Abstract
Objective
Evaluate a computer-assisted telephone counseling (CATC) decision aid for men considering a Prostate Specific Antigen (PSA) test.
Methods
Eligible men were invited by their primary care providers (PCPs) to participate. Those consenting received an educational booklet followed by CATC. The counselor assessed stage of readiness, reviewed booklet information, corrected knowledge deficits and helped with a values clarification exercise. The materials presented advantages and disadvantages of being screened and did not advocate for testing or for not testing. Outcome measures included changes in stage, decisional conflict, decisional satisfaction, perceived vulnerability and congruence of a PSA testing decision with a pros/cons score. Baseline and final surveys were administered by telephone.
Results
There was an increase in PSA knowledge (p<0.001), and in decisional satisfaction (p<0.001), a decrease in decisional conflict (p<0.001), and a general consistency of those decisions with the man's values. Among those initially who had not made a decision, 83.1% made a decision by final survey with decisions equally for or against screening.
Conclusions
The intervention provides realistic, unbiased and effective decision support for men facing a difficult and confusing decision.
Practice Implications
Our intervention could potentially replace a discussion of PSA testing with the PCP for most men.
Keywords: computer-assisted telephone counseling, interactive decision aid, PSA screening
1. Introduction
Considerable controversy exists about the effectiveness of prostate specific antigen (PSA) screening in reducing mortality from prostate cancer (PCa), although there is good evidence that the PSA test can detect early stage prostate cancer. Moreover, there is evidence that screening is associated with important harms: frequent false-positive biopsies, anxiety, overtreatment of non-aggressive cancers. [1]. Most organizations recommend that men should be given the opportunity to discuss the benefits and risks of PSA testing with their primary care providers (PCPs) before making a screening decision [2].
Two recent reports of randomized trials of PSA screening have done little to resolve the screening controversy. One study showed no mortality benefit. The other identified a small impact of PSA testing on PCa mortality but was associated with considerable human and financial cost due to overtreatment [3, 4]. The controversy over whether PSA testing can significantly reduce PCa-specific mortality has resulted in some PCPs who strongly recommend PSA testing, some who strongly recommend against, and few who inform men about the pros and cons and share in the decision-making process. Men may also feel pressure from family, friends, public figures and the media, most of whom urge PSA testing. Given this confusing situation, informed decisions about whether one should or should not get a PSA test have never been more needed.
To make an informed decision, the US Preventive Services Task Force suggests that one should understand the risk or seriousness of the disease and the preventive service offered, one should understand its risks, benefits, alternatives, and uncertainties and one should weigh his values regarding potential harms and benefits before engaging in decision-making. Decision-making may be shared with one's provider and sharing may range from no sharing at all to ceding the decision making to the PCP [5].
In general, decision aids help patients make informed decisions about a number of preventive measures and treatments. Several aids have been developed specifically to address PSA testing [6-13]. O'Connor proposes that a good decision aid should: 1) improve knowledge of the problem, options, and outcomes, 2) create realistic expectations of outcomes, 3) clarify personal values for outcomes 4) promote congruence between values and choice, 5) reduce decisional conflict, 6) promote implementation of choices and 7) improve satisfaction with decision making [11]. These standards seem to us and others [14, 15] to apply to decision-making around cancer control issues in general and PSA screening, in particular.
Evans et al. [16] reviewed eight PCa screening decision aids and concluded that most aids increase knowledge and help subjects feel more confident about their decision. Several reviews confirm that PCa screening decision aids generally increase patient knowledge, decrease decisional conflict, and/or increase greater involvement in decision-making [17, 18]. A Cochrane review of decision aids concluded that PCa screening decision aids also appear to decrease interest in PSA testing [17]. Few studies of PCa screening decision aids have included measures of decision congruence with the patient's preferences and values. Most aids do not promote shared decision-making or define a role for the PCP. Two studies that do address these issues are: a) a randomized trial of a web-based decision aid compared to publicly available websites that showed better congruence of men's decisions and their values after reviewing the web-based aid [19] and b) a video decision aid that showed men who had decided not to be screened were less likely to discuss their decision with their PCP compared to men who had decided otherwise [20].
Telephone counseling has been successful in many health promotion efforts focused on moving individuals to a desired health behavior such as having regular screening mammograms. But, to our knowledge, it has not focused on the outcome being an informed decision, rather than a specific desirable behavior [21-29]. Decision making about PCa screening is complex because the value of PCa screening is unproven. A PCa screening decision aid should therefore not promote screening but rather promote informed decision making that is congruent with a man's values and understanding, regardless of whether the decision is for or against screening. A decision aid may also serve to complement discussion with one's PCP, although few engage in balanced discussions and most do not discuss the negative aspects of PSA testing [30].
The purpose of the pilot study reported here was twofold: 1) to evaluate the effectiveness of computer-assisted telephone counseling (CATC) as a decision aid for men considering PSA testing and 2) to present a testable surrogate for discussion and decision sharing with one's PCP. The more common model of informed decision making includes a decision aid (print, video, etc.) with no or limited live interaction between decision aid and subject, sometimes followed by discussion and/or shared decision making between patient and PCP. Our intervention is distinguished from other decision aids by the use of a CATC system and a counselor who played several roles: educator, facilitator of values clarification, and motivational interviewer. Our study is also distinguished from many other studies of informed decision making by the inclusion of measures of stage of readiness and stage change, perceived vulnerability, decisional conflict, decisional satisfaction, as well as pros and cons scores to quantify values, and the difference between pros and cons scores to quantify the consistency of values with the PSA decision made.
2. Methods
2.1. Study sample and selection criteria
Three large primary care medicine practices in Worcester MA participated in the study. Eligibility criteria included: being male, ability to speak English, age 50-70 years (45-70 for African-Americans), no history of PCa and no PSA test in the last 12 months. Providers reviewed lists of their patients who met these criteria and eliminated those they thought were not study candidates (life expectancy of ≤ 5 years, dementia). The University of Massachusetts Medical School Institutional Review Board approved the study that was conducted in 2007-8.
