Abstract
Objectives
The study objectives were to evaluate adequacy of prenatal care and risk for preterm birth among Medicaid clients in Virginia and to determine if payment method is associated with the risk of preterm birth.
Methods
Birth certificate data for the Commonwealth of Virginia for 2007 and 2008 were linked with Medicaid claims data. Analysis was limited to singleton births. Three payment methods were evaluated: private insurance, self-pay, and Medicaid. The prevalence of preterm birth for each level of prenatal care defined by the Kotelchuck prenatal care index was assessed for each payment method. Unconditional logistic regression modeling was used to assess the association between payment method and preterm birth risk while controlling for known preterm birth risk factors.
Results
Preterm birth prevalences (95% confidence interval [CI]) for the different payment methods were 7.9% (4.79-8.07) for the privately insured, 10.1% (9.57-10.60) for the self-pay group, and 10.2% (9.95-10.45) for Medicaid recipients. Compared with those with private insurance, women on Medicaid had an adjusted odds ratio (OR) for preterm birth (95% CI) of 0.99 (0.94-1.03). Self-pay mothers had a 32% increase in the odds of preterm birth relative to the privately insured. All payment groups show a trend toward significant reduction in preterm birth prevalence as adequacy of prenatal care improved from inadequate to adequate. Medicaid enrollees had a high prevalence of known risk factors, including smoking and illicit drug use and cervical insufficiency.
Conclusions
When known risk factors have been controlled, preterm birth risk for Medicaid enrollees did not differ significantly from the privately insured.
Introduction
Together, preterm birth and low birth weight account for more than 70% of all neonatal morbidity and mortality.1 Risk factors associated with preterm birth include cigarette smoking, alcohol and illicit drug use, delayed or inadequate prenatal care, race/ethnicity, deficiency of nutritional factors (e.g., iron, folic acid, vitamin D) during pregnancy, low educational attainment, poverty, and genetic factors.2 One of the vehicles state and the federal governments have employed to improve pregnancy outcomes among impoverished women is Medicaid, a cofunded program that aims at improving access to and adequacy of prenatal care for poor and medically needy populations.
The federal minimum Medicaid eligibility level is 133% of the federal poverty level,3 but states cover pregnant women with incomes ranging from the federal minimum in Alabama, Colorado, Idaho, Montana, Nevada, North Dakota, Oregon, Virginia, and Wyoming to 300% of the federal poverty level in New Hampshire, Wisconsin, Iowa, Hawaii, Vermont, and the District of Columbia. This includes populations that are covered under Medicaid waivers or the Children's Health Insurance Program (CHIP) or both (www.statehealthfacts.org/). From 1985 through 1998, the proportion of pregnant women whose healthcare was supported by Medicaid increased from 17% to 35%.4
Evaluations of the impact of Medicaid sponsorship on pregnancy outcomes have been reported previously. Krieger et al.5 found significant differences between Medicaid and non-Medicaid enrollees of managed care plans in both prenatal care use and birth outcome in Washington State. The Medicaid group had enrolled in care for fewer months of pregnancy, had a higher prevalence of smokers, and also had a higher mean number of prior preterm pregnancies. Whereas only 2.3% of the non-Medicaid members enrolled during the last trimester of pregnancy, among the Medicaid group, the proportion was 25.3%. After adjusting for known risk factors, the difference in low birth weight risk between the Medicaid and non-Medicaid women was not statistically significant. Another study that compared obstetric care in Medicaid and privately insured women who entered prenatal care at low risk in Washington State found no significant differences in preterm birth rates.6 The two groups showed similar prenatal care and resource use.
A study that compared birth outcomes between Medicaid enrollees and non-Medicaid mothers residing in low-income or high-income areas in California reported a statistically significant difference in low birth weight risk between short-term Medicaid enrollees (enrollment for 0–3 months of pregnancy) and non-Medicaid women residing in high-income areas.7 As noted by the authors, however, Medicaid eligibility procedures in California during the study period allowed for retroactive enrollment after experiencing a high-cost delivery, and this may have inflated low birth rates among the Medicaid recipients. Examination of the impact of Medicaid expansion in prenatal care access on birth outcomes in Florida during the period 1989–1994 found similar low birth weight rates between Medicaid enrollees receiving care in the public health system and women with private insurance.8 Higher birth weight rate was reported for Medicaid women receiving care in the private system. Using data from the National Maternal and Infant Health Survey, Kaestner9 found evidence that Medicaid recipients received less prenatal care than privately insured women. There was, however, no evidence that Medicaid recipients received lower-quality prenatal care than the privately insured.
