Abstract
Objective
To assess racial differences in attitudes and knowledge about sterilization.
Design
Cross-sectional survey
Setting
Questionnaires were mailed to participants’ home addresses
Patients
193 women aged 18–45 who had undergone tubal sterilization.
Intervention(s)
None
Main Outcome Measure
Attitudes and knowledge about tubal sterilization and awareness of contraceptive alternatives
Results
We received 193 completed surveys (64% response rate). AA woman were more likely to have a family member who had undergone tubal sterilization, to report that their mothers influenced their sterilization decisions, and to report that prior unintended pregnancy and desire to avoid insertion of a foreign object were very important factors in their decision to choose sterilization over other methods. Compared to white women, AA women more often thought that sterilization reversal could easily restore fertility (62 % vs 36%); that a woman’s sterilization would reverse itself after 5 years (60% vs 23%); and that a man cannot ejaculate after vasectomy (38% vs 13%). Fewer AA women had ever heard of intrauterine contraception (90% vs 98%). Racial differences in knowledge remained statistically significant after adjusting for socioeconomic confounders.
Conclusions
Misinformation about sterilization and limited awareness of contraceptive alternatives among AA women may contribute to racial disparities in tubal sterilization rates.
Keywords: Tubal sterilization, disparities, knowledge and attitudes, race/ethnicity
INTRODUCTION
African American (AA) women are significantly more likely to undergo tubal sterilization than white women.(1–8) The reasons underlying the difference in sterilization rates remain unclear. While sterilization is a highly-effective method of contraception, many women regret having been sterilized, and the prevalence of regret is especially high among AA women.(9–13) Furthermore, there are other long-term, user-independent contraceptive methods that are as effective as sterilization and are reversible. The higher utilization of sterilization combined with the higher prevalence of subsequent regret among minority populations is potentially concerning and calls for a deeper understanding of the factors that shape sterilization decisions and how these factors may vary by race.
Medical decision making is a complex process that involves patient-, provider-, and system-level factors. Prior research has suggested that patient preferences may be particularly important in sterilization decision making.(1, 14) Preferences may be shaped by specific personal and familial experiences as well as more general knowledge and attitudes about a treatment or procedure and its alternatives.(15–18) Recent qualitative work has suggested that levels of contraceptive misinformation may be higher among minority women.(14) Such misinformation may arise from culturally-based health myths and/or unequal access to health care information, as minorities in the US are disproportionately poor.(15, 19) Accordingly, it is important to understand the underlying attitudes and knowledge that govern preferences and how these factors vary by race. There are no studies that directly compare AA and white women on patient-level factors related to contraceptive decision making. Therefore, the objective of this study was to assess racial differences in attitudes and knowledge about sterilization and contraceptive alternatives.
MATERIALS AND METHODS
Study population
Three hundred AA and white women between the ages of 18–45 who had undergone tubal sterilization between 2002 and 2008 were randomly selected from the Magee-Womens Hospital Research Registry for Women and Infants Health. A self-administered, anonymous questionnaire and a $2.00 bill were mailed to each potential participant’s home address. Two subsequent reminder postcards were sent at 2-week intervals to all potential participants. This study was approved by the University of Pittsburgh Institutional Review Board.
Study questionnaire
The questionnaire was developed using information gathered from a previous focus group study exploring which factors shape women’s decisions about sterilization as a contraceptive method.(14) The questionnaire incorporated the major themes that emerged during the qualitative study and was designed to quantitatively evaluate racial differences with respect to key patient-level factors related to sterilization decision making. The questionnaire ascertained information about sociodemographic characteristics, pregnancy and contraceptive history, reasons for choosing sterilization, persons who influenced sterilization decisions, and a series of questions designed to assess women’s knowledge about sterilization and awareness of alternative contraceptive methods.
