Abstract
Background:
The purposes of this study were to identify changes in tear dimensions, shoulder function, and glenohumeral kinematics when an asymptomatic rotator cuff tear becomes painful and to identify characteristics of individuals who develop pain compared with those who remain asymptomatic.
Methods:
A cohort of 195 subjects with an asymptomatic rotator cuff tear was prospectively monitored for pain development and examined annually for changes in various parameters such as tear size, fatty degeneration of the rotator cuff muscle, glenohumeral kinematics, and shoulder function. Forty-four subjects were found to have developed new pain, and the parameters before and after pain development were compared. The forty-four subjects were then compared with a group of fifty-five subjects who remained asymptomatic over a two-year period.
Results:
With pain development, the size of a full-thickness rotator cuff tear increased significantly, with 18% of the full-thickness tears showing an increase of >5 mm, and 40% of the partial-thickness tears had progressed to a full-thickness tear. In comparison with the assessments made before the onset of pain, the American Shoulder and Elbow Surgeons scores for shoulder function were significantly decreased and all measures of shoulder range of motion were decreased except for external rotation at 90° of abduction. There was an increase in compensatory scapulothoracic motion in relation to the glenohumeral motion during early shoulder abduction with pain development. No significant changes were found in external rotation strength or muscular fatty degeneration. Compared with the subjects who remained asymptomatic, the subjects who developed pain were found to have significantly larger tears at the time of initial enrollment.
Conclusions:
Pain development in shoulders with an asymptomatic rotator cuff tear is associated with an increase in tear size. Larger tears are more likely to develop pain in the short term than are smaller tears. Further research is warranted to investigate the role of prophylactic treatment of asymptomatic shoulders to avoid the development of pain and loss of shoulder function.
Level of Evidence:
Prognostic Level III. See Instructions to Authors for a complete description of levels of evidence.
Little information is available as to why some rotator cuff tears are painful while others are completely asymptomatic. Given the high prevalence of asymptomatic rotator cuff tears in an elderly population1,2 and the considerable rate of subsequent pain development in these tears3, evaluation of the risk of pain development and identification of the factors that are related to pain development would be fundamental to understanding the natural history of rotator cuff disease. Furthermore, better characterization of these factors will help to identify at-risk individuals and potentially guide preventative and therapeutic treatment strategies.
The assessment of the natural history of asymptomatic rotator cuff tears and the factors related to pain development requires a prospective, longitudinal analysis of a cohort of subjects. By evaluating both shoulders in a cohort of patients with unilateral shoulder pain related to rotator cuff disease, we identified a large cohort of individuals with asymptomatic rotator cuff tears for prospective analysis. The present study represents a preliminary report of an ongoing prospective study. The study purposes were to characterize the changes that occur in tear morphology, shoulder function, and glenohumeral kinematics when an asymptomatic rotator cuff tear becomes painful and to identify the characteristics of the individuals who developed pain compared with those who remained asymptomatic.
Materials and Methods
Study Subjects
The present study was approved by our institutional review board. The subjects of the study represent a subgroup of an ongoing prospective cohort study in which standardized bilateral assessment of shoulder function and shoulder ultrasonography and radiography are performed every twelve months to study the natural history of asymptomatic rotator cuff tears. Inclusion criteria were patients who (1) presented for bilateral shoulder ultrasonography at our institution to investigate unilateral shoulder pain without a history of shoulder injury, (2) were discovered to have a rotator cuff tear in the painful shoulder, (3) were discovered to also have a rotator cuff tear (either full or partial thickness) in the “asymptomatic” contralateral shoulder, (4) were verified as persistently asymptomatic at the time of study initiation, and (5) had no history of trauma to either shoulder and remained free of injury for the duration of the study. Exclusion criteria were (1) any past or current substantial pain in the asymptomatic shoulder at the time of study enrollment, (2) continuous use of narcotic pain medication or anti-inflammatory medication for longer than three months from the time of study enrollment because of the possibility of pain-masking, (3) a traumatic episode to the asymptomatic shoulder, (4) inflammatory arthropathy, (5) a history of seeking medical attention for other problems in the asymptomatic shoulder (such as instability or arthritis), (6) use of the upper extremity for weight-bearing, (7) a very small (<5-mm) partial-thickness tear in the asymptomatic shoulder, and (8) a tear of the subscapularis tendon. Substantial pain was defined as (1) any pain of ≥3 on a 10-point visual analog pain scale that had lasted longer than six weeks, (2) any pain considered to be greater than that normally experienced as part of daily living, (3) any pain requiring the use of medications such as narcotics or nonsteroidal anti-inflammatory drugs, or (4) any pain that prompted a physician visit for evaluation. A pain score of 3 was chosen as the minimal pain level for distinction of “substantial pain” as our clinical experience demonstrates that patients seeking medical evaluation for a painful shoulder generally report pain scores of ≥5. A total of 195 subjects who met the selection criteria were identified and entered the study at various time points over a period of approximately five years. At the time of data collection for the present study, the follow-up period for the 195 subjects ranged from 0.5 year to approximately five years.
The subjects were carefully monitored for the onset of new pain in the asymptomatic shoulder and were examined every twelve months. They were asked to contact the study coordinator when new pain developed so that a determination could be made as to whether the symptoms met the criteria of new pain and to record the time of pain development. The definition of new pain was shoulder pain that developed spontaneously without an injury and met one of the following conditions: (1) any pain with a score of ≥3 on the 10-point pain scale and lasting longer than six weeks, (2) any pain that required formal consultation with a physician, (3) any pain that required the use of pain medications, or (4) any pain that was present at night and had affected sleep for longer than six weeks. Subjects who had forgotten to call us at the time of pain development were asked at their annual visit to recall when the pain had started. Regardless of the time of pain development, the subjects were examined only at their yearly visits.
