Abstract
Alterations in lower extremity kinetics have been shown to exist in persons with knee osteoarthritis (OA), however few investigations have examined how the intersegmental coordination of the lower extremity kinetic chain varies in the presence of knee joint pathology. The objective of this study was to evaluate the how knee OA and walking speed affect total support moment and individual joint contributions to the total support moment. Fifteen healthy subjects and 30 persons with knee OA participated in 3D walking analysis at constrained (1.0 m/s), self-selected and fastest tolerable walking speeds. Individual joint contributions to total support moment were analyzed using separate ANOVAs with one repeated measure (walking speed). Linear regression analysis was used to evaluate the relationship between walking speed and joint contribution. Persons with knee OA reduced the contribution of the knee joint when walking at constrained (p=0.04) and self-selected walking speeds (p=0.009). There was a significant increase in the ankle contribution and a significant decrease in the hip contribution when walking speed was increased (P<0.004), however individual walking speeds were not significantly related to joint contributions. This suggests that the relationship between walking speed and joint contribution is dependent on the individual’s control strategy and we cannot estimate the joint contribution solely on walking speed. The slower gait speed observed in persons with knee OA is not responsible for the reduction in knee joint moments, rather this change is likely due to alterations in the neuromuscular strategy of the lower extremity kinetic chain in response to joint pain or muscle weakness.
Keywords: osteoarthritis, knee, gait, kinesiology, inverse dynamics
1. Introduction
Alterations in lower extremity kinetics and kinematics have been shown to exist in persons with knee osteoarthritis (OA) [1-7]. While many previous authors have focused on kinetic changes that occur in individual lower extremity joints, few have examined how the intersegmental coordination of the lower extremity kinetic chain varies in the presence of knee joint pathology. During gait, muscle moments generated about the hip, knee and ankle joints are responsible for maintaining vertical support of the body as well as propagating forward progression of the center of mass [8, 9]. Sagittal plane joint moments induced by hip and knee extensors as well as ankle plantar flexors play important roles in overcoming the effects of gravitational forces during walking. Summation of these joint moments results in the support moment, the overall moment providing support to the body during stance [10]. This moment has been shown to be a reliable and less variable measure of lower extremity kinetic chain synergy when compared to the analysis of individual joint moments [11, 12].
Alterations in lower extremity kinetics have been suggested by other authors in the presence of knee pathology or advanced age [4, 13, 14]. Even if the magnitude of the support moment is similar, persons with knee pathology will alter individual joint contributions to the total support moment [15-17]. In particular, subjects with OA may adopt different patterns of movement that distribute the contribution to support away from painful joints [18]. This redistribution of moments suggests a reorganization of motor control. Understanding which joints provide support during movement may provide a basis for interventions that promote successful compensatory strategies in persons with knee OA.
Changes in walking speed have been shown to affect gait variables in persons with and without knee OA [19-22]. The influence of walking speed is especially apparent in kinetic values that are based on changes in ground contact force and segmental accelerations, which increase when walking velocity increases. It is known that persons with knee OA adopt a slower self-selected walking speed and this may be partially responsible for previously reported differences in joint moments found in persons with knee OA [4, 18]. While the effect of walking speed on individual joint moments has been studied [19, 21, 23], the effect of walking speed on joint contributions to total support moment has not been critically evaluated. Therefore, the objective of the current study was twofold. The first objective was to determine how adults with and without knee OA utilize the ankle, knee and hip moments relative to the total support moment during self-selected and fast walking conditions. The second objective was to determine how the kinetic walking patterns are related to walking speed in individuals with knee OA. Because of pain, weakness and other factors associated with knee OA, we hypothesized that during walking, persons with OA will have a lower contribution to total support moment from the knee joint when compared to healthy controls. Additionally, we hypothesize that the slower gait speed observed in persons with knee OA will not be responsible for the reduction in knee joint moments.
