Abstract
Background.
Although rare in occurrence, a dorsal dislocation of the 1st metatarsophalangeal (MTP) joint has been successfully treated using surgical and/or non-operative treatment. No descriptions of conservative intervention following a dorsal dislocation of the MTP joint in an athlete participating in a high contact sport are present in the literature.
Objectives.
The purpose of this case report is to describe the intervention and clinical reasoning during the rehabilitative process of a collegiate football player diagnosed with a 1st MTP joint dorsal dislocation. The plan of care and return to play criteria used for this athlete are presented.
Case Description.
The case involved a 19-year-old male Division IA football player, who suffered a traumatic dorsal dislocation of the 1st MTP joint during practice. The dislocation was initially treated on-site by closed reduction. Non-operative management included immobilization, therapeutic exercises, non-steroidal anti-inflammatories, manual treatment, modalities, prophylactic athletic taping, gait training, and a sport specific progression program for full return to Division IA football.
Outcomes.
Discharge from physical therapy occurred after six weeks of treatment. At discharge, no significant deviations existed during running, burst, and agility related drills. At a six-month follow-up, the patient reported full return to all football activities including contact drills without restrictions.
Discussion.
This case describes an effective six-week rehabilitation intervention for a collegiate football player who sustained a traumatic great toe dorsal dislocation. Further study is suggested to evaluate the intervention strategies and timeframe for return to contact sports.
Keywords: dislocation, metatarsophalangeal joint, football
INTRODUCTION
A dorsal dislocation of the 1st metatarsophalangeal (MTP) joint is a rare occurrence in sport. Motor vehicle accidents are the most common cause of injury, followed by both falls from heights and athletic injuries.1 The mechanism of injury occurs from a high energy force acting from distal to proximal with forced hyperextension at the MTP joint.2 Consistent physical impairments with this injury include fixed plantar dislocation of the 1st metatarsal head,3 dorsal extension of the proximal phalanx,1 shortening of the 1st ray, edema, and loss of great toe function.4
A Type I MTP dislocation, under the classification scheme designed by Jahss,3 is a dislocation of the hallux with no disruption of the sesamoid mass. (Tables 1 and 2). The incidence and prevalence of this dislocation in sport is unknown. Jahss reported an extremely low incidence of 0.008%, in non-sport cases, which equals two traumatic dislocations in 25,000 patients. Successes of both operative and non-operative management are presently unclear in the literature as functional outcomes have not been consistently reported. Rather, authors have commonly reported range of motion and pain as outcome measures.1,5–7
Table 1.
Jahss Classifi cation System of 1st Metatarsophalangeal Joint Dislocations.3
| Type I | Dorsal dislocation with no disruption of the sesamoid mass, usually irreducible on closed reduction attempts |
| Type 1IA | Dorsal dislocation with a rupture of the intersesamoidal ligament resulting in a wide separation of the sesamoids on the metatarsal head allowing an easier reduction to occur |
| Type 1IB | Dorsal dislocation with a medial sesamoid transverse fracture, usually reducible |
| Type III | Dorsal dislocation with the sesamoids maintaining the same anatomical position with complete ruptures of the conjoint tendons and intact sesamoids and volar plate |
Table 2.
Type IIC addition to the Jahss Classification System, as proposed by Copeland and Kanat.16
| Type IIC | Dorsal dislocation with a medial sesamoid transverse fracture usually reducible |
Only two cases have been reported in sport of 1st MTP dorsal dislocations. Wolf et al5 reported a non-contact injury, resulting from a decelerated landing in basketball, treated surgically after repeated attempts at closed reduction failed. Two months after the injury, the athlete was asymptomatic and had full range of motion of the great toe. Whether the patient received a rehabilitation program or if the individual returned to sport was not noted. De Palma et al4 reported a dorsal dislocation, non-contact injury, in a football player who struck his great toe against the playing surface. The 1st MTP was immobilized for four weeks, and the patient was non-weight-bearing (NWB) with functional exercises beginning four weeks post-injury. Details of the treatment plan were not described, although the athlete returned to sport successfully. Other than these reports, the literature does not provide clear long term outcomes, or a treatment plan with return to play guidelines for an athlete who sustains a MTP dislocation in a contact sport. Information on a progressive treatment program and timeframe for immobilization may help prevent unnecessary lost training time for the athlete.
The Hallux Metatarsophalangeal-Interphalangeal Scale developed by The American Orthopaedic Foot and Ankle Society (AOFAS) is a clinical numerical rating system describing function, pain, and alignment of the great toe. One hundred total points are possible in a patient who is pain free and has normal metatarsophalangeal (MTP) and interphalangeal (IP) joint ROM, an absence of MTP or IP joint instability, good alignment, no recreational or daily activity limitations, and no limitations in footwear.8,9 Forty points are possible for pain (four choices with fixed number of points), 45 points are possible for function (six subcategories with four choices each containing fixed number of points), and 15 points are possible for alignment (3 choices with fixed points), and scoring involves both objective and subjective factors. The highest score in each of the three categories demonstrates no presence of pain, no functional limitations, and a well aligned hallux. The lowest score in each of the three categories demonstrates severe pain, severe functional limitations, and a poor symptomatic hallux alignment.