2.2 Intervention overview
Eligible men from selected primary care practices who were approved for study by their PCP were invited by a letter signed by their PCP recommending participation in the study. The letter stated that the recipient had an opportunity to join a study to learn about PCa and a test for PCa, that study personnel would be calling to enroll him and that, if he enrolled, he would receive an informative booklet and be referred to a counseling service to discuss the booklet. Within 1-2 weeks, the research assistant made up to 8 attempts to reach each subject leaving up to 2 voice messages. When an eligible man was reached, consent to be in the study was obtained, the baseline survey administered, an appointment made for the telephone counselor call, and the booklet sent. 1-2 weeks after the booklet was sent, the telephone counselor called and followed the CATC protocol that included assessment of stage of readiness to make a decision about whether or not to be tested, review of the information in the booklet, correction of any knowledge deficits and assistance in a values clarification exercise. Congruence of stated values with the testing decision was assessed at the end of the call. Men whose overall values contradicted their screening decision received additional counseling. A final telephone survey was administered 4-8 weeks following the counseling call.
2.3 Booklet development
The booklet was patterned after the PROCASE booklet of Partin et al. [6, 31] who had included concepts that patients, urologists and oncologists consider key to understanding PCa and the PSA test. With the help of a low literacy consultant, the booklet was revised to accommodate low literacy participants at a 5th grade reading level. The revised booklet ultimately included findings from focus groups and key informant interviews with African-American and non African-American and low-literate men. Low literate men were identified by their PCP and confirmed by their answers to several literacy questions (see section 2.5). The same qualitative research consultant conducted the focus groups, telephone interviews, and in-person interviews. When asked to evaluate the fairness of the booklet, men reported that the booklet seemed well-balanced and unbiased regarding PSA testing options. See Table 1 for methodology of booklet development.
TABLE 1. Methodology for Booklet Development.
| Setting | Participants | Overall Task | Specific Task | Facilitator Role |
|---|---|---|---|---|
| 2 Focus Groups | AA* men group (n=5) | Review overheads of revised PROCASE booklet | React to each page, title, text, illustrations, formatting and overall reaction | Respond to questions and objections; seek suggestions for revision |
| Non-AA men group (n=9) | ||||
| Individual Telephone Interviews | Focus group participants: AA men (n=2) Non-AA men (n=3) | Review booklet, now revised again after above focus group input | Review each page, added material from focus group suggestions | Seek feedback on revision, seek additional changes to be made |
| Non-focus group participants: AA men (n=2) Non-AA men (n=2) | ||||
| Individual face-to-face meetings at UMass | Low literate AA men (n=2) Low literate Non-AA men (n=2) |
Review revised PROCASE booklet | Review for need for clarification of concepts | Assist men in reading booklet; 2 men wanted the facilitator to read the pages to them. Assess need to revise for clarification. |
AA refers to African-American
2.4 Counselor training, counselor protocol and computer support
The counselor had a master's degree (MPH) and had experience interviewing and counseling participants in prior studies. The training protocol involved practice in the use of the CATC system, education about the basics of PCa and PSA testing controversy and motivational interviewing techniques including the use of open-ended questions, reflective listening and asking permission to give information. Training was conducted by the study oncologist, psychologist and project director, included role playing lasted about 20 hours. Random calls were monitored for quality control [29].
The counseling call protocol and the design of the supporting computer software were adapted from our previously developed computer-assisted telephone counseling (CATC) systems for breast and colon cancer screening [26-29, 32]. The CATC system directed the telephone counselor to screens displaying messages appropriately tailored to the subject's level of interest and knowledge and enabled the counselor to easily access information required to address patient questions from menus linked to scripted answers to frequently asked questions. The protocol directed the counselor to identify a man's stage of readiness to make a decision about PSA testing at several points during the call, based on the stage classification in the Precaution Adoption Process Model (PAPM) [33, 34]. Table 2 shows how the counselor introduced the purpose of the call. Table 3 shows a typical exchange between a Stage 3 (Undecided) participant and the counselor.
TABLE 2. Counselor Presentation of Rationale for Booklet and Call.
| We will be talking about testing for prostate cancer today. Page 3 of your booklet explains why your doctor wants you to talk about prostate cancer with me today. |
| Getting tested for prostate cancer may not be a good thing for everyone. |
| In fact expert doctors do not agree on routine testing for prostate |
| Some doctors say all men should get tested. |
| Others say that no men should be tested because they believe that many more men would be harmed by testing than would be helped. |
| Your doctor wants to be sure you understand all the reasons for and against getting tested and come to a decision that fits with your personal values. |
| Your doctor believes it would be OK for you to get tested, but also fine if you decide against testing, as long as you are comfortable with your decision. |
| Do you have any questions about why your doctor wants you to talk with me today? |
TABLE 3. Typical Dialogue between Counselor and Stage 3 (Undecided) Man.
| Counselor: So you know about the PSA screening blood test. Have you made a decision about whether to get the test or not? |
| Participant: I've been thinking a lot about it. But, no, I haven't made a decision. I really can't make up my mind. It seems awful confusing. I think of reasons to get it and reasons not to get it. |
| Counselor: Well, you're not alone. It's hard for many men to make a decision about testing. There are good reasons FOR getting tested and there are good reasons AGAINST getting tested. |
| Participant: I want to be sure I choose the right answer. |
| Counselor: There is really no right or wrong answer. Each man should look at his personal reasons for being tested or not being tested and weigh them. Your values are most important in choosing the right decision for you. |
| Participant: You mean the facts aren't enough. |
| Counselor: Right. The facts alone are not enough. By looking at the reasons you have for and against getting tested, we may be able to help you make a decision. If you've gotten any of the facts wrong, I can help straighten that out. That way your decision will be based on the facts and also on your personal values. |
| Participant: OK. |
| Counselor: [Reviews participant's reasons for and against] Is there any more information that would help you make a decision about getting tested? |
| Participant: No. |
| Counselor: OK. [Moves to pros/cons value clarification exercise] Let's look again at your reasons for and against testing, but this time let's look carefully at how much each reason means to you. By weighing how much a reason means to you, you may see what decision best fits you. |
In addition to addressing knowledge deficits, the counselor assisted men in a values clarification exercise. In the values clarification exercise, a man was asked to rate the importance of reasons favoring PSA testing (pros) and reasons against screening (cons). The CATC system calculated the difference between the total pros and cons scores, yielding a positive value if pros scored higher than cons and a negative value if cons scored higher. If the pros/cons score conflicted with a man's testing decision (e.g., a negative score but a decision to get tested), the counselors employed motivational interviewing principles [35-37] to assist him in exploring and resolving the conflict.