Questions assessing reasons for choosing sterilization used a Likert-type scale in which women were asked to rate the importance of listed reasons as “very important,” “somewhat important,” “not at all important,” or “does not apply.” Women were also given the opportunity to list and rate other reasons that were important in their sterilization decision-making process. Knowledge items were true/false questions, including a “don’t know” response category to reduce guessing and improve reliability.(20) Knowledge items were based on comments that arose during the focus group discussions that indicated potential misinformation as well as an internet search on common myths about sterilization. In addition, two items were adapted from the Postpartum Tubal Sterilization Knowledge Questionnaire (PTSK-Q).(21) The PTSK-Q is a valid and reliable instrument for assessing understanding of postpartum sterilization. A separate group of items asked women whether or not they had ever heard of each of the following contraceptive methods by type or brand name: birth control pill, contraceptive patch (Ortho Evra), contraceptive vaginal ring (NuvaRing), progestin implant (Implanon or Norplant), intra-uterine device (IUD), contraceptive injection (Depo-Provera), and vasectomy.
Analysis
African American and white women’s responses to survey items were compared using t-tests for continuous variables and Chi-square tests for categorical variables. When the assumptions of these parametric tests were violated, the Wilcoxon rank sum and Fisher’s exact tests were conducted. For the Likert-type question about the relative importance of factors in sterilization decisions, we dichotomized responses to “very important” versus all other responses. To compare knowledge between the two groups, we compared percentage of correct answers for each item and for the total set of knowledge items. For items that were significant in bivariate analysis, we conducted multivariable logistic regression analysis to compare responses while controlling for age, education, insurance status, and marital status at the time of sterilization. Because we were interested in factors that may have influenced sterilization decisions, we adjusted for women’s sociodemographic characteristics at the time of the procedure rather than their current characteristics. However, we conducted secondary analyses for knowledge outcomes in which we adjusted for age, education, insurance status, and income at the time of survey completion. All analyses were performed using SAS, version 9.1 and STATA, version 11. Statistical significance was defined as a p-value of <0.05.
RESULTS
We received a total of 193 completed surveys (64% response rate). By race, the response rate was 61/115 (53%) for AA women and 130/185 (70%) for white women. Two of the respondents self-identified as “other” race on the questionnaire and were excluded from all analyses.
Sociodemographic and reproductive characteristics
Sociodemographic and reproductive characteristics of the study sample are shown by race in Table 1. Significantly more AA women reported a history of unintended pregnancy, abortion, and conception while using contraception. Among subjects with prior contraceptive failure, there were no racial differences in type of contraceptive method being used at the time of failure. Hormonal contraception (i.e., pill, patch, or vaginal ring) was the most commonly cited method being used when conception occurred for both AAs and whites (67% and 79%, respectively; p=0.30), and condoms were the second leading cause of contraceptive failures (29% for AAs and 33% for whites, p=0.74).