Of the 195 subjects enrolled, forty-four were found to have developed new pain in the asymptomatic shoulder after study enrollment. The mean follow-up period (and standard deviation) for these forty-four subjects was 1.93 ± 1.2 years (range, 0.4 to 4.4 years). These subjects were assigned to the symptomatic group. To further characterize these subjects in contrast to those who remained asymptomatic, we grouped all fifty-five subjects who had been enrolled in the study for at least two years and had remained asymptomatic until the time of the present study as the asymptomatic group. The remaining ninety-six subjects who were not included in either group comprised sixty-two who remained asymptomatic but had been in the study for less than two years, thirty-two who withdrew from the study permanently, and two who had inadequate data for this study. There were three study time-points. One was the time of enrollment, which referred to the time point when a subject entered the study and completed the initial shoulder assessment. Visit 1 was the time point when subjects in the asymptomatic group returned for their first annual shoulder examination or when subjects in the symptomatic group were last evaluated before the onset of new pain. Visit 2 was the time point when subjects in the asymptomatic group returned for their second annual shoulder examination or when subjects in the symptomatic group were evaluated for the first time after pain development.
Shoulder Ultrasonography
Shoulder ultrasonography was performed in real time with use of Siemens Elegra and Antares scanners (Siemens Medical Solutions, Mountain View, California) and a variable high-frequency linear array transducer (7.5 to 13 MHz) by one of three radiologists with extensive experience in musculoskeletal ultrasonography. Each subject had standardized ultrasonography of both shoulders as previously described4,5. Ultrasonography has gained popularity for imaging of rotator cuff abnormalities and is accepted as an accurate imaging modality for rotator cuff disease4-7. The accuracy of ultrasonography for identifying and quantifying the size of full-thickness and partial-thickness cuff tears has been shown to be comparable with that of magnetic resonance imaging, with an overall accuracy of 87% at our institution5. The maximum anteroposterior dimension of a tear was measured in transverse views (i.e., perpendicular to the long axis of the rotator cuff) and designated as the width of the tear. The maximum degree of retraction was measured in longitudinal views (i.e., parallel to the long axis of the rotator cuff) and designated as the length of the tear. Tear length was measured from the lateral edge of the rotator cuff footprint on the greater tuberosity. Although tear size measurement had been performed for both full-thickness and partial-thickness tears, only the data from full-thickness tears were used for comparisons because of the relatively low accuracy of ultrasonography for measuring the size of partial-thickness tears5. Substantial tear progression was defined as transformation of a partial-thickness tear into a full-thickness tear or a size increase of >5 mm in either the width or the length of a full-thickness tear compared with that at the time of enrollment. To evaluate fatty degeneration of the rotator cuff muscles, the echogenicity and echotexture of each cuff muscle was examined with use of a 3-point scale as described by Strobel et al.8. The echogenicity was graded in comparison with the echogenicity of the overlying muscle (i.e., the deltoid for supraspinatus grading and the trapezius for infraspinatus grading). The echotexture was graded on the basis of the visibility of the central tendon and the normal muscular pennate pattern. The sum of the echogenicity and echotexture grades was calculated and used for data analysis. The radiologists were blinded as to the pain status and history of the subjects but were aware of the results of the previous sonography examinations.
Shoulder Function Assessment
Shoulder function was assessed with use of validated shoulder outcome tools and objective functional instruments. The assessment of subjective shoulder function included questionnaires pertaining to the American Shoulder and Elbow Surgeons (ASES) score9 and the 36-Item Short-Form Health Survey (SF-36)10. The self-assessment domain of the ASES score includes a pain score assessed with use of a visual analog scale and a summary score for various activities of daily living. The SF-36 questionnaire was used to determine the global effect that pain development in a previously asymptomatic shoulder may have on a person's general health status. The assessment of objective shoulder function included physical examination with goniometric measurement of active and passive ranges of motion of the shoulder including forward elevation, external rotation at the side, external rotation and internal rotation at 90° of abduction, and internal rotation in extension. The range of internal rotation in extension was categorized in such a way that the least internal rotation (i.e., the hand can reach to the waist) was given a grade of 6, and the greatest internal rotation (i.e., the thumb reaching the level of the fifth thoracic vertebra) was given a grade of 1. Isometric external rotation strength was measured at 0° of abduction and 45° of internal rotation of the shoulder with the subject in a sitting position. Strength measurement was repeated three times for each shoulder with use of an Isobex dynamometer (Cursor AG, Bern, Switzerland), and the average of the three measurements was obtained and used for analysis. All physical examinations were performed by either a dedicated research nurse (G.S.) or a research fellow (H.M.K., a medical doctor). Both were independent examiners with extensive experience with the study protocol.
Radiographic Analysis of Glenohumeral Kinematics
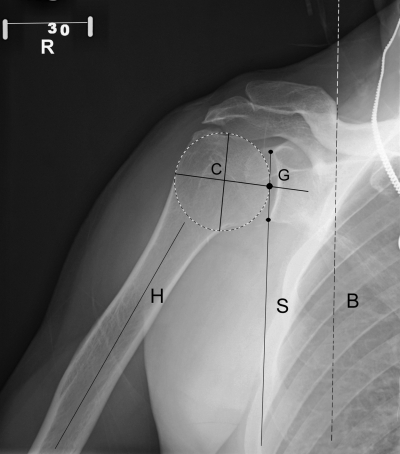
Standardized radiographic studies were performed as previously described11,12. Three radiology technicians were specifically selected and trained to standardize the quality of the radiographs. According to the study protocol, bilateral modified scapular plane anteroposterior radiographs were made for all subjects. Radiographs were made with the patient in the standing position with the body rotated 30° so that the plane of the scapula was parallel to the plane of the x-ray cassette and perpendicular to the x-ray beam. Each subject actively elevated the shoulder in the plane of the scapula with the shoulder in neutral rotation (the forearm parallel to the floor). Radiographs were made at 0°, 30°, 60°, and 90° of scapular plane abduction. A grid was constructed to precisely control the angle of abduction. The distance between the shoulder and the cassette, and between the shoulder and the x-ray beam column, was kept constant to avoid magnification errors. A premeasured, radiopaque marker was placed on all cassettes to further standardize magnification. Radiographs were saved in the Picture Archiving and Communication System (PACS; Siemens, Munich, Germany) and retrieved later for analysis. Radiographic measurements were performed by two independent observers (one fellow [H.M.K.] and one resident [N.A.M.]) with use of a software-enhanced modification (Scion Image; Scion, Frederick, Maryland) of the technique described by Poppen and Walker13. The geometric center of the humeral head was located first with a so-called best-fit circle positioned over the humeral articular surface (Fig. 1). The superior and inferior rims of the glenoid were then marked to demarcate the glenoid line. The glenoid center point was calculated by the software. The vertical distance from the geometric center of the humeral head to the glenoid center was calculated by the software to assess superior humeral head migration. A line drawn along the long axis of the humerus was compared with the glenoid line to calculate the glenohumeral angle. The glenoid line was compared with the vertical axis of the body to calculate the scapulothoracic angle. The ratio of glenohumeral to scapulothoracic motion was obtained at each abduction angle by dividing the glenohumeral angle by the scapulothoracic angle. The length of the radiopaque marker was measured and compared with the known length to control for subtle variations in magnification. Kinematic analysis was performed only on the symptomatic group.