The purpose of this case report is to describe the intervention, including the return to play of a collegiate football player diagnosed with a 1st MTP joint dorsal dislocation as well as the clinical reasoning process utilized by both the physical therapist and athletic trainer to formulate the plan for intervention. The patient's plan of care included therapeutic exercises, joint mobilizations, prophylactic athletic taping, non-steroidal anti-inflammatories, manual treatment, modalities, neuromuscular training, gait, and sports-specific drills for full return to Division IA football. To the authors' knowledge, no descriptions of conservative interventions following a dorsal dislocation of the MTP joint for return to high-contact sport are present in the literature.
CASE DESCRIPTION
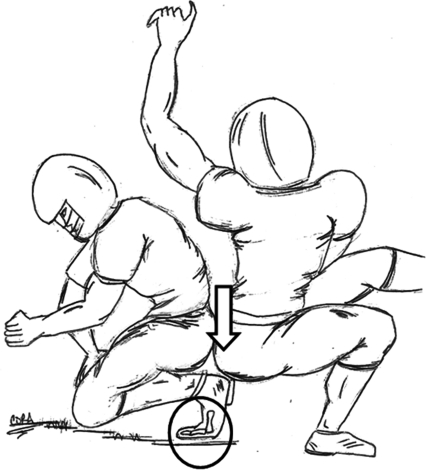
The patient was a 19-year-old male Division IA football player (tight end) who fell after a tackle during practice, and a 302-pound linebacker landed on his right foot. The patient suffered a traumatic dorsal dislocation of the 1st metatarsophalangeal (MTP) joint. He described that his forefoot was in contact with the ground, with the great toe in extension when another player sat on his heel during a tackle (Figure 1) (Video Clip Re-Enactment available on the NAJSPT website). He was a well-conditioned, 230 pound sophomore lineman, 6 feet, 3 inches in height. He had successfully completed preseason football and finished one in-season football game. His primary goal was to return to in-season football. Recreational activities included Olympic lifting, exercising on the elliptical, and golfing.
Figure 1.
Graphic Representation of the Mechanism of Injury
EXAMINATION
On-Site Initial Assessment
The initial examination was performed by the staff athletic trainer on-site at practice within seconds after the injury occurred. On observation, the 1st MTP joint was positioned in a varus deformity with the proximal phalanx being displaced both dorsally and laterally. These mechanics will be referenced throughout this report as a dorsal dislocation of the first metatarsophalangeal joint. The patient reported pain, numbness, and tingling at the 1st MTP joint radiating distally to the distal phalanx. He was unable to rise from a quadruped position. The athletic trainer on site performed a closed reduction by applying a longitudinal distraction to the joint. The patient was immediately referred to the team physician in the clinic who ordered radiographs to rule out a fracture and also ordered an MRI to check for the extent of the damage to the plantar plate.10
Following the closed reduction, radiographs taken the same day were unremarkable with no signs of a fracture. The sesamoid bones were intact with minor sesamoid widening. No sign of sesamoidal proximal migration was present. Magnetic resonance (MR) imaging was performed with multiple sagittal T1 and gradient images to check for soft tissue abnormalities. The radiologist noted a stretch in the plantar aspect of the capsule in the 1st MTP joint with a small amount of fluid present. A small focus of intra articular low signal intensity has an appearance suggesting the presence of air in the joint space. In the setting of recent trauma, intra articular air implies joint capsule disruption and joint trauma following dislocation. Both the flexor hallicus longus and flexor hallicus brevis muscles appeared normal. Based on the MR imaging, the patient's injury most closely matched a Type I MTP joint dislocation according to the Jahss Classification System.3 A Type I dislocation is a dorsal dislocation without disruption of the sesamoid mass. It should be noted that this patient suffered a stretch of the plantar aspect of the 1st MTP joint, which will later be discussed as this patient may not be classified as a true, uncomplicated, Type I dislocation. In conclusion, both clinical examination and the MR imaging suggested that the patient sustained a right 1st MTP dorsal dislocation. The team physician determined surgery was not indicated, and the subject was therefore referred for conservative management.
INTERVENTION
The patient was treated three times a week by the physical therapist and three times a week by the staff athletic trainer over a six-week period in 3 phases: Phase I: Early Protection, Phase II: Activity Progression, and Phase III: Return to Sport (Table 3). The goal of the treatment was to regain full strength, range of motion, joint mobility, proprioception, gait, and agility for return to collegiate football. No previous interventions or return-to-play criteria were cited in the literature, therefore, the authors of this case report have provided an intervention strategy with a rationale for each phase that was used throughout the rehabilitation of this patient (Table 4).
Table 3.
The 3 Phases of Intervention Used For a Collegiate Athlete after sustaining 1st MTP Dorsal Dislocation.
