Abstract
This study examined the association of autonomy-related variables, including exercise motivation, with psychological well-being and quality of life, during obesity treatment. Middle-aged overweight/obese women (n = 239) participated in a 1-year behavioral program and completed questionnaires measuring need support, general self-determination, and exercise and treatment motivation. General and obesity-specific health-related quality of life (HRQOL), self-esteem, depression, and anxiety were also assessed. Results showed positive correlations of self-determination and perceived need support with HRQOL and self-esteem, and negative associations with depression and anxiety (P < .001). Treatment autonomous motivation correlated positively with physical (P = .004) and weight-related HRQOL (P < .001), and negatively with depression (P = .025) and anxiety (P = .001). Exercise autonomous motivation was positively correlated with physical HRQOL (P < .001), mental HRQOL (P = .003), weight-related HRQOL (P < .001), and self-esteem (P = .003), and negatively with anxiety (P = .016). Findings confirm that self-determination theory's predictions apply to this population and setting, showing that self-determination, perceived need support, and autonomous self-regulation positively predict HRQOL and psychological well-being.
1. Introduction
Self-determination theory is a well-known psychological framework to study people's behavior, based on the assumption that humans are innately motivated toward growth and health, a process which can be nurtured or thwarted by the social environment [1, 2]. Much research on self-determination theory, particularly in the health domain, has focused on the study of the characteristics of motivation and associated regulatory processes. For instance, the degree to which people feel autonomous (i.e., self-determined) versus controlled in their motivated pursuits, and how this relates to behavioral persistence (e.g., [3, 4]). Intrinsic motivation, the doing of an activity for its inherent satisfactions, is highly autonomous and represents the prototypic instance of self-determination, while extrinsically motivated behaviors, by contrast, cover the continuum between amotivation and intrinsic motivation, varying in the extent to which their regulation is autonomous. Within extrinsic regulations, autonomous regulations (identified and integrated) reflect a sense of personal volition and recognition of the importance of the target behavior and its consequences. In contrast, in controlled regulations (external and introjected) people feel forced to comply with outside demands or feel guilty or ashamed if they do not perform the target behavior [1, 2].
The concept of basic needs is central for self-determination theory. It states that people have innate psychological needs that when fulfilled have an effect on personal growth, psychosocial adjustment, feelings of integrity, and well-being [5]. Additionally, it clarifies the relationships between the satisfaction of the needs for competence, autonomy, and relatedness and psychological functioning and well-being. It should be noted that, from a self-determination theory perspective, well-being is not concerned exclusively with “hedonic” or subjective well-being in the tradition of Positive Psychology [6], namely, the experience of happiness, usually characterized by high positive affect, reduced negative affect, and life satisfaction [7]. Self-determination theory favors a “eudaimonic” view of well-being, focused on feeling fully functioning, self-coherent, and with a deep sense of wellness, and vitality [8], rooted on the idea of fulfilling or realizing one's daimon or true nature [9]. As a consequence of this broader notion of well-being, which includes happiness and emotional well-being but also meaning and personal growth, psychological well-being has been assessed in self-determination theory studies with indicators of positive affect and mental health. Some examples are self-esteem, vitality, life satisfaction, and also (low levels of) depression and anxiety [10, 11].
Previous studies in exercise contexts which examined perceived choice, a marker of autonomy, in relation to well-being found that it was associated with reduced negative affect [12] and positive well-being [13]. More recent studies in the exercise domain showed that the satisfaction of basic psychological needs for competence, autonomy, and relatedness enhanced psychological well-being in the form of physical self-perception [14], subjective vitality and positive affect [10, 11], enjoyment and intrinsic motivation for exercise [15], and satisfaction with life [11].
Numerous studies have demonstrated that obese individuals experience significant impairments in health-related quality of life (HRQOL) as a result of their weight, with greater impairments being associated with greater degrees of obesity [16–18]. Conversely, weight loss has been shown to improve quality of life in obese persons undergoing a variety of treatments [16]. Assessing quality of life is especially important to help determine the comparative efficacy of different treatments and to assess the impact of treatment on how patients feel and function in their everyday life [19, 20]. The use of both general and specific quality of life instruments is a methodological recommendation from previous obesity HRQOL research [21].
HRQOL, as measured by the SF-36, improves after small to moderate amounts of weight loss with nonsurgical methods [16]. Not only weight loss [22] but also weight maintenance is considered to be beneficial for physical HRQOL [23]. Using obesity-specific measures, such as the IWQOL and IWQOL-Lite, quality of life improvements were associated with decrease in body weight in different studies [22, 24–26]. In a recent meta-analysis, weight loss treatment was associated with lowered depression and increased self-esteem [27]; only treatments that produced actual weight loss predicted increased self-esteem, whereas improvements in depression were independent of weight loss.