2.5 Data collection
The surveys: The baseline survey included items on socio-demographics, family history of PCa and literacy skills. Both the baseline and final surveys included items on knowledge and beliefs about PCa and PSA testing, stage of readiness to make a decision about PSA testing, perceived risk, questions about decisional conflict, decisional satisfaction and perceived vulnerability. The surveys did not include pros or cons about PSA screening or about the controversy regarding PSA's role in reducing PCa mortality. The baseline survey estimated literacy with 2 items: highest education level and interest in reading (like to read a lot; like to read short things; don't like to read much; or have trouble reading). Men were offered a gift card as an incentive for answering the surveys.
2.6 Measures
Outcome measures: See Table 4. Knowledge, perceived vulnerability, decisional conflict, decisional satisfaction and the subject's stages of readiness were measured on the baseline survey and on the final survey. Staging information was also collected during the counseling call. Perceived vulnerability items were included because the literature has reported a general relationship of perceived vulnerability and screening [40]. The Values Clarification score was obtained at the end of the counseling call. Each man was asked to weigh the importance of each of five core pro reasons and each of five core con reasons by circling asterisks which were placed next to each item in the booklet. There were six possible choices from ‘no asterisk circled’ (of no importance to the man) to ‘five asterisks circled’ (extremely important). Each star counted 1 point. A pro reason got a plus score and a con reason a minus score. Men could add and score personal pros and cons, which were then collapsed into five additional pro and con categories. A man's final score indicated whether he was leaning against screening (negative number) or towards screening (positive number) and with what strength.
TABLE 4. Outcome Measures.
| Measure | Number of items | Score Range | Scoring | Validated | Possible answers |
|---|---|---|---|---|---|
| Knowledge | 10 | 0-10 | Correct answers =1 point | Radosevich [38] | True |
| False | |||||
| Don't Know | |||||
| Perceived Vulnerability | 2 | 0-4 | 0= not at all | Clemow [39] | Not all concerned |
| 1= moderately | Moderately | ||||
| 2=very | Very | ||||
| Decisional Conflict | 10 | 10-30 | 1=yes | O'Connor [[11, 12, 41, 42]. | Yes |
| 2=unsure | No | ||||
| 3=no | Unsure | ||||
| Decisional satisfaction | 6 | 6-18 | 1=disagree | Holmes-Rover [43,44] | Disagree |
| 2=neither | Neither | ||||
| 3=agree | Agree | ||||
| Values Clarification | 10 | -50 to +50 | 0= no importance 1 point for each star circled. A negative number given for reasons against and a positive number for reasons being screened | O'Connor [11, 12, 41, 42] | No star - no importance 1 to 5 stars – lowest to highest importance |
| Partin [6,31] | |||||
| Rakowski [45] | |||||
| Staging | 5 | 1-5 | 1=Unaware | Weinstein [33,34] |
|
| 2=Unengaged | |||||
| 3=Thinking About | |||||
| 4=Decided No | |||||
| 5=Decided Yes | |||||
2.7 Statistical Analysis
All analyses were performed using Stata SE v.10.1 [46]. Characteristics of the sample were summarized using frequency tabulations for categorical variables and means and standard deviations for continuous variables. Nonparametric versions of the chi-square test, t-test and ANOVA were used to account for small cell frequencies and non-normal distributions of continuous data. Comparisons of continuous variables with 2 groups were analyzed using the sign test and Kruskal-Wallis test for data with more than 2 groups. Comparisons of categorical variables with cell counts >5 were analyzed using the chi-square test. A p value of <0.05 was considered statistically significant. Except where noted, p-values were calculated using the chi-square test.
3. Results
3.1 Patient population recruitment and participation
Study PCPs approved 310 men. Of these, 18 (5.8%) were found to be ineligible when contacted, 57 (18.4%) had disconnected phones, 79 (25.5%) were unreachable, and 41(13.2%) refused study participation, leaving 115 (37.1%) men who completed the baseline survey, seven of these had low literacy. 101 of the men who completed the baseline survey completed the counseling call, representing 43.0% of the 235 men who were eligible and had a current phone number. Table 5 shows selected characteristics of those 101 men. Of the 101 men who completed the baseline survey and counseling, 92 completed the final survey. Only 17.1% of African-American men could be contacted and agreed to counseling compared to 38.4% of Caucasian men (p=.001). Fewer African-American men had current telephone numbers than Caucasian men (p=.008). Of the 41 refusals, 11 responded: 5 were “not interested,” 4 had “no time”, 1 wanted “to talk with my PCP first”, and 1 didn't understand the prompt. Ages and prior PSA testing of those completing the baseline survey and those unreachable or refusing were not statistically significantly different (p>.05).
TABLE 5. Characteristics of Counseled Men (N=101).
| Characteristic | N (%) |
|---|---|
| Age | |
| 40-49 | 6 (5.9) |
| 50-64 | 87 (86.1) |
| ≥65 | 8 (7.9) |
| Race | |
| African American | 12 (11.9) |
| White | 84 (83.2) |
| Other | 5 (5.1) |
| Education | |
| < High school | 4 (4.0) |
| Grad HS or tech | 17 (16.8) |
| Some college | 26 (25.7) |
| College grad | 29 (28.7) |
| Post grad | 25 (24.8) |
| Household financial situation | |
| Very comfortable with money for extras | 49 (48.5) |
| Can make ends meet without cutting back | 28 (27.7) |
| Have cut back just to make ends meet | 14 (13.9) |
| Very hard to get by | 6 (5.9) |
| Refused | 4 (4.0) |
| Married or living with partner | |
| No | 12 (12.0) |
| Yes | 87 (87.0) |
| Refused | 1 (1.0) |
| Goes for checkups when well | 82 (81.2) |
| Family history | 8 (7.9) |
| Low literacy | 7 (6.9) |
| Stage at baseline survey | |
| 1: Unaware | 22 (21.8) |
| 2: Unengaged | 28 (27.0) |
| 3: Undecided | 15 (14.9) |
| 4&5: Decided | 36 (35.6) |
| 4: Decided No | 4 (4.0) |
| 5: Decided Yes | 32 (31.7) |
The average counseling call took 20 minutes. All men received some basic motivational interviewing components: assessing stage, giving feedback on staging/intentions, eliciting pros/cons regarding screening, assessing self-efficacy (if Decided Yes). Three men had made decisions that were non-congruent with their pros/cons scores. When the discrepancy was noted, they changed their decision to match their pros/cons values (1 Decided No; 2 Decided Yes), adding about 5 minutes to the call.