Fig. 1.
Radiographic measurement of glenohumeral kinematics. The geometric center of the humeral head (C) was located first with a so-called best-fit circle positioned over the humeral head outline. The superior and inferior rims of the glenoid were then marked to demarcate the glenoid line. The glenoid center point (G) was then located automatically by the software. The vertical distance from the geometric center of the humeral head to the glenoid center was measured for superior humeral head migration. The angle formed by the line drawn along the long axis of the humerus (H) and the glenoid line (S) was measured to calculate the glenohumeral angle. The glenoid line (S) was compared with the vertical axis of the body (B) to calculate the scapulothoracic angle. A reference bar (R) with a known length (5 cm) was always included in radiographs to adjust for magnification differences.
Statistical Methods
Comparisons of the outcome variables between Visit 1 and Visit 2 (i.e., visits before and after pain development) within groups were performed with either paired t tests or Wilcoxon signed-rank tests depending on the normality of the data. Comparisons between the symptomatic and the asymptomatic group at the time of enrollment for continuous measurements were performed with either unpaired t tests or Mann-Whitney U tests depending on the normality of the data. Normality was examined with use of the Shapiro-Wilk and Kolmogorov-Smirnov tests with visual inspection of stem-and-leaf and normal probability plots. For categorical variables, comparisons between groups at a single time point were performed with chi-square or Fisher exact tests depending on the scarcity of the data. Changes in glenohumeral kinematics along different abduction angles were analyzed with mixed-model repeated-measures analysis of variance. When significant, and within the mixed model, statistical contrasts were used to assess the change between specific abduction angles. Significance was set at p ≤ 0.05. When appropriate, continuous variables were reported as the means and the standard deviations with 95% confidence intervals. Medians with 25th and 75th percentiles (interquartile range) were reported for variables whose distribution deviated from normal.
Intraclass correlation coefficients and 95% confidence intervals were calculated to indicate interobserver reliability of the radiographic variables for a subset of thirty-seven patients who were evaluated by the two independent observers. Fifteen outliers that were beyond the range of five standard deviations above or below the mean were identified in the measurements of the ratio of glenohumeral to scapulothoracic motion and were removed from the data analysis to avoid adverse effects of these data because the values were not clinically feasible. The mean of the two ratings was used for all subsequent analyses of these variables. Post hoc power analyses were determined with use of a power of 0.8 at an alpha of 0.05 for two-tailed unpaired and paired t tests. For rank-transformed data prior to analysis, Winsorized variances were used as robust variance estimates for power computations.
Source of Funding
This project was funded by a grant from the National Institutes of Health (R01 AR051026) as part of an ongoing prospective cohort study with a specific aim of describing the natural history of rotator cuff tears.
Results
Study Subject Demographics
Forty-four subjects with an asymptomatic rotator cuff became symptomatic. The mean age (and standard deviation) of the subjects at the time of study enrollment was 63.3 ± 11 years for the symptomatic group and 63.1 ± 9 years for the asymptomatic group. Thirty subjects (55%) in the asymptomatic group and twenty-nine (66%) in the symptomatic group were male. For the symptomatic group, shoulder pain developed at a mean of 1.93 ± 1.2 years (range, 0.4 to 4.4 years) after enrollment in the study. After excluding two subjects who were ambidextrous, twenty-four (56%) of the forty-three subjects of the symptomatic group had the asymptomatic tear in the dominant-side shoulder, while fourteen (26%) of the fifty-four subjects of the asymptomatic group had the asymptomatic tear in the dominant side (p < 0.01, chi-square test). When data regarding treatment of the contralateral symptomatic shoulder were analyzed, twenty-nine (53%) of the fifty-five subjects in the asymptomatic group and nineteen (43%) of the forty-four in the symptomatic group underwent surgery on the non-study, symptomatic shoulder prior to or after study enrollment (p = 0.34).
Few subjects (eleven in the asymptomatic group and eight in the symptomatic group) reported their work demands as sedentary as opposed to most (forty-four in the asymptomatic group and thirty-six in the symptomatic group) who described their work as manual labor or in between sedentary and manual labor. Most patients (thirty in the asymptomatic group and twenty-three in the symptomatic group) reported participating in some level of sport. The most commonly reported sports were golf, swimming, racquet sports, and weight lifting. The ninety-six subjects who were excluded from the present study were not substantially different from the ninety-nine subjects included in the study in terms of age, sex, tear type, and tear size.
Rotator Cuff Tear Progression
At the time of enrollment, ten (23%) of forty-four subjects in the symptomatic group had a partial-thickness rotator cuff tear and thirty-four subjects (77%) had a full-thickness tear. In the asymptomatic group, twenty (36%) of the fifty-five subjects had a partial-thickness tear and thirty-five (64%) had a full-thickness tear. The proportion of partial-thickness to full-thickness tears in the symptomatic group was not significantly different from that in the asymptomatic group (p = 0.14). When full-thickness tear size at the time of enrollment was compared, the symptomatic group had significantly greater tear width than the asymptomatic group (median, 13.5 mm and 10.0 mm, respectively; p = 0.02). However, there were no significant differences between the symptomatic and asymptomatic groups with regard to tear length (median, 12.5 mm and 11.0 mm, respectively; p = 0.34) and area (median, 182 mm2 and 109 mm2; p = 0.10). Post hoc power analyses demonstrated that the sample size available in this study could detect between-group differences as small as 5.7 mm for tear length and 153 mm2 for tear area. At Visit 2 for the symptomatic group, four of the ten subjects with a partial-thickness tear had progression to a full-thickness tear, and six (18%) of the thirty-four patients with a full-thickness tear had an increase in tear size of >5 mm. Thus, ten (23%) of the forty-four patients demonstrated substantial tear progression. The median length and width of the full-thickness tears at Visit 1 were 12.7 mm and 13.2 mm, respectively (Table I). At Visit 2, the tear size increased significantly, with a median length of 13.2 mm (p = 0.008) and a median width of 14.0 mm (p = 0.01). Likewise, the median area of the full-thickness tears also increased significantly from 158 mm2 at Visit 1 to 189 mm2 at Visit 2 (p = 0.006).
