Abstract
Are brief cognitive-behavioral treatments for posttraumatic stress disorder (PTSD) also effective for the wider range of symptoms conceptualized as complex PTSD? Female rape victims, most of whom had extensive histories of trauma, were randomly assigned to cognitive-processing therapy, prolonged exposure, or a delayed-treatment waiting-list condition. After determining that both types of treatment were equally effective for treating complex PTSD symptoms, we divided the sample of 121 participants into two groups depending upon whether they had a history of child sexual abuse. Both groups improved significantly over the course of treatment with regard to PTSD, depression, and the symptoms of complex PTSD as measured by the Trauma Symptom Inventory. Improvements were maintained for at least 9 months. Although there were group main effects on the Self and Trauma factors, there were no differences between the two groups at posttreatment once pretreatment scores were covaried. These findings indicate that cognitive-behavioral therapies are effective for patients with complex trauma histories and symptoms patterns.
INTRODUCTION
Among the varieties of traumatic stressors that have been implicated in the development of psychopathology, sexual assault is the event most likely to result in posttraumatic stress disorder (PTSD).1,2 A large retrospective epidemiology study of women indicated that 13% of women reported a completed rape while another 14% reported attempted rape or molestation.2 Among those victimized by rape, 32% experienced PTSD at some point, as did 31% of the attempted rape victims. Numerous studies have documented previous incidents of both childhood and adult sexual assault among rape survivors.3–8 A previous history of interpersonal victimization has been shown to be the single best predictor of subsequent victimization.9–11 The combined effect of prior victimization has been shown to predict lasting pathology in female survivors of interpersonal assault.7
Specifically, childhood trauma has been shown to increase the risk for a variety of psychiatric disorders, including borderline personality disorder,12,13 somatization disorder,14 dissociative disorders,15,16 self-mutilation,17 eating disorders,18 and substance use disorders.19 While women reporting prior trauma histories are also more likely to meet symptom criteria for PTSD,7,20–22 it has been suggested that the current diagnostic formulation of PTSD23 fails to capture the more complex, diffuse, and tenacious symptom picture associated with a history of prolonged, repeated childhood trauma.24
The term “complex PTSD”24 has been proposed to capture this more complicated symptom picture associated with a history of childhood interpersonal trauma. The symptoms comprising complex PTSD have been clustered into five main categories24 and proposed as criteria for Disorders of Extreme Stress-Not Otherwise Specified. The five symptom categories include: (1) alterations in regulating affective arousal; (2) alterations in attention and consciousness; (3) somatization; (4) chronic characterologic changes; and (5) alterations in systems of meaning. These Disorders of Extreme Stress-Not Otherwise Specified criteria have been incorporated in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, under the section of “Associated Features and Disorders.”23
Treatment-outcome research with female rape victims has largely involved the use of controlled and comparative trials of cognitive-behavioral therapy (CBT), which have been found to be highly successful in treatment of PTSD and depression symptoms in a relatively short period of time (6–12 sessions). Two of the more researched treatments used with this population are prolonged-exposure therapy25,26 and cognitive-processing therapy (CPT).27,28 Prolonged exposure is an exposure-based therapy that includes both imaginal and in vivo exposures. After an education phase and breathing retraining, the therapist and client develop a hierarchy of feared situations, on which the client begins to practice at home. In session, the therapist has the client spend 45–60 minutes each session conducting imaginal exposures to the worst traumatic memory, in first-person present tense. CPT also has an exposure component, in this case a written account of the most traumatic event(s), but the majority of therapy is spent analyzing the meaning of the event(s) for the client and training the client to challenge distorted or over-generalized beliefs about the event, self and world. The method of challenging is through Socratic questioning and the use of a sequence of worksheets.
Clinical trials conducted with these therapies have established the initial efficacy for both these treatments. Resick and colleagues29 reported on a clinical trial comparing prolonged exposure and CPT with a minimal attention delayed treatment control group. While both therapies proved to be superior to the delayed-treatment group, there were no differences between prolonged exposure and CPT on either PTSD or depression symptom outcome measures. The only difference was for greater improvement among the CPT participants in specific guilt cognitions.
However, it is not entirely clear whether these CBT protocols are also efficacious in treating the range of symptoms that are associated with PTSD in female rape victims with a prior childhood victimization history. Retrospective studies of rape survivors have documented a clear relationship between early victimization history, increased post-rape pathology, and prolonged or compromised recovery. 30–33 Cloitre and colleagues34 recently reported on the outcome of a CBT trial that compared a combination of skills training in affective and interpersonal regulation with imaginal exposure to a waiting-list control condition. The therapy consisted of 16 sessions and, aside from PTSD and depression, a range of complex trauma symptoms, such as affect regulation and interpersonal impairment were assessed. This CBT treatment was very successful in reducing all of the symptoms assessed. However, the results are somewhat limited because the researchers excluded women who met the criteria for eating disorders, dissociative disorders, bipolar disorder, or borderline personality disorder.
The purpose of the present study, was to conduct further analyses on the data from the Resick and colleagues29 studyto compare rape victims with a child sexual abuse history to those women who were raped but had no child sexual abuse history on PTSD symptoms, depression symptoms, and on indicators of more complex symptoms of trauma response, such as dissociation, impaired self-reference, and tension reduction behaviors before and after cognitive behavioral treatments. The exclusion criteria were limited to methodologic considerations, such as recent trauma for chronicity or ability to give informed consent, or for current risk for which immediate intervention would be required (current self-harm behaviors or intent; current violence). Women were not excluded if they had other comorbid Axis I or Axis II disorders in addition to their PTSD.