Table 1.
Sociodemographic and reproductive characteristics of study sample
| At time of sterilization | At time of survey | |||||
|---|---|---|---|---|---|---|
| Variable | AA (n=61) | White (n=130) | p-value | AA (n=61) | White (n=130) | p-value |
|
Sociodemographic characteristics | ||||||
| Age (mean) | 32.5 | 35.7 | <0.001 | 36.0 | 38.2 | 0.013a |
| Education (%) | 0.20 | 0.48 | ||||
| High school or less | 28.8 | 20.3 | 24.1 | 19.5 | ||
| At least some college | 71.2 | 79.7 | 75.9 | 80.5 | ||
| Insurance status (%) | 0.003b | 0.10b | ||||
| Public | 30.0 | 11.0 | 21.3 | 10.3 | ||
| Private or group | 70.0 | 88.2 | 75.4 | 87.3 | ||
| None | 0.0 | 0.8 | 3.3 | 2.4 | ||
| Marital status (%) | <0.001 | |||||
| Married | 34.4 | 73.0 | ----- | ----- | ----- | |
| D/S/W | 8.2 | 8.7 | ----- | ----- | ----- | |
| Cohabitating | 26.2 | 8.7 | ----- | ----- | ----- | |
| Single | 31.2 | 9.5 | ----- | ----- | ----- | |
| Annual household income | <0.001 | |||||
| <$20,000 | ----- | ----- | 35.0 | 13.1 | ||
| $20,000–$50,000 | ----- | ----- | ----- | 31.7 | 20.5 | |
| >$50,000 | ----- | ----- | 33.3 | 66.4 | ||
|
Reproductive characteristics | ||||||
| Number of children (mean) | 2.9 | 2.2 | 0.014a | ----- | ----- | ----- |
| Number of pregnancies (mean) | ----- | ----- | ----- | 4.5 | 3.1 | <0.001 |
| History of abortion (%) | ----- | ----- | ----- | 54.4 | 21.3 | <0.001 |
| History of unintended pregnancy c (%) | ----- | ----- | ----- | 80.0 | 54.5 | <0.001 |
| History of pregnancy while using a contraceptive method (%) | ----- | ----- | ----- | 41.4 | 26.6 | 0.045 |
AA = African American
Wilcoxon rank-sum test
Fisher’s exact test
Includes both unwanted or mistimed pregnancies
Attitudes
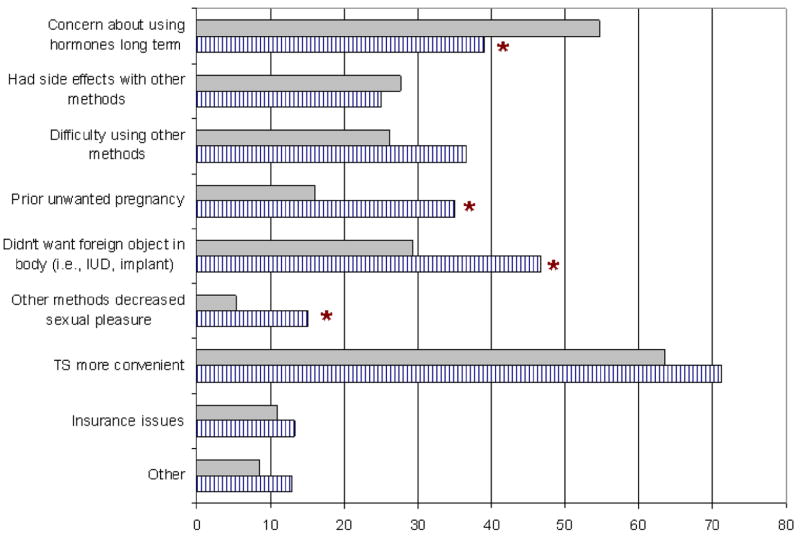
Women’s reasons for choosing sterilization over other contraceptive methods are shown in Figure 1. In unadjusted analyses, there were significant racial differences in ratings of several factors as depicted in the figure. When we adjusted for age, marital status, education, and insurance status at the time of sterilization, we found most of these racial differences were no longer statistically significant (Table 2).
Figure 1.
Percentage of women who rated each factor as “very important” in influencing her decision to choose sterilization over other contraceptive methods.
Grey bars represent white women; striped bars represent African American women TS = tubal sterilization; IUD = intrauterine device
*p-values < 0.05 in unadjusted analysis
Note: “Other” unique reasons listed by women as very important were: “higher likelihood of effectiveness”, “husband would not have vasectomy”, “IUD got infected”, “cannot use an IUD”, “Essure [procedure] did not work”, “tired of taking birth control pills”, and “the doctor encouraged it”
Table 2.
Unadjusted and adjusted odds ratios of responses to questions that were significant at the bivariate level
| Question (variable) | Unadjusted OR (95% CI) | Adjusted OR (95% CI)a |
|---|---|---|
| Attitudinal questionsb | ||
| Concern about using hormones long term | 0.53 (0.28 – 0.99) | 0.68 (0.33 – 1.39) |
| Prior unwanted pregnancy | 2.79 (1.38 – 5.67) | 1.94 (0.85 – 4.41) |
| Didn’t want foreign object in body (ie. IUD or implant) | 2.11 (1.12 – 3.99) | 1.95 (0.94 – 4.02) |