TABLE I.
Changes in Tear Size and Fatty Infiltration Between Visits in Shoulders with a Full-Thickness Tear
| Asymptomatic Group (N = 35) | Symptomatic Group (N = 34) | |||
| Variable | Median* (Interquartile Range) | P Value† | Median* (Interquartile Range) | P Value† |
| Tear length (mm) | 0.62 | 0.008 | ||
| Visit 1 | 11.0 (8.0-15.0) | 12.7 (8.0-28.0) | ||
| Visit 2 | 11.0 (9.0-18.0) | 13.2 (9.0-32.0) | ||
| Change | 0 (–1.0-1.0) | 1.0 (–1.0-3.0) | ||
| Tear width (mm) | 0.70 | 0.01 | ||
| Visit 1 | 10.0 (7.0-14.0) | 13.2 (9.0-22.0) | ||
| Visit 2 | 10.0 (8.0-16.0) | 14.0 (10.0-24.0) | ||
| Change | 0 (–1.0-1.0) | 1.0 (–1.0-4.0) | ||
| Tear area (mm2) | 0.86 | 0.006 | ||
| Visit 1 | 117 (63.0-210) | 158 (84.0-493) | ||
| Visit 2 | 126 (73.0-224) | 189 (96.0-504) | ||
| Change | 0 (–15.6-18.7) | 25.0 (–14.0-86.0) | ||
The 25th and 75th percentiles are in parentheses.
P value compares data between visits within the group (Wilcoxon signed-rank test).
At Visit 2 for the asymptomatic group, none of the twenty partial-thickness tears had progressed to a full-thickness tear and two of the thirty-five full-thickness tears demonstrated progression in size of >5 mm. Thus, only two (4%) of the fifty-five patients had substantial tear progression. The rate of tear progression in the asymptomatic group (4%) was significantly less than that of the symptomatic group (23%) (p < 0.01). Unlike the symptomatic group, the asymptomatic group showed no significant change in mean tear size between visits.
Of the sixty-nine full-thickness tears included in this study, twenty-seven were in the dominant shoulder and forty-two were in the nondominant shoulder. At the time of enrollment, the median tear width was 10 mm (range, 7 to 14 mm) in the nondominant shoulders and was significantly larger at 13 mm (range, 9 to 27 mm; p = 0.009) in the dominant shoulders. There was no difference in the median tear length between the nondominant shoulders (10 mm; range, 7 to 14 mm) and the dominant shoulders (16 mm; range, 8 to 27 mm; p = 0.06).
Fatty Degeneration of the Rotator Cuff Muscles
Because there was little variability in the fatty degeneration scores and there is currently no consensus regarding the minimal clinically important change for these scores, we elected to report these data without formal statistical analyses. None of the shoulders with a partial-thickness tear showed fatty degeneration of the supraspinatus at any time point, and only two shoulders showed fatty degeneration of the infraspinatus. All asymptomatic full-thickness tears showed no evidence of fatty infiltration in the supraspinatus muscle at the initial visit, while seven (21%) of the thirty-three symptomatic full-thickness tears had some evidence of fatty degeneration at the initial visit. However, 12% of both the asymptomatic and symptomatic full-thickness tears showed an increase in the fatty infiltration of the supraspinatus muscle from the time of the initial visit to Visit 2.
Ninety-six percent of the asymptomatic full-thickness tears and 82% of the symptomatic full-thickness tears had no evidence of fatty infiltration in the infraspinatus muscle at the initial visit. As was seen in the supraspinatus muscle in the two groups, there was a similar percentage of tears (15%) that had increased fatty infiltration in the infraspinatus muscle between the initial visit and Visit 2.
Shoulder Function
At the time of enrollment, there were no significant differences in shoulder function or physical examination findings between the symptomatic and asymptomatic groups, with the exception of increased internal rotation at 90° of abduction in the asymptomatic group (71.9° ± 19.0° compared with 63.9° ± 20.4° in the symptomatic group; p = 0.05) (Table II).
TABLE II.
Comparison of Variables Between Groups at the Time of Enrollment
| Variable | Asymptomatic Group (N = 55) | Symptomatic Group (N = 44) | P Value* |
| Cuff tear length†‡(mm) | 11.0 (8.0-15.0) | 12.5 (8.0-26.0) | 0.34§ |
| Cuff tear width†‡(mm) | 10.0 (7.0-12.0) | 13.5 (8.4-19.0) | 0.02§ |
| Cuff tear area†‡(mm2) | 109 (64.0-187) | 182 (70.0-496) | 0.10§ |
| Pain score on visual analog scale‡(points) | 1.00 (1.00-1.00) | 1.00 (1.00-1.00) | 0.85§ |
| ASES score‡#(points) | 97.5 (93.3-100) | 96.7 (90.0-100) | 0.35§ |
| External rotation strength**(N) | 63.3 ± 25.5 (56.4-70.2) | 65.5 ± 33.2 (55.4-75.6) | 0.71 |
| Forward elevation‡(deg) | 160 (150-170) | 160 (155-170) | 0.67§ |
| External rotation at 90° abduction**(deg) | 91.1 ± 11.0 (88.1-94.1) | 89.9 ± 12.5 (86.1-93.7) | 0.61 |
| Internal rotation at 90° abduction**(deg) | 71.9 ± 19.0 (66.7-77.0) | 63.9 ± 20.4 (57.6-70.1) | 0.05 |
| External rotation at side#**(deg) | 70.8 ± 16.3 (66.4-75.2) | 75.8 ± 19.7 (69.8-81.8) | 0.17 |
| Internal rotation in extension‡ | 2.00 (2.00-3.00) | 3.00 (2.00-3.00) | 0.17§ |
| SF-36 physical health summary score#** | 43.5 ± 10.5 (40.6-46.4) | 43.4 ± 9.7 (40.5-46.4) | 0.98 |
| SF-36 mental health summary score#** | 52.1 ± 3.7 (51.1-53.1) | 50.8 ± 5.3 (49.2-52.4) | 0.16 |
P value derived from an unpaired t test, unless otherwise specified.