These studies on Medicaid effectiveness must be placed in a regional context, as the preterm birth and low birth weight rates differ substantially across the United States.10,11 The Southeast has the highest preterm birth, with rates ranging from 12.1% in Virginia to 18.3% in Mississippi. Enhanced services, including psychosocial, nutritional, health promotion assessment, counseling, and referral to public health and social services that some Medicaid programs offer, have reduced preterm births in states and regions with low preterm birth rates, but such programs have not been uniformly successful in the Southeast region.12
Demographic and socioeconomic characteristics of women enrolled in Medicaid programs may increase their risk for adverse birth outcomes. A criterion for Medicaid eligibility during pregnancy is the pregnancy itself; thus, a woman's insurance status before becoming eligible for Medicaid is a major determinant of when prenatal care is initiated. Medicaid women also engage in high-risk behaviors, for example, cigarette smoking and illicit drug use, is greater than women on private insurance,5,13,14 but the effect that method of payment has on preterm birth has not been fully explored, especially in regions with a high prevalence of preterm birth and low birth weight.
The objectives of the present study were to evaluate the adequacy of prenatal care and risk for prematurity among Medicaid clients in Virginia, a state whose antenatal Medicaid program has not heretofore been critically examined, and to determine if method of payment is associated with the risk of preterm birth.
Materials and Methods
Birth certificate data for all live births in the Commonwealth of Virginia for 2007 and 2008 were linked with Medicaid claims data from the same time interval. The purpose of the linkage was to ensure that all Medicaid recipients had been correctly identified. Over 99% of records were successfully matched. To eliminate the confounding effect that twin and any higher order gestation may have on the outcome, analysis was limited to singleton births. The small fraction of records with missing gestational age (0.02%) or payment information (2.3%) was excluded from analysis. Comparison of birth weights between mothers with and without missing gestational age or payment information showed no systematic differences. Preterm birth was defined as birth before 37 completed weeks of gestation. Variables on the birth certificate data included mother's demographic information, history of tobacco and illicit drug use, pregnancy and obstetrics history, number of previous live births who are living, number of previous live births who are dead, medical history, number of previous pregnancy terminations, payment source, and information on the baby. Three payment methods were analyzed: private insurance, self-pay, and Medicaid. Covariates included race, mother's age and education level, previous pregnancy history, medical history of the pregnancy, tobacco and illicit drug use, and adequacy of prenatal care. The Kotelchuck prenatal care index was used to assess adequacy of prenatal care (www.mchlibrary.info/databases/HSNRCPDFs/APNCU994_20SAS.pdf/).
Proportions of the various maternal characteristics by payment method were computed, and group differences were assessed using the chi-square test of association. Ethnicity/race was self-reported. The prevalence of preterm birth within each level of maternal characteristic was assessed for each payment method. Odds ratios (ORs) for the association between each covariate and preterm birth were computed. All clinically significant variables and any variable showing a p value of ≤0.25 from the crude analysis were considered candidates for the multivariate model. Unconditional logistic regression modeling was used to assess the association between payment method and preterm risk while controlling for known preterm risk factors. Model adequacy was assessed using the Hosmer and Lemeshow goodness-of-fit statistic. SAS 9.2 was used for statistical analysis (SAS Institute, Cary, NC).
Results
For the period 2007–2008, there were 219,666 live births recorded in Virginia, with 211,724 being singleton births. An analysis of method of payment revealed that 55,206 (26.7%) of the singleton births were paid for by Medicaid, 138,205 (66.8%) were paid for by private insurance, and 13,491 (6.5%) were classified as self-pay. There were 4,822 records where method of payment was not known. Of all Medicaid recipients, 58.8% were white, 36.2% were black, and the rest were either Asians or women of other races (Table 1). Medicaid enrollees represented a much higher proportion of births among teenagers and among mothers with a high school education or less. Over half of all pregnancies in unmarried women were paid for by Medicaid. The proportions of married women within the Medicaid, self-pay, and privately insured, groups were 27.8%, 42.0%, and 80.5%, respectively. The proportion of mothers who had no prenatal visit was 0.2% for the privately insured, 1.6% for Medicaid enrollees, and 7.6% for women with self-pay status. Whereas only 6.0% of the privately insured had inadequate prenatal care, among the Medicaid and self-pay groups, the proportions were 18.2%, and 31.7%, respectively. The prevalence of tobacco, methadone, marijuana, and cocaine use was highest among the Medicaid group. More than 60% of women who used tobacco or illicit drugs (methadone, heroin, cocaine, marijuana) were Medicaid beneficiaries. It should, however, be noted that unlike tobacco use, where data collected were virtually complete (<0.01% of records had missing data), each illicit drug had 1.4% of records with missing data.