| Other methods decreased sexual pleasure | 3.07 (1.09 – 8.70) | 3.98 (1.14 – 13.86) |
| Family Influence | ||
| Likelihood of family members with TS | 2.36 (1.33 – 4.17) | 2.39 (1.25 – 4.53) |
| Mother most influential person in sterilization decision | 5.83 (1.45 – 23.46) | 4.34 (0.99 – 18.94) |
| Doctor most influential person in sterilization decision | 0.35 (0.14 – 0.90) | 0.40 (0.14 – 1.10) |
| Knowledge questionsc | ||
| TS reversal can easily restore fertility | 0.34 (0.18 – 0.64) | 0.44 (0.22 – 0.91) |
| TS will reverse itself after 5 years | 0.21 (0.11 – 0.40) | 0.30 (0.14 – 0.63) |
| A man can still ejaculate after vasectomy | 0.25 (0.12 – 0.51) | 0.29 (0.12 – 0.68) |
| Ovaries and uterus are removed during sterilization | 0.086 (0.01 – 0.76) | 0.09 (0.008 – 1.03) |
| Have ever heard of IUDs | 0.14 (0.028 – 0.072) | 0.11 (0.015 – 0.83) |
OR = odd ratio; CI = confidence interval; TS = tubal sterilization
Odds ratios represent responses for African American (AA) women and white women as reference group
Adjusted for age, marital status, education level, and insurance status at the time of sterilization
OR represents the odds of rating the factor as “very important” in sterilization decisions
OR represents the odds of answering true/false item correctly
The influence of family members in sterilization decision making also appeared to be different for AA and white women. AAs reported higher numbers of female family members that had undergone sterilization compared to whites (AA: mean=2.3; median = 2; range = 0–20; white: mean=1.3; median =1; range 0–8; p=0.003). More AAs reported that their mother was the most influential person in their decision to undergo sterilization (12% compared to 2% of white women; p=0.013). Conversely, fewer AAs reported that their doctor had played a significant role in their decision (10% compared to 25% of white women; p=0.029). After adjusting for socio-economic variables (age, education, marital status, and insurance status), the association between race and number of family members with tubal sterilization remained statistically significant (Table 2).
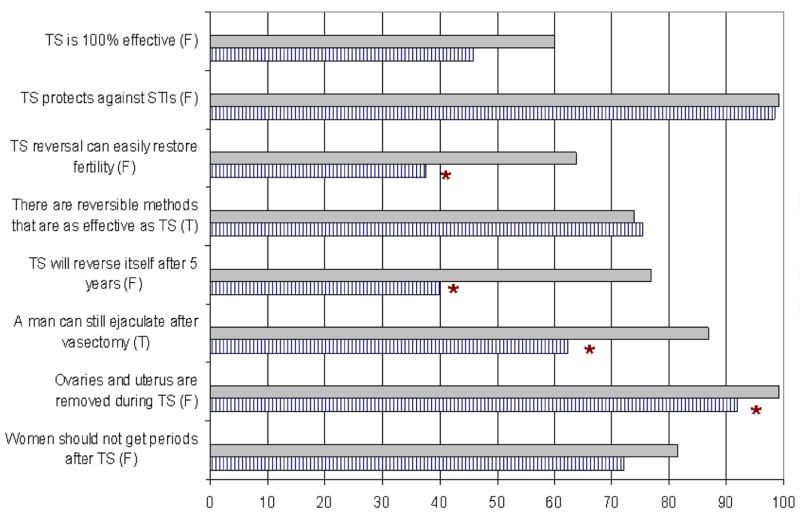
Knowledge
Comparison of responses of the true/false knowledge questions indicated that AA women had more misinformation about sterilization than white women (Figure 2). When we adjusted for age, marital status, education, and insurance status at the time of sterilization, all of the racial differences observed in bivariate analyses except one remained significant (Table 2). Overall, AA women had a significantly lower mean correct score (65% vs 80%; p<0.001) in both unadjusted and adjusted analyses. When we adjusted for current socioeconomic characeteristics (age, education, insurance status, and income), the results remained similar.
Figure 2.
Percentage of women who answered each true/false statement correctly
Grey bars represent white women; striped bars represent African American women
TS = tubal sterilization; STI = sexually transmitted infection
*p-values < 0.05 in unadjusted analysis
AA and white women were equally likely to have heard of all contraceptive alternatives except for IUDs, in which case 10% of AA women had never heard of this form of contraception compared to 2% of white women (p=0.013). This difference in IUD awareness remained after adjusting for socio-economic characteristics (Table 2). In both racial groups, progestin implants were the least known and the pill the most commonly known contraceptive method.