2. Methods
2.1 Subjects
Fifteen healthy subjects and 30 subjects with knee OA were recruited from the local community (Table 1). Subjects with knee OA demonstrated radiographic evidence of knee OA in the medial tibiofemoral compartment with a Kellgren-Lawrence grade ≥ 2 as evidenced on a 30 degree bilateral flexed knee radiograph [24]. Healthy subjects were excluded if they had knee pain or radiographic evidence of osteophytes or narrowing of the tibiofemoral joint space. Subjects with and without OA were excluded if they had a history of systemic neurological, cardiopulmonary or orthopedic disease or trauma at any other lower extremity joint. For all of the OA subjects, only the more painful knee was included in the analysis. For subjects without knee OA, the leg chosen for analysis alternated between the left and right side. Prior to participation, all subjects signed an informed consent form approved by the Human Subjects Review Board.
Table 1. Subject demographics.
| Control (n=15) | OA (n=30) | p-value | |
|---|---|---|---|
| Age | 58 (9) | 63 (7) | 0.067 |
| Height | 1.66 (0.05) | 1.71 (0.10) | 0.076 |
| Weight | 70.13 (8.5) | 86.83 (13.3) | <0.001 * |
| Body mass index | 25.58 (3.5) | 29.75 (4.2) | 0.002 * |
| Quadriceps Strength (Nm/BW) | 1.76 (0.68) | 1.26 (0.45) | 0.010 * |
| Hamstring Strength (Nm/BW) | 1.06 (0.45) | 0.82 (0.33) | 0.077 |
| KOOS | 481 (23) | 270 (86) | <0.001 * |
| Self-selected Speed | 1.24 (0.17) | 1.08 (0.20) | 0.014 * |
| Fast Speed | 1.75 (0.22) | 1.42 (0.22) | <0.001 * |
p<0.05
Nm/BW = Newton*meters/body weight; KOOS = Knee Osteoarthritis and Outcome Score [max score = 500]
2.2 Gait Analysis
Three-dimensional kinematics were recorded at 60 Hz using a six camera Motion Analysis reflective marker system (Santa Rosa, CA, USA). A modified Helen Hayes marker set was used. Ground reaction forces and center of pressure data were recorded at 1080 Hz during walking trials on an instrumented split-belt treadmill with dual forceplates (Bertec Corp., Columbus, OH, USA). This instrument has previously been validated [25]. Self-selected walking speed was determined by a timed 10 meter walk in the hallway. After allowing time for familiarization to the treadmill [26], subjects walked at the self-selected speed for 30 seconds, during which time the data were recorded. Treadmill speed was then increased to the subject’s fastest tolerable speed at which a 30 second walking trial was recorded. Fastest tolerable speed was defined as the maximum speed at which the subjects were able to safely walk on the treadmill without running or holding onto the handrails. Data were also collected at a control speed of 1.0 m/s to control for the effect of walking speed on the gait variables. All subjects were attached to an overhead harness as a safety precaution and were instructed to walk without use of the handrails.
2.3 Data reduction
Coordinate positions of the reflective markers were smoothed using a phase-corrected Butterworth filter with a cutoff frequency of 6 Hz (EvaRT 5.0.4, Motion Analysis Corp) and joint angles were reconstructed using Euler angles. Inverse dynamic calculations of joint moments were performed using OrthoTrak 6.3.5 (Motion Analysis Corp.) and were normalized to the individuals’ body mass. All of the moments are reported as external joint moments. Gait cycles were divided from heel strike to ipsilateral heel strike as determined from kinematic data of the foot and sacral markers [27]. These cycles were then time normalized to 101 points and averaged for each variable. Summation of the hip, knee and ankle extensor moments provided a total support moment at each time step [10]. In order to assess differences in total support moment, mean peak total support moment was determined. Relative hip, knee and ankle joint contributions were determined as a percent of the total support and reported at the time of peak support moment.
For the self-selected and fast walking speeds, differences in mean peak total support moment were assessed using an ANOVA with one repeated measure (walking speed). Similarly, differences in individual joint contributions were evaluated using separate ANOVAs with one repeated measure (walking speed). Differences in walking speed between groups and conditions were assessed using a repeated measure ANOVA. At 1.0 m/s, differences were evaluated using separate one-way ANOVAs for the hip, knee and ankle contributions. Relational comparisons between the individual’s walking speed and joint contribution were separately evaluated for the OA and control groups at the self-selected and fast walking speeds using a linear regression analysis. All statistical tests were performed using SPSS software version 15 (Chicago, IL, USA).
