Abstract
Brief measures of anxiety related severity and impairment that can be used across anxiety disorders and with subsyndromal anxiety are lacking. The Overall Anxiety Severity and Impairment Scale (OASIS) have shown strong psychometric properties with college students and primary care patients. This study examines sensitivity, specificity, and efficiency of an abbreviated version of the OASIS that takes only 2–3 minutes to complete using a non-clinical (college student) sample. 48 participants completed the OASIS and SCID for anxiety disorders, 21 had a diagnosis of ≥1 anxiety disorder, and 4 additional participants had a subthreshold diagnosis. A cut-score of 8 best discriminated those with anxiety disorders from those without, successfully classifying 78% of the sample with 69% sensitivity and 74% specificity. Results from a larger sample (n=171) showed a single factor structure and excellent convergent and divergent validity. The availability of cut-scores for a non-clinical sample furthers the utility of this measure for settings where screening or brief assessment of anxiety is needed.
Keywords: anxiety, measurement, psychometrics, screening
1. Introduction
Anxiety disorders are one of the most prevalent classes of psychiatric disorders with 18.1% of adults meeting diagnostic criteria (Kessler et al., 2006). In addition to the often-disabling symptoms, anxiety disorders are associated with poorer quality of life and elevated rates of co-occurring medical and psychiatric problems (Kroenke, Spitzer, Williams, Monahan, & Lowe, 2007; Mendlowicz & Stein, 2000; Stein et al., 2005; Sareen et al., 2006;).
Individuals diagnosed with an anxiety disorder have up to twelve times higher odds of additional anxiety disorder diagnoses (i.e., many have more than one anxiety disorder; Carter Wittchen, Pfister, & Kessler, 2001; Kessler et al., 2006; Ruscio et al., 2008) than those without an anxiety disorder. Research indicates that those with comorbid anxiety disorders experience greater distress and impairment than those with a single anxiety disorder diagnosis (Mennin, & Heimberg, & Jack, 2000; Kroenke et al., 2007). Subsyndromal anxiety disorders are also common and associated with significant impairment (e.g., Weiller, Bisserbe, Maier, & Lecrubier, 1998). Capturing the severity and impairment associated with anxiety disorders is important, as research has shown these factors influence whether or not individuals may benefit from treatment for their anxiety (e.g., Mathias et al., 1994; Nisenson, Pepper, Schwenk, & Coyne, 1998). Thus, screening and monitoring not only the occurrence of but also the severity and impairment associated with single anxiety disorders, multiple co-occurring anxiety disorders, and subsyndromal anxiety disorders is important in a variety of clinical and research settings.
Currently, a variety of well-validated measures assessing different aspects of anxiety exist. For example, measures assessing specific anxiety disorders are available such as the Panic Disorder Severity Scale-Self Report Version (Houck, Spiegel, Shear, & Rucci, 2002) and the Liebowitz Self-Rated Disability Scale for Social Phobia (Schneier et al., 1994). While very useful for thorough assessment of specific disorders these measures fail to capture anxiety-related severity and impairment across anxiety disorders or for comorbid diagnoses which is sometimes needed in settings where giving multiple disorder scales is not feasible. Additionally, disorder specific scales may be less feasible when broad assessments of anxiety-related difficulties are needed and time limitations prohibit the use of multiple measures for individuals with more than one anxiety disorder. An example would be a medical or research setting where many people need to be screened in a short amount of time and only those who appear to have anxiety related problems would warrant further disorder specific or diagnostic assessment.
Measures of overall anxiety severity also exist such as the Beck Anxiety Inventory (BAI; Beck & Steer, 1993), the State-Trait Anxiety Inventory (STAI; Spielberger, 1983), the Brief Symptom Inventory-18 (BSI-18) Anxiety Subscale (Derogatis, 1993), and the Hamilton Anxiety Rating Scale (HAM-A; Hamilton, 1959). At 21-items and 40-items respectively, the BAI and the STAI may be lengthy for some uses (e.g., epidemiological studies) and items assess somatic, cognitive and emotional symptoms, but not functional or behavioral difficulties. While the BSI-18-Anxiety is brief (only 6 items), the questionnaire asks exclusively about cognitive and affective symptoms. The HAM-A is 14 items and assesses a variety of somatic symptoms. Cognitive and affective symptoms are also assessed. These measures have shown strong psychometric properties in prior investigations. However, they fail to capture the functional and behavioral difficulties that often result from anxiety disorders. Such difficulties are often as clinically important as frequency and intensity of somatic and cognitive-affective symptoms (Telch et al. 1995).
The Overall Anxiety Severity and Impairment Scale (OASIS; Norman, Hami-Cissell, Means-Christensen, & Stein, 2006; supplemental materials), a 5-item self-report measure, was designed with these limitations in mind and aims to identify patients with probable anxiety disorders while assessing the frequency and intensity of anxiety symptoms, the functional impairment related to these anxiety symptoms, as well as behavioral avoidance across anxiety disorders or for subsyndromal anxiety. Each item of the OASIS instructs respondents to endorse one of five responses that best describes their experiences over the past week. Response items are coded from 0 to 4 and can be summed to obtain a total score ranging from 0 to 20. This study used a version of the OASIS in which the descriptions provided for each response option were abbreviated, compared to the original instrument [see supplemental materials and cf. Norman et al. 2006]. This version of the OASIS takes only 2–3 minutes to complete. The brevity of the OASIS makes it particularly useful for various clinical and research purposes such as community settings or epidemiological investigations requiring broad and efficient assessments due to time limitations and or client burden concerns. To the best of our knowledge the OASIS is the only available self-report scale assessing severity and impairment across anxiety disorders.