Tear size was compared only for full-thickness tears of both groups (thirty-five shoulders in the asymptomatic group and thirty-four in the symptomatic group).
The values are given as the median, with the interquartile range in parentheses.
ASES = American Shoulder and Elbow Surgeons, and SF-36 = Short Form-36.
Mann-Whitney U test.
The values are given as the mean and the standard deviation, with the 95% confidence interval in parentheses.
In the symptomatic group, the median pain score on the visual analog scale increased significantly from 1.0 at Visit 1 to 4.0 at Visit 2 (p < 0.0001) (Table III). The median ASES score decreased significantly from 93.3 points at Visit 1 to 65.8 points at Visit 2 (p < 0.0001). Isometric external rotation strength was not significantly different between visits (p = 0.37). All shoulder range-of-motion values decreased significantly at Visit 2 (p < 0.05), with the exception of external rotation at 90° of abduction (p = 0.11) (Table III). The SF-36 scores did not change significantly between visits (p = 0.41 for physical, and p = 0.56 for mental health summary scores). Post hoc power analyses demonstrated a power of 0.80 to detect differences of 11.6 N and 8.6° of external rotation at 90° of abduction. No data on minimal clinically important differences are known for these two measures of shoulder function. However, post hoc power analyses demonstrated this study could detect differences of 4.2 for the physical and 1.6 for the mental component of the SF-36, indicating the sample size was large enough to detect a clinically relevant difference14.
TABLE III.
Changes in Shoulder Function Between Visits
| Variable | Asymptomatic Group (N = 55) | Symptomatic Group (N = 44) | ||
| Result | P Value* | Result | P Value* | |
| Pain score on visual analog scale†(points) | 0.48‡ | <0.0001‡ | ||
| Visit 1 | 1.0 (1.0 to 2.0) | 1.0 (1.0 to 1.5) | ||
| Visit 2 | 1.0 (1.0 to 2.0) | 4.0 (3.0 to 6.0) | ||
| Change | 0 (0 to 0) | 3.0 (2.0 to 5.0) | ||
| ASES score†(points) | 0.83‡ | <0.0001 | ||
| Visit 1 | 95.0 (83.3 to 100) | 93.3 (85.0 to 100) | ||
| Visit 2 | 95.0 (84.4 to 100) | 65.8 (49.0 to 77.5) | ||
| Change | 0 (–5.0 to 5.0) | –27.5 (–35.8 to –18.0) | ||
| External rotation strength§(N) | 0.41 | 0.37 | ||
| Visit 1 | 64.6 ± 28.0 (56.9 to 72.3) | 61.8 ± 30.3 (52.3 to 71.2) | ||
| Visit 2 | 62.7 ± 27.4 (55.2 to 70.3) | 58.0 ± 32.5 (47.9 to 68.2) | ||
| Change | –1.9 ± 16.4 (–6.4 to 2.6) | –3.8 ± 26.9 (–12.1 to 4.6) | ||
| Forward elevation§(deg) | 0.004 | <0.0001‡ | ||
| Visit 1 | 153 ± 12.6 (150 to 156) | 160 (145 to 160) | ||
| Visit 2 | 146 ± 13.6 (142 to 150) | 150 (140 to 150) | ||
| Change | –6.9 ± 16.7 (–11.4 to –2.3) | –10.0 (–20.0 to 0) | ||
| External rotation at 90° of abduction§(deg) | 0.15 | 0.11 | ||
| Visit 1 | 90.1 ± 11.7 (86.9 to 93.2) | 86.6 ± 14.1 (82.2 to 90.9) | ||
| Visit 2 | 86.8 ± 12.9 (83.3 to 90.3) | 81.4 ± 14.5 (76.9 to 85.9) | ||
| Change | –3.3 ± 16.5 (–7.7 to 1.2) | –5.1 ± 20.1 (–11.4 to 1.1) | ||
| Internal rotation at 90° of abduction§(deg) | 0.20 | 0.02 | ||
| Visit 1 | 66.6 ± 19.3 (61.3 to 71.8) | 66.6 ± 17.7 (61.2 to 72.1) | ||
| Visit 2 | 69.6 ± 11.9 (66.3 to 72.8) | 58.4 ± 16.8 (53.2 to 63.5) | ||
| Change | 3.0 ± 17.1 (–1.6 to 7.6) | –8.3 ± 22.8 (–15.3 to –1.2) | ||
| External rotation at side§(deg) | 0.07 | 0.03 | ||
| Visit 1 | 70.3 ± 15.9 (66.0 to 74.6) | 68.7 ± 21.1 (62.2 to 75.2) | ||
| Visit 2 | 64.7 ± 14.7 (60.8 to 68.7) | 60.6 ± 14.4 (56.1 to 65.0) | ||
| Change | –5.6 ± 22.2 (–11.5 to 0.4) | –8.1 ± 24.3 (–15.6 to –0.7) | ||
| Internal rotation in extension† | 0.001‡ | 0.002‡ | ||
| Visit 1 | 3.0 (2.0 to 3.0) | 3.0 (2.0 to 3.0) | ||
| Visit 2 | 3.0 (2.0 to 3.0) | 3.0 (3.0 to 4.0) | ||
| Change | 0 (0 to 1.0) | 1.0 (0 to 1.0) | ||
| SF-36 physical health summary score§(points) | 0.05 | 0.41 | ||
| Visit 1 | 45.6 ± 9.7 (43.0 to 48.3) | 43.7 ± 10.3 (40.6 to 46.9) | ||
| Visit 2 | 47.6 ± 8.9 (45.1 to 50.0) | 42.5 ± 8.3 (40.0 to 45.1) | ||
| Change | 2.0 ± 7.1 (0 to 3.9) | –1.2 ± 9.7 (–4.1 to 1.7) | ||
| SF-36 mental health summary score§(points) | 0.08 | 0.56 | ||
| Visit 1 | 53.0 ± 3.8 (52.0 to 54.0) | 50.9 ± 4.9 (49.4 to 52.4) | ||
| Visit 2 | 52.1 ± 4.3 (50.9 to 53.3) | 50.5 ± 4.9 (49.1 to 52.0) | ||
| Change | –0.9 ± 3.7 (–1.9 to 0.1) | –0.3 ± 3.8 (–1.5 to 0.8) | ||
P value, derived with the paired t test, for the comparison of data between visits within the group.