3 Results
3.1 Walking Speed
In this study, subjects with OA chose a self-selected walking speed that was significantly slower than the freely chosen walking speed of the control group. The control group walked at 1.24 ± 0.17 m/s and the OA group at 1.08 ± 0.19 m/s (p<0.001). The trend was the same at the fast walking speed and subjects in the control group had a mean fast speed of 1.75 ± 0.22 m/s and the OA group walked at 1.43 ± 0.22 m/s (p<0.001). There was a significant speed by group interaction effect as the control group demonstrated a larger increase in speed between the self-selected and fast walking conditions (p<0.001).
3.2 Total Support Moment
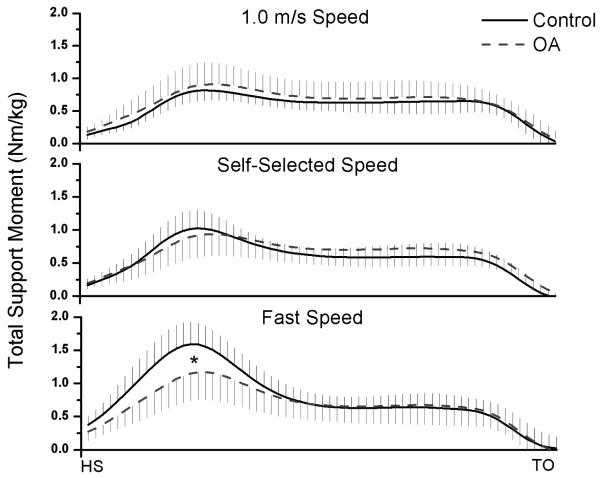
At 1.0 m/s, no significant differences existed between the groups for peak total support moment (p=0.15) (Figure 1). Peak total support moment for the control and OA group were 0.86 ± 0.16 Nm/kg and 0.96 ± 0.31 Nm/kg, respectively. There was a significant increase in total support moment peaks for both groups between the self-selected and fast walking speeds (p<0.001). At the self-selected walking speed, peak total support moment for the control and OA groups were 1.05 ± 0.25 Nm/kg and 0.96 ± 0.31 Nm/kg, respectively. This difference was not significantly different (p=0.36). At the fast walking speed, significant differences in peak total support moment were seen between the control (1.62 ± 0.33 Nm/kg) and OA group (1.20 ± 0.40 Nm/kg) (p=0.001).
Figure 1.
Peak total support moment was significantly greater in the control group at the fast walking speed (p<0.001). There was a significant increase in peak total support between the self-selected and fast walking condition in both groups (p<0.001).
3.3 Individual Joint Contribution
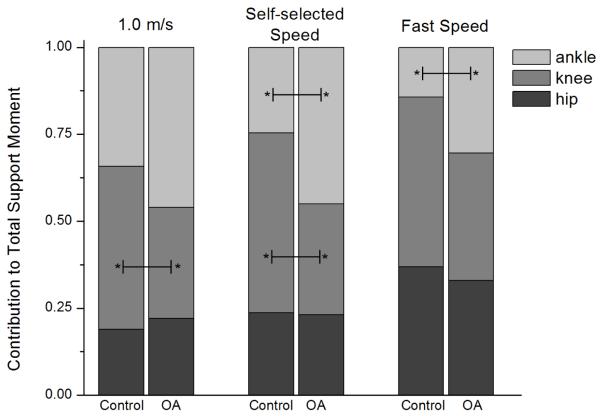
At 1.0 m/s, persons with knee OA demonstrated reduced knee contribution to total support (p=0.04), but no significant differences were seen for the hip (p=0.96) or ankle (p=0.07) (Figure 2). Knee contribution for the control and OA groups were 47% ± 17% and 32% ± 25%, respectively. A similar trend was seen at the self-selected walking speed and the OA group demonstrated a reduction in the contribution from the knee (p=0.009) and ankle (p=0.024) (Figure 2). Knee contribution to total support in the control group was 51% ± 15%, which was higher than 32% ± 26% in the OA group. The control group demonstrated a lower contribution from the ankle (25% ± 16%) when compared to the OA group (45% ± 32%). In the fast walking condition, only the contribution from the ankle demonstrated significant differences between groups. Ankle contribution to total support at the fast speed from the control and OA groups were 14% ± 12% and 30% ± 22%, respectively. Knee contribution from the control group was 49% ± 16% and was 37% ± 31% in the OA group. Although the mean knee contribution at the fast speed was 12.2% higher in the control group, there was large variability and the difference was not significant (p=0.09).