| PHASE I | PHASE II | PHASE III |
|---|---|---|
| Early Protection | Activity Progression | Return To Sport |
| Days 1 to 3 | Day 3 to 4 Weeks | Weeks 5 to 6 |
| NWB, short leg walking boot | PWBAT (day 4–8) | Orthotics/shank |
| AROM | Discontinue walking boot (2 wks) | Great Toe Taping |
| Great Toe Flexion and Extension | Orthotics/shank (2 wks) | Gait Training |
| Great Toe Taping | Jogging sagittal plane (limiting extension and abduction) | |
| Ankle Circles | Jogging multiplanar | |
| Ankle Pumps | Agility: | |
| BAPS Board (anterior-posterior, medial-lateral, clockwise and counterclockwise) | Long sit hamstring stretch, kneeling hip flexor stretch, piriformis stretch | - running routes |
| - passing/driving blocks: non-contact. | ||
| Longsit and Standing Gastroc Stretch, Great Toe flexion and extension stretching | ->With sandband-> with sled-> live contact | |
| Towel Toe Crunches | ||
| Marble Toe Pick Ups | ||
| Gait Training | 4 way SLR with cuff weights (ie hip flexion, adduction, extension abduction) | Return to practice non-contact prior to live contact |
| Ultrasound, 2 MHz 8 min, pulsed 50% | ||
| Electrical Stimulation premodulation 15 minutes | Ankle Theraband 4 way | Full Return to Practice |
| Ankle Isolator Exerciser | Electrical Stimulation premodulation 15 minutes as needed. | |
| Contrast Bath (alternating cold/warm whirpool) 15 minutes | SL balance with balance pad | |
| Clamshell | ||
| Step up (forward and sideways) | Cold Pack 20 minutes | |
| Cold Pack 20 minutes | Lunges (clock) | |
| Compression Wrap | Leg press with resistance cords | |
| Leg curl | ||
| Leg extension | ||
| Walking program | ||
| Sidelying leg press (shuttle) | ||
| Hip extension in standing with pulleys | ||
| Forward and lateral step ups | ||
| Heel raises | ||
| Core program (ie bridges on ball with sagittal flexion and oblique curl ups) | ||
| Ultrasound, 2 MHz 8 min, pulsed 50% | ||
| Electrical Stimulation premodulation 15 minutes | ||
| Cold Pack 20 minutes | ||
| Compression Wrap |
Table 4.
The Clinical Decision Making Table: A summary of the examination findings, clinical reasoning, and intervention utilized throughout the Case Report.
| TIMEFRAME | EXAMINATION FINDINGS | CLINICAL DECISION MAKING (Goals) | INTERVENTION (Refer to text for dosage details) |
|---|---|---|---|
| Days 1 -3 | Edema & ecchymosis at 1st MTP PROM R MTP flexion and extension limited | Restore AROM and PROM at MTP for normalized gait | AROM; great toe flexion and extension, ankle circles, ankle pumps, BAPS board (anterior-posterior, medial-lateral, and clockwise-counterclockwise), towel toe crunches, marble toe pick up- |
| Compression wrap | |||
| Modalities: Contrast bath, US. electrical stimulation, cold pack | |||
| Days 4–8 | Pain 3-4/10 during gait and 0/10 at rest | Restore gait, strength, and balance | Continued AROM exercises as above |
| Trendelenburg gait, L gluteus medius weakness | Initiate tendon training progressing to strengthening | Longsit hamstring stretch. kneeling hip flexor stretch, piriformis stretch, longsit gastroc stretch, great toe flexion and extension stretch | |
| Decreased strength R FHL, EHL, and posterior tibialis, all 4-/5 | Initiate proprioception | ||
| Ecchymosis and edema present | |||
| PWBAT, with crutches, short walking boot | Hip SLR with ankle weight (abduction, extension) | ||
| Leg extension, leg curl, leg press, clamshells | |||
| Modalities: continue same modalities | |||
| Day 9 | Decreased WB during stance phase of gait | Remodeling and strengthening of connective tissues | Gait training, |
| Progressed previous exercises by adjusting resistance loads according to the patients repetition endurance and symptom response | |||
| Decreased R tibial advancement also during stance phase | |||
| Modalities: continue same modalities | |||
| 2 Weeks | No pain reported during gait when using orthotics and tape | Restore gait mechanics | Single leg balancing on balance pad progressing with to without shoe support |
| Continue to protect MTP after walking boot is discontinued | |||
| Limited MTP extension during gait as expected (due to orthotics w/shank) | |||
| Ankle isolator (plate loaded resisted plantar flexion, dorsi flexion, inversion and eversion). sidelying leg press on shuttle (resistance cords), | |||
| Decreased strength R posterior tibialis and gluteus medius, 4-/5 | |||
| Walking program: gait instructions emphasizing equal WB, and introduce MTP ext in late stance | |||
| Core Program (bridges on gym ball with trunk sagittal flexion, oblique curl ups. and lower trunk curl ups) | |||
| Discontinued contrast bath and continued all remaining modalities | |||
| Orthotics/shank placed in shoe | |||
| Great toe athletic taping limiting abduction and extension | |||
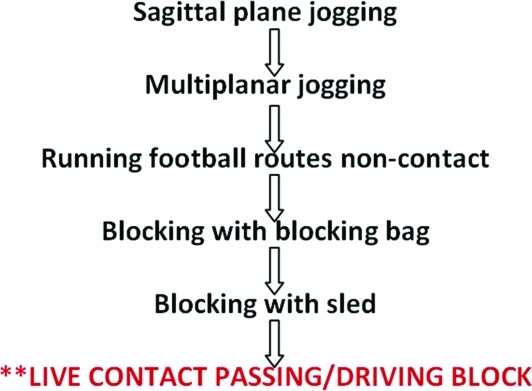
| 5 Weeks | Restored 1st MTP PROM to uninvolved side | Begin to introduce sports specific activities | Sagittal plane jogging progressing to multiplanar jogging with zig zag patterns |