The values are shown as the median with the interquartile range in parentheses.
Wilcoxon signed-rank test.
Data are shown as the mean and the standard deviation, with the 95% confidence interval in parentheses.
In the asymptomatic group, there were no significant changes in the median pain score on the visual analog scale, median ASES score, or mean external rotation strength between visits (p = 0.48, 0.83, and 0.41, respectively; Table III). The mean range of forward elevation showed a significant decrease (–6.9° ± 16.7°; p = 0.004) at Visit 2. The median internal rotation in extension decreased significantly at Visit 2 (p = 0.001). Unlike the symptomatic group, the mean internal rotation at 90° of abduction and mean external rotation at the side did not change significantly between visits in this group (p = 0.20 and 0.07, respectively). The mean SF-36 physical health summary score showed a significant increase at Visit 2 (47.6 ± 8.9) compared with Visit 1 (45.6 ± 9.7; p = 0.05), but this change did not reach the suggested minimal clinically important difference of this dimension (3 to 5 points)14. The mean mental health summary score did not show any significant change between visits. Post hoc power analyses demonstrated an ability to detect differences of 6.3 N of external rotation strength and 6.4° of external rotation at 90° of abduction. Further analyses revealed enough power to detect differences of 2.7 and 1.4 for the physical and mental components, respectively, of the SF-36, again indicating adequate power to detect clinically important differences.
Glenohumeral Kinematics
The interobserver reliability between the two authors measuring the glenohumeral kinematics was excellent. The intraclass correlation coefficient was 0.75 (95% confidence interval, 0.69 to 0.80) for the position of the humeral head center, 0.98 (95% confidence interval, 0.98 to 0.99) for the scapulothoracic angle, and 0.99 (95% confidence interval, 0.99 to 0.99) for the glenohumeral angle.
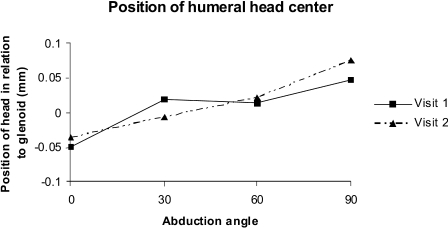
In the symptomatic group, the humeral head center migrated superiorly with an increasing shoulder abduction angle regardless of the presence of pain (p = 0.04 for Visit 1 and 0.03 for Visit 2, respectively) (Fig. 2). However, between Visit 1 and Visit 2, no significant change was detected in the humeral head position (p ≥ 0.20) or the amount of humeral head migration with increasing shoulder abduction (p = 0.73). Similarly, the glenohumeral angle and scapulothoracic angle were not significantly different between visits at any of the abduction angles (p > 0.05). Before pain development (at Visit 1), the ratio of glenohumeral to scapulothoracic motion was greatest during abduction from 0° to 30° (median ratio, 4.2), which was significantly greater than the ratios of other abduction segments (p = 0.008) (Table IV). However, after pain development (at Visit 2), the motion ratio during abduction from 0° to 30° was a median (and interquartile range) of 2.5 (1.5 to 6.4), which was not significantly different from the ratios of other abduction segments (p = 0.20 for overall analysis of variance). When the ratios were compared for each abduction segment, no significant differences were seen between visits (p > 0.10).
Fig. 2.
The position of the humeral head in relation to the glenoid showed a gradual superior translation with shoulder abduction at both Visit 1 and Visit 2. However, there were no significant differences between visits at any of the abduction angles.
TABLE IV.
Ratio of Glenohumeral to Scapulothoracic Motion During Abduction in the Symptomatic Group
| Abduction Angle | Visit 1 | Visit 2 | P Value‡ | ||
| Median* (Interquartile Range) | P Value† | Median* (Interquartile Range) | P Value† | ||
| 0° to 30° | 4.2 (1.8-6.8) | 0.008§ | 2.5 (1.5-6.4) | 0.20 | 0.13 |
| 30° to 60° | 2.2 (1.2-3.8) | 1.4 (0.6-4.7) | 0.38 | ||
| 60° to 90° | 2.0 (1.4-2.8) | 2.1 (1.1-3.2) | 0.23 | ||
| 0° to 90° | 2.6 (1.7-4.0) | 2.4 (1.9-3.8) | 0.94 | ||
The 25th and 75th percentiles are given in parentheses.
P value for comparison of the values between different abduction segments within a visit is derived by mixed-model repeated-measures analysis of variance using rank-transformed data.
P value, derived with the Wilcoxon signed-rank test, for the comparison of certain abduction segments between visits.
Post hoc analysis of this comparison by statistical contrasts showed p = 0.02 for 0° to 30° versus 30° to 60°, p = 0.001 for 0° to 30° versus 60° to 90°, p = 0.09 for 0° to 30° versus 0° to 90°, p = 0.41 for 30° to 60° versus 30° to 90°, and p = 0.38 for 30° to 60° versus 0° to 90°.
Discussion
This study demonstrates that a substantial proportion of subjects with asymptomatic rotator cuff tears become symptomatic after a short-term follow-up period. Pain development in asymptomatic rotator cuff tears is associated with tear size progression. Collectively, the subjects who developed new shoulder pain showed significant tear size increases compared with baseline measurements, whereas those who remained asymptomatic had no significant change in tear size. Likewise, the rate of tear progression, as defined in this study, for the symptomatic group (23%) was significantly greater than the rate for the asymptomatic group (4%). Tear progression manifested as both enlargement of full-thickness tears as well as conversion of partial-thickness to full-thickness tendon defects. The lack of tear progression seen in the majority of newly symptomatic tears, however, suggests that factors other than tear progression likely play a role in the evolution of symptoms for these patients. Given the high prevalence of asymptomatic rotator cuff disease, especially in individuals older than sixty years or in patients with a painful rotator cuff tear in the contralateral shoulder, these findings are clinically relevant. The onset of shoulder pain in a patient with a known preexisting asymptomatic tear may indicate an increase in tear size, which would potentially affect the clinical management of these patients.