Figure 2.
Individual joint contributions to total support moment (*p<0.05). There was a significant increase in the hip moment (p=0.004) and reduction in the ankle moment (p<0.001).
For both groups, significant differences were found between self-selected and fast walking speeds for the hip (p=0.004) and ankle (p<0.001) contributions. There was a significant increase in the ankle contribution and a significant decrease for the hip contribution. No differences were found between speeds for the knee contribution. No group by speed interaction effects were seen for the hip, knee or ankle contributions. Using a regression model, self-selected and fast walking speeds were not significantly related to the respective hip, knee or ankle contribution, with the exception of the hip contribution in the control group at the fast walking speed. The significant relationship between the hip contribution and fast walking speed in the control group had an R2 value of 0.353 (p=0.019), with faster walking speeds resulting in higher hip contribution.
4 Discussion
The evaluation of knee contribution to total support adds to the understanding of compensatory strategies utilized by persons with knee OA. The magnitude of the total support moment remains unchanged between groups at the self-selected and controlled walking speeds, but individuals with knee OA alter the distribution of the load shared by the lower extremity kinetic chain. While previous investigations have revealed a reduction in the magnitude of the knee flexion moment in persons with knee OA [28, 29], we have found that subjects with OA adopt a reorganized control strategy to achieve a similar total support moment by reducing the knee contribution and increasing the ankle joint contribution.
Using the regression model, there was no consistent relationship between walking speed and joint contributions; however, there was an effect of speed on the joint contributions in both groups. Between self-selected and fast walking speeds, there was a consistent increase in the hip joint contribution and reduction in the ankle contribution. This suggests that the relationship between walking speed and joint contribution is dependent on the individual’s muscle coordination patterns (or control strategy) and we cannot estimate the joint contribution solely on walking speed. However, for each person, we can assume that an increase in walking speed above the self-selected speed will reduce the ankle contribution and increase the hip contribution, regardless of whether or not the individual has knee pathology. This supports previous research that has implicated the hip moment as playing a larger role during faster walking speeds [21, 22].
It appears that the strategy adopted by persons with knee OA is aimed at reducing the knee flexion moment at all walking speeds. It can be assumed that higher knee joint moments will result in higher muscle forces crossing the joint [30, 31]. An increase in muscle force may result in higher knee joint compression forces [32], which in turn may accelerate cartilage degeneration [33]. The reduction in contribution from the knee joint to total support may represent a compensatory strategy to reduce the need for quadriceps force during walking in order to reduce joint loading and joint pain. It is also possible that this strategy is a consequence of persistent quadriceps weakness in persons with knee OA [34-36]. If there is substantial weakness of the knee extensors, persons with knee OA may rely on the antigravity hip and ankle muscles during locomotion. As seen in the OA group, the reduction in knee contribution was augmented by an increase in the ankle moment. This tradeoff is in accordance with previous work that found increased ankle contribution may propagate a reduction in knee joint moment through segmental interaction [37].
As cartilage degrades in the medial compartment of the knee, there is an inherent loss of stability as the passive structures become lax. It is suggested that persons with knee OA ambulate with increased co-contraction of the quadriceps and hamstrings to overcome the passive laxity of the knee joint [38]. Although we did not analyze muscle activity, increased co-contraction of the quadriceps and hamstring muscle groups may lead to a knee stiffening strategy and subsequent reduction of the knee flexion moment during gait. Despite reducing the external knee flexion moment, this method of stabilization may increase the compression forces at the knee joint.