3.2 Changes in stage of readiness
Table 6 shows the distribution of stages of readiness of the 92 counseled men who completed both surveys at 1) baseline survey, 2) beginning of the call, 3) end of the call, and 4) final survey. Initially 47.8% of men were unaware of or unengaged in PSA testing, but after receiving the booklet, only 7 (7.6%) were still unengaged or unaware. At the baseline survey, only 35.9% of men had made a decision about PSA testing: 3.3% decided not to be tested and 32.6% decided to be tested. After receiving the booklet, 71.7% had made a decision about the testing issue. From baseline to final surveys, men making a PSA testing decision increased from 35.9% (n=33) to 85.9% (n=79) (p<0.001).
TABLE 6. Stage of Adoption from Baseline Through Final Survey.
|
Baseline Survey n (%) |
Before Counseling n (%) |
After Counseling* n (%) |
Final Survey n (%) |
|
|---|---|---|---|---|
| Unaware | 20 (21.7) | 1 (1.1) | 0 | 0 |
| Unengaged | 24 (26.1) | 6 (6.5) | 0 | 0 |
| Undecided | 15 (16.3) | 19 (20.1) | 5 (5.5) | 13 (14.1) |
| Decided | 33 (35.9) | 66 (71.7) | 86 (94.5) | 79 (85.9) |
| Decided No | 3 (3.3) | 20 (21.7) | 28 (30.8) | 30 (32.6) |
| Decided Yes | 30 (32.6) | 46 (50.0) | 58 (63.7) | 49 (53.3) |
N=91 due to missing data
Table 7 shows the stage at final survey for men in each stage on the baseline survey. The initial Decided No group was very small and remained Decided No. Most of the initial Decided Yes group (22/27, 81.5%) also did not change stage. Of the 59 men who initially had not made a testing decision (Unaware, Unengaged, Undecided), 49 (83.1%) made a decision by final survey. Nearly equal numbers of these 49 men, Decided Yes (27/49, 55.1%, 95% CI: 40.2%, 69.3%) and Decided No (22/49, 44.9%, 95% CI: 30.7%, 59.8%.
TABLE 7. Stage of Adoption at Baseline and Final Surveys (N=92).
| Stage at Baseline Survey | Stage at Final Survey | Total n (%) |
|||
|---|---|---|---|---|---|
| Undecided n (%) |
Decided (Total) n (%) |
Decided No n (% of decided) |
Decided Yes n (% of decided) |
||
| Unaware | 4 (20.0) | 16 (80.0) | 8 (50) | 8 (50) | 20 (100) |
| Unengaged | 5 (20.8) | 19 (79.2) | 9 (47.4) | 10 (52.6) | 24 (100) |
| Undecided | 1 (6.7) | 14 (93.3) | 5 (35.7) | 9 (64.3) | 15 (100) |
| Decided (Total) | 3 (9.1) | 30 (90.9) | 8 (26.7) | 22 (73.3) | 33 (100) |
| Decided No | 0 | 3 (100) | 3 (100) | 0 | 3 (100) |
| Decided Yes | 3 (10.0) | 27 (90.0) | 5 (18.5) | 22 (81.5) | 30 (100) |
3.3 Changes in knowledge, perceived vulnerability, decisional conflict and decisional satisfaction
Table 8 shows changes in knowledge, perceived vulnerability, decisional conflict and decisional satisfaction. All changed significantly except for perceived vulnerability, even though the intervention included information about PCa risk as it related to age, family history and race. Men showed significant improvement on several knowledge items: the most common cause of problems with urination; most men with PCa die from something else; the main adverse effects of PCa treatment (urine loss; sexual dysfunction).
TABLE 8. Mean Score at Baseline and Final Surveys for Knowledge, Perceived Vulnerability, Decisional Conflict, and Decisional Satisfaction (N=92).
| Score | Completed baseline and final surveys | Score Range | Baseline Mean | Final Mean | P -value for change from baseline survey*** |
|---|---|---|---|---|---|
| Knowledge | N=92 | 0-10 | 6.97 | 9.01 | <0.001 |
| Perceived vulnerability | N=76* | 0-4 | 1.18 | 1.07 | 0.073 |
| Decisional conflict | N=72** | 10-30 | 18.92 | 11.36 | <0.001 |
| Decisional satisfaction | N=72** | 6-18 | 15.56 | 17.66 | <0.001 |
16 men in Stage 1 (Unaware of PSA testing) did not have an opinion at pre-test
20 men in Stage 1(Unaware of PSA testing) had no knowledge about the PSA test and could not make any decision
p-values are from the sign test
3.4 Pros and cons score and stage correlations
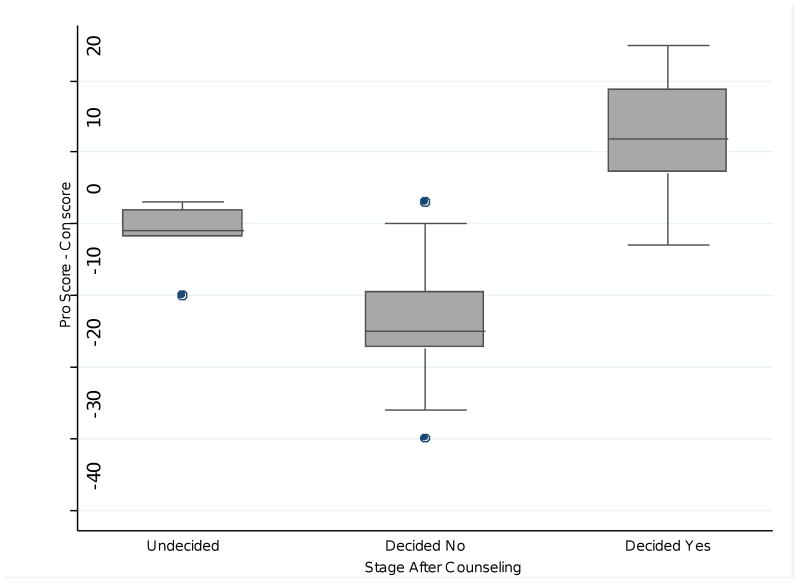
Regarding distribution of scores, 25% of men had strong pros scores compared to 10.9% of men with strong cons score and 37% of men had moderate pros scores compared to 34% of men with moderate cons scores. Figure 1 shows the relationship between the summed pros-cons scores and the participants' stages at the end of the counseling call. The median scores are statistically significantly different (Kruskal Wallis p = 0.0001) and consistent with the related stages: Decided Yes is associated with the highest positive score, Decided No with the lowest negative score, and Undecided scores cluster around a pro/con difference of zero. Thus the men's decisions, represented by the stages, are mostly consistent with their values, as measured by the pro/con score difference.
