Abstract
Study Design:
Resident's case report
Background:
There have been only a few case reports in the literature mentioning sciatic nerve injury following a hamstring tear. In previous cases surgical intervention was performed to debride scar tissue around the sciatic nerve with the goal of full return to function for the patient.
Objectives:
The purpose of this case report is to describe the conservative interventions that allowed for recovery from a hamstring tear with sciatic nerve involvement.
Case Description:
The subject was a 53 year old female who developed foot drop and weakness in the common fibular nerve distribution following a grade 3 hamstring injury sustained during Nordic skiing. Nerve function and strength gradually returned over the course of several months of conservative rehabilitation which included on neural gliding and strengthening exercises.
Outcomes:
At 18 months post injury, the subject had returned to 95% of full sport function and 98% of full function with activities of daily living, as rated by the Hip Outcome Scale, and had full strength with manual muscle testing. Isokinetic testing revealed strength deficits of 11–23% in knee flexion peak torque at 60 degrees/second and 180 degrees/second respectively.
Discussion:
Sciatic nerve injury is a rare, but important potential consequence of severe hamstring strains. Clinicians should be cognizant of the potential injury to the nerve tissue following hamstring strains, so they may be dealt with in a prompt and appropriate manner. The use of neural gliding may be worth considering for a prophylactic effect following hamstring strains.
Keywords: foot drop, nerve glide, sciatic nerve, hamstring strain
INTRODUCTION
Hamstring tears are common sports injuries that often require physical therapy intervention. In a literature review of hamstring avulsion injuries that required surgical intervention, it was found that skiing was one of the most common mechanisms of injury.1–2 Water skiing accounts for almost 30% of hamstring tears in Australia1 and Nordic skiing has been reported to account for 40% of tears in Finland.2
A rare sequela associated with a hamstring tear is an injury to the sciatic nerve due to the proximity of the anatomical structures. There have been a few reports of sciatic nerve involvement with hamstring injuries in the literature.3–8 Each of these cases involved at least a partial avulsion/tear of the proximal hamstrings. In all of these cases, surgical intervention was the only reported intervention that alleviated the subjects' symptoms related to the nerve injury. The surgery was performed to attempt to release scar tissue from around the sciatic nerve. In one case where symptoms did not improve, surgery was performed to reattach the hamstring but no debridement of scar tissue was performed.7 At the time of the writing of this case report, there were no documented cases detailing the successful conservative rehabilitation of a complete hamstring tear with sciatic nerve involvement. The purpose of this report is to present the details of a case where a patient recovered from a hamstring tear with sciatic nerve involvement with conservative care as the only intervention. The patient described in this case report gave written informed consent for the description of her case and use of diagnostic images (magnetic resonance imaging {MRI} and photograph of leg) to be published.
CASE DESCRIPTION
Subjective – Initial Evaluation
The patient was a 53 year old female who was referred to physical therapy with a diagnosis of a Grade III (complete) tear of the medial hamstring following a cross country ski accident involving a fall. During the fall, she reported that the right lower extremity slid forward while her trunk moved forward creating hyper flexion at the right hip. Ecchymosis was noted by the patient extending from her posterior thigh down to her ankle two days following the injury (Figure 1). Medical care was sought five days following the injury at which time she was diagnosed with a grade 3 hamstring tear and referred to physical therapy.
Figure 1.
Ecchymosis in posterior leg 2 days following injury.
At the initial physical therapy visit, the patient reported that she had been icing and elevating her leg since her injury. She used an ACE wrap for compression around her thigh to allow her to walk and stand for longer periods of time. Walking for extended periods of time was difficult. While ascending stairs, she had to use a step to step gait pattern, relying on the left lower extremity. She also reported that knee extension with hip flexion (as in sitting), caused distal hamstring pain. As a result, she kept her knee flexed a majority of the time. The patient reported pain rated at 4/10 at rest, experienced mostly in her calf. With movements such as getting in and out of a car, pain was rated at 8/10. She denied any previous leg or back injuries. Her occupation as a teacher required her to stand for long periods of time and she found this to be difficult to perform due to pain. On the Hip Outcome Scale (HOS) she rated her function at 60% for activities of daily living (ADLs) and 0% for sports activities. The HOS asks patients to rate their ability to perform different daily activities. A copy of the HOS is included in Appendix 1. The patient had the most difficulty with squatting, putting on sock/shoes, rolling over in bed, pivoting on her involved leg, heavy work (pushing/pulling/carrying), and recreational activities. The HOS has been suggested in an unpublished report, to have excellent test-re-test reliability for the HOS ADL subscale (ICC = 0.96) and moderate to strong correlations (r = 0.69-0.74) with the physical function subscale and physical summary score of the SF-36.9 Her main goals were to return to ascending and descending stairs, walking, running, biking, and cross country skiing.