In Portugal, the prevalence of overweight and obesity is 53.6% in adult women; of these 13.4% are obese and 34.4% are overweight [28]. However, there are very few studies that have analyzed markers of quality of life and well-being among the Portuguese population, particularly in overweight or obese individuals. One study showed that body image and physical dimensions of obesity-specific quality of life improved significantly during the course of treatment [29]. Another study indicated that changes in weight and body image may reciprocally affect each other during the course of behavioral obesity treatment, and that weight loss partially mediated the effect of treatment on quality of life and on self-esteem [30].
In the present study, our goal was to assess the association of perceived need support, general self-determination (as measured by perceived choice), and treatment and exercise motivation (autonomous versus controlled regulation) with variables reflecting psychological well-being and quality of life, during a behavioral obesity treatment program lasting 1 year. Based on self-determination theory, we predicted that higher perceived need support, higher self-determination, and more autonomous treatment and exercise self-regulation would be associated with higher HRQOL and improved psychological well-being. To our knowledge, only a few studies have examined predictors of psychological well-being in overweight/obese persons during behavioral treatment [29, 30] and none have tested self-determination theory variables as putative predictors.
2. Materials and Methods
2.1. Design
The study was conducted within a randomized controlled trial in overweight and moderately obese women, primarily focused on increasing exercise self-motivation and exercise adherence, aiming at long-term weight control. The intervention group participated in weekly or bimonthly sessions during approximately one year. The program's principles and intervention style were based on self-determination theory, while the control group received a general health education program. The intervention and its theoretical rationale have been described in detail elsewhere [31, 32]. The Faculty of Human Kinetics Ethics Committee reviewed and approved the study.
2.2. Participants
Participants (n = 239, 37.6 ± 7.1 years old; BMI = 31.5 ± 4.1 kg/m2) were recruited from the community at large through media advertisements. About 67% of the study participants had at least some college education, 23% had between 10 and 12 years of school and 10% had 9 years or less of school. At baseline, women in the intervention group did not differ from those in the control group in terms of BMI, age, education, or marital status [31]. There were also no differences between the 208 women who completed the 12-month intervention and the 31 who withdrew from the program, for any demographic or baseline psychosocial variable, with the exception of age; women who stayed in the program were on average four years older (P = .01).
2.3. Measurements
Data was collected at baseline, corresponding to the pretreatment scores, and at 12 months, corresponding to the end of the treatment. The instruments were validated Portuguese versions of some of the most commonly used psychosocial instruments in obesity research and are described in detail below.
2.3.1. Self-Determination Measures
Self-determination was assessed with the Perceived Choice subscale from the Self-Determination Scale [33], an instrument designed to evaluate individual differences in the extent to which people function in a self-determined way (e.g., “I do what I do because it interests me”, “I do what I do because I have to”, “What I do is often not what I'd choose to do”). Cronbach's α was 0.83. Participants' perceived need support was evaluated with the Health Care Climate Questionnaire [3]. It includes items reflecting fostering of autonomy (e.g., “I feel that the staff has provided me choices and options”), involvement (e.g., “The staff handles peoples' emotions very well”), and the provision of structure (e.g., “the staff has made sure I really understand my condition and what I need to do”). Total score is calculated by summing response items, higher scores indicating higher perceptions of need support climate (Cronbach's α = 0.96).
Self-regulation for treatment was measured with the Treatment Self-Regulation Questionnaire [3] assessing the degree to which a person's motivation for participating in treatment is autonomous versus controlled. Items are summed into two subscales, one measuring autonomous (Cronbach's α = 0.86), the other controlled (Cronbach's α = 0.80) regulation. Exercise regulations were assessed by the Self-Regulation Questionnaire for Exercise [34] measuring exercise regulatory motives. The scale can also be summarized into two subscales, autonomous (Cronbach's α = 0.91) and controlled exercise regulation (Cronbach's α = 0.73).
2.3.2. Health-Related Quality of Life Measures
General quality of life was measured with the SF-36 [35, 36], composed of two scales and a total of 36 items, reflecting physical (physical component summary, PCS) and psychological (mental component summary, MCS) composite values (Cronbach's α between 0.66 to 0.87), in which higher results represent greater quality of life perception. The weight-related aspects of health-related quality of life was assessed using the Impact of Weight on Quality of Life – Lite scale (IWQOL-L) [37, 38], a 31-item questionnaire (Cronbach's α = 0.93). Higher scores indicate higher weight-related quality of life.