Figure 1. Box Plot of Pro Sum Score-Con Sum Score by Stage at End of Counseling Call.
Each box represents the interquartile range (middle 50% of values), the line in the box the median, the vertical lines the extent of the highest and lowest quartiles, and the dots represent values that lie more than 1.5 times the interquartile range from the median.
4. Discussion and conclusion
4.1 Discussion
Overall, the intervention was well received by the men. Almost all considered the booklet and the counseling improved their knowledge of PCa and PSA. We believe the booklet and counseling presented a balanced picture, neither for nor against testing. This contention is supported by two facts: a) men in two focus groups reviewed the booklet and informed us that the booklet was not biased but balanced regarding PSA testing and b) men who had not made a decision prior to the intervention were equally apt to make a pro or a con testing decision following the intervention.
Our intervention was highly successful in helping men make an informed decision by the end of counseling. At the baseline survey, only 36% of the group had made a decision. But by the final survey, 86% had made a decision. Although more men ultimately decided in favor of screening (n=49, 53%) than decided against (n=30, 33%), this finding is primarily due the large number of men whose initial stage was Decided Yes (n=30), most of whom did not change stage. For men in all other stages at baseline (Unaware, Unengaged, Undecided), nearly equal numbers moved to either Decided No or Decided Yes by the final survey. Perhaps more importantly, the intervention helped almost all of the men either make or confirm a decision that was congruent with their values.
Staging men at different points in the intervention was an important aspect of the study and allow us to judge the value of various intervention components. For example, as shown in Table 6, the booklet alone moved almost all men from Unaware and Unengaged to higher stages. Staging also permitted us to key the counseling script to the individual participant's stage. Table 3 shows a typical counseling sequence for a Stage 3 (Undecided) participant.
We believe the addition of a telephone counselor to the mailed booklet was critical. Although in a randomized study, the PROCASE booklet alone demonstrated an improvement in knowledge and clarity about preference [6, 31], only 50% of men mailed the PROCASE booklet looked at it [47-49]. In Partin's qualitative work, men said they would not complete the self-administered values clarification exercise, considered an essential component of decision aids [50]. We hypothesized that the addition of a follow-up call from a counselor would be an encouragement for men to read the booklet and complete the exercise with the help of the counselor. In our study, 99% of the men read the booklet and every counseled man completed the exercise. The interaction with the counselor also provided an opportunity to correct any misunderstandings in real time and permitted low-literacy men to have an “interpreter” of the booklet's information. While the counselor in this pilot study was master's prepared, typical requirements for a counselor would be bachelor's prepared, familiarity and ease with computers, informal experience with counseling and 40 hours of training using the CATC system.
An informed decision should rest on adequate knowledge. In this study, at baseline, only 43% of men had a knowledge score >= 80%, suggesting insufficient knowledge to make an informed decision. By the final survey, 92% of men had achieved a knowledge score >=80% score, a reasonable knowledge base for informed decision-making. Results from the final survey showed a significant and substantial increase not only in knowledge, but also a significant decrease in decisional conflict, a significant increase in decisional satisfaction, a consistency of decisions with values and the movement of the majority of initially undecided men to a decision.
Generalizability of our study findings is limited by the composition of the study population and selection bias. Most participants were white, middle class and well-educated. Only 7% of the men were low-literate and only 12% were non-Caucasian despite our efforts to promote participation by a diverse population that included a personalized invitational letter with an enthusiastic endorsement of the study by each man's PCP, print materials designed for a 5th grade reading level or less, and multiple attempts to reach each subject. Also, it is likely that the composition of the study population was biased towards men with an interest in learning more about PCa and PSA testing. Most men who actively or passively refused to participate did not share their reasons. Other study limitations include the absence of a control group and possible impact of the surveys on participation and outcome.
A disturbing finding was the low number of African-Americans who participated. One reason was that 30% did not have a working phone number. Another 30% had a working phone number but did not answer or return any of the counselor's eight calls. This may reflect distrust of the medical system, a firm PSA testing decision already made and/or the men may have felt no need to review the issues or their motivations. More vigorous attempts to engage this population could involve alternate recruitment strategies (e.g. referral at the time of a clinic visit) and community outreach programs (e.g. through community or church groups).
4.2 Conclusions
Our pilot study was successful in significantly improving knowledge, decreasing decisional conflict, increasing decisional satisfaction and increasing the number of men making a decision about PSA testing. We believe that enough men were motivated to receive telephone counseling to justify further study of this method. A print decision aid alone may be adequate for some men (e.g., many of those decided yes after reading the booklet). Measuring key outcomes after men read the booklet and before counseling could confirm this observation. Values clarification may not be required for men to achieve similar outcomes given that very few men changed stage after the values clarification exercise. Because we did not measure decisional conflict and decisional satisfaction before and after the values clarification exercise, we cannot judge the impact of the exercise on these measures. We believe the intervention, combining print material with a CATC system provides realistic and effective decision support for men facing a difficult decision and could potentially substitute for discussion of PSA testing with their PCPs. However, in the absence of a controlled trial, this is speculation.