| Strength of FHL, EHL, peroneals 4/5 | |||
| Agility: progression of running route non-contact->hitting blocking sandbag->hitting sled->live contact passing/driving block. | |||
| SL balance with perturbations unremarkable | |||
| Jogging gait tolerated without alterations | |||
| Modalities: Electrical Stimulation and cold pack. | |||
| Orthoties/Shank remains in shoe | |||
| Taping | |||
| 6 Weeks | Normal running gait in sagittal and mulliplanar directions | Progress contact drills for sports specific conditioning | Progress number of consecutive plays during practice (initial 5-6 consecutive plays during practice) |
| Mild stiffness reported at R 1st MTP during performance of 90 degree cutting maneuver at full speed. | Prepare for full return to sport | ||
| Modalities: Electrical Stimulation and cold pack | |||
| Orthotics/Shank remains in shoe | |||
| PROM R 1st MTP extension normal relative to uninvolved side | Taping |
MTP- Metatarsoprialangeal joint
PROM- Passive range of motion
R- Right
AROM- Active range of motion
L-Left
FHL- Flexor hallicus longus muscle
EHL- Extensor hallicus longus muscle
PWBAT- Partial weight-bearing as tolerated
WB- Weight-bearing
LE- Lower extremity
SL- Single leg
PHASE I: Early Protection (Days 1-3)
Examination
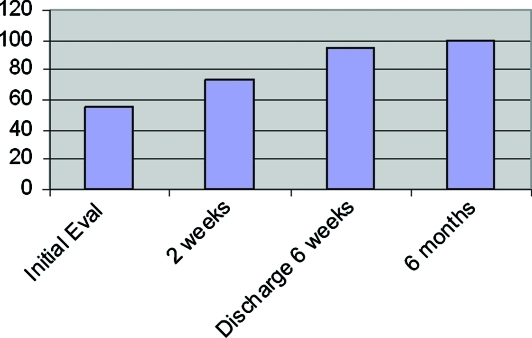
The patient was seen shortly after injury by the physical therapist from athletic rehabilitation services. During a brief exam, visual inspection revealed severe ecchymosis and diffuse soft tissue edema surrounding the 1st MTP joint. The exam was limited secondary to pain. On the American Orthopaedic Foot and Ankle Society (AOFAS) Hallux Metatarsophalangeal-Interphalangeal Scale8 (100 possible points), the patient scored 55 points at the time of initial injury. Low scores represent severe limitations and higher scores represent least limitations in the given categories. The patient received low scores in the function subcategories of activity limitations, footwear requirements, MTP joint motion, and metatarsophalangeal joint-interphalangeal joint stability.
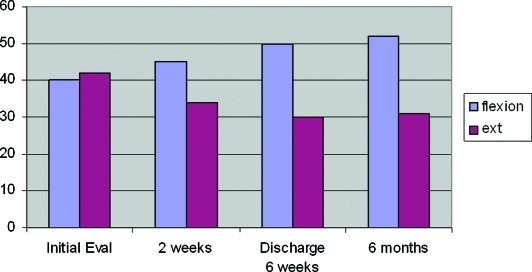
The patient reported a verbal rating pain scale of 3/10 only during gait. During examination on day three, observation revealed continued edema, ecchymosis, and limited 1st MTP joint flexion and extension. Passive range of motion (PROM) of the right 1st MTP joint extension was 0-42 degrees and flexion 0-40 degrees. Passive range of motion of the non-injured side was 0-60 degrees of extension and 0-50 flexion. Manual muscle testing revealed flexor digitorum longus, peroneals, and tibialis posterior strength of 4−/5 with pain upon testing, extensor hallicus longus, extensor digitorum longus, and gluteus medius muscle strength of 4−/5 and pain free; flexor hallucis longus strength of 4/5 and pain free; tibialis anterior, gastrocnemius, and soleus muscles, 5/5 and pain free.
Intervention
The clinical goals during Phase I were to protect the joint and allow for tissue regeneration and collagen remodeling. Other goals included control of pain, edema, and inflammation. Instructions for gait included a non weight-bearing (NWB) status utilizing crutches with a short leg walking boot. Although evidence does not support the use of modalities for pain and edema control, modalities were applied over the R foot surrounding 1st MTP joint area with the goals of controlling both pain and edema control, per institutional policy. This included pulsed ultrasound 2MHz (Dynatron 150 Combo, Isokinetics, Inc.™) at 50% for 8 minutes, contrast bath (alternating cold and warm bath for 15 minutes total), electrical stimulation using Premodulated Interferential current for 15 minutes, and cryotherapy (cold pack 20 minutes). Clinical judgment was used to determine modality use and parameters as there is lack of supportive research for modality application for any of the chosen modalities as applied after a first MTP joint dorsal dislocation. A compression wrap was administered and therapeutic exercises were restricted during the first two days to help reduce edema and pain. Edema reduction is important in order to help improve joint motion needed for gait in later rehabilitation. During heel off, the hallux reaches near end range extension during the gait cycle.11 The team physician restricted the athlete from participation in any football activities.
On day 3, the goals were advanced to address the restoration of the MTP joint active range of motion (AROM) needed for gait. Normal active range of motion MTP joint extension during the gait cycle is 0-60 degrees. Therefore, active range of motion exercises were prescribed to help the patient restore joint motion needed for gait. Land and pool exercises were performed consisting of AROM of great toe flexion and extension, ankle dorsiflexion/plantarflexion, inversion and eversion. Additional land exercises included baps board (anterior-posterior, medial-lateral, and ankle circles both clockwise and counterclockwise), towel crunches with toes and marble pick ups.