2.3.3. Psychological Well-Being Measures
Self-esteem was assessed with the Rosenberg Self-Concept/Self-Esteem Scale [39, 40] with higher scores of the RSES representing greater self-esteem (Cronbach's α = 0.88). Depression was evaluated with the Beck Depression Inventory [41, 42], where higher scores represent greater levels of depressive symptoms (Cronbach's α = 0.87). State anxiety was assessed with the State-Trait Anxiety Inventory [43], where higher scores represent greater levels of anxiety (Cronbach's α = 0.92).
2.3.4. Body Weight
Body weight was measured twice with a standardized procedure (average was used) at baseline and at the end of the treatment (12 months) using an electronic scale (SECA model 770, Hamburg, Germany). Height was measured with a balance-mounted stadiometer to the nearest 0.1 cm.
2.4. Statistical Procedures
For quality of life and psychological well-being variables, 12-month standardized residuals were used, calculated by regressing the 12-month value onto the baseline value, producing an outcome variable which is entirely orthogonal to (i.e., adjusted for) the baseline value [44]. Unadjusted 12-month scores were used for treatment and exercise motivation, perceived need support, and self-determination. This option was based on the fact that most participants did not engage in regular exercise at the beginning of the intervention, which yielded exercise self-regulation measures less valid (e.g., “I exercise because I”…). Also, treatment self-regulation (i.e., reasons to stay in treatment) and perceived need support from the intervention team could only be evaluated after participants started the intervention. For consistency, the same procedure was adopted for general self-determination.
Statistical analyses were completed using the Statistical Package for the Social Sciences (PASW Statistics 18). Pearson correlations and partial correlations were used to test associations among all variables in the study, and also to examine associations between the independent variables and a global well-being z-score, computed as mean value of all HRQOL and psychological well-being z-scores, before and after adjusting for group. Stepwise linear regressions were used to analyze the independent effect of self-determination theory's factors on HRQOL and psychological well-being. We ran the same analysis controlling separately for a potential intervention effect and for an effect of weight change on outcomes. Tertiles were computed based on the mean z-score value to define success groups. Mean differences in HRQOL and psychological well-being between women in the “low HRQOL and psychological well-being” and “high HRQOL and psychological well-being” tertile-formed groups were tested using independent t-tests. Type I error was set at α = 0.05 (two-tailed) for all tests.
3. Results
At the end of the 12-month intervention, there was an overall 87% retention rate. Correlations among independent variables and measures of well-being are presented in Table 1. Self-determination (P = .001), perceived need support (P < .001), treatment autonomous self-regulation (P < .001), and exercise autonomous self-regulation (P < .001) were positively associated with the global well-being z-score, while treatment controlled self-regulation was negatively correlated with well-being (P = .001). Similar results were found after adjusting for group. More specifically, self-determination correlated positively with HRQOL and self-esteem, and negatively with depression and anxiety. Regarding self-determination theory treatment variables, perceived need support was positively correlated with physical, mental, and weight-related HRQOL, and with self-esteem; in turn, correlations were negative with depression and anxiety. Treatment autonomous self-regulation was positively associated with physical and weight-related HRQOL, negatively with depression and anxiety, and not related to mental HRQOL. Conversely, treatment controlled self-regulation correlated positively with anxiety and negatively with self-esteem, physical, and weight-related HRQOL. For exercise variables, results indicated that autonomous self-regulation was positively associated with HRQOL and self-esteem, but negatively correlated with anxiety. Controlled exercise self-regulation was generally not associated with psychological outcomes.
Table 1.
Self-determination theory variables correlation with HRQOL and psychological well-being (at 12 months).
| PCS HRQOL | MCS HRQOL | Obesity specific HRQOL | Self-Esteem | Depression | Anxiety | z-score well-being | ||
|---|---|---|---|---|---|---|---|---|
| r | r | r | r | r | r | r | r partial | |
| Self-determination | 0.27*** | 0.33*** | 0.18* | 0.27*** | −0.16* | −0.33*** | 0.37*** | 0.36*** |
| Perceived need support | 0.19** | 0.15* | 0.29*** | 0.15* | −0.16* | −0.25** | 0.28*** | 0.20** |
| Treatment controlled self-regulation | −0.14* | −0.09 | −0.26*** | −0.14* | 0.11 | 0.28*** | −0.23** | −0.27*** |
| Treatment autonomous self-regulation | 0.20** | 0.12 | 0.26*** | 0.12 | −0.17* | −0.24** | 0.27*** | 0.16* |
| Exercise controlled self-regulation | 0.01 | −0.01 | −0.07 | −0.12 | 0.08 | 0.09 | −0.06 | −0.11 |
| Exercise autonomous self-regulation | 0.28*** | 0.21** | 0.27*** | 0.15* | −0.11 | −0.17* | 0.30*** | 0.23** |
r: Person's correlation coefficient; *P < .05, **P < .05, ***P < .001; r partial: partial correlation coefficient adjusting for group; PCS: physical component summary; MCS: mental component summary; z-score was computed as mean value of all HRQOL and psychological well-being z-scores.
