction with antitumour monoclonal antibodies to treat cancer. Expert Opin Biol Ther. 2005;5:691–702. doi: 10.1517/14712598.5.5.691. [DOI] [PubMed] [Google Scholar]
- 37.Croci DO, Zacarias Fluck MF, Rico MJ, Matar P, Rabinovich GA, Scharovsky OG. Dynamic cross-talk between tumor and immune cells in orchestrating the immunosuppressive network at the tumor microenvironment. Cancer Immunol Immunother. 2007;56:1687–700. doi: 10.1007/s00262-007-0343-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rabinovich GA, Gabrilovich D, Sotomayor EM. Immunosuppressive strategies that are mediated by tumor cells. Annu Rev Immunol. 2007;25:267–96. doi: 10.1146/annurev.immunol.25.022106.141609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hoption Cann SA, van Netten JP, van Netten C. Dr William Coley and tumour regression: a place in history or in the future. Postgrad Med J. 2003;79:672–80. [PMC free article] [PubMed] [Google Scholar]
- 40.Heine H, Ulmer AJ. Recognition of bacterial products by toll-like receptors. Chem Immunol Allergy. 2005;86:99–119. doi: 10.1159/000086654. [DOI] [PubMed] [Google Scholar]
- 41.Liu J, Gunn L, Hansen R, Yan J. Combined yeast-derived beta-glucan with anti-tumor monoclonal antibody for cancer immunotherapy. Exp Mol Pathol. 2009;86:208–14. doi: 10.1016/j.yexmp.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tamayo MEGHC, Bautista JB, Flores ML, Kurman MR, Paul MM, Gargano MA, Patchen ML. A phase Ib/2, dose-escalating, safety, and efficacy study of imprime PGG, cetuximab and irinotecan in patients with advanced colorectal cancer (CRC) J Clin Oncol. 2009;27(suppl; abstr e15062):e15062. Abstract. [Google Scholar]
- 43.Aouadi M, Tesz GJ, Nicoloro SM, Wang M, Chouinard M, Soto E, et al. Orally delivered siRNA targeting macrophage Map4k4 suppresses systemic inflammation. Nature. 2009;458:1180–4. doi: 10.1038/nature07774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karumuthil-Melethil S, Perez N, Li R, Vasu C. Induction of innate immune response through TLR2 and dectin 1 prevents type 1 diabetes. J Immunol. 2008;181:8323–34. doi: 10.4049/jimmunol.181.12.8323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li B, Cramer D, Wagner S, Hansen R, King C, Kakar S, et al. Yeast glucan particles activate murine resident macrophages to secrete proinflammatory cytokines via MyD88- and Syk kinase-dependent pathways. Clin Immunol. 2007;124:170–81. doi: 10.1016/j.clim.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cramer DE, Wagner S, Li B, Liu J, Hansen R, Reca R, et al. Mobilization of hematopoietic progenitor cells by yeast-derived beta-glucan requires activation of matrix metalloproteinase-9. Stem Cells. 2008;26:1231–40. doi: 10.1634/stemcells.2007-0712. [DOI] [PubMed] [Google Scholar]
- 47.Cramer DE, Allendorf DJ, Baran JT, Hansen R, Marroquin J, Li B, et al. {beta}-Glucan enhances complement-mediated hematopoietic recovery after bone marrow injury. Blood. 2006;107:835–40. doi: 10.1182/blood-2005-07-2705. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.