Objective - Initial Examination
Upon observation during the initial examination, ecchymosis was present from the patient's posterior thigh, medial greater than lateral, down to the medial calf (Figure 1). She ambulated with an antalgic gait due to pain with bearing weight on the right leg and decreased extension of her right knee during stance phase. Due to decreased excursion of the right leg, heel strike was decreased. With palpation, there was a firm mass noted in the mid third of the semitendinosus and semimembranosus muscle bellies. She displayed tenderness from the posterior thigh extending down the entire right lower leg with Grade I pitting edema in the lower leg. Active range of motion (AROM) of the right knee via a heel slide while the patient was supine was measured at 0°−4°−95° compared to 0°−133° degrees on the left knee. Circumferential measurements revealed that the right leg was 2.5 cm greater at 15 cm distal to the knee joint line, 3 cm greater at the knee joint line, 2 cm greater at 10 cm proximal to the knee joint line, and 2 cm greater at 20 cm proximal to the knee joint line. Due to patient discomfort, strength testing was not performed during the initial examination.
It was determined that the patient had signs and symptoms consistent with the medical diagnosis of a grade III hamstring tear. Her primary impairments included limited range of motion (ROM), lower extremity edema, and gait deviations. Strength was also likely impaired, but due to pain levels formal muscle testing was not performed.
Intervention provided at the initial visit consisted of retrograde massage in the right leg and instruction in the performance of a home exercise program. The home program consisted of ankle pumps with the lower extremity elevated to decrease lower extremity swelling, quad sets to facilitate muscle activation in the right lower extremity, very gentle passive hamstring stretching in the longsitting position via use of a towel, and education regarding the importance of continued use of ice and compression.
Visits 2-5
Over the next 4 visits lower extremity stretching and strengthening was progressed (refer to Table 1). Closed chain exercises consisting of single limb balance work to improve proprioception and trunk stability were added based upon the work by Sherry and Best that showed improved outcomes when agility and trunk stabilization exercises were incorporated into a rehabilitation program for hamstring strains.10 Retrograde massage was continued to help decrease swelling and light cross friction massage was added to assist in tissue remodeling in the medial hamstring muscles.
Table 1.
General progression of interventions through course of treatment.
| Weeks | Interventions and changes in interventions |
|---|---|
| 1–2 | STM to calf/distal HS, HS stretching, quad sets, ice, Nu-step/bike, calf and HS isotonics, calf stretching |
| 3–4 | Added CKC hip strengthening, PF/DF isokinetics, OKC HS isotonics, CKC isokinetic step machine, leg press, squats, and ball toss in single leg stance |
| 5 | Added eccentric prone HS AROM and resisted sidesteps for hip strengthening |
| 6 | Eliminated STM, added resisted DF/eversion and AAROM for HS curls |
| 11–12 | Instituted sciatic nerve glides performed in sitting, electrical stimulation for DF/eversion, and isotonic prone HS, and continued with CKC stability exercises, squats on tilt board, bike and leg press |
| 13–14 | Added STM to posterior knee/proximal gastrocnemius, isokinetics for ankle inversion/eversion, OKC HS curls, resumed isokinetics for PF/DF, and eliminated electrical-stimulation |
| 15 | Eliminated STM, advanced CKC stability via circle board balance exercises |
| 16–33 | Continued with ankle isotonics/isokinetics, HS isotonics, nerve glides and CKC stability. Increased difficulty of CKC exercises by advancing speed and decreasing stability of surfaces. Added dead lifts, elliptical trainer, and lateral bounding |
Key: STM = soft tissue mobilization, HS = hamstring, CKC = closed kinetic chain, OKC = open kinetic chain, DF = dorsiflexion, AAROM = active-assisted range of motion, PF = plantarflexion
The patient displayed steady progress over these visits. Gait returned to normal with normal excursion and heel strike, AROM was restored to full as compared to the other leg and the patient was able to return to previous work activities without restrictions.