Participants
Exclusion criteria from the clinical trial included current psychosis, suicidal intent, parasuicidal behavior, dependence upon drugs or alcohol, or illiteracy. In addition, participants could not be in a currently abusive relationship or being stalked. Participants were included if they had experienced at least one completed rape, were at least 3-months posttrauma (no upper limit), and if on medication, were stabilized. Women with prior substance dependence were included if/when they had been off of the substance(s) for 6 months. Those with current substance abuse were permitted to participate if they agreed and were deemed able to desist in usage during the period of treatment. Participants were only included in the trial if they met full criteria for PTSD. Participants were not excluded if they had previously received diagnoses of psychosis, bipolar disorder, dissociative disorders, or any other Axis I or Axis II disorder as long as they were not currently engaging in the self-harm behaviors previously listed and were not at active risk from others.
Two hundred sixty-seven women were assessed for possible participation. The most common reason for exclusion from the study (n=74) was not meeting the criteria for PTSD (74%). There were 121 women who completed all sessions of treatment plus at least the posttreatment assessment: 41 CPT clients, 40 prolonged-exposure patientss, and 40 wait-list control patients. Dropout rates for the two active-treatment groups were similar at 26.8% for CPT and 27.3% for prolonged exposure. In the delayed-treatment condition, 14.9% did not return for the second assessment. There were no significant differences between women who dropped out of therapy and those who completed with regard to their initial PTSD or depression scores. A χ2 indicated that there were no differences between the two treatment groups with regard to child sexual abuse dropout status. The wait-list participants who were then randomized and completed one of the two treatments were folded into the primary CPT and prolonged-exposure groups.
In the original sample of 171 women randomized into the trial, there were no significant differences in demographics between the three groups. Overall, on average, the women were 32 years of age (SD=9.9), and had 14.3 years of education (SD=2.6). The majority of the women were never married, divorced, or separated (75.7%). The sample was 71% white, 25% African American, and 4% were from other racial groups. The average length of time since the rape was 8.5 years (SD=8.5 years) with a range from 3 months to 33 years. Eighty-six percent of the sample had experienced at least one other major traumatic crime experience in addition to the index rape, and 41% of the sample reported a history of child sexual abuse. The samples sizes for the child sexual abuse status comparisons were 74 non-child sexual abuse and 47 child sexual abuse participants for the Clinician-Administered PTSD Scale35,36 (CAPS) and Beck Depression Inventory (BDI)37,38 and 71 and 43, respectively, for the analyses on the Trauma Symptom Inventory (TSI).39
Instruments
Clinician-Administered PTSD Scale
The CAPS is an interviewer-administered diagnostic interview that measures PTSD and has been found to have excellent psychometric properties.
Beck Depression Inventory
The BDI is a 21-item self-report questionnaire, widely used in research on depression. It has also been used to assess depression in rape victims.25,26,27,29
Standardized Trauma Interview
The standardized trauma interview was adapted from a previous treatment study by Resick and colleagues40 The structured interview covered the following topics: demographic information, information about the rape, within-crime reactions, trauma history, social support, and treatment history. Only the demographics and trauma history sections were included in this paper. In addition to questions about adult crimes and other traumas, child sexual abuse was assessed with the Sexual Abuse Exposure Questionnaire (Part I): (SAEQ)41 incorporated into the interview. The SAEQ (Part I) is a 10-item self-report measure designed to assess sexual acts experienced before 16 years of age. The interview also includes the Assessing Environments-III-Physical Punishment Scale (AE-III-PP).41 The AE-III-PP consists of 12 behaviorally anchored true/false items designed to assess a range of childhood physical discipline events from mild forms of physical discipline (eg, spanking) to potentially injurious physical events identified in the literature as common forms of abusive parenting. The AE-III-PP scale has been shown to successfully discriminate between abused and nonabused individuals. A score of 4 or higher on this scale suggests a history of childhood physical abuse.42
Trauma Symptom Inventory
The TSI is a 100-item self-report measure developed to assess both short-term and long-term sequelae of traumatic experiences. It contains nine clinical scales: Anxious Arousal, Anger-Irritability, Depression, Defensive Avoidance, Dissociation, Dysfunctional Sexual Behavior, Intrusive Experiences, Impaired Self-Reference, and Sexual Concerns. It is intended for use in the evaluation of, not only symptoms typically associated with PTSD and Acute Stress Disorder (ASD) but also those intra- and interpersonal difficulties often associated with more chronic psychological trauma that are subsumed under Disorders of Extreme Stress-Not Otherwise Specified. While the subscales of the TSI do not reflect the exact criteria of the hypothesized Disorders of Extreme Stress-Not Otherwise Specified/complex PTSD disorder, they do reflect many of the more complex sequellae of the trauma response beyond simple PTSD.
The TSI exhibits convergent, predictive, and incremental validity in both clinical and nonclinical samples. Factor analyses39 have established that there are three factors: the Dysphoria factor consisting of depression, anger-irritability, and anxious arousal; the Trauma factor, consisting of Intrusive Experiences, Defensive Avoidance, Dissociation, and Impaired Self-Reference; and the Self factor, consisting of Sexual Concerns, Dysfunctional Sexual Behavior, and Tension Reduction Behavior.