Compared with the group of subjects who remained asymptomatic, the subjects who developed pain were found to have significantly larger tears at the time of enrollment. This suggests that the absolute size of an asymptomatic tear may be a predictor of future pain development. Previously, we reported the average size of symptomatic tears to be 30% larger than that of asymptomatic tears15. There may be a cuff tear size threshold that predisposes a subject to future pain development, irrespective of tear progression. Future studies are necessary to define the relationship of absolute tear size and tear progression with pain development in the shoulders with an asymptomatic rotator cuff tear. In addition, a significant difference in predilection toward hand dominance was seen between the shoulders that developed pain (56% were on the dominant side) and those that remained asymptomatic (26% were on the dominant side). This may be explained by the finding that the dominant-side shoulders initially had larger tears than the nondominant shoulders. It is also possible that hand dominance, irrespective of tear size, predisposes a shoulder with an asymptomatic tear to develop symptoms.
This study demonstrates that shoulder function deteriorates as asymptomatic rotator cuff tears became painful. The ASES score decreased by a median of 28 points in the shoulders that became symptomatic, whereas no significant changes were observed in ASES scores in the shoulders that remained asymptomatic. All measures of active range of motion of the shoulder, with the exception of external rotation at 90° of abduction, decreased significantly after pain development. Interestingly, the subjects who remained asymptomatic also showed a decrease in forward elevation and internal rotation in extension. These findings suggest that progressive loss of range of motion of the shoulder may be a consequence of the presence of a rotator cuff tear, regardless of the presence of symptoms. The declines in active range of motion seen in this study were small at this short-term time point and would be difficult to appreciate clinically. Furthermore, the differences seen between symptomatic and asymptomatic shoulders were not clinically important. Further studies are needed to determine if this loss of shoulder motion progresses over time and if specific strategies can prevent or correct the functional changes in this patient cohort. Contrary to our expectations, SF-36 scores did not decrease after shoulder pain development, which may be due to a lack of sensitivity of this general health assessment tool to detect early declines in shoulder function.
External rotation strength of the shoulder was not significantly affected by new pain development. This can be explained by the fact that the tears included in this study were relatively small in size. These tears primarily involved the supraspinatus tendon, whereas the majority of the infraspinatus tendon was preserved, thus minimizing external rotation weakness. Furthermore, degenerative changes within the rotator cuff musculature were minimal, likely preserving cuff strength. It is possible that scapular plane abduction strength may have been a more sensitive test for the detection of disease progression in these subjects as this test is more sensitive to detect supraspinatus tears and has been previously correlated to the size of asymptomatic rotator cuff tears16,17.
This study demonstrates that pain development in asymptomatic rotator cuff tears is not associated with progression of fatty degeneration of the rotator cuff muscles. This may be explained by the relatively short time period (one year) between the evaluation time points and the relatively small size of the tears included in this study. Nonetheless, it is notable that progressive fatty degeneration is not associated with pain development or tear enlargement in previously asymptomatic rotator cuff tears.
Glenohumeral kinematics have been shown to change in patients with symptomatic rotator cuff tears11,13,18-21, but little is known regarding the effect of pain on these kinematics. In our study, the glenohumeral kinematics did not change significantly with pain development except for a tendency for increased compensatory scapulothoracic motion during early abduction after pain development. The lack of proximal humeral migration may be explained by the fact that the time period between pain development and examination was short (less than one year) and the majority of the tears in this study were relatively small. Changes in glenohumeral kinematics are most likely to occur in advanced stages of rotator cuff tears. Other studies have shown that normal glenohumeral kinematics can be maintained in the presence of a rotator cuff tear if the rotator cuff force couple remains intact and that disruption of the infraspinatus is necessary to affect kinematics21,22.
There are several limitations of this study that warrant discussion. Given that this is an early report of an ongoing longitudinal cohort study, only a subset of subjects who had developed pain at the time of this analysis were included. The comparison group was chosen to mirror the follow-up of the painful shoulders and comprised subjects who had been in the study two years or longer. A longer duration of follow-up is necessary and will enable us to further characterize the risk of symptom progression over time. Nonetheless, we believe reporting preliminary results at this point to be reasonable for a few reasons. First, although new pain would be discovered in more subjects after a longer duration of follow-up, early follow-up evaluation detected the development of pain in forty-four subjects, which was a clinically important number. Second, this preliminary report can serve as a mid-term examination of the ongoing prospective study. Lessons learned from this early analysis can prevent errors with future reports and enable fine-tuning of the study design. Third, the findings observed in this preliminary report could guide a more focused research effort for identification of factors associated with pain development. Most notably, despite the use of short-term data, the present study produced both clinically important and statistically significant results with direct clinical applicability.
Our study subjects included those with a painful rotator cuff tear in the contralateral shoulder. The subjects in this series may differ in natural history from those without painful rotator cuff disease in the contralateral shoulder. Also, the chronicity of the cuff tears in this study cohort is unknown. It is possible that unknown differences in disease duration may have affected the onset of symptoms. We anticipate these differences would be minimal, given the similar ages of the groups, but this remains unknown. The assessment of glenohumeral kinematics in this study included only a two-dimensional analysis of shoulder function and may not have detected potential three-dimensional alterations in kinematics. In addition, as only external rotation strength was measured in the present study, subtle potential changes in rotator cuff strength in the setting of relatively small tears may not have been detected. It would have been more informative to also include abduction strength measures. The accuracy of ultrasound estimation of fatty degeneration of the rotator cuff muscles has yet to be validated in our institution. However, two previous studies8,23 that investigated the accuracy of ultrasonography for fatty muscular degeneration concluded that ultrasonography had excellent accuracy in detecting the presence of fatty degeneration. In addition, the sonographic grading of fatty degeneration has been found to correlate well with magnetic resonance imaging24-26. Although the radiologists were blinded to the history and symptomatology of the subjects, they were not blinded to the results of the previous sonography, which may have introduced bias to the interpretation of sonographic findings.