Table 1.
Method of Payment According to Various Maternal Characteristics Among Singleton Live Births in Virginia, 2007–2008
| Characteristic | Medicaid (%) | Private insurance (%) | Self-pay (%) |
|---|---|---|---|
| Race | |||
| White | 58.8 | 71.7 | 63.9 |
| Black | 36.2 | 17.9 | 16.8 |
| Asian | 2.0 | 8.2 | 4.8 |
| Other | 3.1 | 2.2 | 14.5 |
| Age group | |||
| ≤19 | 18.5 | 4.4 | 11.9 |
| 20–24 | 39.5 | 17.2 | 28.4 |
| 25–34 | 35.8 | 58.7 | 48.1 |
| 35+ | 6.2 | 19.7 | 11.6 |
| Mother's education level | |||
| High school or less | 78.2 | 30.9 | 76.0 |
| College | 21.8 | 69.1 | 24.0 |
| Prenatal visits | |||
| None | 1.6 | 0.2 | 7.6 |
| 1–4 | 4.7 | 1.6 | 8.4 |
| 5–9 | 24.3 | 16.2 | 35.8 |
| 10–14 | 56.2 | 66.8 | 43.7 |
| 15–19 | 11.3 | 12.8 | 3.8 |
| 20+ | 1.9 | 2.5 | 0.7 |
| Prenatal care adequacy | |||
| Inadequate | 18.2 | 6.0 | 31.7 |
| Intermediate | 11.3 | 11.0 | 17.2 |
| Adequate | 41.9 | 53.3 | 36.2 |
| Adequate plus | 28.6 | 29.8 | 14.9 |
| Marital status (married) | 27.8 | 80.5 | 42.0 |
| Tobacco use | 15.0 | 3.0 | 5.3 |
| Methadone use | 0.21 | 0.03 | 0.13 |
| Heroin use | 0.09 | 0.01 | 0.13 |
| Marijuana use | 1.32 | 0.12 | 0.56 |
| Cocaine use | 0.51 | 0.04 | 0.47 |
| No. of pregnancy terminations | |||
| None | 79.5 | 79.7 | 83.2 |
| 1 | 13.7 | 13.6 | 11.9 |
| 2 | 4.4 | 4.5 | 3.4 |
| ≥3 | 2.5 | 2.2 | 1.5 |
| Incompetent cervix | 0.21 | 0.25 | 0.15 |
| Previous preterm delivery | 1.04 | 0.75 | 1.04 |
| History of diabetes | 4.02 | 5.17 | 3.54 |
| Pregnancy induced hypertension | 3.5 | 3.53 | 2.28 |
| n (Total) | 55,206 | 138,205 | 13,491 |
All records with missing values for maternal characteristic or method of payment were excluded from analysis.
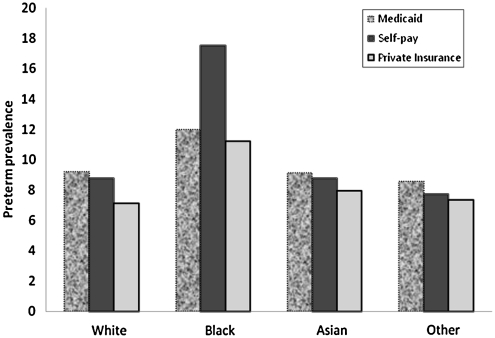
Preterm birth prevalences (95% confidence interval [CI]) for the different payment methods were 7.9% (4.79-8.07) for the privately insured, 10.1% (9.57-10.60) for self-pay, and 10.2% (9.95-10.45) for Medicaid recipients. Among whites, Asians, and those of other ethnicities, Medicaid recipients had the highest preterm birth prevalence. For blacks, however, the highest preterm birth rate was recorded among those who self-paid for delivery services (Table 2 and Fig. 1). Among all ethnic groups, the privately insured had the lowest preterm birth prevalence (Table 2).
Table 2.