In the absence of antagonistic muscle activity, increasing the external knee flexion moment has been suggested to be a compensatory method to overcome the condylar lift-off induced by the frontal plane knee adduction moment [39]. However, in this study, we found a relative decrease in the contribution of the knee flexion moment in persons with knee OA and an increase in the contribution from the ankle. This supports previous studies that found increased activity of the plantarflexor muscles in addition to the quadriceps, may help control the frontal plane knee laxity [40, 41]. It should be pointed out that the gastrocnemius is a biarticular muscle that does cross the knee joint, and therefore increased moments at the ankle may coincide with higher gastrocnemius muscle activity and, subsequently, higher compressive force at the knee [42].
The use of the support moment in gait analysis provides us with information about how the individual joints are coordinated to maintain support of the body during walking. Comparison of the individual joint contributions to this moment allows us to formulate potential control strategies used to coordinate human movement and support. The results from our study show that persons with knee OA adopt a kinetic coordination strategy that reduces the contribution from the knee and increases contributions from ipsilateral joints, in particular, the ankle joint. This strategy was seen irrespective of freely chosen or constrained walking speed, suggesting that the reduction in knee contribution in persons with knee OA is not dependent on the lower freely chosen walking speed. Furthermore, increasing walking speed in all of the subject populations resulted in greater contribution from the hip joint. The slower gait speed observed in persons with knee OA is not responsible for the reduction in contribution from the knee joint. Instead, this change is likely due to alterations in the neuromuscular strategy of the lower extremity kinetic chain in response to joint pain, muscle weakness or a generalized stiffening strategy of antagonistic knee muscles.
5 Acknowledgements
Funding for this study was provided by National Institutes of Health P20-RR16458.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Childs JD, Sparto PJ, Fitzgerald GK, Bizzini M, Irrgang JJ. Alterations in lower extremity movement and muscle activation patterns in individuals with knee osteoarthritis. Clin Biomech. 2004;19:44–49. doi: 10.1016/j.clinbiomech.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Baliunas AJ, Hurwitz DE, Ryals AB, Karrar A, Case JP, Block JA, et al. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage. 2002;10:573–579. doi: 10.1053/joca.2002.0797. [DOI] [PubMed] [Google Scholar]
- 3.Thorp LE, Sumner DR, Block JA, Moisio KC, Shott S, Wimmer MA. Knee joint loading differs in individuals with mild compared with moderate medial knee osteoarthritis. Arthritis Rheum. 2006;54:3842–3849. doi: 10.1002/art.22247. [DOI] [PubMed] [Google Scholar]
- 4.Al-Zahrani KS, Bakheit AM. A study of the gait characteristics of patients with chronic osteoarthritis of the knee. Disabil Rehabil. 2002;24:275–280. doi: 10.1080/09638280110087098. [DOI] [PubMed] [Google Scholar]
- 5.Kaufman KR, Hughes C, Morrey BF, Morrey M, An KN. Gait characteristics of patients with knee osteoarthritis. J Biomech. 2001;34:907–915. doi: 10.1016/s0021-9290(01)00036-7. [DOI] [PubMed] [Google Scholar]
- 6.Gok H, Ergin S, Yavuzer G. Kinetic and kinematic characteristics of gait in patients with medial knee arthrosis. Acta Orthop Scand. 2002;73:647–652. doi: 10.1080/000164702321039606. [DOI] [PubMed] [Google Scholar]