Visits 6-10
At visit number 6, the patient reported slipping at home three days prior in a mechanism similar to her original injury. This slip occurred 28 days after her initial cross country skiing injury. Following this slip, she reported some soreness in the original injury location, however, she returned to pain-free walking by the time she presented to the clinic for the sixth visit.
By the seventh visit, she reported her lateral hamstring tendons “felt different” and she had increased soreness in her posterior knee and calf. Upon inspection, there was decreased tone in the gastrocnemius and biceps femoris compared to the uninjured side. By the eighth visit, her gait was altered in that she advanced her right leg more quickly than her left and she noted increased pain in her medial gastrocnemius muscle. During ambulation, she felt decreased control of her leg. By the ninth visit, 17 days after her slip on the floor and 40 days after the initial skiing injury, she started to exhibit a foot drop while ambulating.
At PT visit 10 the patient reported numbness in the calf where it had previously been sore and progressive symptoms of weakness in her lower extremity. Re-examination prior to a medical visit revealed muscular weakness in dorsiflexion, eversion, and toe extension of all digits when compared to the uninjured side (Table 2). Hamstring strength had also decreased to the point of not being able to perform a prone hamstring curl without assistance, signifying a muscle test grade of 2/5. During an active hamstring curl, minimal contribution from the biceps femoris was noted. Palpation revealed tenderness in the popliteal fossa, extending proximally in the leg just medial to the biceps femoris. Decreased tone was still noted in the biceps femoris. Sensation to light touch was intact and symmetrical and deep tendon reflexes were rated at 2+.
Table 2.
Objective measurements taken throughout course of treatment.
| Week | HOS (ADL/ Sport) | DF MMT | PF MMT | Eversion MMT | Inversion MMT | DF AROM | DF PROM | HS MMT | EHL MMT | EDL MMT |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 (week 1) | 60/0 | |||||||||
| 10 (week 6) | 2+/5 | 5/5 | 4/5 | 5/5 | −10 | 5 | 2/5 | 4/5 | 4/5 | |
| 14 (week 12) | 4 | 10 | ||||||||
| 17 (week 14) | 4/5 | 3 | ||||||||
| 19 (week 15) | 2+/5 | 5/5 | 5/5 | 5/5 | 0 | 5 | 4/5 | |||
| 22 (week 16 | 3 | |||||||||
| 23 (week 17) | 1 | |||||||||
| 24 (week 18) | 6 | |||||||||
| 25 (week 19) | 2+/5 | 5/5 | 5/5 | 5/5 | 0 | 4/5 | ||||
| 26 (week 20) | 6 | |||||||||
| 27 (week 21) | 2+/5 | 4/5 | 5/5 | 5 | 10 | 4/5 | ||||
| Recheck, 18 months post injury | 98/95 | 5/5 | 5/5 | 5/5 | 5/5 | 10 | 10 | 5/5 | 4/5 (B) |
Key: HOS = Hip Outcome Scale, ADL = Activities of Daily Living, DF = dorsiflexion, MMT = Manual Muscle Test, PF = plantarflexion, HS = hamstring, EHL = Extensor Hallucis Longus, EDL = Extensor Digitorum Longus
Based on these findings, it was determined the patient had sustained an injury to the sciatic nerve, particularly affecting the common fibular nerve division. She was provided active dorsiflexion and eversion exercises in attempts to maintain ankle range of motion and was also advised to continue with her hamstring strengthening exercises as able. Due to her neurologic injury, she was instructed to use her opposite leg to assist in performing prone knee flexion for hamstring strengthening. Due to the progressive change in her status, she was referred back to her physician for further diagnostic testing.
Diagnostic tests
Following evaluation by her physician, further diagnostic tests were ordered. An electromyographic (EMG) analysis revealed severe denervation of the biceps femoris and tibialis anterior, and to a lesser extent denervation to the semitendinosis. It was concluded that an injury to the branches off of the tibial and common fibular portion of the sciatic nerve had occurred. Neurapraxia of the common fibular nerve or posterior tibial nerve was not reported.