Method of Payment and Preterm Birth Prevalence by Maternal Characteristics, Virginia, 2007–2008
| |
Preterm prevalence (%) |
|||
|---|---|---|---|---|
| Variable | Medicaid | Private insurance | Self-pay | p valuea |
| Race | ||||
| White | 9.2 | 7.1 | 8.8 | <0.001 |
| Black | 12 | 11.2 | 17.5 | <0.001 |
| Asian | 9.1 | 7.9 | 8.8 | 0.30 |
| Other | 8.6 | 7.3 | 7.7 | 0.30 |
| Age group | ||||
| ≤19 | 10.3 | 9.8 | 13.2 | <0.001 |
| 20–24 | 9.7 | 8.1 | 10.1 | <0.001 |
| 25–34 | 10.2 | 7.4 | 9.1 | <0.001 |
| 35+ | 13.1 | 9 | 10.6 | <0.001 |
| Mother's education level | ||||
| High school or less | 10.3 | 9 | 10.5 | <0.001 |
| College | 9.5 | 7.4 | 8.5 | <0.001 |
| Prenatal care adequacy | ||||
| Inadequate | 11.3 | 9.1 | 11.8 | <0.001 |
| Intermediate | 4 | 3.4 | 2.2 | <0.001 |
| Adequate | 2.8 | 2.4 | 3.6 | <0.001 |
| Adequate plus | 22.5 | 19.2 | 30.5 | <0.001 |
| Marital status | ||||
| Married | 9.9 | 7.5 | 8.1 | <0.001 |
| Not married | 10.3 | 9.9 | 11.5 | <0.001 |
| Tobacco use | ||||
| Yes | 11.3 | 10.5 | 21.4 | <0.001 |
| No | 10 | 7.9 | 9.4 | <0.001 |
| Methadone use | ||||
| Yes | 21.7 | 26.2 | 41.2 | 0.22 |
| No | 10.2 | 7.9 | 10 | <0.001 |
| Heroin use | ||||
| Yes | 19.6 | 27.3 | 66.7 | 0.001 |
| No | 10.2 | 7.9 | 10 | <0.001 |
| Marijuana use | ||||
| Yes | 15.3 | 13 | 27.4 | 0.03 |
| No | 10.1 | 7.9 | 10 | <0.001 |
| Cocaine use | ||||
| Yes | 20.6 | 18.3 | 39.7 | 0.003 |
| No | 10.1 | 7.9 | 9.9 | <0.001 |
| Incompetent cervix | ||||
| Yes | 55.7 | 32.7 | 60 | <0.001 |
| No | 10.1 | 7.9 | 10 | <0.001 |
| Previous preterm delivery | ||||
| Yes | 34.4 | 26.1 | 35.5 | <0.001 |
| No | 9.9 | 7.8 | 9.8 | <0.001 |
| History of diabetes | ||||
| Yes | 13.8 | 12.3 | 13 | 0.20 |
| No | 10.1 | 7.7 | 10 | <0.001 |
| Pregnancy-induced hypertension | ||||
| Yes | 20.9 | 20.4 | 20.5 | 0.92 |
| No | 9.8 | 7.5 | 9.8 | <0.001 |
Chi-square test for difference in preterm birth prevalence among the different payment methods.
FIG. 1.
Payment method and prevalence of preterm birth by mother's race among singleton live births in Virginia, 2007–2008.
Across the three payment methods, women receiving intermediate or adequate prenatal care, defined by the Kotelchuck prenatal care index, had preterm birth rates that were less than half the rates of those who received inadequate care. Preterm birth rates among women determined to have had more than adequate prenatal care (i.e., the adequate plus group) were more than twice the prevalence rates for those who received inadequate care (Table 2). A closer examination of the adequate plus group revealed that it comprised approximately 58% of all women with a history of incompetent cervix, 48% of women with pregnancy-induced hypertension, and 44% of all women with a history of a prior preterm delivery (data not shown). A subanalysis of the adequate plus group showed the percentages of women with incompetent cervix within the different payment types to be 60% for Medicaid, 57% for private insurance, and 50% for self-pay.
For women with a history of previous preterm birth, the percentages were 42% for Medicaid, 46% for private insurance, and 30% for self-pay. Women with self-pay status had the least percentage of pregnancy-induced hypertension (30%). The pregnancy-related hypertension percentages among the Medicaid and privately insured groups were 46% and 50%, respectively (data not shown). Tobacco or illicit drug users had preterm rates that were significantly higher than those of nonusers. As expected, a very high preterm prevalence (20.4%–60%) was recorded among women with a history of a previous preterm birth, an incompetent cervix, or pregnancy-induced hypertension (Table 2).