METHODS
Both CPT and prolonged exposure consisted of 13 hours of therapy configured across 12 and 9 sessions, respectively. Sessions were conducted twice weekly. CPT consists of systematic cognitive therapy, including daily homework and two sessions of exposure by means of a written account of the worst rape, which is read to the therapist and read daily as homework.28 Prolonged exposure consists of daily behavioral exposures at home, verbal imaginal exposure of the worst rape with the therapist, and listening to therapy tapes at home.43 Therapists were trained by the developers of each of the therapies25–28 and were supervised throughout the study. Adherence and competence ratings were conducted by experts in each therapy who were not associated with the study. Details regarding these fidelity ratings can be found in the parent study publication.29
This project was reviewed and approved by the institutional review board of the University of Missouri–St. Louis and all participants provided written informed consent. Participants were assessed at pretreatment, posttreatment, 3-months, and 9-months posttreatment. Because of the length of the battery, the TSI was dropped from the 3-month follow-up. However, if someone was missing her 9-month assessment, and happened to have a 3-month assessment, their data were carried forward for the 9-month analyses.
RESULTS
First, a power analysis was conducted to determine whether the sample size of 114 was sufficient to detect differences on the TSI.44 If one hypothesizes that rape victims with a child sexual abuse history will not respond to treatment as well as rape victims without a child sexual abuse history then setting the effect size at .50 is a reasonable estimate. With the alpha set at .01 and power set at .95, only 76 participants would be needed to find differences that exist. Given the overall findings of the parent study, one would also predict large effect sizes from pre- to posttreatment; therefore, the samples are also sufficient to detect pre- to posttreatment differences.
The child sexual abuse and non-child sexual abuse samples were compared with regard to their demographic and other trauma history variables aside from child sexual abuse (Table 1). The child sexual abuse sample reported significantly more robberies, kidnappings, rapes, attempted rapes, other sexual assaults, physical assaults with minor injuries, attempted murder, child physical abuse, and number of crime victimizations. There were no significant differences in the number of assaults with serious injuries or the criminal/vehicular death of a loved one between the two samples. There were no differences between the child sexual abuse and non-child sexual abuse samples regarding which treatment they received or whether they completed treatment.
TABLE 1.
Comparison of non-child sexual abuse versus child sexual abuse survivors on demographic and crime history variables
| Non-Child Sexual Abuse | Child Sexual Abuse | |||||
|---|---|---|---|---|---|---|
| Variable | ||||||
| Race (percentage)* | % | % | χ2 | P | ||
| Black | 15 | 26 | 2.1 | NS | ||
| White | 85 | 74 | ||||
| M | SD | M | SD | F | P | |
| Age (years) | 31.3 | 10.2 | 34.9 | 9.5 | 3.6 | NS |
| Education (years) | 14.5 | 2.7 | 14.0 | 2.4 | 1.3 | NS |
| Months since index rape | 91.8 | 98.6 | 111.8 | 103.4 | 1.6 | NS |
| Criminal Victimization History | ||||||
| Number of times a victim of crime | 5.2 | 4.7 | 7.8 | 4.7 | 13.7 | 0.001 |
| Childhood physical abuse | 3.6 | 2.7 | 4.7 | 2.3 | 6.9 | 0.005 |
| Robbery | 0.17 | 0.54 | 0.40 | 0.79 | 5.0 | 0.03 |
| Kidnapping | 0.16 | 0.40 | 0.59 | 1.10 | 12.5 | 0.001 |
| Rape (prior to index) | 0.60 | 1.10 | 1.81 | 1.80 | 30.2 | 0.001 |
| Attempted rape | 0.36 | 0.63 | 0.97 | 1.46 | 13.5 | 0.001 |
| Sexually assaulted | 0.30 | 0.78 | 1.47 | 1.77 | 33.8 | 0.001 |
| Serious physical assault | 0.15 | 0.54 | 0.34 | 0.87 | 3.1 | NS |
| Minor physical assault | 1.23 | 1.82 | 2.02 | 2.02 | 7.1 | 0.01 |
| Attempted murder | 0.08 | 0.34 | 0.31 | 0.58 | 10.8 | 0.001 |
| Homicide of close family member | 0.39 | 0.75 | 0.54 | 0.96 | 1.3 | NS |
χ2 and P are derived from the four race percentages
NS=nonsignificant.
Resick PA, Nishith P, Griffin MG. CNS Spectr. Vol 8, No 5. 2003.
Because, for these analyses, the delayed-treatment samples were folded into the samples that were treated immediately, preliminary analyses were conducted comparing these collapsed samples first on the CAPS and BDI, then the TSI subscales. The three TSI factors were subjected to two 2 × 3 multivariate analysis of variances (MANOVAs), representing treatment type (CPT or prolonged exposure), and assessments (pretreatment, posttreatment, and 9-month posttreatment). In the first analysis, CAPS total score and BDI scores were the dependent variables. The analysis resulted in a significant assessment effect, F(4,472)=61.1, Pillai’s trace=.68, P=.000, but no treatment-type effect or interaction. Both CAPS and BDI changed significantly from pre to posttreatment and there were no changes from the posttreatment to the 9-month assessment on either measure. In the second analysis, the three TSI factors were the dependent variables. This analysis also resulted in an assessment effect, F(6,446)=35.0, Pillai’s trace = .64, P=.000, but no treatment type effect or interaction. Significant assessment effects were found for all three TSI factors with significant decreases in scores occurring from pre to posttreatment, and no change from the posttreatment to follow-up assessments. Because there were no differences between the two types of therapy on any measure at any time point, the data were collapsed for the comparison of rape victims with or without a child sexual abuse history.
The means and standard deviations of the CAPS, BDI, and TSI subscale raw scores for the child sexual abuse and non-child sexual abuse samples are located in Table 2. The two groups were then compared by means of repeated measures MANOVA on the CAPS total score and BDI. This analysis produced a significant assessment period effect, F(4,472)=60.3, Pillai’s trace=.68, P=.000, but no group main effect or interaction. The participants improved on both the CAPS and BDI from pre- to posttreatment and then maintained their improvement through the 9-month follow-up.