PHASE II: Activity Progression (Day 3 – week 4)
Examination (days 3-8)
During days four to eight, the examination findings revealed a Trendelenburg gait with left gluteus medius muscle weakness, decreased strength at the right flexor hallicus longus (FHL), extensor hallicus longus (EHL) and posterior tibialis muscles, rated 4−/5. His previous medical records indicated that the Trendelenburg gait was present from a previous left ankle surgery. Ecchymosis and edema were still present about the MTP. The patient reported complaints of right great toe pain rated 3-4/10 with gait and 0/10 at rest.
Intervention
The clinical goals were to restore gait, strength, and balance. Other factors included initiating proprioception and tendon training, progressing to strengthening. Tendon training refers to high repetition activities with low resistance loads. Tendon training prepares the patient to withstand stresses to the tendons that occur during gait. The MTP joint approaches an extension load during heel off placing stress on the hallux flexor tendons. Therefore, tendon training plays an important role in preparing the foot for repetitive motions that gait demands. The patient was advised to continue wearing a short leg walking boot, continue partial weight-bearing as tolerated with crutches from days four to eight, gradually tapering off crutch use during this time frame.
Phase II Activity Progression intervention lasted from day three to week four. Lower extremity exercises were prescribed for the ankle, calf, and foot intrinsic muscles. Isotonic ankle exercises were prescribed using a plate loaded platform ankle device called “The Ankle Isolator”, which allowed for resisted plantar flexion, dorsiflexion, inversion, and eversion. Also, hip strengthening and balance exercise progression were incorporated over this time period. This included isotonic leg extension, leg curl, clams shells (resisted hip abduction with external rotation), prone hip extension and sidelying leg raises. The patient performed 2 sets of 20 repetitions increasing the resistance loads and sets progressively based on his symptoms and endurance ability. The repetitions were progressed to 12-15 repetitions with the weights adjusted accordingly based on the patient's ability to safely withstand the new loads. Balance training included single leg balancing with a balance pad, starting with 30 seconds with shoe support and increasing the seconds based on patient tolerance. The shoe was removed for balance training when the patient discontinued the walking boot at 2 weeks. Gait training was continued.
Examination (days 9-10)
On day nine, the patient was FWB and completely discontinued the use of crutches. Decreased WB during the loading phase and decreased tibial advancement during the midstance phase was revealed during visual analysis of gait. Visual inspection 10 days post-injury revealed presence of ecchymosis although it had decreased by 30% since initial exam. The surface area of the ecchymosis remained the same. Soft tissue edema was present located at the plantar, dorsal, and medial surfaces along the 1st metatarsal joint and surrounding tissues. The patient reported tenderness to palpation along the 1st MTP joint line on all surfaces. Negative tenderness to palpation along the intertarsal joint and the remaining lesser MTP joints were noted. Valgus and varus tests of the 1st MTP joint at 0 and 30 degrees were negative. Static positional hallux valgus in the resting position was unremarkable. Further exam of the ankle ligaments was unremarkable for pain or ligamentous instability. Strength testing performed using methods described by Daniels and Worthingham12 revealed decreased strength in the right posterior tibialis, right FHL, and right EHL muscles, rated 4−/5. The plantardorsal translation test, also known as the vertical stress test,13 of the 1st MTP joint was negative with a good endpoint. This test is used to check for a tear of the plantar plate.
Intervention
The clinical goals were progressed to address remodeling and strengthening of the connective tissue. The functional demands of walking require good strength of contractile and non-contractile tissues about the great toe. Therefore, strengthening exercises were prescribed and progressed to help meet the muscular and soft tissue demands of gait as previously discussed. Gait training progression emphasized a gradual return of MTP joint extension during late stance. Gentle great toe flexion and extension passive range of motion was gradually introduced during this time frame. Weight bearing loads on the forefoot were progressed during the loading phase until weight bearing was symmetrical. Intervention included gait training and a strengthening progression program The exercises performed during days 9-10 were isotonic leg extension, leg curl, clam shells (hip abduction with external rotation), prone hip extension and sidelying leg raises. The patient performed 2 sets of 15-20 repetitions increasing the resistance loads and sets progressively based on his symptoms and endurance ability. The repetitions were progressed to 12-15 repetitions with the weights adjusted accordingly based on the patient's ability to safely withstand the new loads. Single leg balancing with shoe support was performed increasing the time duration based on patient ability and tolerance. The patient's gait was progressed to full weightbearing without crutches as he demonstrated a stable, unimpaired gait.
Examination (2 weeks)
At two weeks, the patient was prescribed custom fitted orthotics with a semi-rigid carbon shank and polyurethane cover for protection of the MTP joint. Visual analysis of gait revealed limited right MTP joint extension as expected since he was wearing the orthotics during the exam for protection. Decreased stance time during stance phase was present on the injured lower extremity. Manual muscle testing revealed right posterior tibialis and gluteus medius weakness strength of 4−/5. The AOFAS score at two weeks post-injury was 74 points. The subcategories of function in which the patient did not receive total points were activity limitations, footwear requirements, and MTP joint motion. Passive range of motion testing of the right 1st MTP joint revealed 0-34 degrees extension and 0-45 degrees flexion. Manual muscle testing revealed FHL, EHL, extensor digitorum longus (EDL), tibialis posterior, and gluteus medius muscles, all 4−/5 and pain free; flexor digitorum longus (FDL) muscle, 4/5; peroneal muscles, 4+/5; Tibialis anterior, gastrocnemius, and soleus muscles, 5/5. Although manual muscle testing strength grades did not improve at 2 weeks, his ability to achieve full weightbearing with a stable gait and no loss of balance demonstrated increased function.