The psychometric properties of the OASIS have been evaluated in two previous investigations. The OASIS was found to have excellent test-retest reliability in addition to good convergent and discriminant validity in a sample of college students (Norman et al., 2006). The OASIS was also found to be unidimensional, with the five items showing high internal consistency. Additionally, in a sample of primary care patients referred to an anxiety disorder treatment study (Campbell-Sills et al., 2008), the OASIS again demonstrated a unidimensional factor structure. OASIS total scores correlated strongly with overall and single disorder measures of anxiety, and weakly with measures of unrelated constructs. A cut-score of 8 was identified as the most appropriate value, correctly classifying 87% of this sample as having an anxiety diagnosis or not. Taken together, these studies suggest that the OASIS is a valid instrument for measurement of anxiety severity and impairment in clinical and non-clinical samples; however, to date, there has been no evaluation of an optimal cut-score for identifying anxiety disorders in a non-clinical sample. This is important as base rates of anxiety are expected to be lower in a non-clinical sample than in a sample of primary care patients referred to anxiety treatment. The lower base rate may mean that a lower cut-score than the one found in a clinical sample may best distinguish those with from those without an anxiety disorder (e.g., Kraemer, 1992). In addition, the psychometric properties of the abbreviated version of the OASIS (which has shorter descriptions associated with the response options) have not been previously evaluated.
The goals of the present study were threefold: 1) determine sensitivity and specificity of the OASIS for a non-clinical sample, 2) determine an appropriate OASIS cut-score for classifying clinically significant anxiety in a college student sample to understand appropriate parameters for using the OASIS as a screening tool, and 3) conduct additional psychometric analyses including confirmatory factor analysis, internal consistency, convergent validity, and discriminant validity in this new sample of college students, and with this abbreviated version of the scale.
2. Method
2.1 Participants and Procedures
Participants were drawn from a large subject pool of undergraduates at San Diego State University (N > 2,500), who completed a questionnaire battery for course credit during the first month of the academic semester. This questionnaire battery included the Brief Symptom Inventory – Anxiety subscale (BSI-A; Derogatis, 1993). Each semester, subjects who score in the “high” and “normal” range on the BSI-A who check that they are willing to be contacted regarding further research participation are invited by our lab to participate in an experimental session that includes computer tasks and a questionnaire packet. Subjects selected for the “high anxiety” group score in the upper 15th percentile of the distribution of the BSI-A for that semester, while subjects in the “normal anxiety” group score in the 40th–60th percentile. The students from these groups who agreed to participate in the experimental session (n = 171) comprise the sample for this study. Because subjects were selected based on being in the “high” or “normal” range on the BSI-A, mean scores on the OASIS and other measures reported here should not be considered representative of a general undergraduate sample.
A total of 171 undergraduates agreed to participate in the experimental session for additional course credit and a payment of $25. Average age was 19.0 (SD=2.30). The majority was female (78.4 %). Participants were 50.3% Caucasian, 19.3 % Latino, 18.7 % Asian, 3.5% African American, and 7.6% mixed or other.
Forty eight participants who completed the experimental session also agreed to participate in additional research that involved completion of a diagnostic interview and (if eligible) an MRI scan. These participants did not differ from the rest of the sample on demographic or symptom measures. These participants were administered a modified version of the Structured Clinical Interview for DSM IV with Psychotic Screen (Patient Edition) (SCID- I/P; First, Spitzer, Gibbon, & William, 1997. This sample was 77.1% female, 64.6% Caucasian, 22.9% Asian American, 8.3% Hispanic, and 4.2% other, with a mean age of 19 (SD = 1.31). Twenty were identified as “high anxiety” participants and 28 were selected as “normal anxiety” participants using the BSI-A criteria described earlier. Twenty-one had a diagnosis of at least one anxiety disorder on the SCID (20 “high anxiety” and 1 “normal anxiety” subjects). One participant had obsessive compulsive disorder (OCD), 18 had generalized anxiety disorder (GAD), and 15 had social phobia. None had posttraumatic stress disorder, panic disorder or panic disorder with agoraphobia. Specific phobia was not assessed. One participant (who also met criteria for social phobia) met subthreshold criteria for panic disorder with agoraphobia. Six participants met subthreshold criteria for social phobia, four of whom did not meet criteria for any full anxiety disorder. Eight participants (38.1% of those with an anxiety disorder) met criteria for one anxiety disorder, thirteen (61.9% of those with an anxiety disorder) met criteria for two anxiety disorders. None met criteria for more than two. In addition, seven met criteria for major depressive disorder (MDD) and one participant met criteria for dysthymia. All individuals with MDD or dysthymia also met criteria for at least one anxiety disorder.
Trained interviewers with a range of education levels (doctoral level, master level, and bachelor level) administered the SCIDs. All interviewers completed a training process in which they participated in didactics, observed interview administration by senior staff, and completed three interviews in which they had to match diagnoses with a senior staff member. All SCIDs were reviewed and diagnoses approved by the study psychiatrist (MBS).
The investigation was carried out in accordance with the latest version of the Declaration of Helsinki. The study was reviewed by a university based human subjects review board and informed consent of the participants was obtained after the nature of the procedures had been fully explained.