Next, we ran multiple regression models, using self-determination, perceived need support, treatment self-regulation, and exercise self-regulation as independent variables and global well-being as the dependent variable. Results are presented in Table 2. Self-determination, perceived need support, controlled treatment self-regulation (negative association), and exercise autonomous self-regulation were independent predictors of global psychological well-being and explained 29% of the variance. To test whether these relations held when adjusting for group (i.e., controlling for the intervention effect), the same regression model was run, this time with group assignment forced into the model. Results were comparable to the unadjusted model (28% variance explained, P < .001); however, only self-determination, controlled treatment self-regulation (negatively), and perceived need support were found to predict psychological well-being (see Model 2 in Table 2). To test if weight change was a confounding factor in these relations, the same regression model was run with weight change also in the model (see Model 3 in Table 2). Results were comparable to Model 2 (33% variance explained; P < .001).
Table 2.
Multiple regression for psychological well-being z-score at intervention's end.
| B | SE B | β | Adj R2 | P | ||
|---|---|---|---|---|---|---|
| Model 1 | ||||||
| Self-determination | 0.04 | 0.010 | .25*** | |||
| Perceived need support | 0.01 | 0.003 | .16* | |||
| Treatment controlled self-regulation | −0.02 | 0.005 | −.22** | |||
| Exercise autonomous self-regulation | 0.01 | 0.006 | .18* | 0.24 | <.001 | |
| Model 2 | ||||||
| Group | 0.11 | 0.048 | .16* | |||
| Self-determination | 0.04 | 0.010 | .28*** | |||
| Perceived need support | 0.01 | 0.003 | .17* | |||
| Treatment controlled self-regulation | −0.02 | 0.005 | −.22** | 0.24 | <.001 | |
| Model 3 | ||||||
| Weight change | −0.14 | 0.043 | −.22** | |||
| Self-determination | 0.04 | 0.010 | .28*** | |||
| Perceived need support | 0.01 | 0.003 | .22** | |||
| Treatment controlled self-regulation | −0.02 | 0.005 | −.20** | 0.28 | <.001 | |
z-score was computed as mean value of all HRQOL and psychological well-being z-scores; group was coded as 1 to the intervention group, −1 to the control group; note that a negative weight change represents weight loss (a positive outcome); *P < .05; **P < .01; ***P < .001.
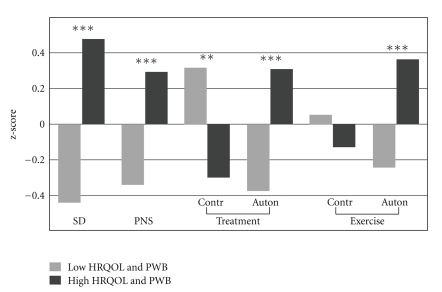
A final analysis was conducted, comparing z-scored self-determination theory variables at the highest and lowest of tertiles of global well-being (z-scored) (see Figure 1). Participants in the higher psychological well-being group had higher self-determination (P < .001), perceived need support (P < .001), lower treatment controlled self-regulation (P = .001), higher treatment autonomous self-regulation (P < .001), and higher exercise autonomous self-regulation (P < .001). The groups did not differ for exercise controlled self-regulation.
Figure 1.
Self-determination theory-based variables by tertile-split group of HRQOL and psychological well-being (at 12 months). HRQOL: health-related quality of life; PWB: psychological well-being; SD: self-determination; PNS: perceived need support; Contr: controlled; Auton: autonomous; P: P values for independent t-test comparing two tertiles considering global HRQOL and PWB z-score, tertile 1 defined as unsuccessful (low) HRQOL and PWB group and tertile 3 defined as successful (high) HRQOL and PWB group; **P < .01; ***P < .001.
4. Discussion
The primary goal of this study was to examine the association of general, contextual (obesity treatment), and situation-specific (exercise-related) measures of self-determination with psychological well-being and HRQOL. To briefly summarize our findings, higher self-determination and perceived need support, lower treatment controlled self-regulation, and higher exercise autonomous self-regulation were significant predictors of well-being in the course of a 1-year behavioral treatment for obesity, before and after adjustment for weight change.