- 7.Astephen JL, Deluzio KJ, Caldwell GE, Dunbar MJ. Biomechanical changes at the hip, knee, and ankle joints during gait are associated with knee osteoarthritis severity. J Orthop Res. 2008;26:332–341. doi: 10.1002/jor.20496. [DOI] [PubMed] [Google Scholar]
- 8.Anderson FC, Pandy MG. Individual muscle contributions to support in normal walking. Gait Posture. 2003;17:159–169. doi: 10.1016/s0966-6362(02)00073-5. [DOI] [PubMed] [Google Scholar]
- 9.Kepple T, Siegel K, Stanhope SJ. Relative contributions of the lower extremity joint moments to forward progression and support during gait. Gait and Posture. 1997;6:1–8. [Google Scholar]
- 10.Winter DA. Overall principle of lower limb support during stance phase of gait. J Biomech. 1980;13:923–927. doi: 10.1016/0021-9290(80)90162-1. [DOI] [PubMed] [Google Scholar]
- 11.Flanagan SP, Salem GP. The validity of summing lower extremity individual joint kinetic measures. J Appl Biomech. 2005;21:181–188. doi: 10.1123/jab.21.2.181. [DOI] [PubMed] [Google Scholar]
- 12.Winter D. Biomechanics and Motor Control of Human Movement. John Wiley and Sons; Hoboken, NJ: 2005. [Google Scholar]
- 13.DeVita P, Hortobagyi T. Age causes a redistribution of joint torques and powers during gait. J Appl Physiol. 2000;88:1804–1811. doi: 10.1152/jappl.2000.88.5.1804. [DOI] [PubMed] [Google Scholar]
- 14.Mundermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52:2835–2844. doi: 10.1002/art.21262. [DOI] [PubMed] [Google Scholar]
- 15.Mandeville D, Osternig LR, Chou LS. The effect of total knee replacement on dynamic support of the body during walking and stair ascent. Clin Biomech. 2007;22:787–794. doi: 10.1016/j.clinbiomech.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 16.Hurd WJ, Snyder-Mackler L. Knee instability after acute ACL rupture affects movement patterns during the mid-stance phase of gait. J Orthop Res. 2007 doi: 10.1002/jor.20440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rudolph KS, Axe MJ, Buchanan TS, Scholz JP, Snyder-Mackler L. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc. 2001;9:62–71. doi: 10.1007/s001670000166. [DOI] [PubMed] [Google Scholar]
- 18.Ouellet D, Moffet H. Locomotor deficits before and two months after knee arthroplasty. Arthritis Rheum. 2002;47:484–493. doi: 10.1002/art.10652. [DOI] [PubMed] [Google Scholar]
- 19.Bejek Z, Paroczai R, Illyes A, Kiss RM. The influence of walking speed on gait parameters in healthy people and in patients with osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2006;14:612–622. doi: 10.1007/s00167-005-0005-6. [DOI] [PubMed] [Google Scholar]
- 20.Landry SC, McKean KA, Hubley-Kozey CL, Stanish WD, Deluzio KJ. Knee biomechanics of moderate OA patients measured during gait at a self-selected and fast walking speed. J Biomech. 2007;40:1754–1761. doi: 10.1016/j.jbiomech.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 21.Lelas JL, Merriman GJ, Riley PO, Kerrigan DC. Predicting peak kinematic and kinetic parameters from gait speed. Gait Posture. 2003;17:106–112. doi: 10.1016/s0966-6362(02)00060-7. [DOI] [PubMed] [Google Scholar]
- 22.Riley PO, Della Croce U, Kerrigan DC. Propulsive adaptation to changing gait speed. J Biomech. 2001;34:197–202. doi: 10.1016/s0021-9290(00)00174-3. [DOI] [PubMed] [Google Scholar]
- 23.Mockel G, Perka C, Labs K, Duda G. The influence of walking speed on kinetic and kinematic parameters in patients with osteoarthritis of the hip using a force-instrumented treadmill and standardised gait speeds. Arch Orthop Trauma Surg. 2003;123:278–282. doi: 10.1007/s00402-003-0513-0. [DOI] [PubMed] [Google Scholar]
- 24.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tesio L, Rota V. Gait analysis on split-belt force treadmills: validation of an instrument. Am J Phys Med Rehabil. 2008;87:515–526. doi: 10.1097/PHM.0b013e31816f17e1. [DOI] [PubMed] [Google Scholar]