TABLE 2.
Means, standard deviations, and pre-post hedges’ g effect sizes of non child sexual abuse versus child sexual abuse survivors on clinical scales.
| No Childhood Sexual Abuse | Childhood Sexual Abuse | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Pretreatment | Posttreatment | Pre- to Posttreatment | 9-month Posttreatment | Pretreatment | Posttreatment | 9-month Posttreatment | Pre-Posttreatment | ||||||
| TSI subscale | M | SD | M | SD | G | M | SD | M | SD | M | SD | M | SD | G |
| Anxious Arousal | 13.8 | 5.1 | 7.2 | 5.4 | 1.26 | 7.2 | 4.9 | 15.8 | 4.7 | 8.8 | 5.7 | 8.3 | 6.4 | 1.34 |
| Depression | 13.0 | 5.3 | 6.7 | 5.8 | 1.13 | 7.1 | 5.9 | 14.7 | 6.4 | 7.5 | 6.3 | 7.4 | 6.8 | 1.13 |
| Anger/Irritability | 12.6 | 5.9 | 6.7 | 5.0 | 1.08 | 6.6 | 5.5 | 14.0 | 6.0 | 8.0 | 6.4 | 8.2 | 6.6 | 0.97 |
| Intrusive Experiences | 12.7 | 5.1 | 5.8 | 5.4 | 1.31 | 5.2 | 5.5 | 15.1 | 6.4 | 7.3 | 6.4 | 6.3 | 6.8 | 1.22 |
| Defensive Avoidance | 15.8 | 5.3 | 6.7 | 6.3 | 1.56 | 6.2 | 6.1 | 16.9 | 5 | 7.8 | 6.5 | 6.9 | 7.4 | 1.57 |
| Dissociation | 11.0 | 5.0 | 5.4 | 4.3 | 1.20 | 5.6 | 4.1 | 14.2 | 6.2 | 7.2 | 5.8 | 6.8 | 6.0 | 1.17 |
| Impaired Self-Reference | 12.4 | 6.2 | 6.1 | 4.9 | 1.13 | 6.3 | 5.4 | 16.9 | 15.7 | 10.7 | 16.8 | 9.7 | 17.1 | 0.38 |
| Sexual Concerns | 9.9 | 6.5 | 4.7 | 4.6 | 0.92 | 4.6 | 4.2 | 13.5 | 7.5 | 6.8 | 6.1 | 6.7 | 6.9 | 0.98 |
| Dysfunctional Sexual Behavior | 4.5 | 4.8 | 1.5 | 2.9 | 0.76 | 2.3 | 4.2 | 7.0 | 7.5 | 2.6 | 4.1 | 2.9 | 4.5 | 0.73 |
| Tension Reduction Behavior | 5.0 | 3.7 | 2.4 | 2.7 | 0.80 | 2.4 | 2.5 | 6.7 | 4.9 | 3.1 | 3.1 | 3.1 | 2.9 | 0.88 |
| CAPS Total Score | 70.6 | 18.9 | 28.0 | 20.7 | 2.15 | 29.4 | 22.7 | 76.8 | 18.4 | 28.4 | 27.1 | 33.3 | 29.6 | 2.09 |
| BDI | 22.4 | 9.5 | 10.0 | 8.3 | 1.39 | 10.9 | 9.1 | 24.9 | 9.1 | 11.4 | 10.4 | 12.9 | 12.7 | 1.38 |
TSI=Trauma Symptom Inventory; CAPS=Clinician-Administered PTSD Scale; BDI=Beck Depression Inventory.
Resick PA, Nishith P, Griffin MG. CNS Spectr. Vol 8, No 5. 2003.
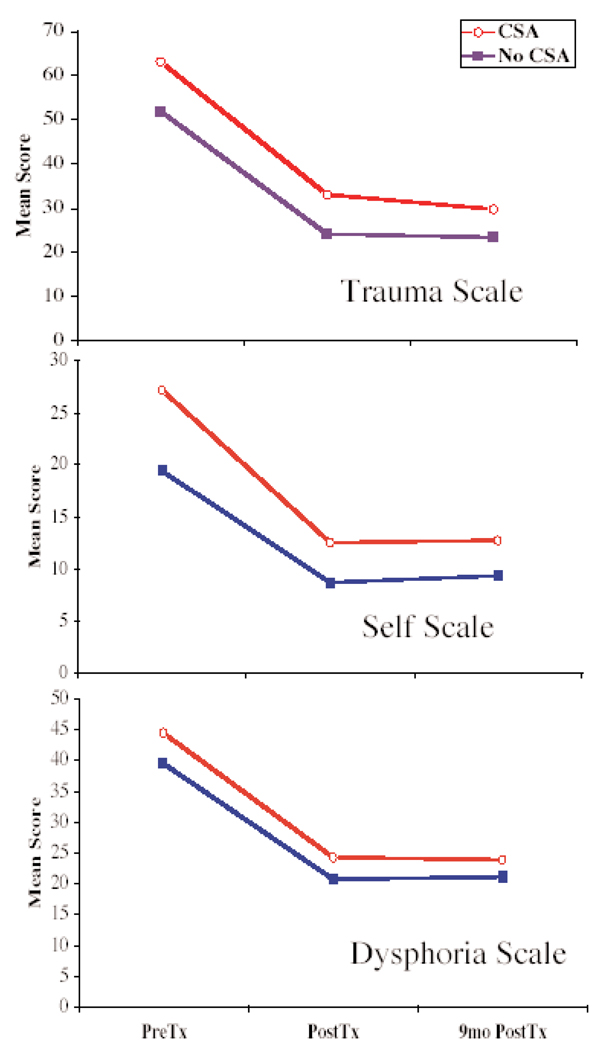
An initial MANOVA comparing the two groups at pretreatment on the three TSI factors was significant overall, F(3,111)=3.7, Pillai’s trace=.09, P=.02, indicated that the child sexual abuse participants reported significantly higher scores at pretreatment on two of the three factors, the Self factor, F(1,113)=7.3, P=.008 and the Trauma factor, F(1,113)=8.8, P=.004. There was only a trend for the two groups to be different on the Dysphoria factor. A repeated measures MANOVA of the three TSI factors resulted in significant child sexual abuse status main effect, F(3,110)=2.9, Pillai’s trace=.07, P=.039, an assessment main effect, F(6,446)=34.8, Pillais trace=.64, P=.000, but no assessment by child sexual abuse status interaction. Post hoc univariate analyses indicated that, while the two groups improved significantly on all three factors from pre- to posttreatment and maintained their improvement, there were also significant differences between the two groups on 2 of the 3 factors. The two groups differed overall on the Trauma, F(1,112)=5.8, P=.02, and Self factors, F(1,112)=6.9, P=.01, but not on the Dysphoria factor. The findings are depicted in Figure 1.