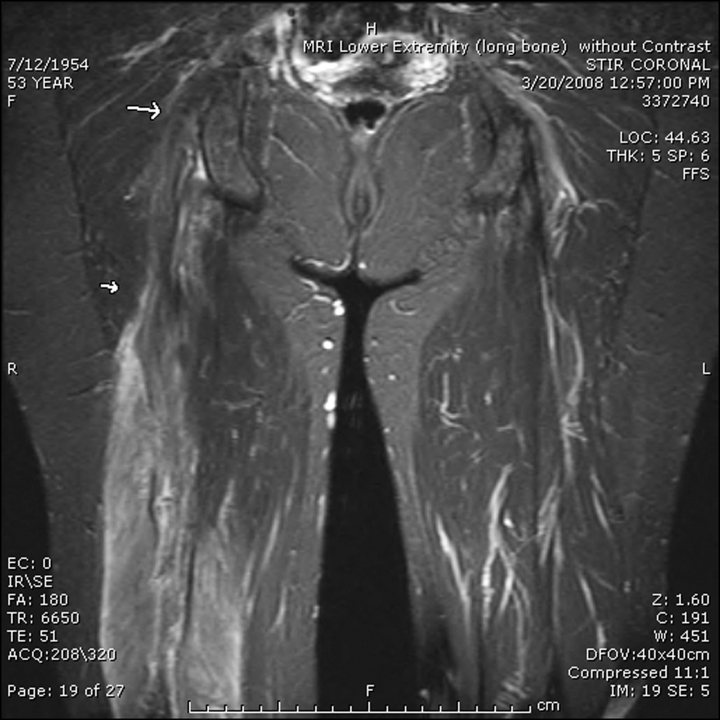
Based on these results, an MRI was recommended. The MRI revealed abnormal signal intensity throughout all 3 muscles of the hamstring, with a focus of extremely low signal intensity extending a length of 12 cm from the common insertion on the ischium (Figure 2). These findings suggested a subacute to chronic tear with fibrosis and musclular atrophy. The MRI findings did not reveal any damage to the sciatic nerve. Based on these results, it was decided to focus PT interventions upon improving sciatic nerve mobility in order to prevent the fibrosis within the muscle from affecting the nerve.
Figure 2.
MRI image of hamstring. There is diffuse abnormal signal intensity throughout the semimembranosus, semitendinosus, and biceps femoris tendons with a focus of extremely low signal intensity proximally. This suggests a subacute to chronic tear with fibrosis and diffuse muscle atrophy.
Re-initiation of PT
Visit 12
Following her examination, the patient's primary physician recommended continued conservative management to address the patient's impairments. Dependant upon how the patient responded to conservative care, the need for neuolysis surgery was to be determined. She was re-examined by the physical therapist after a 35 day break from conservative treatment. This re-examination was performed 89 days after the original skiing injury. During the time off from therapy, she continued to perform active range of motion exercises for ankle dorsiflexion and eversion, as well as prone knee flexion, (which she acquired the ability to perform independently during this time). She maintained a very light stretching program for the hamstrings, performed in the long sitting position, using 30 sec holds.
Upon examination, muscle recruitment of the biceps femoris had increased from the last visit prior to her diagnostic testing, but was still greatly reduced when compared to the unaffected side. She was able to perform a prone hamstring curl without assistance and strength was rated at 3/5. Additional objective measures are noted in Table 2. The HOS was not issued again at this visit.
Following the reexamination, the plan of care was modified to include sciatic nerve glides (both in the clinic and at home) in a seated position with the knee extended and moving the ankle into dorsiflexion and plantarflexion. Butler proposes that healing tissues need movement to assist healing and neural glides were added with this goal in mind.11 Neuromuscular electrical stimulation (NMES) was included to facilitate musclular recruitment of the peroneals and tibilalis anterior during active dorsiflexion and eversion performed by the patient. This was added because the EMG revealed severe, but not complete denervation and the treating therapist thought that NMES might help with muscular recruitment. She was encouraged to continue with her active knee and ankle motion at home.