Intervention
The clinical goals were to restore gait mechanics and continue to protect the MTP joint. Presence of pain and joint edema inhibits normal muscle contraction which could interfere with gait. Protecting the MTP joint by use of the orthotic assisted in preventing further pain and joint edema during tissue healing. During a trial of both great toe taping and the orthotics with an incorporated shank, the patient denied any pain during gait. The purpose of the great toe taping was to limit the patient's metatarsophalageal joint extension and intermetatarsal joint abduction for joint capsule protection during collagen remodeling. One-inch width athletic tape was used to apply anchors at the distal great toe and midfoot. Next, longitudinal strips and spica strips were applied to both anchors restricting excessive great toe hyperextension and intermetatarsal joint abduction. Next 1/2 circumferential closing strips were applied. Lastly, the midfoot, forefoot and great toe were fully closed with lightplast.
The patient was advised by the team physician to discontinue the walking boot and begin to utilize the orthotics in a supportive shoe in order to continue to protect the joint. The great toe taping was also added as a supplement to the orthotic as the patient reported it made him feel better. The rehabilitation prescription included strengthening using leg press with resistance cords (ie Shuttle™), single leg stance hip extension with pulleys, forward and lateral step ups, step downs, and lunges in clock positions. The patient performed 3 sets of 20 repetitions, progressing to 3 sets of 12-15 repetitions with adjusted resistance based on his symptoms and his endurance to withstand increased loads and decreased repetitions. He also performed leg press and heel raises on his uninjured lower extremity starting at 3 sets of 12-15 repetitions. Airex™ single leg balance training was performed in order to improve both balance and proprioception, progressing from 30 to 60 seconds for 3- 6 repetitions (wearing shoe support). The patient's gait continued to be monitored with instruction emphasizing equal weight bearing and gradually progressing MTP joint extension motion during late stance as mentioned previously. The patient also performed core exercises in a bridge position on a Swiss ball (sagittal plane flexion, oblique sit ups). He also performed lower trunk curl ups without the ball. At 3 weeks post injury the patient began walking on the treadmill for 10 minutes practicing his gait pattern. The duration was gradually increased over the course of treatment.
PHASE III: Return to Sport (Weeks 5-6)
Examination (week 5)
At 5 weeks, the patient continued to be pain-free with a walking gait. A trial of jogging gait was unremarkable for any deviation of gait biomechanics, balance, or presence of pain. The examination revealed restored right 1st MTP PROM relative to the uninvolved side. The patient had adequate strength assessed functionally by demonstration of a normal gait cycle although great toe flexor and extensor muscles and peroneals still demonstrated strength of 4/5 at 6 weeks. (See Table 4). Single-leg (SL) balance testing with perturbations was unremarkable demonstrated by no loss of balance or pain being reported during 60-90 seconds holds. The patient's uninvolved side tested at 90 seconds. Intermittent mild edema was present at the great toe.
Intervention
The clinical goals included introducing sports specific activities that were position-specific for a tight end. The activity demanded of a tight-end offensive lineman includes multi-planar running, cutting, tackling, striking, and blocking. Strength, explosive power, speed, agility, are all needed throughout a running gait cycle for a tight end. The activities of a lineman/tight end are primarily anaerobic. Therefore, the intervention prescribed included a striking/blocking progression where the patient explodes from a stance phase hitting a sand bag, then a sled, then live contact play during practice which progressed throughout weeks five to six. The running progression program incorporated sagittal plane, then multi-planar running with zigzag patterns. Noncontact football routes both with and without live practice were included (Figure 2). For all phase III activities, the intensity and duration were increased over time and as the patient tolerated. The use of electrical stimulation tapered off as great toe swelling diminished and a cold pack continued to be administered as needed during the presence of edema. Noncontact practice was resumed at week five.
Figure 2.
Sport Specific Functional Progression for Tight End.
Examination (week 6)
At six weeks, examination revealed a normal running gait both in sagittal and multi-planar directions. Passive range of motion of the right 1st MTP joint was normal relative to the uninvolved side in both extension and flexion. Mild stiffness was reported during gait at the right 1st MTP joint while cutting at a 90 degree angle at full speed. The AOFAS score at six weeks was 95 points. The patient scored 5 points out of a total possible 10 points in the subcategory of footwear requirements as he was still wearing his shoe orthotic. Passive range of motion testing of the right 1st MTP joint revealed 0-30 degrees extension and 0-50 degrees flexion,. Manual muscle testing of the flexor hallicus longus, flexor digitorum longus, extensor hallicus longus, and extensor digitorum longus muscles, demonstrated continued strength of 4/5; peroneal and gluteus medius muscles, 4+/5; tibialis posterior muscle, 5−/5; tibialis anterior, gastrocnemius, and soleus muscles, 5/5.
Intervention
The clinical goals were progressed to include contact drills for sports-specific conditioning and increase his endurance. The same concepts mentioned in week 5 of the patient needing explosive power, speed, and agility to achieve a running gait cycle continued to be applied at week 6. The intervention progressed to increase the number of consecutive plays during practice. He initially was instructed to limit his consecutive plays to not exceed five to seven plays. Over time, participation in plays slowly increased. He continued his rehabilitation program independently and was taped throughout the remainder of the season. Electrical stimulation with ice (ie 15 minutes, premodulation) continued to be used as needed for edema control.