According to self-determination theory, more self-determined behavior, which is partially derived from need-supportive interactions with one's environment, leads to improved psychological well-being [45]. This causal path is supported by the present results, the first of this kind to be conducted in the context of behavioral obesity treatment. Additionally, participants in this study who indicated more autonomous reasons to participate in treatment also reported higher scores on most markers of psychological well-being. Finally, women with higher HRQOL and enhanced psychological well-being were those for whom exercise behavior was associated with valued outcomes and/or for whom being physically active was enjoyable and optimally challenging (autonomous regulation). We have previously detailed the mechanisms by which interventions can promote autonomous self-regulation for treatment and specifically for exercise [31, 32].
In an exercise-specific context, a study by Wilson et al. showed that if the needs for competence, autonomy, and relatedness in an exercise setting are satisfied, subjective vitality and the degree of positive affect typically experienced within one's exercise session are enhanced [10]. In overweight sedentary women, externally imposed exercise intensity led to a significant decline in ratings of pleasure during exercise session, compared to self-selected intensity [15]. These findings have bearing on the importance of perceived choice in exercising, which could exert positive effects on autonomous regulation, intrinsic motivation, and adherence [15]. Another study with overweight and obese individuals, using positive and negative affect, subjective vitality, and satisfaction with life as measures of well-being, showed that exercise-related autonomy positively predicted satisfaction with life and that intrinsic motivation was a positive predictor of positive affect, while introjected regulation was found to be a negative predictor of subjective vitality [11]. In fact, research generally indicates that more autonomous regulations enhance not only behavioral persistence but also psychological well-being [3, 46, 47]. In contrast, controlled regulations are typically associated with diminished psychological well-being, also reflected in lower self-esteem [48]. Results of the present work are consistent with these findings in showing that treatment and exercise autonomous self-regulation also predict better psychological well-being in overweight or obese women undergoing treatment.
In the present study, as predicted, controlled reasons to stay in treatment predicted poorer psychological well-being. However, controlled motivation towards exercise was generally not related to psychological outcomes. As assessed in this study, controlled regulations include reasons with a clear external frame of reference (e.g., “I exercise because I want others to see me as physically fit”, “I exercise because I want others to see me as physically fit”) and reasons which have been introjected or partially internalized (e.g., “I exercise because I'd be afraid of falling too far out of shape”, “I exercise because I would feel bad about myself if I did not do it”). One interpretation for the present findings is that external demands and pressures to exercise in this study were perceived by participants as coming mostly from the intervention team. To the extent that this occurred, external contingencies and incentives, which normally could have been felt as controlling and a potential cause of anxiety, may have been perceived as normal, expected, and even positive by some participants. This was likely the case in the main intervention group, for whom introjected, integrated, and intrinsic exercise motivation were found to increase (compared to controls) at the end of an intervention which was overwhelmingly perceived as supporting participants' autonomy [31]. In fact, group differences in the psychological impact of introjected and/or external regulations may partially explain the generally nonsignificant results.
According to self-determination theory, satisfaction of competence, autonomy, and relatedness, the three basic psychological needs, provide a basis for predicting when the pursuit and attainment of goals will be associated with more positive versus more negative well-being outcomes [45]. In contrast, thwarted satisfaction of these needs results in negative functional consequences for mental health. Persistent deprivation of any need has costs for health and well-being, leading to the development of compensatory processes, such as substitute motives and non-autonomous regulatory styles, which are expected to result in worse well-being. Thus, need thwarting conditions lead to specifiable patterns of behaviors, regulations, goals, and affects that do not represent optimal development and well-being, which would occur in supportive environments [45]. Our findings suggest that, in the context of weight loss treatment, perceived need support and autonomous self-regulation will also lead to increased HRQOL and improved psychological well-being.
Several studies showed that weight loss is important in overweight and obese populations in part due to beneficial effects on HRQOL and psychological well-being. For example, Kolotkin and colleagues found that obesity-specific HRQOL changes were strongly related to weight reduction among 161 participants (88% women) [49]. Additionally, improved mood, affect, and psychological well-being may also facilitate the adoption and maintenance of behavior needed to regulate one's weight [30]. Thus, improving psychological well-being is not only ethically appropriate but could also be good clinical practice, to the extent that it contributes to enhanced treatment outcomes. Unfortunately, investigating predictors of psychological well-being in obesity treatment has not been the focus of much prior research. An additional ethical medical mandate is to promote patients' autonomy [50]. Interestingly, an increasing body of research shows that promoting autonomy is also advisable from a treatment efficacy viewpoint. For example, in weight loss and weight maintenance, more autonomous and intrinsic motivation have been shown to significantly predict more successful weight and exercise-related outcomes [3, 51–53].