FIGURE 1.
Pretreatment, posttreatment, and 9-month follow-up comparison of rape victims with and without a history of CSA on three factors of the Trauma Symptom Inventory: Trauma, Self, and Dysphoria.
CSA=child sexual abuse; PreTx=pretreatment; PostTx=posttreatment; 9mo PostTx=9-months follow-up.
Resick PA, Nishith P, Griffin MG. CNS Spectr. Vol 8, No 5. 2003.
In order to explore which of the subscales contributed to the group differences, the MANOVAs were repeated for the constituent subscales of the Trauma and Self factors. The Trauma factor includes intrusive experiences, defensive avoidance, dissociation, and impaired self-reference. These subscales were subjected to a repeated measures MANOVA, which resulted in a significant assessment period effect, F(8,444)=24.9, Pillai’s trace=.62, P=.000, but no interaction and only a trend for a group main effect (P=.07). Post hoc pairwise comparisons indicated that the sample improved from pre- to posttreatment on all four subscales and these improvements were maintained through the 9-month follow-up.
On the Self scale, consisting of sexual concerns, dysfunctional sexual behavior, and tension reduction behaviors, the MANOVA resulted in a significant group main effect, F(3,111)=2.7, Pillai’s trace=.07, P=.05, a significant assessment period effect, F(6,450)=24.8, Pillai’s trace=.50, P=.000, but no group by assessment interaction. Post hoc analyses on the assessment periods indicated that all three subscale scores improved significantly from pre- to posttreatment and were then maintained over the 9-month follow-up period. Post hoc analyses of the group effect indicated significant overall group differences on all three subscales. Pre- to post-effect sizes calculated with Hedge’s G on all TSI sub-scales as well as the CAPS and BDI are located in Table 2. There were large effect sizes for all subscales with one exception. In the child sexual abuse group, there was a medium effect size on the impaired self-reference scale. That subscale had a very large standard deviation compared with the other subscales, indicating greater variability of responses to treatment on that scale.
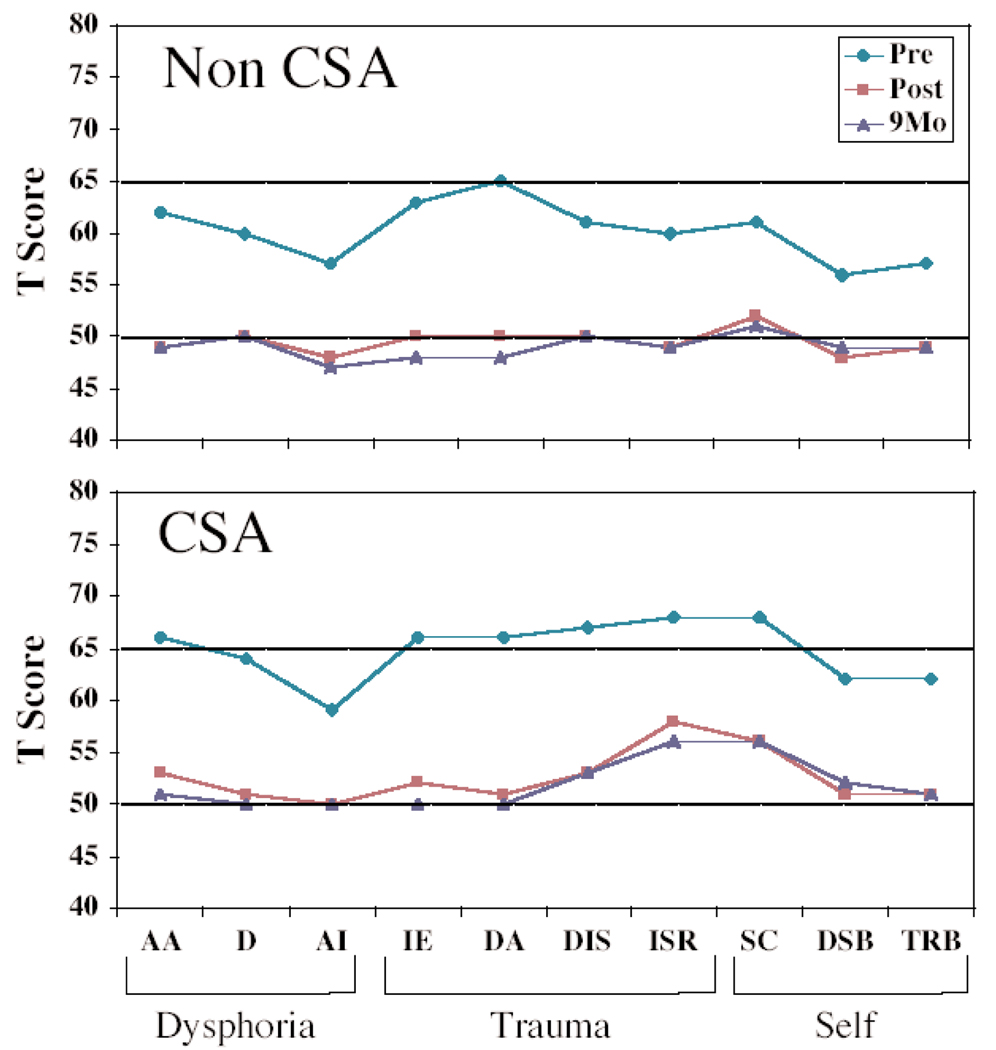
In order to determine how much of the overall group effect was determined by pretreatment differences, a MANOVA was conducted on the three Self subscales at posttreatment using the pretreatment scores as covariates. The MANOVA was nonsignificant, indicating that there were no differences between the child sexual abuse and non-child sexual abuse groups at posttreatment, once pretreatment scores had been accounted for. The same thing occurred with a MANOVA on the Trauma factor subscales. Once the pretreatment differences were accounted for there were no differences between the child sexual abuse and non-child sexual abuse groups at posttreatment. Figure 2 depicts the subscale scores plotted on a TSI profile. Both groups are within normal limits at the posttreatment and follow-up periods.
FIGURE 2.
Pretreatment, posttreatment, and 9-month follow-up comparison of rape victims with and without a history of CSA on the 10 subscales of the Trauma Symptom Inventory.
CSA=child sexual abuse; Pre=pretreatment; Post=posttreatment; 9Mo=9-months follow-up; AA=anxious arousal; D=depression; AI=anger/irritability; IE=intrusive experiences; DA=defensive avoidance; DIS=dissociation; ISR=impaired self-reference; SC=sexual concerns; DSB=dysfunctional sexual behavior; TRB=tension reduction behavior.
Resick PA, Nishith P, Griffin MG. CNS Spectr. Vol 8, No 5. 2003.
DISCUSSION