OUTCOMES
On the American Orthopaedic Foot and Ankle Society (AOFAS) Hallux Metatarsophalangeal-Interphalangeal Scale8 (100 possible points), the patient scored 55 points at the time of initial injury, 74 points at two weeks, and 95 points at six weeks (time of discharge) (Figure 3). At six months, he scored 100 points demonstrating no disability associated with his previous left foot pain (Table 5). A summary of the strength outcomes as measured by manual muscle testing per procedures of Daniels and Worthingham12 is provided in (Table 6), and the passive range of motion outcomes as measured per procedures of Norkin and White14 are provided in Figure 4.
Figure 3.
Scores on the American Orthopaedic Foot and Ankle Society (AOFAS) Hallux Metatarsophalangeal Interphalangeal Scale, in points (100 possible)
Table 5.
The American Orthopaedic Foot and Ankle Society (AOFAS) Hallux Metatarsophalangeal-Interphalangeal Scale8 (100 possible points).
| Parameter | Initial Eval | 2 weeks | Discharge 6 weeks | 6 months |
|---|---|---|---|---|
| AOFAS | 55 | 74 | 95 | 100 |
| Pain Scale | 3/10w/gait 0/10 rest | 0/10 rest and gait | 0/10 rest and gait | 0/10 rest and gait |
Table 6.
Strength testing12 of the right lower extremity measured at four time intervals
| STRENGTH: R LE | Initial Eval | 2 weeks | Discharge 6 weeks | 6 months |
|---|---|---|---|---|
| Flexor Hallicus Longus (FHL) | 4/5. | 4-/5 | 4/5. | 5/5. |
| Flexor Digitorum Longus (FDL) | 4-/5 w/pain | 4/5. | 4/5. | 5-/5 |
| Extensor Hallicus Longus (EHL) | 4-/5. | 4-/5. | 4/5. | 5-/5 |
| Extensor Digitorum Longus (EDL) | 4-/5 | 4-/5. | 4/5. | 5-/5 |
| Posterior Tibialis | 4-/5 w/pain | 4-/5 | 5-/5 | 5-/5 |
| Peroneals | 4-/5 w/pain | 4+/5 | 4+/5 | 5-/5 |
| Gluteus Medius | 4-/5 | 4-/5 | 4+/5 | 4+/5. |
R- Right
LE = Lower extremity
w/pain = Testing elicited pain
Figure 4.
MTP Joint Range of Motion, in degrees.
DISCUSSION
To the knowledge of the authors, no other case report exists detailing the results of conservative management following a 1st MTP dorsal dislocation for a patient returning to in-season, Division IA football. The clinical goals were centered around the desire to minimize the time lost in-season and to maximize the effectiveness of the rehabilitation. Clinical interventions included modalities, strengthening, joint range of motion exercises, proprioceptive exercises, gait, and agility drills during a progressive rehabilitation program. Following a successful rehabilitation program, the patient returned to football in six weeks time. Only two sport-related cases of a 1st MTP dislocation have been reported in the literature, one of which reported successful return to sport.4,5 Neither case clearly discussed long-term outcomes nor a treatment plan with return to play guidelines for sport. De Palma et al4 reported a 1st MTP dorsal dislocation with immobilization for four weeks non-weightbearing and functional exercise, which began after four weeks time. This patient was immobilized for two weeks in the walking boot and was partial weight-bearing with crutches at day four. The walking boot was removed for his rehabilitation sessions. He began range of motion exercises on day three. These findings indicate it is possible for an athlete to follow a conservative rehabilitation approach and successfully return to football.
This patient was classified as a Jahss Type I dislocation. As previously mentioned, the Jahss classification1 refers to Type I being a dislocated hallux with no sesamoid mass disruption. Type II is a rupture in the intersesamoidal ligament with widened sesamoids. The authors believe this patient likely suffered a Type I+ dorsal dislocation as the hallux dislocated while the intersesamoidal ligament did not rupture but suffered a partial stretch. This description, to our knowledge, has not yet been noted in the literature. Also noted in the literature is that Type I dislocations are often irreducible and require surgery.1 However, this case demonstrates that closed reduction was possible, and was followed by an excellent outcome.
At four weeks and 5 days post injury, the patient was able to return to light jogging non-contact football practice. At six months follow-up, this patient was able to demonstrate all football activities including multiplanar running, cutting, tackling, and striking without difficulty. Seven months post injury, he continued full participation in spring season football and was without disability. The patient's only complaint was mild soreness at the right 1st MTP joint during 90-degree cutting maneuvers, which he reported did not interfere with his full speed running ability. Gait examined during cutting appeared unremarkable both with and without his custom orthotics.
The authors discussed whether or not the patient may have benefitted from removing the walking boot several days earlier should another athlete present with this type of injury. This patient progressed and performed so well using implemented treatment program in the described time frames that a shorter period of immobilization might be considered. It must be acknowledged however, that the long term outcomes of such an injury managed with shorter immobilization timeframe is unknown.
A MTP joint ROM impairment can affect the gait cycle. Normal ROM of the 1st MTP joint is 30 degrees flexion and 90 degrees extension. 60 degrees extension is required for the gait cycle. When heel rise and toe off occur in the stance phase, the hallux and lesser toes reach end-range maximum extension.11 If the MTP joint is prevented from fully extending, the heel-off to toe-off phase is impaired which can alter running, jogging, and cutting mechanics. An athlete with impaired great toe ROM can be functionally disabled, thereby limiting sports performance.