2.2 Measures
The Overall Anxiety Severity and Impairment Scale (OASIS; Norman et al., 2006). All participants completed the OASIS, which consists of five items that measure the frequency and severity of anxiety, avoidance, work/school/home interference, and social interference due to anxiety. The instructions direct the respondent to consider experiences of “anxiety and fear” over the past week. Respondents select among five different response options for each item, which are coded 0–4 and summed to obtain a total score. Psychometric analyses of the OASIS with an undergraduate sample and a primary care sample suggested that the scale is unidimensional and has good internal consistency, test-retest reliability, and convergent/discriminant validity (Norman et al., 2006; Campbell-Sills et al., 2008). As noted above, the version of the OASIS used in this study was abbreviated in that the descriptions associated with response options were shorter. The instructions also were shortened (see supplemental materials and cf. Norman et al. 2006).
The Structured Clinical Interview for DSM-IV with psychotic screen (SCID-I/P; First et al., 1997) is a validated and well-recognized semi-structured interview used to establish DSM-IV Axis 1 diagnoses. The modules for all anxiety (except for specific phobias) and depressive disorders were administered. General administration of the SCID was around 1 hour to 1 ½ hours. Both current and lifetime diagnoses were assessed. A diagnosis of an anxiety or depressive disorder was met if a participant met full DSM-IV criteria for a disorder. A disorder was considered subthreshold if most (but not all) of the diagnostic criteria were met; this included cases in which all of the symptom criteria were met but clinically significant interference or distress (required for most diagnoses) was not present.
The following additional measures were in the initial questionnaire packet completed by 171 participants:
The Brief Symptom Inventory (BSI-18; Derogatis, 1993) is a widely used self-report measure of psychological symptoms. Respondents indicate how much discomfort each of the 18 items (e.g., nervousness or shakiness inside, poor appetite, trouble remembering things, feeling fearful, trouble falling asleep) has caused them during the past week on a 5 point scale, ranging from 0 (not al all) to 4 (extremely). Anxiety, depression, and somatization subscales can be computed. The Global Severity Index is the mean of the summed responses (range 0 – 4). The anxiety subscale (BSI-18-A) was used in this study as an indicator of convergent validity.
The Anxiety Sensitivity Index (ASI; Reiss, Peterson, Gursky, & McNally, 1986) is a well validated self report measure of sensitivity to anxiety-related sensations. Respondents rate how fearful they are on each of the 16 items (e.g., It scares me when I feel “shaky,” when my stomach is upset, I worry I might be seriously ill) on a 5 point scale, ranging from 0 (very little) to 4 (very much). Elevated scores on the ASI are associated with anxiety disorders and may predict risk for panic disorder (Blais et al., 2001) The ASI total score is the sum of the three ASI subscales (physical, psychological, and social).
The Spielberger State/Trait Anxiety Inventory (STAI; Spielberger, 1983; Spielberger et al., 1970) is self report measure of anxiety used in over 2000 published studies. For the “trait” version, respondents are instructed to answer the 20 items (e.g., I feel nervous and restless, I worry too much over something that really doesn’t matter) indicating how they generally feel using a 4 point scale; 1 (almost never) to 4 (almost always). Total trait anxiety (STAI-T) scores were used to assess the convergent validity of the OASIS.
The Social Interaction Anxiety Scale (SIAS). The SIAS (Mattick & Clarke, 1998) was designed to capture social interaction anxiety that has been defined as “distress when meeting and talking with others.” Respondents indicate how characteristic each of the 20 items (e.g., I tense up if I meet an acquaintance in the street, I have difficulty talking with other people) is of them using a 5 point scale; 0 (not at all) to 4 (extremely). The SIAS has good internal consistency, adequate convergent, but inadequate discriminant validity with similar/different measures of anxiety and mood disturbances. The measure was used in convergent validity analyses as an indicator of social anxiety.
The NEO personality inventory (NEO-PI-R; Costa & McCrae, 1992) is comprised of 240 questions measuring the Five Factor Model of personality. Respondents rate their agreement with statements on a 5 point scale; 0 (strongly disagree) to 4 (strongly agree). Item responses are summed to create an overall domain scores for Neuroticism, Extraversion, Openness, Agreeableness, and Conscientiousness, as well as six facet scores for each of the domains. The neuroticism subscale (NEO-N) was used to assess convergent validity with the OASIS and the agreeableness subscale (NEO-A) was used to assess discriminant validity.
The Connor-Davidson Resilience scale (CD-RISC). The CD-RISC (Connor & Davidson, 2003) is a self-report measure comprised of 25 items (e.g., I am able to adapt when changes occur; under pressure, I stay focused and think clearly), each rated on a 5-point scale, ranging from 0 (not true at all) to 4 (true nearly all of the time). Respondents are instructed to focus on how they felt over the past month when completing the measure. Scores are computed by summing the item responses (range 0–4) with higher scores reflecting greater resilience. This measure has shown sound psychometric properties, with good internal consistency and test–retest reliability in both general and clinical samples (Connor & Davidson, 2003). Total score was predicted to be negatively correlated with OASIS scores.