On the TSI profiles at pretreatment, the rape victims without a history of child sexual abuse were characterized by peak elevations on defensive avoidance, intrusive experiences and anxious arousal, the symptom clusters of PTSD. The non-child sexual abuse patients did, in fact, appear to have a simple form of PTSD although they showed general elevations across the subscale profile. On the other hand, the rape victims with a child sexual abuse history, as a group, exhibited elevations beyond the clinical cut-off (T score >65) on 6 of the 10 scales, indicating a more complex symptom picture. At the posttreatment and 9-month follow-up assessments the non-child sexual abuse patients fell right on the population norms on all subscales (T score=50), while the child sexual abuse patients were at the norms for most of the subscales. Although there were no significant differences at posttreatment between the non-child sexual abuse and child sexual abuse patients on the subscales once the pretreatment scores were accounted for, on an absolute level, the child sexual abuse patients, as a group, appeared to be elevated about a half standard deviation on the impaired Self-reference and Sexual Concerns subscales. For those clients who have remaining problems with sexual dysfunctions or identity confusion, therapists may want to address these problems as well.
The results of this study indicate that both types of CBT, CPT, and prolonged exposure are effective not only for symptoms of PTSD and depression, but also the more complex symptoms that have been observed among those with histories of child sexual abuse. Even though the women with a child sexual abuse history had greater trauma histories generally than those without child sexual abuse, the two groups did not differ with regard to PTSD symptoms, depression, or other dysphoric emotions. They did differ with regard to the Self factor, which consists of Sexual Concerns, Dysfunctional Sexual Behavior, and Tension Reduction Behaviors; and the Trauma factor, when examined as a single measure, but not as individual subscales. However, the participants improved significantly as a result of treatment on the 3 factors and all 10 subscales of the TSI. There were no significant interactions between child sexual abuse status and assessment periods, on any of the measures, indicating that the child sexual abuse patients improved as much as the non-child sexual abuse patients. On the Self factor and the component subscales, child sexual abuse patients started with higher scores but reported an equal benefit through treatment. At the posttreatment and 9-month follow-up assessments, both groups fell within normal ranges on the Self factor subscales as well as the other measures. It should be noted here, that dissociation, which is often of concern to clinicians, improved significantly as a result of treatment without any particular attention or differential treatment.
While the TSI captures many of the symptoms that comprise the complex PTSD spectrum, this instrument does not map exactly onto the complex PTSD/Disorders of Extreme Stress Not Otherwise Specified categories of symptoms. Further research using other instruments tailored to assess complex PTSD would be helpful in delineating whether there are any limitations in the use of CBT with child sexual abuse survivors with a complex symptom picture. However, unlike some of the complex PTSD interviews, such as the Structured Interview for Disorders of Extreme Stress,45 which results in a categorical diagnosis with limited statistical potential, the TSI was empirically generated, normed, and can be subjected to the full range of statistical procedures.