Visits 13-34 (weeks 12-33 of treatment)
Over the next 22 weeks, lower extremity strengthening and functional demands were progressed, as shown in Table 1. Progression of exercises was based on patient strength and ability to perform exercises, with focus on proprioceptive training and isolated muscle strengthening activities. Emphasis was placed on hamstring and dorsiflexion strengthening in both open chain and in closed chain through use of single leg stability exercises. Her home program continued to emphasize nerve glides, as previously instructed, as well as active dorsiflexion and knee flexion. Electrical stimulation of the muscles responsible for dorsiflexion was eliminated from the treatment program after visit 16 as the electrical stimulation was not improving the quality of muscle contraction over volitional contraction of the muscles alone. Electrical stimulation was attempted on the hamstrings in order to attempt to improve muscle recruitment, but a contraction could not be elicited within the amount of current tolerated by the patient.
An initial Biodex™ isokinetic test for knee flexion/extension was performed at visit 19 (Table 3). Analysis of peak torque revealed a 62.1% flexion strength deficit at 60 degrees per second and a 49.9% flexion strength deficit at 180 degrees per second when compared to unaffected leg.
Table 3.
Biodex™ isokinetic test results for knee flexion.
| Week | Peak torque in Newton/meters at 60 deg/sec | % Deficit from left leg | Peak torque in Newton/meters at 180 deg/sec | % Deficit from left leg |
|---|---|---|---|---|
| 15 | 15.1 | 62.1 | 13.1 | 49.9 |
| 23 | 34.5 | 35.5 | 27.4 | 29.6 |
| 32 | 31.1 | 46.8 | 24.7 | 42.6 |
| 37 | 44.1 | 7.0 | 26.9 | 32.5 |
| 42 | 38.4 | 22.9 | 30.0 | 23.3 |
| 74 (18 months post injury) | 50.1 | 11.5 | 34.7 | 23.3 |
By the time of re-examination at week 19, the patient was ambulating without restrictions and with a normal pattern during ADLs, however she continued to display a notable foot drop if she tried to walk at a brisk pace. She had returned to biking without limitation. Strength had steadily improved to 4/5 for -hamstrings and 5/5 for eversion and hamstring recruitment was continuing to improve, however dorsiflexion strength did not display a consistent progression in strength staying at 2+/5. Over the next several weeks, the patient noted increased symptoms of diffuse numbness into her lower leg, below the level of the knee if she was not diligent with her home exercises. At week 20, due to the subject's schedule, she missed a few days of exercises and noted more numbness in her lower leg. This went away after she returned to diligently performing her exercises.
She attempted to begin a run/walk program in week 23, but this was difficult as she felt that she did not have as much control over her right foot. She continued to be seen in physical therapy every one to two weeks until week 33, at which point she was allowed to continue her care independently with a home exercise program.
OUTCOMES
Eighteen months after the patient's initial injury and 7 months after her discharge from physical therapy, she returned to the clinic for reassessment. She reported occasional numbness in the right lower leg which resolved with periods of walking. She reported she had returned to running up to 2 miles, 3 times per week and completed a 5 kilometer recreational run. She denied experiencing pain while running but she still described a sense of weakness in her involved extremity. She did not ski the winter following her injury due to fear of reinjury.
Objectively, on the HOS, the patient had improved from 65% to 98% for ADLs and 0% to 95% for sport activities when compared to her initial visit in physical therapy. Manual muscle testing was equal between legs, rated at 5/5 for all previously tested muscles, except great toe extension which was graded at a 4/5 bilaterally. Slump-sit testing revealed slightly more tension on the left leg versus the right but motion was equal. Hamstring flexibility via a passive straight leg raise was 86 degrees of hip flexion on the right and 92 degrees on the left.
Analysis of peak torque via Biodex™ testing (Table 3) revealed a deficit in knee flexion strength of 11.5% at 60 deg/sec and 23.3% at 180 deg/sec when compared to the uninvolved leg. This demonstrates a 50.6 percentage point improvement at 60 deg/sec and 26.6 percentage point improvement at 180 deg/sec when comparing the initial testing session to last testing session. The deficit that remains at the faster testing speed illustrates the patient's incomplete recovery, particularly for higher level activities that require faster speeds of muscular contraction, such as those required in athletics. Table 3 shows the progression of strength via BiodexTM testing over the 6 tests that were performed during the course of PT.
DISCUSSION
In this case, a patient was able to return to near full function following a sciatic nerve injury that occurred following a grade 3 hamstring tear. This is the first report of recovery from this type of combined muscular and nerve injury that did not involve surgical intervention. While it cannot be proven in a case report that the physical therapy interventions were any more effective than time alone, a previous case report does not mention spontaneous improvement of an injury to the sciatic nerve with time alone.6 Furthermore, in the current case report, when the patient stopped performing her nerve glides for a few days around week 20, her symptoms started to return. Through utilization of prescribed physical therapy exercises, the patient was able to regain strength and extensibility in muscles, as well as restore normal neurodynamics. In the author's opinion, these gains together contributed to her successful outcome.