The Barratt Impulsiveness Scale (BIS-11; Patton, Stanford, & Barratt, 1995) has been shown to be a psychometrically sound measure of impulsiveness (Mcleish & Oxoby, 2007). Respondents are asked to answer 30 items “quickly and honestly” (e.g. I plan tasks carefully; I act “on impulse”) rating their answers on a 4 point scale ranging from 1 (rarely/never) to 4 (almost always). A total score is computed by summing the scores of the three subscales- Planning, Motor, and Cognitive. The Motor subscale (BIS-M) was used to assess discriminant validity with the OASIS.
The Zuckerman Sensation-Seeking Scale (SSS-V; Zuckerman, 1994) is a self report measure consisting of 40 items in which the respondent is asked to choose which of two statements they agree with more (e.g., I like “wild” uninhibited parties vs. I prefer quiet parties with good conversation). The measure can be divided into four different subscales (10 questions each) – Boredom Susceptibility (BS; assessing intolerance of monotony), Thrill and Adventure Seeking (TAS; measuring propensity towards physically dangerous pursuits), Experience Seeking (ES; assessing life-style changes and need for cognitive stimulation), and Disinhibition (D; measuring outgoing social behavior). The total score was used to assess divergent validity with the OASIS.
The Short Form-12 Health Survey (SF-12; Ware, Kosinski, & Keller,1996) was used as a measure of health-related quality of life. Two summary T-scores can be calculated, the mental component summary (MCS) and physical component summary. The physical health component was used to assess discriminant validity with the OASIS.
2.3 Statistical Analysis
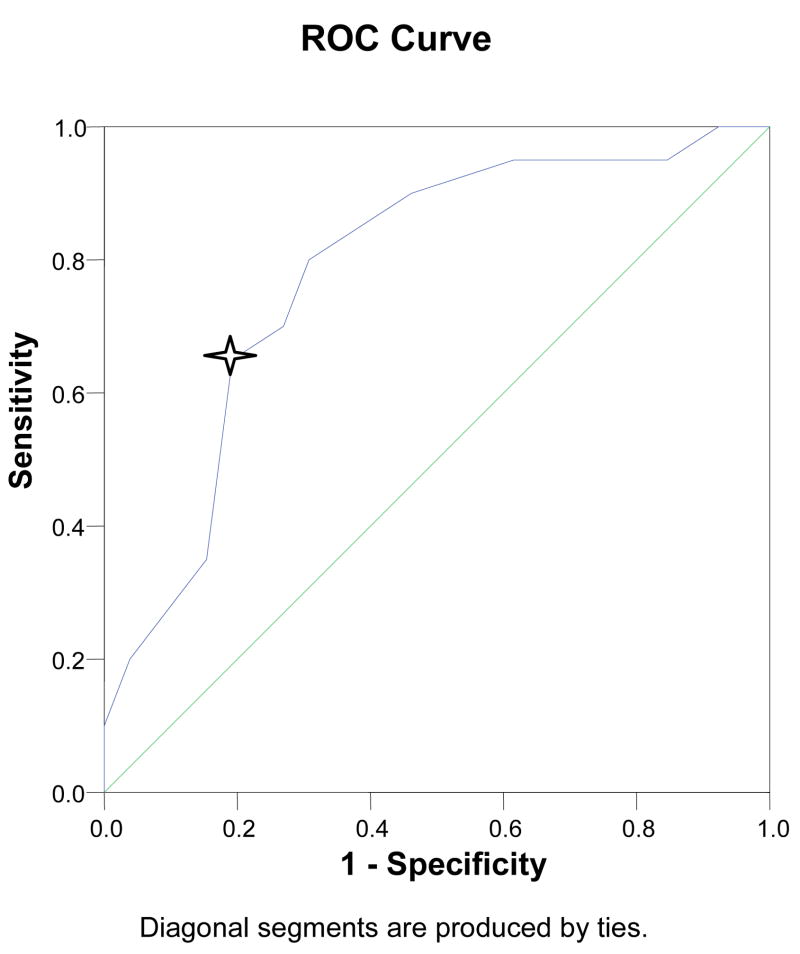
We used the sample of 48 participants who had completed the SCID in analyses to determine clinical cut-scores. Receiver operating characteristics (ROC) curves were used to determine sensitivity and specificity for each cut-score on the OASIS. Presence versus absence of an anxiety disorder diagnosis on the SCID was used as the categorical outcome. A ROC curve is a plot of the true positive rate (sensitivity) against the false positive rate (1- specificity) for the different possible cut points and thus provides a visual representation of the tradeoff between sensitivity and specificity of cut-scores for a diagnostic test. Chi-square tests, sensitivity values, and specificity values were used to calculate percentage of patients correctly classified. The sensitivity, specificity, and percent correctly classified values were used to select an appropriate cut-score for identifying participants with probable anxiety disorders using the OASIS.
Data from a sample of 171 participants (that included the 48 participants in the sensitivity and specificity analyses) were used to confirm previous factor analytic results in undergraduate (Norman et al., 2006) and primary care (Campbell-Sills et al., 2008) samples. Both of these prior studies used exploratory factor analysis (EFA) and one used confirmatory factor analysis (CFA) to evaluate the factor structure of the OASIS, and both concluded that the scale was unidimensional. CFA results from the primary care study further indicated that in addition to a single latent factor explaining covariance among the five items, the error variances of items 1 and 2 were correlated, most likely because responses to item 2 are partially dependent on responses to item 1 (i.e., a zero response to item 1 regarding frequency (“no anxiety in the past week”) necessitates a zero response to item 2 regarding intensity (“anxiety was absent or barely noticeable”). These findings served as the basis for the CFA model in the present study.