In the multivariate logistic regression that adjusted for known preterm birth risk factors, the preterm birth risk for Medicaid recipients was not significantly different from that of the privately insured. Compared with those with private insurance, women on Medicaid had an adjusted OR (95% CI) for preterm birth of 0.99 (0.94-1.03) (Table 3). Self-pay mothers had a 32% increase in odds of preterm birth relative to the privately insured. The percentage of self-pay women who received inadequate prenatal care was 27.5% for whites, 28.5% for Asians, and 36.1% for blacks (data not shown).
Table 3.
Crude and Adjusted Odds Ratio for Preterm Birth by Maternal Characteristics Among Singleton Live Births in Virginia, 2007–2008
| |
Preterm birth |
|
|---|---|---|
| Variable | Crude OR (95% CI) | Adjusted ORa(95% CI) |
| Race (ref = white) | ||
| Black | 1.60 (1.55-1.66) | 1.47 (1.41-1.53) |
| Asian | 1.05 (0.98-1.12) | 1.15 (1.07-1.24) |
| Other | 1.01 (0.92-1.10) | 1.01-0.91-1.11) |
| Age group (ref = 20–24) | ||
| ≤19 | 1.18 (1.12-1.25) | 1.04 (0.97-1.11) |
| 25–34 | 0.89 (0.86-0.92) | 1.00 (0.96-1.05) |
| 35+ | 1.07 (1.02-1.12) | 1.19 (1.13-1.27) |
| Mother's education level (ref = college) | ||
| High school or less | 1.30 (1.26-1.34) | 1.25 (1.20-1.30) |
| Prenatal care adequacy (ref = adequate) | ||
| Inadequate | 4.53 (4.28-4.79) | 3.87 (3.64-4.12) |
| Intermediate | 1.37 (1.27-1.48) | 1.32 (1.22-1.44) |
| Adequate plus | 9.88 (9.46-10.32) | 9.61 (9.19-10.06) |
| Marital status (ref = married) | 1.36 (1.32-1.40) | 1.09 (1.04-1.13) |
| Tobacco use | 1.41 (1.34-1.49) | 1.10 (1.03-1.17) |
| Methadone use | 3.36 (2.37-4.77) | 2.30 (1.54-3.44) |
| Heroin use | 4.37 (2.66-7.17) | 2.22 (1.27-3.90) |
| Marijuana use | 1.98 (1.66-2.36) | 1.32 (1.08-1.61) |
| Cocaine use | 3.17 (2.51-4.02) | 1.94 (1.47-2.54) |
| Incompetent cervix | 7.07 (5.91-8.46) | 4.16(3.37-5.13) |
| Previous preterm delivery | 4.51 (4.07-5.00) | 3.71 (3.30-4.17) |
| History of diabetes | 1.58 (1.49-1.68) | 1.10 (1.03-1.18) |
| Pregnancy-induced hypertension | 2.89 (2.73-3.07) | 2.11 (1.97-(2.25) |
| Method of Payment (ref = private insurance) | 1.32 (1.28-1.36) | 0.99 (0.94-1.03) |
| Medicaid | ||
| Self-pay | 1.30 (1.23-1.38) | 1.32 (1.23-1.42) |
Other covariates adjusted for were gender of child, number of live births who are living, and number of live births who are dead.
CI, confidence interval; OR, odds ratio; ref, reference group.
The strongest predictors of preterm birth were incompetent cervix, previous preterm delivery, pregnancy-induced hypertension, illicit drug use, and adequacy of prenatal care (Table 3). The preterm birth risk for mothers with incompetent cervix was about four times higher than that of those with no history of incompetent cervix. Women with a history of previous preterm delivery had a preterm risk that was more than three times the risk for those with no such history (OR [95% CI] 3.71 [3.30-4.17]). Mothers who had pregnancy-induced hypertension also had a 2-fold increase in preterm birth risk. Methadone and heroin use were each associated with a 2-fold increase in preterm birth risk. Compared with those who received adequate prenatal care, women receiving inadequate and intermediate care had ORs (95% CI) of 3.87 (3.64-4.12) and 1.32 (1.22-1.44), respectively. Mothers in the adequate plus group had preterm birth risk that was about nine times the risk of those who received adequate prenatal care (OR [95% CI] 9.61 [9.19-10.06]). It is worth noting, however, that the group that received more than adequate care had the highest proportion of women with an incompetent cervix, pregnancy-induced hypertension, and a history of a previous preterm birth. Relative to whites, blacks had an OR (95% CI) of 1.47 (1.41-1.53). Other variables that showed significant association with preterm birth included education level, marital status, history of diabetes, and tobacco use. Pregnancy-related variables, such as the number of live births living, number of live births dead, and sex of the child (effect estimates not shown), also showed significant association with preterm birth.