In conclusion, this work supports predictions based on self-determination theory in relation to correlates of quality of live and psychological functioning. For obesity treatment, this study furthers our understanding of mechanisms associated with enhanced psychological outcomes, which is of direct relevance for health care providers in this field. Promoting self-determined motivation for health and health behaviors, particularly exercise, may positively influence a number of relevant psychological variables. Importantly, during weight control, these associations appear to hold independently of actual weight changes.
Acknowledgments
This study was funded by Grants by the Portuguese Science and Technology Foundation (FCT-POCI/DES/57705/2004 and SFRH/BD/31408/2006 to Paulo Vieira) and the Calouste Gulbenkian Foundation (Grant no. 65565/2004). The investigators are also grateful to the Oeiras City Council, Nestlé Portugal, and IBESA for their additional financial support.
References
- 1.Deci E, Ryan R. Intrinsic Motivation and Self-Determination in Human Behavior. New York, NY, USA: Plenum; 1985. [Google Scholar]
- 2.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 3.Williams GC, Grow VM, Freedman ZR, Ryan RM, Deci EL. Motivational predictors of weight loss and weight-loss maintenance. Journal of Personality and Social Psychology. 1996;70(1):115–126. doi: 10.1037//0022-3514.70.1.115. [DOI] [PubMed] [Google Scholar]
- 4.Pelletier LG, Fortier MS, Vallerand RJ, Brière NM. Associations among perceived autonomy support, forms of self-regulation, and persistence: a prospective study. Motivation and Emotion. 2001;25(4):279–306. [Google Scholar]
- 5.Deci E, Ryan R, editors. Handbook of Self-Determination Research. The University of Rochester Press; 2002. [Google Scholar]
- 6.Kahneman D, Diener E, Schwartz N, editors. Well-Being: The Foundations of Hedonic Psychology. New York, NY, USA: Russel Sage Found; 1999. [Google Scholar]
- 7.Diener E, Lucas RE. Personality and subjective well-being. In: Kahneman D, Diener E, Schwarz N, editors. Well-Being: The Foundations of Hedonic Psychology. 1999. pp. 213–229. [Google Scholar]
- 8.Ryan RM, Deci EL. On happiness and human potentials: a review of research on hedonic and eudaimonic well-being. Annual Review of Psychology. 2001;52:141–166. doi: 10.1146/annurev.psych.52.1.141. [DOI] [PubMed] [Google Scholar]
- 9.Waterman AS. Two conceptions of happiness: contrasts of personal expressiveness (eudaimonia) and hedonic enjoyment. Journal of Personality and Social Psychology. 1993;64(4):678–691. [Google Scholar]
- 10.Wilson PM, Longley K, Muon S, Rodgers WM, Murray TC. Examining the contributions of perceived psychological need satisfaction to well-being in exercise. Journal of Applied Biobehavioral Research. 2006;11(3-4):243–264. [Google Scholar]
- 11.Edmunds J, Ntoumanis N, Duda J. Understanding exercise adherence and psychological well-being from a self determination theory perspective among a cohort of obese patients referred to an exercise on prescription scheme. Psychology of Sport & Exercise. 2007;8:722–740. [Google Scholar]
- 12.Daley AJ, Maynard IW. Preferred exercise mode and affective responses in physically active adults. Psychology of Sport and Exercise. 2003;4(4):347–356. [Google Scholar]
- 13.Parfitt G, Gledhill C. The effect of choice of exercise mode on psychological responses. Psychology of Sport and Exercise. 2004;5(2):111–117. [Google Scholar]
- 14.Hagger M, Chatzisarantis N. Intrinsic Motivation and Self-Determination in Exercise and Sport. Human Kinetics; 2007. [Google Scholar]
- 15.Ekkekakis P, Lind E. Exercise does not feel the same when you are overweight: the impact of self-selected and imposed intensity on affect and exertion. International Journal of Obesity. 2006;30(4):652–660. doi: 10.1038/sj.ijo.0803052. [DOI] [PubMed] [Google Scholar]
- 16.Kolotkin RL, Meter K, Williams GR. Quality of life and obesity. Obesity Reviews. 2001;2(4):219–229. doi: 10.1046/j.1467-789x.2001.00040.x. [DOI] [PubMed] [Google Scholar]