4.3 Practice implications
Adequately informing men about the uncertainties and tradeoffs involved in PSA testing so they can make an informed and value-concordant decision takes time to do well. With most practitioners working under pressure to see more patients in less time, helping patients understand complex health issues has become a luxury few PCPs can afford [51]. Less than 16% of study subjects had had a discussion about PSA testing with their PCP at their last clinic visit, a finding consistent with a recent report of shared decision making [30].
The current crisis in the PCP workforce has serious detrimental effects on patient education and counseling [52]. Given patients average face-to-face time with PCPs of 15 minutes, it seems unlikely that men could receive an adequate education about PSA testing during a routine visit [53]. Even if PCPs had adequate time and compensation, it is unclear whether they have the skills to counsel men to make an informed decision. Our intervention could potentially replace a men's discussion of PSA testing with their PCP. The small minority of men who remain undecided after receiving the intervention could request discussion and shared decision making with their PCP.
Future research should investigate reasons for refusal and for the difficulty in reaching patients by telephone. A randomized controlled trial comparing other decision aids to our intervention would clarify its relative efficacy and cost-efficiency.
Acknowledgments
This study was supported by NIH grant R21 CA 108666. The authors thank Amin Vidal for development of the CATC system.
Footnotes
Certification: I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.US Preventive Services Task Force. Prostate Cancer Screening Recommendations. [3/4/2009]; http://www.ahrq.gov/clinic/uspstf/uspsprca.htm.
- 2.Woolf SH, Krist AH. Shared decision making for prostate cancer screening: Do patients or clinicians have a choice? Archives of Internal Medicine. 2009;169:1557–1559. doi: 10.1001/archinternmed.2009.291. [DOI] [PubMed] [Google Scholar]
- 3.Andriole GL, Grubb RL, 3rd, Buys SS, Chia D, Church TR, Fouad MN, Gelmann EP, Kvale PA, Reding DJ, Weissfeld JL, Yokochi LA, Crawford ED, O'Brien B, Clapp JD, Rathmell JM, Riley TL, Hayes RB, Kramer BS, Izmirlian G, Miller AB, Pinsky PF, Prorok PC, Gohagan JK, Berg CD, PLCO Project Team Mortality results from a randomized prostate cancer screening trial. New England Journal of Medicine. 2009;360(13):1310–1319. doi: 10.1056/NEJMoa0810696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schroder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, Kwiatkowski M, Lujan M, Lilja H, Zappa M, Denis LJ, Recker F, Berenguer A, Maattanen L, Bangma CH, Aus G, Villers A, Rebillard X, van der Kwast T, Blijenberg BG, Moss SM, de Koning HJ, Auvinen A, ERSPC Investigators Screening and prostate-cancer mortality in a randomized European study. New England Journal of Medicine. 2009;360(13):1320–1328. doi: 10.1056/NEJMoa0810084. [DOI] [PubMed] [Google Scholar]
- 5.Sheridan SL, Harris RP, Woolf SH, Shared Decisionmaking Workgroup of the United States Preventive Services Task Force Shared Decisionmaking About Screening and Chemoprevention: A Suggested Approach from the U.S. Preventive Services Task Force. (Background Article) [01/16/2009]; http://www.ahrq.gov/clinic/3rduspstf/shared/sharedba2.htm.
- 6.Partin MR, Nelson D, Radosevich DM, Nugent S, Flood AB, Dillon N, Holtzman J, Haas M, Wilt TJ. Randomized trial examining the effect of two prostate cancer screening educational interventions on patient knowledge, preferences, and behaviors. Journal of General Internal Medicine. 2004;19:835–842. doi: 10.1111/j.1525-1497.2004.30047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frosch DL, Kaplan RM, Felitti V. A randomized controlled trial comparing internet and video to facilitate patient education for men considering the prostate specific antigen test. Journal of General Internal Medicine. 2003;18:781–787. doi: 10.1046/j.1525-1497.2003.20911.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frosch DL, Kaplan RM, Felitti V. Evaluation of two methods to facilitate shared decision making for men considering the prostate-specific antigen test. Journal of General Internal Medicine. 2001;16:391–398. doi: 10.1046/j.1525-1497.2001.016006391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taylor KL, Davis JL, 3rd, Turner RO, Johnson L, Schwartz MD, Kerner JF, Leak C. Educating African American men about the prostate cancer-screening dilemma: A randomized intervention. Cancer Epidemiology, Biomarkers and Prevention. 2006;15:2179–2188. doi: 10.1158/1055-9965.EPI-05-0417. [DOI] [PubMed] [Google Scholar]
- 10.Myers RE, Daskalakis C, Cocroft J, Kunkel EJ, Delmoor E, Liberatore M, Nydick RL, Brown ER, Gay RN, Powell T, Powell RL. Preparing African-American men in community primary care practices to decide whether or not to have prostate cancer screening. Journal of the National Medical Association. 2005;97:1143–1154. [PMC free article] [PubMed] [Google Scholar]
- 11.O'Connor AM, Fiset V, DeGrasse C, Graham ID, Evans W, Stacey D, Laupacis A, Tugwell P. Decision aids for patients considering options affecting cancer outcomes: evidence for efficacy and policy implications. Journal of the National Cancer Institute Monographs. 1999;25:67–80. doi: 10.1093/oxfordjournals.jncimonographs.a024212. [DOI] [PubMed] [Google Scholar]
- 12.O'Connor AM, Bennett C, Stacey D, Barry MJ, Col NF, Eden KB, Entwistle V, Fiset V, Holmes-Rovner M, Khangura S, Llewellyn-Thomas H, Rovner DR. Do patient decision aids meet effectiveness criteria of the international patient decision aid standards collaboration? A systematic review and meta-analysis. Medical Decision Making. 2007;27:554–574. doi: 10.1177/0272989X07307319. [DOI] [PubMed] [Google Scholar]