For CFA, the sample variance-covariance matrices were analyzed using a latent variable software program (Mplus 2.12, Muthén & Muthén, 1998) and maximum likelihood estimation. Goodness of fit was evaluated using the chi-square test (χ2), root-mean-square error of approximation (RMSEA) and its 90% confidence interval, p value for test of closeness of fit (Cfit; estimates the probability that RMSEA < .05), standardized root-mean-square residual (SRMR), and comparative fit index (CFI). Final acceptance or rejection of models was based on conventional criteria for good model fit (RMSEA < .08, Cfit, 90% CI < .08; SRMR < .05; CFI > .90; Jaccard & Wan, 1996), strength of parameter estimates (i.e., primary factor loadings > .35, absence of salient cross-loadings), and the conceptual interpretability of the solution.
The larger sample was also used for calculation of internal consistency. Strong positive correlations of the OASIS with anxiety scales including the BSI-18; ASI, STAI-T, SIAS, and NEO-N and negative correlation with the CD-RISC were interpreted as evidence for convergent validity. To assess discriminant validity, we computed correlations between the OASIS and the NEO-A, BIS-M, and SSS-V. Correlations below .30 were considered supportive of discriminant validity.
3. Results
3.1 Preliminary Analyses
The mean OASIS score for the sample of 171 participants who completed self-report measures was 6.61 (SD = 4.01, range = 0–20). The mean for those in the normal anxiety group was 4.86 (SD = 2.75) and the means for those in the high anxiety group was 9.92 (SD = 3.70); T (139) = 9.25, P<.001. There were no significant differences in score by gender, ethnicity, or family income. Cronbach’s alpha for the 5 items of the OASIS was .89.
3.2 Sensitivity, Specificity, and Correct Classification
Scores on the OASIS for the 48 participants who completed the SCID ranged from 0 to 15 (M = 7.19, SD. = 3.67). Mean OASIS score among those without an anxiety diagnosis was 5.69 (sd = 3.27) and for those with was 9.15 (sd = 3.28), T(44,1) = 3.45, p < .001. We assessed whether a particular cut-score on the OASIS was best able to discriminate those who met criteria for any anxiety disorder from those who did not. Since all of participants who met criteria for a depressive disorder (MDD or dysthymia) also met criteria for at least one anxiety disorder, they were grouped into the anxiety diagnosis category. We generated a ROC curve with the OASIS total score as the continuous variable and diagnostic status as the categorical outcome of interest. We then computed percent of patients correctly classified using all viable cut-scores. Correct classification was calculated as the sum of true positives plus true negatives divided by the total sample size. We stopped computing sensitivity and specificity for cut-scores after 10 because of the chi-square value was no longer significant and the percent correctly classified was diminishing (Table 2).
Table 2.
Sensitivity, Specificity, and Percent Correctly Classified of OASIS Cut-Scores for Identification of Individuals with Anxiety Diagnoses
| OASIS Score | χ2 (1, 48) | Sensitivity | Specificity | % Correctly Classified |
|---|---|---|---|---|
| 2 | .62 | .95 | .11 | .47 |
| 3 | .76 | .90 | .18 | .50 |
| 4 | 1.37 | .90 | .21 | .52 |
| 5 | 5.82* | .90 | .40 | .62 |
| 6 | 8.58** | .86 | .55 | .70 |
| 7 | 10.24** | .76 | .70 | .72 |
| 8 | 7.96* | .69 | .74 | .78 |
| 9 | 9.48** | .61 | .81 | .72 |
| 10 | 2.29 | .33 | .85 | .62 |
| 11 | 2.36 | .28 | .88 | .62 |
p < .05;
p < .01
The ROC curve and corresponding sensitivity and specificity values indicated that a cut-score between 7 and 8 would maximize sensitivity relative to specificity (Figure 1). Table 2 shows the chi-square values and percentages of patients correctly classified with cut-scores of two through eleven. A cut-score of >8 was judged to be optimal given that it successfully classified 78% of the sample with the most favorable balance of sensitivity (69%) and specificity (74%).
Figure 1. Receiver Operating Characteristic (ROC) Curve for OASIS Scores to Predict Presence of Anxiety Disorders.
Receiving Operator Characteristic (ROC) Curve for OASIS score to Predict Anxiety Disorder Diagnostic Status
*A cut-score of 8 correctly identified the anxiety disorder status of 78% of the sample (i.e., an OASIS score of 8 or above indicates probable anxiety disorder).
We ran the same procedures but included the four individuals who only had subthreshold diagnoses to identify the best cut-score for those with any significant anxiety (full or subthreshold diagnosis) from those without. Results did not differ when these four subthreshold patients were included.
3.3. Confirmatory Factor Analysis
The hypothesized model specified paths from a single factor (“anxiety”) to each of the five items, as well as a path between the error terms of items 1 and 2 to account for the partial interdependence of responses to these two items (i.e., a “0” response to item 1 necessitates a “0” response to item 2; see Campbell-Sills et al., 2008). This model fit the data very well, χ2 (4) = 5.605, ns; RMSEA = .048, 90% CI = .000–.133, CFit = .424; SRMR = .017; CFI = .997. Each item displayed salient loadings on the latent factor (.64 to .91) and the correlation between the error terms of items 1 and 2 was significant (r = .18, z = 3.71, p < .001). Standardized residuals and modification indices did not suggest any points of strain in the model. Factor determinacies are validity coefficients indicating the correlation between factor score estimates and their respective factors (Grice, 2001). The determinacy of the single factor was favorable at .95 (Gorsuch, 1983).