Because several currently available methods were approved by the US Food and Drug Administration (FDA) in 2001 [i.e., levonorgestrel-containing IUD (Mirena), birth control patch (Ortho Evra), and vaginal ring (NuvaRing)], we attempted to limit our study sample to women who had their sterilization procedure after 2002 to avoid any interaction between year of sterilization and contraceptive knowledge scores. However, 24 women (14 white and 10 AA) reported that they obtained their procedure prior to 2002. It is unclear whether our administrative database or women’s reports were more accurate in these cases. Therefore, we conducted secondary analyses for knowledge outcomes in which we excluded these 24 women and found that general trends with regard to racial differences in overall knowledge scores and awareness of IUDs did not change.
DISCUSSION
In this survey of 191 AA and white women of reproductive age, we found important racial differences in attitudes and knowledge regarding sterilization that may potentially contribute to observed racial differences in sterilization rates. We identified specific patient-level factors that may steer AA women toward sterilization over other contraceptive methods. These factors included a higher prevalence of previous unintended pregnancy, higher numbers of family members who have undergone sterilization coupled with greater family influence in sterilization decisions, greater preference to avoid a method that required insertion of a foreign object or that decreased sexual pleasure, greater misinformation about sterilization, and less awareness of IUDs among AA women compared to white women.
Previous research has indicated that a history of unintended pregnancy, which is experienced more often by AA women, may mediate the relationship between race and unintended pregnancy.(22) Our results are consistent with this prior research in that AA women in our sample, 80% of whom reported an unintended pregnancy, were more likely than white women to report that this experience motivated them to seek out sterilization. Women who have experienced an unintended pregnancy may develop a heightened sense of perceived fertility and/or diminished locus of control and perceive sterilization to be an effective way to gain control over their fertility. Once we adjusted for sociodemographic confounders, the racial difference was somewhat attenuated and no longer statistically significant. While the drop in level of significance may be related to sample size issues, it may also suggest that factors related to socioeconomic status (SES) play a larger role than race in shaping women’s responses to unintended pregnancy and whether or not she turns to sterilization versus considering other highly-effective methods. That is, a woman’s awareness of and access to contraceptive options other than sterilization and confidence in her ability to obtain and use such methods (i.e., self-efficacy) may be more related to SES than to race.
Another interesting finding is the racial variation in the role of family in contraceptive decision making. AA women in our sample reported higher numbers of family members who had undergone the procedure and also more often reported that their mothers influenced their decisions. These findings are consistent with our focus group study in which many AA women explained that they had been familiar with tubal ligations since an early age because family members had had the procedure, and that it, therefore seemed a natural choice.(14) This familiarity coupled with direct familial input in contraceptive decision making may perpetuate higher rates of sterilization among AA women.
Some of the attitudinal factors that may steer AA toward sterilization are not necessarily concerning or even modifiable (e.g., greater familiarity and family influence and less desire to have insertion of a foreign object); what is concerning is that such attitudes may be paired with erroneous contraceptive information. AA women in our sample seemed to have overly positive perceptions of female sterilization, overly negative perceptions of male sterilization, and less awareness about other long-acting, highly-effective reversible methods. Ironically, some of the characteristics that AA women incorrectly attributed to sterilization (high effectiveness for 5 years with easy return to fertility upon discontinuation/reversal) are actually more consistent with the characteristics of the IUD. AA women who have experienced unintended pregnancy, in particular, may be motivated to seek out a highly-effective method of contraception and because of familiarity with sterilization, belief that the procedure is 100% effective and easily reversible, and lack of awareness of IUDs, may turn to sterilization. Although there was no statistically significant racial difference with regard to percentage of women who believed that sterilization was 100% effective, 45% of women overall thought this to be the case (54% of AAs and 40% of whites). This is particularly concerning in light of recent data that sterilization failure rates may be higher than previously believed, approaching 7.5% over 10 years.(23) Such misunderstandings of the procedure may help to explain why the prevalence of sterilization regret is so high, especially among AA women.(9–13) Because sterilization is a provider-dependent method that requires informed consent, it is critical that providers assess the underlying attitudes and knowledge that govern a woman’s preference for sterilization. Given the number and potential complexity of factors that may shape women’s sterilization decisions, providing effective counseling may be challenging. As a starting point, Zite et. al have developed a validated questionnaire to assess patients’ understanding of tubal sterilization in an effort to help providers tailor pre-sterilization counseling and guide the informed consent process.