Passive range of motion extension at the 1st MTP joint did not progressively increase over the course of rehabilitation as did flexion range of motion. The subject's passive range of motion at initial evaluation was 0-42 degrees whereas at six months, it was 0-31degrees. Although this reported range of motion does not reach the value for “normal,” the patient's gait function was good and he reported minimal symptoms, so we did not push his range. Perhaps he was performing within a range that he only functionally needed, which may have allowed him to return to running without difficulty. The cause of the decrease in range of motion could have been from scar tissue developing during the foot protection progression from the walking boot, to shoes with custom orthotics, with additional taping as needed. The amount of foot protection provided was based on both the stage of his injury, the quality of the patient's gait, and any presence of symptoms.
Notice should be taken that this proposed Type I+ dislocation was treated immediately on the field with closed reduction. Rehabilitation with early protection began on day one of injury without a time delay. The time between injury occurrence and treatment has been noted to affect the ability for the dislocation to maintain closed reduction.15 Similar Type I dislocations amongst athletes treated with early intervention, proper immobilization and rehabilitation can possibly result in a successful return to sport.
SUMMARY
First MTP joint dorsal dislocations are rare in the general population and are even a rarer occurrence in sport. No evidence exists in the literature regarding rehabilitation and return to play guidelines for a football player. In this case study, the patient who was treated with closed reduction with no sign of complications returned to in-season Division IA college football six weeks post-injury following conservative management with minimal disability (AOFAS) and a normalized running gait. Further study is necessary to evaluate a wide variety of possible intervention strategies and timeframe for return to contact sports with greater numbers of patients who sustain a MTP dislocation.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Kerry Mullenix, MPT, ATC, LAT, Nancy Major, MD, and Harvey Johnson.
REFERENCES
- 1.Killian FJ, Carpenter BB, Mostone E. Dorsal dislocation of the first metatarsophalangeal joint. J Foot Ankle Surg. Mar-Apr 1997;36(2):131–135 [DOI] [PubMed] [Google Scholar]
- 2.Smith T. Dislocations. In: McGlamry E, Banks AS, Downey MS, ed. The Comprehensive Textbook of Foot Surgery. Vol 2 2nd ed. Baltimore: Williams & Wilkins; 1992:1481–1484 [Google Scholar]
- 3.Jahss MH. Traumatic dislocations of the first metatarsophalangeal joint. Foot Ankle. Jul 1980;1(1):15–21 [DOI] [PubMed] [Google Scholar]
- 4.De Palma L, Santucci A, Marinelli M. Traumatic dislocation of metatarsophalangeal joints: report of three different cases. J Foot and Ankle Surgery. 2001;7:229–234 [Google Scholar]
- 5.Wolfe J, Goodhart C. Irreducible dislocation of the great toe following a sports injury. A case report. Am J Sports Med. Sep-Oct 1989;17(5):695–696 [DOI] [PubMed] [Google Scholar]
- 6.Isefuku S, Hatori M, Kurata Y. Traumatic dislocation of the first metatarsophalangeal joint with tibial sesamoid fracture: a case report. Foot Ankle Int. Sep 2004;25(9):674–679 [DOI] [PubMed] [Google Scholar]
- 7.Good JJ, Weinfeld GD, Yu GV. Fracture-dislocation of the first metatarsophalangeal joint: open reduction through a medial incisional approach. J Foot Ankle Surg. Sep-Oct 2001;40(5):311–317 [DOI] [PubMed] [Google Scholar]
- 8.Baumhauer JF, Nawoczenski DA, DiGiovanni BF, Wilding GE. Reliability and validity of the American Orthopaedic Foot and Ankle Society Clinical Rating Scale: a pilot study for the hallux and lesser toes. Foot Ankle Int. Dec 2006;27(12):1014–1019 [DOI] [PubMed] [Google Scholar]
- 9.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. Jul 1994;15(7):349–353 [DOI] [PubMed] [Google Scholar]
- 10.Ashman CJ, Klecker RJ, Yu JS. Forefoot pain involving the metatarsal region: differential diagnosis with MR imaging. Radiographics. Nov-Dec 2001;21(6):1425–1440 [DOI] [PubMed] [Google Scholar]
- 11.Hockenbury RT. Forefoot problems in athletes. Med Sci Sports Exerc. Jul 1999;31(7 Suppl):S448–458 [DOI] [PubMed] [Google Scholar]
- 12.Hislop H, Montgomery J. Daniels and Worthingham's Muscle Testing: Techniques of Manual Examination. 6th ed: W.B. Saunders Company; 1956 [Google Scholar]
- 13.Dilnot M, Michaud TC. Plantar Plate Rupture. Australasian Journal of Podiatric Medicine. 2003;37,(2):43–46 [Google Scholar]
- 14.Norkin C, White DJ. Measurement of Joint Motion: A Guide to Goniometry. 2nd Edition ed. Philadelphia: F.A. Davis Company; 1995 [Google Scholar]
- 15.Jahss MH. Disorders of the hallux and first ray. In: Wickland E, ed. Disorders of the Foot and Ankle: Medical and Surgical Management. 2nd ed. Philadelphia: WB Saunders Company; 1991:1125–1129 [Google Scholar]
- 16.Copeland CL, Kanat IO. A new classification for traumatic dislocations of the first metatarsophalangeal joint: type IIC. J Foot Surg. May-Jun 1991;30(3):234–237 [PubMed] [Google Scholar]