CONCLUSION
Overall, the results of this study are very encouraging. CBT protocols, implemented over a 6-week period were highly effective in reducing, not only chronic PTSD and depressive symptoms, but more insidious symptoms, such as dissociation, impaired self-reference, dysfunctional sexual behavior, and tension reduction behaviors. Although longstanding clinical stereotypes among some therapists persist that CBT therapy is “superficial” and only for simple cases, and some trauma experts46 have argued that child sexual abuse survivors need longer and more in-depth therapy than trauma victims without such a history, the findings of this study illustrate that short-term CBT, provided in a structured and focused protocol, might be quite sufficient for the range of symptoms of complex PTSD. While there is evidence that those with repeated traumas may have more complex symptom patterns that may prolong or compromise natural recovery, brief CBT appears to be effective in remediating these problems. Recovery through therapy does not appear to be hampered by a complex presentation. However, longer follow-ups will be needed to determine whether the improvements remain over a longer period of time. Five-year follow-up assessments on this treatment sample are currently underway.
FOCUS POINTS
Can brief cognitive-behavioral treatments work to treat complex posttraumatic stress disorder (PTSD)?
Findings indicated that brief cognitive-behavioral treatments significantly reduced both PTSD symptoms and complex PTSD symptoms.
The findings suggest that brief cognitive-behavioral approaches can be used to successfully treat patients with complex trauma histories.
Acknowledgments
The authors would like to thank all of the staff and faculty of the Center for Trauma Recovery and our community collaborators for their assistance on this project.
Footnotes
Disclosure: This work was supported by a grant from the National Institute of Mental Health (Grant #NIH-1 R01-MH51509) awarded to Dr. Resick.
REFERENCES
- 1.Kessler R, Sonnega A, Bromet E, Hughes M, Nelson C. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 2.Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol. 1993;61:984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- 3.Briere J, Runtz M. Symptomatology associated with childhood sexual victimization in a nonclinical adult sample. Child Abuse Negl. 1988;12:51–59. doi: 10.1016/0145-2134(88)90007-5. [DOI] [PubMed] [Google Scholar]
- 4.Gershenson HP, Musick JS, Ruch-Ross HS, Magee V, Rubino KK, Rosenberg D. The prevalence of coercive sexual experience among teenage mothers. J Interpers Violence. 1989;4:204–219. [Google Scholar]
- 5.Jackson JL, Calhoun KS, Amick AE, Madderer HM, Habif VL. Young adult women who report childhood intrafamilial sexual abuse: subsequent adjustment. Arch Sex Behav. 1990;19:211–221. doi: 10.1007/BF01541547. [DOI] [PubMed] [Google Scholar]
- 6.Kendall-Tackett K, Simon A. Molestation and the onset of puberty: data from 365 adults molested as children. Child Abuse Negl. 1988;12:73–81. doi: 10.1016/0145-2134(88)90009-9. [DOI] [PubMed] [Google Scholar]
- 7.Nishith P, Mechanic MB, Resick PA. Prior interpersonal trauma: The contribution to current PTSD symptoms in female rape victims. J Abnorm Psychol. 2000;109:20–25. [PMC free article] [PubMed] [Google Scholar]
- 8.Wyatt GE, Newcomb M. Internal and external mediators of women’s sexual abuse in childhood. J Consult Clin Psychol. 1990;58:758–767. doi: 10.1037//0022-006x.58.6.758. [DOI] [PubMed] [Google Scholar]
- 9.Koss MP, Dinero TE. Discriminant analysis of risk factors for sexual victimization among a national sample of college women. J Consult Clin Psychol. 1989;57:242–250. doi: 10.1037//0022-006x.57.2.242. [DOI] [PubMed] [Google Scholar]
- 10.Norris F, Johnson K. The effects of “self-help” precautionary measures on criminal victimization and fear. J Urban Affairs. 1988;10:161–181. [Google Scholar]
- 11.Norris F, Kaniasty K. Psychological distress following criminal victimization in the general population: cross-sectional, longitudinal, and prospective analyses. J Consult Clin Psychol. 1994;62:111–123. doi: 10.1037//0022-006x.62.1.111. [DOI] [PubMed] [Google Scholar]
- 12.Herman JL, Perry C, van der Kolk BA. Childhood trauma in borderline personality disorder. Am J Psychiatry. 1989;146:490–495. doi: 10.1176/ajp.146.4.490. [DOI] [PubMed] [Google Scholar]
- 13.Ogata SN, Silk KR, Goodrich S, Lohr NE, Westen D, Hill EM. Childhood sexual and physical abuse in adult patients with borderline personality disorder. Am J Psychiatry. 1990;147:1008–1013. doi: 10.1176/ajp.147.8.1008. [DOI] [PubMed] [Google Scholar]
- 14.Saxe GN, Chinman G, Berkowitz R, et al. Somatization in patients with dissociative disorders. Am J Psychiatry. 1994;151:1329–1335. doi: 10.1176/ajp.151.9.1329. [DOI] [PubMed] [Google Scholar]
- 15.Ross CA, Miller SD, Reagor P, Bjornson L, Fraser GA, Anderson G. Multicenter structured interview data on 102 cases of multiple personality disorder from four centers. Am J Psychiatry. 1990;147:596–601. doi: 10.1176/ajp.147.5.596. [DOI] [PubMed] [Google Scholar]
- 16.Saxe G, van der Kolk BA, Hall K, et al. Dissociative disorders in psychiatric inpatients. Am J Psychiatry. 1993;150:1037–1042. doi: 10.1176/ajp.150.7.1037. [DOI] [PubMed] [Google Scholar]