- 26.Zeni JA, Jr., Higginson JS. Gait parameters and stride-to-stride variability during familiarization to walking on a split-belt treadmill. Clin Biomech. 2009 doi: 10.1016/j.clinbiomech.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zeni J, Jr, Richards J, Higginson J. Two simple methods for determining gait events during treadmill and overground walking using kinematic data. Gait Posture. 2008;27:710–714. doi: 10.1016/j.gaitpost.2007.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McKean KA, Landry SC, Hubley-Kozey CL, Dunbar MJ, Stanish WD, Deluzio KJ. Gender differences exist in osteoarthritic gait. Clin Biomech. 2007;22:400–409. doi: 10.1016/j.clinbiomech.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 29.Astephen JL, Deluzio KJ, Caldwell GE, Dunbar MJ, Hubley-Kozey CL. Gait and neuromuscular pattern changes are associated with differences in knee osteoarthritis severity levels. J Biomech. 2008;41:868–876. doi: 10.1016/j.jbiomech.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 30.Crowninshield RD, Brand RA. A physiologically based criterion of muscle force prediction in locomotion. J Biomech. 1981;14:793–801. doi: 10.1016/0021-9290(81)90035-x. [DOI] [PubMed] [Google Scholar]
- 31.Challis JH. Producing physiologically realistic individual muscle force estimations by imposing constraints when using optimization techniques. Med Eng Phys. 1997;19:253–261. doi: 10.1016/s1350-4533(96)00062-8. [DOI] [PubMed] [Google Scholar]
- 32.Mesfar W, Shirazi-Adl A. Biomechanics of the knee joint in flexion under various quadriceps forces. Knee. 2005;12:424–434. doi: 10.1016/j.knee.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 33.Griffin TM, Guilak F. The role of mechanical loading in the onset and progression of osteoarthritis. Exerc Sport Sci Rev. 2005;33:195–200. doi: 10.1097/00003677-200510000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Fisher NM, Pendergast DR. Reduced muscle function in patients with osteoarthritis. Scand J Rehabil Med. 1997;29:213–221. [PubMed] [Google Scholar]
- 35.Slemenda C, Brandt KD, Heilman DK, Mazzuca S, Braunstein EM, Katz BP, et al. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med. 1997;127:97–104. doi: 10.7326/0003-4819-127-2-199707150-00001. [DOI] [PubMed] [Google Scholar]
- 36.O’Reilly S, Jones A, Doherty M. Muscle weakness in osteoarthritis. Curr Opin Rheumatol. 1997;9:259–262. doi: 10.1097/00002281-199705000-00014. [DOI] [PubMed] [Google Scholar]
- 37.Simonsen EB, Dyhre-Poulsen P, Voigt M, Aagaard P, Fallentin N. Mechanisms contributing to different joint moments observed during human walking. Scand J Med Sci Sports. 1997;7:1–13. doi: 10.1111/j.1600-0838.1997.tb00110.x. [DOI] [PubMed] [Google Scholar]
- 38.Zeni JA, Rudolph K, Higginson JS. Alterations in quadriceps and hamstrings coordination in persons with medial compartment knee osteoarthritis. J Electromyogr Kinesiol. 2009 doi: 10.1016/j.jelekin.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9:113–119. doi: 10.1002/jor.1100090114. [DOI] [PubMed] [Google Scholar]
- 40.Lewek MD, Ramsey DK, Snyder-Mackler L, Rudolph KS. Knee stabilization in patients with medial compartment knee osteoarthritis. Arthritis Rheum. 2005;52:2845–2853. doi: 10.1002/art.21237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lewek MD, Rudolph KS, Snyder-Mackler L. Control of frontal plane knee laxity during gait in patients with medial compartment knee osteoarthritis. Osteoarthritis Cartilage. 2004;12:745–751. doi: 10.1016/j.joca.2004.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Robon MJ, Perell KL, Fang M, Guererro E. The relationship between ankle plantar flexor muscle moments and knee compressive forces in subjects with and without pain. Clin Biomech. 2000;15:522–527. doi: 10.1016/s0268-0033(00)00007-3. [DOI] [PubMed] [Google Scholar]