Discussion
The Medicaid group in our study was younger, and approximately 30% received intermediate or inadequate prenatal care. Medicaid enrollees also had a high prevalence of smoking and illicit drug use, but when known risk factors were controlled for, preterm birth risk for Medicaid enrollees did not differ significantly from that of the privately insured. This finding is consistent with what we reported in a recent review of birth outcomes among Medicaid recipients nationally.12 In a study examining gestational age distributions among preterm births by insurance status, Branden et al.15 found no differences in gestational age at birth between Medicaid recipients on managed care and privately insured women. Babies delivered to women on private insurance were, however, found to have a higher mean birth weight. Dobie et al.6 also found no significant differences in preterm birth rates between Medicaid and privately insured women who entered prenatal care at low risk.
The main risk factors contributing to preterm birth among Medicaid enrollees, in rank order, were cervical incompetence, illicit drug use, inadequate prenatal care, and tobacco use. Other risk factors included younger age and number of years of education.
Women with self-pay status for prenatal and delivery services had a 32% increase in preterm birth risk compared with those with private insurance. The self-pay women were the group most likely to have no prenatal visits and the least likely to have adequate prenatal care (Table 1). With the exception of women who received prenatal care that was categorized as adequate plus, all payment groups showed a trend toward significant reduction in preterm birth prevalence as adequacy of prenatal care improved from inadequate to adequate. Women in the adequate plus group received more attention because of severe medical conditions or pregnancy complications likely to increase their risk for preterm delivery. A higher number of prenatal care visits resulting in increased risk for preterm birth would seem counterintuitive, but the Kotelchuck prenatal care index uses two prenatal care indices, number of prenatal visits and month when prenatal care started, to arrive at a composite prenatal care adequacy. This group of women with medical conditions likely to increase their risk for preterm birth would, therefore, show a prenatal care index that is much higher than what is considered adequate.
The increased preterm birth risk for blacks, relative to whites, has been consistently reported. This study shows blacks with a 47% increase in risk for preterm birth compared with whites. The underlying factors that cause the racial/ethnic disparities in preterm birth in the United States are not well understood. Factors that have been proposed to contribute to the disparities in birth outcomes between whites and blacks include genetics, behavioral and socioeconomic factors, maternal stress, and racism.2,16 Giscombé and Lobel16 noted that explanations advanced to explain ethnic disparities in preterm birth (i.e., higher levels of stress and greater susceptibility to stress in African American women; impact of racism; ethnic differences in stress-related neuroendocrine, vascular, and immunological processes; health behaviors, and socioeconomic status) each have merit, although none sufficiently explains the white/black ethnic disparities in adverse birth outcomes. Genetic and biological factors accounting for the white/black disparity in birth outcomes may not be modifiable, but several other factors originating from the physical and social environments and maternal health behaviors may be targets for change.17
The period 1991–2004 saw a 10-fold increase in the number of Medicaid beneficiaries enrolled in some form of managed care (from 2.7 million to 27 million), in the United States, with approximately 60% of all Medicaid enrollees receiving benefits through managed care in 2004 (www.cms.hhs.gov). The rationale for most states moving toward managed care is based on presumed cost saving, improved access, and continuity of care. In a national evaluation of the impact of Medicaid managed care on infant health, Kaestner et al.,18 found no evidence that the move to managed care within Medicaid caused improvements in prenatal care or in infant health. In a review of the impact of Medicaid expansions for pregnant women, Howell19 reported improvement in the use of prenatal care services among low-income women. Most of the studies reviewed, however, reported no effect of the eligibility expansion on preterm birth. Preterm birth and low birth weight rates have been shown not to differ between Medicaid recipients in managed care and those in traditional fee-for-service.20–29
Several study limitations deserve mention. Whereas we may be certain about the completeness of the Medicaid data, we cannot say the same for the private insurance and self-pay groups, as we had no payment source information for 2% of the data. As was noted earlier, however, there was no systematic difference between this group of women and the group with known payment source information. Number of prenatal visits is one of the indices used in the computation of the Kotelchuck prenatal care index, and because women who had early premature deliveries would not have had the time to complete the required number of prenatal visits, their fewer number of prenatal visits would be a consequence of the premature delivery. Linking birth certificate data with Medicaid enrollment or claims data is prone to selection bias, which tends to underrepresent outcomes of high-risk pregnancies. Preterm rates for Medicaid recipients may thus be underreported.30,31 Our analytic dataset had almost complete information on all Medicaid recipients; thus, selection bias is not likely to be an issue in this analysis.