- 17.van der Kolk BA, Perry C, Herman Jl. Childhood origins of self-destructive behavior. Am J Psychiatry. 1991;148:1665–1671. doi: 10.1176/ajp.148.12.1665. [DOI] [PubMed] [Google Scholar]
- 18.Herzog DB, Staley JE, Carmody S, Robbins WM, van der Kolk BA. Childhood sexual abuse in anorexia nervosa and bulimia nervosa: a pilot study. J Am Acad Child Adol Psychiatry. 1993;32:962–966. doi: 10.1097/00004583-199309000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Abueg FR, Fairbank JA. Behavioral treatment of posttraumatic stress disorder and co-occurring substance abuse. In: Saigh PA, editor. Posttraumatic Stress Disorder: A Behavioral Approach to Assessment and Treatment. Boston, Mass: Allyn & Bacon; 1992. pp. 111–146. [Google Scholar]
- 20.Donaldson M, Gardner J. Traumatic stress among women after childhood incest. In: Figley C, editor. Trauma and Its Wake. New York, NY: Brunner/Mazel; 1985. [Google Scholar]
- 21.Lindberg FH, Distad LJ. Posttraumatic stress disorders in women who experienced childhood incest. Child Abuse Negl. 1985;9:329–334. doi: 10.1016/0145-2134(85)90028-6. [DOI] [PubMed] [Google Scholar]
- 22.Rodriguez N, Ryan SW, Kemp HV, Foy D. Posttraumatic stress disorder in adult female survivors of childhood sexual abuse: A comparison study. J Consult Clin Psychol. 1997;65:53–59. doi: 10.1037//0022-006x.65.1.53. [DOI] [PubMed] [Google Scholar]
- 23.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association Press; 1994. [Google Scholar]
- 24.Herman JL. Complex PTSD: a syndrome in survivors of prolonged and repeated trauma. J Traum Stress. 1992;5:377–391. [Google Scholar]
- 25.Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive-behavioral procedures. J Consult Clin Psychol. 1991;59:715–723. doi: 10.1037//0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- 26.Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. J Consult Clin Psychol. 1999;67:194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- 27.Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. J Consult Clin Psychol. 1992;60:748–756. doi: 10.1037//0022-006x.60.5.748. [DOI] [PubMed] [Google Scholar]
- 28.Resick PA, Schnicke MK. Cognitive processing therapy for rape victims: a treatment manual. Newbury Park, Calif: Sage Publications; 1993. [Google Scholar]
- 29.Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive processing therapy, prolonged exposure, and a waiting condition for the treatment of PTSD in female rape victims. J Consult Clin Psychol. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Frank E, Anderson BP. Psychiatric disorders in rape victims: past history and current symptomatology. Compr Psychiatry. 1987;28:77–82. doi: 10.1016/0010-440x(87)90047-2. [DOI] [PubMed] [Google Scholar]
- 31.Frank E, Turner SM, Stewart BD, Jacob J, West D. Past psychiatric symptoms and the response to sexual assault. Compr Psychiatry. 1981;22:479–487. doi: 10.1016/0010-440x(81)90036-5. [DOI] [PubMed] [Google Scholar]
- 32.Kramer TL, Greene BL. Posttraumatic stress disorder as an early response to sexual assault. J Interpers Viol. 1991;6:160–173. [Google Scholar]
- 33.Roth S, Wayland K, Woolsey M. Victimization history and victim-assailant relationship as factors in recovery from sexual assault. J Traum Stress. 1990;3:169–180. [Google Scholar]
- 34.Cloitre M, Koenen KC, Cohen LR, Han H. J Consult Clin Psychol. 2002;70:1067–1074. doi: 10.1037//0022-006x.70.5.1067. [DOI] [PubMed] [Google Scholar]
- 35.Blake DD, Weathers FW, Nagy LM, et al. The development of a clinician-administered PTSD scale. J Traum Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- 36.Blake DD, Weathers FW, Nagy LM, et al. A clinician rating scale for assessing current and lifetime PTSD: the CAPS-1. Behav Therapist. 1990;13:187–188. [Google Scholar]
- 37.Beck AT, Ward CH, Mendelsohn M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 38.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 39.Briere J. The Trauma Symptom Inventory (TSI): Professional Manual. Odessa, FL: Psychological Assessment Resources; 1995. [Google Scholar]
- 40.Resick PA, Jordan CG, Girelli SA, Hutter CK, Marhoefer-Dvorak S. A comparative outcome study of group behavior therapy for sexual assault victims. Behav Ther. 1988;19:385–401. [Google Scholar]
- 41.Rowan AB, Foy DW, Rodriguez N, Ryan S. Posttraumatic stress disorder in a clinical sample of adults sexually abused as children. Child Abuse Negl. 1994;18:51–61. doi: 10.1016/0145-2134(94)90095-7. [DOI] [PubMed] [Google Scholar]
- 42.Zaidi LY, Knutson JF, Mehm JG. Transgenerational patterns of abusive parenting: Analog and clinical tests. Aggress Behav. 1989;15:137–152. [Google Scholar]
- 43.Foa EB, Rothbaum BO. Treating the Trauma of Rape. New York,NY: Guilford Press; 1997. [Google Scholar]
- 44.Erdfelder E, Faul F, Buchner A. GPOWER: a general power analysis program. Behav Res Methods Instrum Comput. 1996;28:1–11. [Google Scholar]
- 45.Pelcovitz D, van der Kolk B, Roth S, et al. Development of a criteria set and a structured interview for disorders of extreme stress (SIDES) J Traum Stress. 1997;10:3–16. doi: 10.1023/a:1024800212070. [DOI] [PubMed] [Google Scholar]
- 46.Briere J. Complex psychological trauma: clinical implications of an evolving paradigm. Presidential Address at the 18th Annual Meeting of the International Society for Traumatic Stress Studies; November 7–10, 2002; Baltimore, MD. [Google Scholar]