- 17.Kushner RF, Foster GD. Obesity and quality of life. Nutrition. 2000;16(10):947–952. doi: 10.1016/s0899-9007(00)00404-4. [DOI] [PubMed] [Google Scholar]
- 18.Fontaine KR, Barofsky I. Obesity and health-related quality of life. Obesity Reviews. 2001;2(3):173–182. doi: 10.1046/j.1467-789x.2001.00032.x. [DOI] [PubMed] [Google Scholar]
- 19.Fontaine KR, Bartlett SJ. Estimating health-related quality of life in obese individuals. Disease Management and Health Outcomes. 1998;3(2):61–70. [Google Scholar]
- 20.Duval K, Marceau P, Pérusse L, Lacasse Y. An overview of obesity-specific quality of life questionnaires. Obesity Reviews. 2006;7(4):347–360. doi: 10.1111/j.1467-789X.2006.00244.x. [DOI] [PubMed] [Google Scholar]
- 21.Kolotkin RL, Norquist JM, Crosby RD, et al. One-year health-related quality of life outcomes in weight loss trial participants: comparison of three measures. Health and Quality of Life Outcomes. 2009;7 doi: 10.1186/1477-7525-7-53. Article ID 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Samsa GP, Kolotkin RL, Williams GR, Nguyen MH, Mendel CM. Effect of moderate weight loss on health-related quality of life: an analysis of combined data from 4 randomized trials of sibutramine vs placebo. American Journal of Managed Care. 2001;7(9):875–883. [PubMed] [Google Scholar]
- 23.Fine JT, Colditz GA, Coakley EH, et al. A prospective study of weight change and health-related quality of life in women. Journal of the American Medical Association. 1999;282(22):2136–2142. doi: 10.1001/jama.282.22.2136. [DOI] [PubMed] [Google Scholar]
- 24.Kolotkin RL, Head S, Hamilton M, Tse CK. Assessing impact of weight on quality of life. Obesity Research. 1995;3(1):49–56. doi: 10.1002/j.1550-8528.1995.tb00120.x. [DOI] [PubMed] [Google Scholar]
- 25.McMahon FG, Fujioka K, Singh BN, et al. Efficacy and safety of sibutramine in obese white and African American patients with hypertension: a 1-year, double-blind, placebo-controlled, multicenter trial. Archives of Internal Medicine. 2000;160(14):2185–2191. doi: 10.1001/archinte.160.14.2185. [DOI] [PubMed] [Google Scholar]
- 26.Engel SG, Crosby RD, Kolotkin RL, et al. Impact of weight loss and regain on quality of life: mirror image or differential effect? Obesity Research. 2003;11(10):1207–1213. doi: 10.1038/oby.2003.166. [DOI] [PubMed] [Google Scholar]
- 27.Blaine BE, Rodman J, Newman JM. Weight loss treatment and psychological well-being: a review and meta-analysis. Journal of Health Psychology. 2007;12(1):66–82. doi: 10.1177/1359105307071741. [DOI] [PubMed] [Google Scholar]
- 28.do Carmo I, Dos Santos O, Camolas J, et al. Overweight and obesity in Portugal: national prevalence in 2003–2005. Obesity Reviews. 2008;9(1):11–19. doi: 10.1111/j.1467-789X.2007.00422.x. [DOI] [PubMed] [Google Scholar]
- 29.Palmeira AL, Teixeira PJ, Branco TL, et al. Predicting short-term weight loss using four leading health behavior change theories. International Journal of Behavioral Nutrition and Physical Activity. 2007;4 doi: 10.1186/1479-5868-4-14. Article ID 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Palmeira AL, Markland DA, Silva MN, et al. Reciprocal effects among changes in weight, body image, and other psychological factors during behavioral obesity treatment: a mediation analysis. International Journal of Behavioral Nutrition and Physical Activity. 2009;6 doi: 10.1186/1479-5868-6-9. Article ID 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Silva MN, Vieira PN, Coutinho SR, et al. Using self-determination theory to promote physical activity and weight control: a randomized controlled trial in women. Journal of Behavioral Medicine. 2010;33(2):110–122. doi: 10.1007/s10865-009-9239-y. [DOI] [PubMed] [Google Scholar]
- 32.Silva MN, Markland D, Minderico CS, et al. A randomized controlled trial to evaluate self-determination theory for exercise adherence and weight control: rationale and intervention description. BMC Public Health. 2008;8 doi: 10.1186/1471-2458-8-234. Article ID 234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sheldon KM, Ryan R, Reis HT. What makes for a good day? Competence and autonomy in the day and in the person. Personality and Social Psychology Bulletin. 1996;22(12):1270–1279. [Google Scholar]