The findings from this study show that the majority of women with inadequate prenatal care were Medicaid recipients. When known risk factors for prematurity have been controlled for, however, Medicaid as a method of payment for prenatal care and delivery services does not increase a woman's risk for preterm birth. The fact that similar findings have been reported from other states argues strongly in favor of a focus on the approachable underlying factors associated with prematurity as a means to reduce preterm birth rates. Modifiable factors, particularly those related to maternal behavior, including cigarette smoking, illicit drug use, and inadequate prenatal care, should be targeted to reduce preterm birth risk. To the extent that inadequate prenatal care among Medicaid women is due to eligible women delaying enrollment until late in pregnancy, outreach efforts to patients and providers could shorten this delay and, potentially, further improve the outcomes seen among Medicaid insured women. Incompetent cervix, a known risk factor for preterm birth, is strongly associated with the number of previous pregnancy terminations. Preventing unwanted pregnancies through improved family planning services would reduce the number of pregnancy terminations a woman is likely to have and, thus, reduce her risk for cervical incompetence.
Acknowledgments
This work was supported by NIH grant P60 MD002256.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Mathews TJ. MacDorman MF. National vital statistics reports. 2. Vol. 57. Hyattsville, MD: National Center for Health Statistics; 2008. Infant mortality statistics from the 2005 period linked birth/infant death data set. [PubMed] [Google Scholar]
- 2.Anum EA. Springel EH. Shriver MD. Strauss JF III. Genetic contributions to disparities in preterm birth. Pediatr Res. 2009;65:1–9. doi: 10.1203/PDR.0b013e31818912e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenbaum S. Medicaid and national health care reform. N Engl J Med. 2009;361:2009–2012. doi: 10.1056/NEJMp0909449. [DOI] [PubMed] [Google Scholar]
- 4.Adams EK. Gavin NI. Handler A. Manning W. Raskind-Hood C. Transitions in insurance coverage from before pregnancy through delivery in nine states, 1996–1999. Health Aff (Millwood) 2003;22:219–229. doi: 10.1377/hlthaff.22.1.219. [DOI] [PubMed] [Google Scholar]
- 5.Krieger JW. Connell FA. LoGerfo JP. Medicaid prenatal care: A comparison of use and outcomes in fee-for-service and managed care. Am J Public Health. 1992;82:185–190. doi: 10.2105/ajph.82.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dobie S. Hart LG. Fordyce M. Andrilla CH. Rosenblatt RA. Obstetric care and payment source: Do low-risk Medicaid women get less care? Am J Public Health. 1998;88:51–56. doi: 10.2105/ajph.88.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howell EM. Herz EJ. Wang RH. Hirsch MB. A comparison of Medicaid and non-Medicaid obstetrical care in California. Health Care Financ Rev. 1991;12:1–15. [PMC free article] [PubMed] [Google Scholar]
- 8.Susan Marquis M. Long SH. The role of public insurance and the public delivery system in improving birth outcomes for low-income pregnant women. Med Care. 2002;40:1048–1059. doi: 10.1097/00005650-200211000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Kaestner R. Health insurance, the quantity and quality of prenatal care, and infant health. Inquiry. 1999;36:162–175. [PubMed] [Google Scholar]
- 10.Hamilton BE. Martin JA. Ventura SJ. National vital statistics reports, web release. 12. Vol. 57. Hyattsville, MD: National Center for Health Statistics; 2009. Births: Preliminary data for 2007. [Google Scholar]
- 11.Mathews TJ. MacDorman MF. Infant mortality statistics from the 2004 period linked birth/infant death data set. Natl Vital Stat Rep. 2007;55:1–32. [PubMed] [Google Scholar]
- 12.Anum EA. Retchin SM. Strauss JF. Medicaid and preterm birth and low birth weight: The last two decades. J Womens Health. 2010;19:443–451. doi: 10.1089/jwh.2009.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwethelm B. Margolis LH. Miller C. Smith S. Risk status and pregnancy outcome among Medicaid recipients. Am J Prev Med. 1989;5:157–163. [PubMed] [Google Scholar]