Although the hypothesized model provided excellent fit for the data, we ran analyses to test two competing models: (1) a simpler one-factor model with no error theory (i.e., no correlation was permitted between the error terms of items 1 and 2), and (2) a two-factor model in which items 1 and 2 loaded on one factor and items 3, 4, and 5 loaded on a second factor. The single-factor model with no error theory was rejected because it did not meet criteria for good model fit, χ2 (5) = 23.298, p < .001; RMSEA = .146, 90% CI = .090 – .209, CFit = .004; SRMR = .041; CFI = 0.962. Modification indices for this model indicated a clear point of strain in the model pertaining to unexplained covariance between items 1 and 2 (MI = 18.344; Standardized EPC = .179). The two-factor model provided a good fit for the data (fit statistics are identical to those of the hypothesized model), but was rejected on conceptual grounds: the two latent factors were highly overlapping (R = .86) suggesting poor discriminant validity between the two factors.
3.4 Convergent and Discriminant Validity
Table 1 shows that the OASIS correlated moderately (rs =.64 to .70, ps < .001) with the other measures of anxiety and neuroticism (BSI-18-A, ASI, TRAIT, SIAS, NEO-N). The correlation with the CD-RISC was significant and negative as predicted (r = −.60, p < .001). Discriminant validity analyses showed that the OASIS did not correlate (or correlated only weakly) with measures assessing dissimilar constructs including BIS-motor, Zuckerman, NEO-A, and physical health disability (SF-12-P) rs = .01 to −.13
Table 1.
Correlations of OASIS with Convergent and Discriminant Validity Measures
| OASIS | BSI-A | ASI | STAIT | SIAS | NEO-N | CD- RISC | BIS- motor | BIS- plan | SSS-V | NEO-A | NEO-C | SF-12-P | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OASIS | --- | .66 | .64 | .68 | .64 | .69 | −.60 | .11 | .27 | .07 | −.11 | −.33 | .04 |
| BSI-A | --- | .58 | .68 | .47 | .63 | −.53 | .10 | .22 | .06 | −.13 | −.33 | −.03 | |
| ASI | --- | .54 | .55 | .53 | −.42 | .12 | .25 | .01 | −.06 | −.25 | −.03 | ||
| STAIT | --- | .56 | .70 | −.68 | .08 | .33 | .03 | −.13 | −.38 | −.01 | |||
| SIAS | --- | .50 | −.58 | .01 | .29 | −.09 | .04 | −.32 | .04 | ||||
| NEO-N | --- | −.63 | .21 | .28 | .01 | −.25 | −.47 | −.01 | |||||
| CD-RISC | --- | −.05 | −.46 | −.05 | .13 | .56 | .08 | ||||||
| BIS-Mot | --- | .43 | .40 | −.18 | −.43 | .06 | |||||||
| BIS-Plan | --- | .26 | .00 | −.66 | −.01 | ||||||||
| SSS-V | --- | −.22 | −.31 | .06 | |||||||||
| NEO-A | --- | .07 | .11 | ||||||||||
| NEO-C | --- | .03 | |||||||||||
| SF-12-P | --- |
Note. Correlations in bold are statistically significant at p < .0001. OASIS = Overall Anxiety Severity and Impairment Scale. BSI-A = Brief Symptom Inventory – Anxiety Subscale. ASI = Anxiety Sensitivity Index Total Score. TRAIT = Spielberger Trait Anxiety Total Score. NEO-N = NEO Neuroticism Subscale. CD-RISC = Connor-Davidson Resiliency Scale. BIS-Mot = Barrett Impulsivity Scale Motor Subscale. BIS-Plan = Barrett Impulsivity Scale Planning Subscale. SSS-V = Zuckerman Sensation Seeking Scale. NEO-A = NEO Agreeableness Subscale. NEO-C = NEO Consciensciousness Subscale. SF-12-P = Short Form Health Survey – Physical Health Subscale.
4. Discussion
This study evaluated the psychometric properties of the OASIS, a self-report measure of anxiety severity and impairment, including sensitivity, specificity, and most efficient cut-scores for discriminating those significant anxiety symptoms (i.e., full or subthreshold anxiety disorder diagnoses) from those without. Two previous investigations provided evidence for the reliability and validity of the OASIS in a college student (Norman et al. 2006) and primary care sample (Campbell-Sills et al., 2008); however, diagnostic status was not available in the previous college student evaluation so that sensitivity, specificity, and efficiency information could not be computed. This is the first study to assess the measure’s ability to differentiate those with significant anxiety from those without in a non-clinical sample. This information is pivotal if the OASIS is to be used as a screening tool for clinical or research purposes. A score of 8 or higher correctly identified 78% of participants with an anxiety disorder. At this cut-off, 69% of participants with an anxiety disorder and 74% of participants without an anxiety disorder were correctly classified. However, if the goal is to identify all possible cases of anxiety disorders a cut score with higher sensitivity (e.g., 6 or 7) could be used and if the goal is to identify individuals most likely to have no anxiety related severity or impairment, higher cut-scores with greater specificity (e.g., 9) may be considered (see Table 2).