Several limitations need to be considered when interpreting our results. First, the generalizability of these findings may be limited by the fact that participants were recruited from a single hospital research registry. However, this hospital serves women from a large catchment area. Second, our survey asked women to recall events surrounding a procedure that may have occurred several years before and is, therefore, subject to recall bias. However, we are most interested in racial differences in the factors surrounding sterilization decisions and have no reason to suspect that recall differs by race. Third, the knowledge items that we used were created de novo and their psychometric properties were not formally assessed. Lastly, many of the attitudinal items which demonstrated significant racial differences in unadjusted analysis were not statistically significant in adjusted analysis. Given that point estimates remained large, this could suggest issues related to our sample size as we had only 61 participants in the AA group. Alternatively, the drop in level of significance could indicate that certain contraceptive attitudes were shaped more by SES factors (such as access to information and or resources) than cultural factors. Given that contraceptive attitudes and knowledge are shaped by the surrounding socioeconomic and cultural environment,(24) and that AAs in the US are disproportionately poor,(19) it may not be critical to try to tease out the independent effects of these factors when trying to understand how community attributes may impact psychosocial determinants of contraceptive behavior. Therefore, we feel that our unadjusted results are informative and can promote respectful contraceptive care by helping providers be aware of how attitudes may vary in diverse populations.
In summary, we identified specific patient-level factors that may steer AA women toward sterilization over other contraceptive methods and contribute to observed racial variation in sterilization utilization. Greater misinformation about sterilization and less awareness of contraceptive alternatives among AA women was a particularly concerning finding that should be addressed. It is important that providers assess women’s understanding of tubal sterilization including alternative contraceptive options so that all women, regardless of race/ethnicity, can make informed and satisfactory reproductive decisions.
Acknowledgments
This publication was made possible by Grant Number KL2 RR024154 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
Footnotes
Presented at: Portions of this analysis have been presented at: Reproductive Health annual meeting, Los Angeles, CA, September 30-October 4, 2009; 2010 Clinical and Translational Research and Education Meeting, Washington, DC, April 5-7, 2010; Society of General Internal Medicine Meeting, Minneapolis, MN, April 28-May 1, 2010
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Borrero S, Schwarz EB, Reeves MF, Bost JE, Creinin MD, Ibrahim SA. Race, insurance status, and tubal sterilization. Obstet Gynecol. 2007;109:94–100. doi: 10.1097/01.AOG.0000249604.78234.d3. [DOI] [PubMed] [Google Scholar]
- 2.Bumpass LL, Thomson E, Godecker AL. Women, men, and contraceptive sterilization. Fertility and sterility. 2000;73:937–46. doi: 10.1016/s0015-0282(00)00484-2. [DOI] [PubMed] [Google Scholar]
- 3.Chandra A. Surgical sterilization in the United States: prevalence and characteristics, 1965–95. Hyattsville, Maryland: National Center for Health Statistics; 1998. [PubMed] [Google Scholar]
- 4.Godecker AL, Thomson E, Bumpass LL. Fam Plann Perspect. Vol. 33. 2001. Union status, marital history and female contraceptive sterilization in the United States; pp. 35–41.pp. 9 [PubMed] [Google Scholar]
- 5.MacKay AP, Kieke BA, Jr, Koonin LM, Beattie K. Tubal sterilization in the United States, 1994–1996. Fam Plann Perspect. 2001;33:161–5. [PubMed] [Google Scholar]
- 6.Mosher WD, Martinez GM, Chandra A, Abma JC, Wilson SJ. Use of contraception and use of family planning services in the Unites States: 1982–2002. Hyattsville, Maryland: National Center for Health Statistics; 2004. [PubMed] [Google Scholar]