- 14.Buchi KF. Varner MW. Chase RA. The prevalence of substance abuse among pregnant women in Utah. Obstet Gynecol. 1993;81:239–242. [PubMed] [Google Scholar]
- 15.Brandon GD. Adeniyi-Jones S. Kirkby S. Webb D. Culhane JF. Greenspan JS. Are outcomes and care processes for preterm neonates influenced by health insurance status? Pediatrics. 2009;124:122–127. doi: 10.1542/peds.2008-1318. [DOI] [PubMed] [Google Scholar]
- 16.Giscombé CL. Lobel M. Explaining disproportionately high rates of adverse birth outcomes among African Americans: The impact of stress, racism, and related factors in pregnancy. Psychol Bull. 2005;131:662–683. doi: 10.1037/0033-2909.131.5.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bryant AS. Worjoloh A. Caughey AB. Washington AE. Racial/ethnic disparities in obstetric outcomes and care: Prevalence and determinants. Am J Obstet Gynecol. 2010;202:335–343. doi: 10.1016/j.ajog.2009.10.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaestner R. Dubay L. Kenney G. Managed care and infant health: An evaluation of Medicaid in the US. Soc Sci Med. 2005;60:1815–1833. doi: 10.1016/j.socscimed.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 19.Howell EM. The impact of the Medicaid expansions for pregnant women: A synthesis of the evidence. Med Care Res Rev. 2001;58:3–30. doi: 10.1177/107755870105800101. [DOI] [PubMed] [Google Scholar]
- 20.Oleske DM. Branca ML. Schmidt JB. Ferguson R. Linn ES. A comparison of capitated and fee-for-service Medicaid reimbursement methods on pregnancy outcomes. Health Serv Res. 1998;33:55–73. [PMC free article] [PubMed] [Google Scholar]
- 21.Levinson A. Ullman F. Medicaid managed care and infant health. J Health Econ. 1998;17:351–368. doi: 10.1016/s0167-6296(97)00031-3. [DOI] [PubMed] [Google Scholar]
- 22.Freund DA. Rossiter LF. Fox PD, et al. Evaluation of the Medicaid competition demonstrations. Health Care Financ Rev. 1989;11:81–97. [PMC free article] [PubMed] [Google Scholar]
- 23.Carey TS. Weis K. Homer C. Prepaid versus traditional Medicaid plans: Lack of effect on pregnancy outcomes and prenatal care. Health Serv Res. 1991;26:165–181. [PMC free article] [PubMed] [Google Scholar]
- 24.Goldfarb NI. Hillman AL. Eisenberg JM. Kelley MA. Cohen AV. Dellheim M. Impact of a mandatory Medicaid case management program on prenatal care and birth outcomes. A retrospective analysis. Med Care. 1991;29:64–71. doi: 10.1097/00005650-199101000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Schulman ED. Sheriff DJ. Momany ET. Primary care case management and birth outcomes in the Iowa Medicaid program. Am J Public Health. 1997;87:80–84. doi: 10.2105/ajph.87.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reis J. Medicaid maternal and child health care: Prepaid plans vs. private fee-for-service. Res Nurs Health. 1990;13:163–171. doi: 10.1002/nur.4770130305. [DOI] [PubMed] [Google Scholar]
- 27.Sommers AS. Kenney GM. Dubay L. Implementation of mandatory Medicaid managed care in Missouri: Impacts for pregnant women. Am J Manag Care. 2005;11:433–442. [PubMed] [Google Scholar]
- 28.Ray WA. Gigante J. Mitchel EF., Jr Hickson GB. Perinatal outcomes following implementation of TennCare. JAMA. 1998;279:314–316. doi: 10.1001/jama.279.4.314. [DOI] [PubMed] [Google Scholar]
- 29.Conover CJ. Rankin PJ. Sloan FA. Effects of Tennessee Medicaid managed care on obstetrical care and birth outcomes. J Health Polit Policy Law. 2001;26:1291–1324. doi: 10.1215/03616878-26-6-1291. [DOI] [PubMed] [Google Scholar]
- 30.Bronstein JM. Lomatsch CT. Fletcher D, et al. Issues and biases in matching Medicaid pregnancy episodes to vital records data: The Arkansas experience. Matern Child Health J. 2009;13:250–259. doi: 10.1007/s10995-008-0347-z. [DOI] [PubMed] [Google Scholar]
- 31.Bell JF. Zimmerman FJ. Selection bias in prenatal care use by Medicaid recipients. Matern Child Health J. 2003;7:239–252. doi: 10.1023/a:1027323618314. [DOI] [PubMed] [Google Scholar]