The score identified in this report were the same as the cut-score identified for a sample of primary care patients (Campbell-Sills et al., 2008) where ≥8 was found to be the most efficient score, successfully classifying 87% of the sample with 89% sensitivity and 71% specificity. Research with additional samples (e.g., non-college student, non-clinical samples) will help determine if other cut scores are most efficient in other populations.
The results of this study, with a new sample of college students and an abbreviated version of the scale (with shorter instructions and descriptions of response options), were consistent with prior psychometric research on the OASIS (Norman et al., 2006; Campbell-Sills et al., 2008), demonstrating a single factor structure, excellent internal consistency, strong convergent validity with other measures related to anxiety and neuroticism, and divergent validity with non-anxiety/depression measures. The single factor structure identified in all three OASIS evaluations suggests use of a total score (computed by summing the five items). This single total score contributes to ease of use, which combined with its brevity make the OASIS a good candidate for settings in which rapid, efficient assessment of anxiety is needed. All three studies have also shown that OASIS scores have not varied by gender suggesting the cut offs identified here can be used with male and female samples.
In addition to the measures used in the 2006 college student study, this study included the Social Interaction Anxiety Scale for convergent validity as well as the Zuckerman Sensation Seeking Scale and SF-12 Physical Component for divergent validity both of which were related to the OASIS in the expected manner. While the measures selected for assessment of convergent validity generally target symptoms rather than severity and impairment specifically, a strong positive relationship was predicted since anxiety impairment should not be present unless anxiety symptoms are present (Norman et al., 2006). Overall the results of this study add evidence of the sound psychometric properties of the OASIS.
Campbell-Sills et al (2008) noted that a limitation of the OASIS with primary care patients was that it was strongly correlated to measures of depression and not well able to discriminate between anxiety and depression. Several possible explanations were offered (the high comorbidity of these disorders, some symptom overlap, questions regarding whether patients were well able to discern the differences between the two disorders). In the present study, the OASIS was also moderately correlated with a measure of depression (BSI depression subscale, r = .61, p < .001). Unfortunately, we were not able to estimate OASIS norms for patients with mood disorders using this sample because all participants who met criteria for a depressive disorder also met criteria for at least one anxiety disorder. Future research is needed with samples that include depressed non-anxious participants to determine whether the OASIS is able to discriminate anxiety from depression. However, this limitation should not preclude use of the OASIS. Scores above the cut-offs identified here should prompt clinicians and researchers to further assess the presence of anxiety and commonly co-occurring symptoms, which, depending on the purpose, may include assessment to discriminate between anxiety and depression.
Several additional limitations should be noted. Although we had good distribution of ethnicity and gender, our college student sample was limited in age range, which may limit the generalizability of our results. A college student sample may also limit generalizability because of other factors that may characterize college students (e.g., high rates of alcohol abuse). Our cut score analyses were also limited by small sample size and the fact that most participants were female. In addition, convergent validity measures consisted solely of other self-report inventories. Therefore, it is possible that some of the relationships observed between the OASIS and other measures of anxiety may have been attributable to method effects. Future validity studies should include measures of anxiety severity that do not rely on self-report. Selection for participation in the study was contingent on having high or normal scores on a self-report measure of anxiety. Future studies should be designed such that a full range of possible anxiety states are represented. Although the SCID modules for all anxiety disorders except specific phobia were administered, only OCD, GAD, and SAD were present in our sample. Future studies are needed to better understand the discriminant validity of the OASIS in relation to other negative emotional states (in addition to depression) and to further develop the construct validity of the tool in relation to anxiety risk processes.
5. Conclusions
This study adds to the growing literature supporting the OASIS as a valid tool for measuring anxiety severity and impairment that can be used across anxiety disorders, with multiple anxiety disorders, and with subthreshold anxiety disorders. The availability of cut-scores for non-clinical samples, both for likely full diagnosis and for subthreshold or full diagnosis, adds to the utility of the instrument as a screening tool to be used in clinical, community, or research settings where brief assessment is needed. In addition, this study suggests that a version of the OASIS with shorter instructions and response options has comparable reliability, validity, and factor structure to the original instrument (allowing for even greater efficiency of assessment). To the best of our knowledge, the OASIS is the only measure of anxiety severity and impairment validated for such broad application.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Sonya B. Norman, Email: snorman@ucsd.edu.
Laura Campbell-Sills, Email: l2campbellsills@ucsd.edu.
Carla A. Hitchcock, Email: chitchcock@ucsd.edu.
Alexis Rochlin, Email: alexis.rochlin@gmail.com.
Kendall C. Wilkins, Email: kcwilkin@ucsd.edu.
Murray B. Stein, Email: mstein@ucsd.edu.