- 34.Ryan RM, Connell JP. Perceived locus of causality and internalization: examining reasons for acting in two domains. Journal of Personality and Social Psychology. 1989;57(5):749–761. doi: 10.1037//0022-3514.57.5.749. [DOI] [PubMed] [Google Scholar]
- 35.Ware J, et al. SF-36 Health Survey Manual and Interpretation Guide. Boston, Mass, USA: New England Medical Center, The Health Institute; 1993. [Google Scholar]
- 36.Lopes Ferreira P. The development of the Portuguese version of the MOS SF-36. Part II—validation testing. Acta Medica Portuguesa. 2000;13(3):119–127. [PubMed] [Google Scholar]
- 37.Kolotkin RL, Crosby RD. Psychometric evaluation of the impact of weight on quality of life-lite questionnaire (IWQOL-Lite) in a community sample. Quality of Life Research. 2002;11(2):157–171. doi: 10.1023/a:1015081805439. [DOI] [PubMed] [Google Scholar]
- 38.Engel SG, Kolotkin RL, Teixeira PJ, et al. Psychometric and cross-national evaluation of a Portuguese version of the Impact of Weight on Quality of Life-Lite (IWQOL-Lite) questionnaire. European Eating Disorders Review. 2005;13(2):133–143. [Google Scholar]
- 39.Rosenberg M. Society and the Adolescent Self-Image. Princeton, NJ, USA: Princeton University Press; 1965. [Google Scholar]
- 40.Azevedo A, Faria L. Formas e Contextos. Braga, Portugal: Universidade do Minho; 2004. Self-esteem in the scholl' secondary level:validation of the Rosenberg Self-Esteem Scale, Avaliação Psicológica; pp. 415–421. [Google Scholar]
- 41.Beck A, Steer R. Manual for the Beck Depression Inventory. New York, NY, USA: Psychological Corporation; 1987. [Google Scholar]
- 42.Cunha JA. Manual for the Portuguese Version of Beck' Scales. São Paulo, Brazil: The Psychological Corporation; 2001. [Google Scholar]
- 43.Spielberger CD, Vagg PR. Psychometric properties of the STAI: a reply to Ramanaiah, Franzen, and Schill. Journal of Personality Assessment. 1984;48(1):95–97. doi: 10.1207/s15327752jpa4801_16. [DOI] [PubMed] [Google Scholar]
- 44.Cohen J, Cohen P. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. 3nd edition. Mahwah, NJ, USA: Lawrence Erlbaum Associates; 2003. [Google Scholar]
- 45.Deci EL, Ryan RM. The "what" and "why" of goal pursuits: human needs and the self-determination of behavior. Psychological Inquiry. 2000;11(4):227–268. [Google Scholar]
- 46.Ryan RM, Plant RW, O’Malley S. Initial motivations for alcohol treatment: relations with patient characteristics, treatment involvement, and dropout. Addictive Behaviors. 1995;20(3):279–297. doi: 10.1016/0306-4603(94)00072-7. [DOI] [PubMed] [Google Scholar]
- 47.Deci EL, Ryan RM. Facilitating optimal motivation and psychological well-being across life’s domains. Canadian Psychology. 2008;49(1):14–23. [Google Scholar]
- 48.Kernis MH, Paradise AW, Whitaker DJ, Wheatman SR, Goldman BN. Master of one’s psychological domain? Not likely if one’s self-esteem is unstable. Personality and Social Psychology Bulletin. 2000;26(10):1297–1305. [Google Scholar]
- 49.Kolotkin RL, Crosby RD, Williams GR, Hartley GG, Nicol S. The relationship between health-related quality of life and weight loss. Obesity Research. 2001;9(9):564–571. doi: 10.1038/oby.2001.73. [DOI] [PubMed] [Google Scholar]
- 50.Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 3rd edition. Oxford, UK: Oxford University Press; 1989. [Google Scholar]
- 51.Silva MN, et al. Mediators of different types of physical activity during behavioral obesity treatment. Psychology of Sport and Exercise. 2010;11:591–601. [Google Scholar]
- 52.Teixeira PJ, Going SB, Houtkooper LB, et al. Exercise motivation, eating, and body image variables as perdictors of weight control. Medicine and Science in Sports and Exercise. 2006;38(1):179–188. doi: 10.1249/01.mss.0000180906.10445.8d. [DOI] [PubMed] [Google Scholar]
- 53.Teixeira PJ, Silva MN, Coutinho SR, et al. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity. 2010;18(4):725–735. doi: 10.1038/oby.2009.281. [DOI] [PubMed] [Google Scholar]