- 13.Gattellari M, Ward JE. Does evidence-based information about screening for prostate cancer enhance consumer decision-making? A randomized controlled-trial. Journal of Medical Screening. 2003;10:27–39. doi: 10.1258/096914103321610789. [DOI] [PubMed] [Google Scholar]
- 14.Briss P, Rimer B, Reilley B, Coates RC, Lee NC, Mullen P, Corso P, Hutchinson AB, Hiatt R, Kerner J, George P, White C, Gandhi N, Saraiya M, Breslow R, Isham G, Teutsch SM, Hinman AR, Lawrence R. Task Force on Community Preventive Services. Promoting informed decision making about cancer screening: What can communities and health care systems accomplish? American Journal of Preventive Medicine. 2004;26:67–80. doi: 10.1016/j.amepre.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 15.Mullen PD, Allen JD, Glanz K, Fernandez ME, Bowen DJ, Pruitt SL, Glenn BA, Pignone M. Measures used in studies of informed decision making about cancer screening: A systematic review. Annals of Behavioral Medicine. 2006;32:188–201. doi: 10.1207/s15324796abm3203_4. [DOI] [PubMed] [Google Scholar]
- 16.Evans R, Edwards A, Brett J, Bradburn M, Watson E, Austoker J, Elwyn G. Reduction in uptake of PSA tests following decision aids: Systematic review of current aids and their evaluations. Patient Education & Counseling. 2005;58:13–26. doi: 10.1016/j.pec.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 17.O'Connor AM, Bennett CL, Stacey D, Barry M, Col NF, Eden KB, Entwistle VA, Fiset V, Holmes-Rovner M, Khangura S, Llewellyn-Thomas H, Rovner D. Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews. 2009;1 doi: 10.1002/14651858.CD001431.pub2. [DOI] [PubMed] [Google Scholar]
- 18.Volk RJ, Hawley ST, Kneuper S, Holden EW, Stroud LA, Cooper CP, Berkowitz JM, Scholl LE, Saraykar SS, Pavlik VN. Trials of Decision Aids for Prostate Cancer Screening A Systematic Review. American Journal of Preventive Medicine. 2007;33:428–434. doi: 10.1016/j.amepre.2007.07.030. [DOI] [PubMed] [Google Scholar]
- 19.Frosch DL, Bhatnagar V, Tally S, Hamori CJ, Kaplan RM. Internet patient decision support: A randomized controlled trial comparing alternative approaches for men considering prostate cancer screening. Archives of Internal Medicine. 2008;168:363–369. doi: 10.1001/archinternmed.2007.111. [DOI] [PubMed] [Google Scholar]
- 20.Frosch DL, Legare F, Mangione CM. Using decision aids in community-based primary care: A theory-driven evaluation with ethnically diverse patients. Patient Education & Counseling. 2008;73:490–496. doi: 10.1016/j.pec.2008.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lerman C, Hanjani P, Caputo C, Miller S, Delmoor E, Nolte S, Engstrom P. Telephone counseling improves adherence to colposcopy among lower income women. Journal of Clinical Oncology. 1992;10:330–333. doi: 10.1200/JCO.1992.10.2.330. [DOI] [PubMed] [Google Scholar]
- 22.Miller SM, Siejak KK, Schroeder CM, Lerman C, Hernandez E, Helm CW. Enhancing adherence following abnormal Pap smears among lower income minority women: a preventive telephone counseling strategy. Journal of the National Cancer Institute. 1997;89:703–708. doi: 10.1093/jnci/89.10.703. [DOI] [PubMed] [Google Scholar]
- 23.Britt J, Curry SJ, McBride C, Grothaus L, Louie D. Implementation and acceptance of outreach telephone counseling for smoking cessation with nonvolunteer smokers. Health Education Quarterly. 1994;21:55–68. doi: 10.1177/109019819402100107. [DOI] [PubMed] [Google Scholar]
- 24.Leed-Kelly A, Russel KS, Bobo JK, McIlvain H. Feasibility of smoking cessation counseling by phone with alcohol treatment center graduates. Journal of Substance Abuse Treatment. 1996;13:203–210. doi: 10.1016/s0740-5472(96)00052-9. [DOI] [PubMed] [Google Scholar]
- 25.Lando HA, Rommens S, Klevan J, Roski J, Cherney L, Lauger G. Telephone support as an adjunct to transdermal nicotine in smoking cessation. American Journal of Public Health. 1997;87:1670–1674. doi: 10.2105/ajph.87.10.1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Costanza ME, Luckmann R, Stoddard AM, White MJ, Stark JR, Avrunin JS, Rosal MC, Clemow L. Using tailored telephone counseling to accelerate the adoption of colorectal cancer screening. Cancer Detection & Prevention. 2007;31:191–198. doi: 10.1016/j.cdp.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 27.Luckmann R, Savageau J, Clemow L, Stoddard A, Costanza M. A randomized trial of telephone counseling to promote screening mammography in two HMOs. Cancer Detection & Prevention. 2003;27:442–450. doi: 10.1016/j.cdp.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 28.Costanza ME, Stoddard AM, Luckmann R, White MJ, Avrunin JS, Clemow L. Promoting mammography: results of a randomized trial of telephone counseling and a medical practice intervention. American Journal of Preventive Medicine. 2000;19:39–46. doi: 10.1016/s0749-3797(00)00150-1. [DOI] [PubMed] [Google Scholar]
- 29.White MJ, Stark JR, Luckmann R, Rosal MC, Clemow L, Costanza ME. Implementing a computer-assisted telephone interview (CATI) system to increase colorectal cancer screening: a process evaluation. Patient Education and Counseling. 2006;61:419–428. doi: 10.1016/j.pec.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 30.Hoffman RM, Couper MP, Zikmund-Fisher BJ, Levin CA, McNaughton-Collins M, Helitzere DL, VanHoewyk J, Barry MJ. Prostate cancer screening decisions: Results from the National Survey of Medical Decisions (DECISIONS Study) Arch Intern Med. 2009;169:1611–1618. doi: 10.1001/archinternmed.2009.262. [DOI] [PubMed] [Google Scholar]
- 31.Partin MR, Dillon N, Haas M, Wilt TJ. The PSA test for prostate cancer: Is it right for ME? [4/3/2008]; http://www.hsre.minneapolis.med.va.gov/Translation.asp.