References
- Beck AT, Steer RA. Beck Anxiety Inventory Manual. San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- Blais MA, Otto MW, Zucker BG, McNally RJ, Schmidt NB, Fava M. The anxiety sensitivity index: item analysis and suggestions for refinement. Journal of Personality Assessment. 2001;77:272–294. doi: 10.1207/S15327752JPA7702_10. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Norman SB, Craske MG, Sullivan G, Lang AJ, Chavira DA, et al. Validation of a brief measure of anxiety-related severity and impairment: the Overall Anxiety Severity and Impairment Scale (OASIS) Journal of Affective Disorders. 2008;112:92–101. doi: 10.1016/j.jad.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter RM, Wittchen HU, Pfister H, Kessler RC. One-year prevalence of subthreshold and threshold DSM-IV generalized anxiety disorder in a nationally representative sample. Depression and Anxiety. 2001;13:78–88. doi: 10.1002/da.1020. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC) Depression and Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. Revised NEO Personality Inventory (NEO-PIR) and NEO Five-Factor Inventory professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Derogatis LR. Brief Symptom Inventory: Administration, scoring, and procedures manual. Minneapolis, MN: NCS Pearson, Inc; 1993. [Google Scholar]
- Eisenberg D, Gollust SE, Golberstein E, Hefner JL. Prevalence and correlates of depression, anxiety, and suicidality among university students. American Journal of Orthopsychiatry. 2007;77:534–542. doi: 10.1037/0002-9432.77.4.534. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I disorders (SCID I) New York: Biometric Research Department; 1997. [Google Scholar]
- Gorsuch RL. Factor analysis. 2. Erlbaum; Hillsdale, NJ: 1983. [Google Scholar]
- Grice JW. Computing and evaluating factor scores. Psychoogical Methods. 2001;6:430–450. [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Houck PR, Spiegel DA, Shear MK, Rucci P. Reliability of the self-report version of the panic disorder severity scale. Depression and Anxiety. 2002;15:183–185. doi: 10.1002/da.10049. [DOI] [PubMed] [Google Scholar]
- Jaccard J, Wan CK. LISREL approaches to interaction effects in multiple regression. Sage Publications; Thousand Oaks, CA: 1996. [Google Scholar]
- Kessler RC, Chiu WT, Jin R, Ruscio AM, Shear K, Walters EE. The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2006;63:415–424. doi: 10.1001/archpsyc.63.4.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC. Evaluating Medical Tests: Objective and Quantitative Guidelines. Newbury Park, California: Sage Publications; 1992. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Mathias SD, Fifer S, Mazonson PD, Lubeck DP, Buesching DP, Patrick DL. Necessary but not sufficient: The effect of screening and feedback on outcomes of primary care patients with untreated anxiety. Journal of General Internal Medicine. 1994;11:606–615. doi: 10.1007/BF02600303. [DOI] [PubMed] [Google Scholar]
- McLeish KN, Oxoby RJ. Measuring Impatience: Elicited Discount Rates and the Barratt Impulsiveness Scale. Personality and Individual Differences. 2007;43:553–565. [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behavior Research and Therapy. 1998;36:455–470. doi: 10.1016/s0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- Mendlowicz M, Stein MB. Quality of life in individuals with anxiety disorders. American Journal of Psychiatry. 2000;157:669–682. doi: 10.1176/appi.ajp.157.5.669. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Heimberg RG, Jack MS. Comorbid generalized anxiety disorder in primary social phobia: symptom severity, functional impairment, and treatment response. Journal of Anxiety Disorders. 2000;14:325–343. doi: 10.1016/s0887-6185(00)00026-8. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus 3.0 [Computer software] Author; Los Angeles: 1998. [Google Scholar]
- Nisenson LG, Pepper CM, Schwenk TL, Coyne JC. The nature and prevalence of anxiety disorders in primary care. General Hospital Psychiatry. 1998;20:21–28. doi: 10.1016/s0163-8343(97)00096-0. [DOI] [PubMed] [Google Scholar]
- Norman SB, Hami-Cissell S, Means-Christensen AJ, Stein MB. Development and Validation of an Overall Anxiety Severity and Impairment Scale (OASIS) Depression & Anxiety. 2006;23:245–249. doi: 10.1002/da.20182. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, Kessler RC. Social fears and social phobia in the USA: results from the National Comorbidity Survey Replication. Psychological Medicine. 2008;38:15–28. doi: 10.1017/S0033291707001699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sareen J, Jacobi F, Cox BJ, Belik SL, Clara I, Stein MB. Disability and poor quality of life associated with comorbid anxiety disorders and physical conditions. Archives of Internal Medicine. 2006;166:2109–2116. doi: 10.1001/archinte.166.19.2109. [DOI] [PubMed] [Google Scholar]
- Schneier FR, Heckelman LR, Garfinkel R, Campeas R, Fallon BA, Gitow A, et al. Functional impairment in social phobia. Journal of Clinical Psychiatry. 1994;55:322–331. [PubMed] [Google Scholar]
- Spielberger C. Stait-Trait Anxiety Inventory (Form Y) RedwoodCity: Mind Garden; 1983. [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the stait-trait anxiety inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- Stein MB, Roy-Byrne PP, Craske MG, Bystritsky A, Sullivan G, Pyne JM, et al. Functional impact and health utility of anxiety disorders in primary care outpatients. Medical Care. 2005;43:1164–1170. doi: 10.1097/01.mlr.0000185750.18119.fd. [DOI] [PubMed] [Google Scholar]
- Telch MJ, Schmidt NB, Jaimez TL, Jacquin KM, Harrington PJ. Impact of cognitive-behavioral treatment on quality of life in panic disorder patients. J Consult Clin Psychol. 1995;63:823–830. doi: 10.1037//0022-006x.63.5.823. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Weiller E, Bisserbe JC, Maier W, Lecrubier Y. Prevalence and recognition of anxiety syndromes in five European primary care settings: A report from the WHO study on psychological problems in general health care. British Journal of Psychiatry. 1998;34:18–23. [PubMed] [Google Scholar]
- Zuckerman M. Behavioral expressions and biosocial bases of sensation seeking. New York: Cambridge University Press; 1994. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.