- 7.Piccinino LJ, Mosher WD. Trends in contraceptive use in the United States: 1982–1995. Fam Plann Perspect. 1998;30:4–10. 46. [PubMed] [Google Scholar]
- 8.Shapiro TM, Fisher W, Diana A. Family planning and female sterilization in the United States. Soc Sci Med. 1983;17:1847–55. doi: 10.1016/0277-9536(83)90161-2. [DOI] [PubMed] [Google Scholar]
- 9.Borrero SB, Reeves MF, Schwarz EB, Bost JE, Creinin MD, Ibrahim SA. Race, insurance status, and desire for tubal sterilization reversal. Fertility and sterility. 2007 doi: 10.1016/j.fertnstert.2007.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hillis SD, Marchbanks PA, Tylor LR, Peterson HB. Poststerilization regret: findings from the United States Collaborative Review of Sterilization. Obstet Gynecol. 1999;93:889–95. doi: 10.1016/s0029-7844(98)00539-0. [DOI] [PubMed] [Google Scholar]
- 11.Jamieson DJ, Kaufman SC, Costello C, Hillis SD, Marchbanks PA, Peterson HB. A comparison of women’s regret after vasectomy versus tubal sterilization. Obstet Gynecol. 2002;99:1073–9. doi: 10.1016/s0029-7844(02)01981-6. [DOI] [PubMed] [Google Scholar]
- 12.Moseman CP, Robinson RD, Bates GW, Jr, Propst AM. Identifying women who will request sterilization reversal in a military population. Contraception. 2006;73:512–5. doi: 10.1016/j.contraception.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 13.Schmidt JE, Hillis SD, Marchbanks PA, Jeng G, Peterson HB. Requesting information about and obtaining reversal after tubal sterilization: findings from the U.S. Collaborative Review of Sterilization. Fertility and sterility. 2000;74:892–8. doi: 10.1016/s0015-0282(00)01558-2. [DOI] [PubMed] [Google Scholar]
- 14.Borrero S, Nikolajski C, Rodriguez KL, Creinin MD, Arnold RM, Ibrahim SA. “Everything I Know I Learned from My Mother…or Not”: Perspectives of African-American and White Women on Decisions About Tubal Sterilization. J Gen Intern Med. 2008 doi: 10.1007/s11606-008-0887-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: a conceptual framework. American journal of public health. 2006;96:2113–21. doi: 10.2105/AJPH.2005.077628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sangi-Haghpeykar H, Ali N, Posner S, Poindexter AN. Disparities in contraceptive knowledge, attitude and use between Hispanic and non-Hispanic whites. Contraception. 2006;74:125–32. doi: 10.1016/j.contraception.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Understanding ethnic differences in the utilization of joint replacement for osteoarthritis: the role of patient-level factors. Med Care. 2002;40:I44–51. doi: 10.1097/00005650-200201001-00006. [DOI] [PubMed] [Google Scholar]
- 18.Suarez-Almazor ME, Souchek J, Kelly PA, O’Malley K, Byrne M, Richardson M, et al. Ethnic variation in knee replacement: patient preferences or uninformed disparity? Arch Intern Med. 2005;165:1117–24. doi: 10.1001/archinte.165.10.1117. [DOI] [PubMed] [Google Scholar]
- 19.Health, United States, 2004. Hyattsville, Maryland: National Center for Health Statistics; 2004. [Google Scholar]
- 20.Muijtjens AM, Mameren HV, Hoogenboom RJ, Evers JL, van der Vleuten CP. The effect of a ‘don’t know’ option on test scores: number-right and formula scoring compared. Med Educ. 1999;33:267–75. doi: 10.1046/j.1365-2923.1999.00292.x. [DOI] [PubMed] [Google Scholar]
- 21.Zite NB, Wallace LS. Development and validation of a Medicaid Postpartum Tubal Sterilization Knowledge Questionnaire. Contraception. 2007;76:287–91. doi: 10.1016/j.contraception.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 22.Borrero S, Moore CG, Qin L, Akers A, Creinin D, Ibrahim S. Unintended Pregnancy Influences Racial Disparity in Tubal Sterilization Rates. J Gen Intern Med. 2009 doi: 10.1007/s11606-009-1197-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reeves MF, Borrero S, Behringer T, Schwarz EB, Roberts MS, Creinin MD. Pregnancy after tubal sterilization in the United States. Abstract presented at the International Federation of Gynecology and Obstetrics (FIGO); 2009; October 4–9, 2009; Cape Town, South Africa. 2009. [Google Scholar]
- 24.Brown S, Eisenberg L. The best intentions: Unintended pregnancy and the well-being of children and families. Washington, D.C: National Academy Press; 1995. [PubMed] [Google Scholar]