In summary, the risk of symptom progression for asymptomatic rotator cuff tears after a short-term follow-up interval is substantial. In this study, shoulders that developed pain had significantly larger tears at baseline and demonstrated a higher rate of tear progression than those that remained asymptomatic. Shoulder function and active range of motion deteriorated with symptom onset; however, no significant changes were found in external rotation strength or fatty degeneration of the rotator cuff muscles after pain development. There was an increase of compensatory scapulothoracic motion during early shoulder abduction after pain development; however, no increase in proximal humeral migration was seen.
Supplementary Material
Footnotes
Disclosure: In support of their research for or preparation of this work, one or more of the authors received, in any one year, outside funding or grants in excess of $10,000 from the National Institutes of Health (R01 AR051026-01A1). In addition, one or more of the authors or a member of his or her immediate family received, in any one year, payments or other benefits in excess of $10,000 or a commitment or agreement to provide such benefits from commercial entities (Zimmer and Tornier).
References
- 1.Milgrom C, Schaffler M, Gilbert S, van Holsbeeck M. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J Bone Joint Surg Br. 1995;77:296-8 [PubMed] [Google Scholar]
- 2.Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77:10-5 [DOI] [PubMed] [Google Scholar]
- 3.Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10:199-203 [DOI] [PubMed] [Google Scholar]
- 4.Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am. 2000;82:498-504 [PubMed] [Google Scholar]
- 5.Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86:708-16 [PubMed] [Google Scholar]
- 6.de Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol. 2009;192:1701-7 [DOI] [PubMed] [Google Scholar]
- 7.Vlychou M, Dailiana Z, Fotiadou A, Papanagiotou M, Fezoulidis IV, Malizos K. Symptomatic partial rotator cuff tears: diagnostic performance of ultrasound and magnetic resonance imaging with surgical correlation. Acta Radiol. 2009;50:101-5 [DOI] [PubMed] [Google Scholar]
- 8.Strobel K, Hodler J, Meyer DC, Pfirrmann CW, Pirkl C, Zanetti M. Fatty atrophy of supraspinatus and infraspinatus muscles: accuracy of US. Radiology. 2005;237:584-9 [DOI] [PubMed] [Google Scholar]
- 9.Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11:587-94 [DOI] [PubMed] [Google Scholar]
- 10.Tarlov AR, Ware JE, Jr, Greenfield S, Nelson EC, Perrin E, Zubkoff M. The Medical Outcomes Study. An application of methods for monitoring the results of medical care. JAMA. 1989;262:925-30 [DOI] [PubMed] [Google Scholar]
- 11.Yamaguchi K, Sher JS, Andersen WK, Garretson R, Uribe JW, Hechtman K, Neviaser RJ. Glenohumeral motion in patients with rotator cuff tears: a comparison of asymptomatic and symptomatic shoulders. J Shoulder Elbow Surg. 2000;9:6-11 [DOI] [PubMed] [Google Scholar]
- 12.Keener JD, Wei AS, Kim HM, Steger-May K, Yamaguchi K. Proximal humeral migration in shoulders with symptomatic and asymptomatic rotator cuff tears. J Bone Joint Surg Am. 2009;91:1405-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poppen NK, Walker PS. Normal and abnormal motion of the shoulder. J Bone Joint Surg Am. 1976;58:195-201 [PubMed] [Google Scholar]
- 14.Hays RD, Morales LS. The RAND-36 measure of health-related quality of life. Ann Med. 2001;33:350-7 [DOI] [PubMed] [Google Scholar]
- 15.Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88:1699-704 [DOI] [PubMed] [Google Scholar]
- 16.Itoi E, Minagawa H, Yamamoto N, Seki N, Abe H. Are pain location and physical examinations useful in locating a tear site of the rotator cuff? Am J Sports Med. 2006;34:256-64 [DOI] [PubMed] [Google Scholar]
- 17.Kim HM, Teefey SA, Zelig A, Galatz LM, Keener JD, Yamaguchi K. Shoulder strength in asymptomatic individuals with intact compared with torn rotator cuffs. J Bone Joint Surg Am. 2009;91:289-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burkhart SS. Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears. A suspension bridge model. Clin Orthop Relat Res. 1992;284:144-52 [PubMed] [Google Scholar]
- 19.Deutsch A, Altchek DW, Schwartz E, Otis JC, Warren RF. Radiologic measurement of superior displacement of the humeral head in the impingement syndrome. J Shoulder Elbow Surg. 1996;5:186-93 [DOI] [PubMed] [Google Scholar]
- 20.Paletta GA, Jr, Warner JJ, Warren RF, Deutsch A, Altchek DW. Shoulder kinematics with two-plane x-ray evaluation in patients with anterior instability or rotator cuff tearing. J Shoulder Elbow Surg. 1997;6:516-27 [DOI] [PubMed] [Google Scholar]
- 21.Thompson WO, Debski RE, Boardman ND, 3rd, Taskiran E, Warner JJ, Fu FH, Woo SL. A biomechanical analysis of rotator cuff deficiency in a cadaveric model. Am J Sports Med. 1996;24:286-92 [DOI] [PubMed] [Google Scholar]
- 22.Mura N, O'Driscoll SW, Zobitz ME, Heers G, Jenkyn TR, Chou SM, Halder AM, An KN. The effect of infraspinatus disruption on glenohumeral torque and superior migration of the humeral head: a biomechanical study. J Shoulder Elbow Surg. 2003;12:179-84 [DOI] [PubMed] [Google Scholar]
- 23.Khoury V, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscle: sonography versus MRI. AJR Am J Roentgenol. 2008;190:1105-11 [DOI] [PubMed] [Google Scholar]
- 24.Dinnes J, Loveman E, McIntyre L, Waugh N. The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review. Health Technol Assess. 2003;7: iii, 1-166 [DOI] [PubMed] [Google Scholar]
- 25.Frei R, Chládek P, Trc T, Kopecný Z, Kautzner J. Arthroscopic evaluation of ultrasonography and magnetic resonance imaging for diagnosis of rotator cuff tear. Ortop Traumatol Rehabil. 2008;10:111-4 [PubMed] [Google Scholar]
- 26.Shahabpour M, Kichouh M, Laridon E, Gielen JL, De Mey J. The effectiveness of diagnostic imaging methods for the assessment of soft tissue and articular disorders of the shoulder and elbow. Eur J Radiol. 2008;65:194-200 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.