- 32.Costanza ME, Luckmann R, Stoddard AM, Avrunin JS, White MJ, Stark JR, Clemow L, Rosal MC. Applying a stage model of behavior change to colon cancer screening. Preventive Medicine. 2005;41:707–719. doi: 10.1016/j.ypmed.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 33.Weinstein ND. The precaution adoption process. Health Psychology. 1988;7:355–386. doi: 10.1037//0278-6133.7.4.355. [DOI] [PubMed] [Google Scholar]
- 34.Weinstein ND, Sandman PM. A model of the precaution adoption process: evidence from home radon testing. Health Psychology. 1992;11:170–180. doi: 10.1037//0278-6133.11.3.170. [DOI] [PubMed] [Google Scholar]
- 35.Miller W. Motivational interviewing with problem drinkers. Behavioral Psychotherapy. 1983;11:47–72. [Google Scholar]
- 36.Miller W, Rollnick S. Motivational Interviewing: Preparing People for Change. New York, NY: Guilford Press; 2002. [Google Scholar]
- 37.Miller W, Rollnick S. Motivational Interviewing: Preparing people to change addictive behaviors. New York, NY: Guilford Press; 1991. [Google Scholar]
- 38.Radosevich DM, Partin MR, Nugent S, Nelson D, Flood AB, Holtzman J, Dillon N, Haas M, Wilt TJ. Measuring patient knowledge of the risks and benefits of prostate cancer screening. Patient Education and Counseling. 2004;54:143–152. doi: 10.1016/S0738-3991(03)00207-6. [DOI] [PubMed] [Google Scholar]
- 39.Clemow L, Costanza ME, Haddad WP, Luckmann R, White MJ, Klaus D, Stoddard AM. Underutilizers of mammography screening today: Characteristics of women planning, undecided about, and not planning a mammogram. Annals of Behavioral Medicine. 2000;22:80–88. doi: 10.1007/BF02895171. [DOI] [PubMed] [Google Scholar]
- 40.Lerman C, Daly M, Sands C, Balshem A, Lustbader E, Heggan T, Goldstein L, James J, Engstrom P. Mammography adherence and psychological distress among at risk women for breast cancer. Journal of the National Cancer Institute. 1993;85(13):1074–80. doi: 10.1093/jnci/85.13.1074. [DOI] [PubMed] [Google Scholar]
- 41.O'Connor AM. Validation of a decisional conflict scale. Medical Decision Making. 1995;15:25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 42.O'Connor AM, Tugwell P, Wells GA, Elmslie T, Jolly E, Hollingsworth G, McPherson R, Drake E, Hopman W, MacKenzie T. Randomized trial of a portable, self-administered decision aid for postmenopausal women considering long-term hormone therapy. Medical Decision Making. 1998;18:295–303. doi: 10.1177/0272989X9801800307. [DOI] [PubMed] [Google Scholar]
- 43.Holmes-Rovner M, Kroll J, Rovner D, Schmitt N, Rothert ML, Padonu G, Talarczyk G. Patient decision support intervention: increased consistency with decision analytic models. Medical Care. 1999;37:270–284. doi: 10.1097/00005650-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 44.Holmes-Rovner M, Stableford S, Fagerlin A, Wei JT, Dunn RL, Ohene-Frempong J, Kelly-Blake K, Rovner DR. Evidence-based patient choice: A prostate cancer decision aid in plain language. BMC Medical Informed Decision Making. 2005;5(1):16. doi: 10.1186/1472-6947-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rakowski W, Andersen MR, Stoddard AM, Urban N, Rimer BK, Lane DS, Fox SA, Costanza ME. Confirmatory analysis of opinions regarding the pros and cons of mammography. Health Psychology. 1997;16(5):433–441. doi: 10.1037//0278-6133.16.5.433. [DOI] [PubMed] [Google Scholar]
- 46.Stata Data Analysis and Statistical Software, Stata SE v.10.1. [10/26/2009]; http://www.stata.com.
- 47.Partin MR, Nelson D, Flood AB, Friedemann-Sanchez G, Wilt TJ. Who uses decision aids? Subgroup analyses from a randomized controlled effectiveness trial of two prostate cancer screening decision support interventions. Health Expectations. 2006;9:285–95. doi: 10.1111/j.1369-7625.2006.00400.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Partin MR, Wilt TJ. Informing patients about prostate cancer screening: identifying and meeting the challenges while the evidence remains uncertain. American Journal of Medicine. 2002;113:691–693. doi: 10.1016/s0002-9343(02)01423-7. [DOI] [PubMed] [Google Scholar]
- 49.Partin MR, Nelson D, Flood AB, Friedemann-Sanchez G, Wilt TJ. Who uses decision aids? Subgroup analysis from a randomized controlled effectiveness trial of two prostate cancer screening decision support interventions. Health Expectations. 2006;9:285–295. doi: 10.1111/j.1369-7625.2006.00400.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Elwyn G, O'Connor A, Stacey D, Volk R, Edwards A, Coulter A, Thomson R, Barratt A, Barry M, Bernstein S, Butow P, Clarke A, Entwistle V, Feldman-Stewart D, Holmes-Rovner M, Llewellyn-Thomas H, Moumjid N, Mulley A, Ruland C, Sepucha K, Sykes A, Whelan T. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. International Patient Decision Aids Standards (IPDAS) Collaboration. British Medical Journal. 2006;333(7565):417. doi: 10.1136/bmj.38926.629329.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stange KC, Flocke SA, Goodwin MA, Kelly RB, Zyzanski SJ. Direct observation of rates of preventive services delivery in community family practice. Preventive Medicine. 2000;31:167–176. doi: 10.1006/pmed.2000.0700. [DOI] [PubMed] [Google Scholar]
- 52.Moore G, Showstack J. Primary Care Medicine in Crisis: Toward Reconstruction and Renewal. Annals of Internal Medicine. 2003;138:244–247. doi: 10.7326/0003-4819-138-3-200302040-00032. [DOI] [PubMed] [Google Scholar]
- 53.Flocke SA, Frank SH, Wenger DA. Addressing multiple problems in the family practice office visit. Journal of Family Practice. 2001;50:211–216. [PubMed] [Google Scholar]