This case report raises the question of whether nerve glides should be a standard part of treatment following a hamstring tear. A Cochrane systematic review of hamstring strain treatment published in 2009 did not include use of neural glides in its analysis due to the limited number and quality of articles that have mentioned the utilization of this intervention.12 The authors of this case report performed a literature search and found two articles that dealt with grade I hamstring strains and the use of sciatic nerve glides.13,14 In these articles, neural glides improved outcomes in patients with hamstring strains. Heiderscheit, Sherry and Silder recently published a commentary on rehabilitation after hamstring strains stating that while there have been some reports of the use of neural mobilizations with grade I strains, the use of neural mobilizations for more severe strains has not been investigated.15 With regard to making neural glides part of a standard treatment regime following a hamstring tear, it is certainly plausible that neural glides could have a prophylactic effect for preventing scar tissue from developing and entrapping nerve structures which lie in close proximity to the hamstring muscle bellies. Caution should be used during early recovery from a severe hamstring strain in case the neural structures were injured during the hamstring tear and the healing process of the hamstring may be adversely affected by motion that is too aggressive. Pain in the hamstring during exercise should be avoided over the first 4-6 weeks post-injury and a nerve sliding technique versus a more aggressive nerve tensioning technique may be best.
In this case, the patient's symptoms did not start to appear until after she reinjured her leg in a seemingly minor slip on a floor 28 days after the initial injury. This is similar to 2 previous case reports in the literature, where neural symptoms did not appear in subjects until after a subsequent injury.3,4 This delayed onset of neural symptoms may indicate that the injury was due more to excessive traction on the nerve sustained during the re-injury/slip versus true entrapment by scar tissue from the initial muscle injury. It is also possible that the injured hamstring muscle did not reactively contract during the re-injury/slip, contributing additional traction/stress to the nerve, thereby exacerbating symptoms.
In retrospect, neural symptoms that presented in this case may not have been recognized immediately by the treating therapist. Nerve glides were not instituted until the patient returned to PT in week 12 after consultation with MDs (8 weeks after onset of neural symptoms). Increased awareness of the possibility of sciatic nerve concurrent injury associated with or following a hamstring injury may have led to quicker recognition of signs and symptoms and as a result earlier intervention addressing the nerve issues. In turn, earlier intervention may have led to quicker resolution of symptoms. However, with a traction type injury sustained during the slip/re-injury as hypothesized in the previous paragraph, earlier institution of nerve gliding may have been detrimental and more gentle nerve mobility interventions may have been more appropriate.
Foot drop due to nerve entrapment following hamstring tears is rarely reported in the literature. To date, only surgery has been reported as an intervention to address the nerve entrapment.3–6,8 The outcomes described by the authors of this case report demonstrate how conservative rehabilitation incorporating strengthening, stretching, proprioceptive training, neural glides and electrical stimulation had the potential to allow the described patient to achieve satisfactory outcomes without the added cost and risks of surgery.
In summary, this case report documents the successful recovery of a patient from a hamstring tear with sciatic nerve involvement through the use of conservative measures. The subject sustained a hamstring tear that led to nerve involvement after reaggravation of the initial injury. EMG findings revealed severe denervation of the tibialis anterior and biceps femoris. Objectively, patient had weakness in these muscles and demonstrated a foot drop during ambulation. Through a rehabilitation program emphasizing sciatic nerve glides and open and closed chain strengthening, the subject was able to return to almost all desired activities. She scored 95% on the sports subscale of the HOS and 98% on the ADL subscale at 18 months post injury. This is the first published case report in the literature describing recovery from sciatic nerve involvement after a hamstring tear that did not involve surgical intervention.
Appendix 1.
The Hip Outcome Scale (Used with permission of Gunderson Lutheran Sportsmedicine).
| Hip Outcome Scale (HOS) Activities of Daily Living Subscale | ||||||
|---|---|---|---|---|---|---|
| Please answer every question with one response that most clearly describes your condition within the past week. If the activity in question is limited by something other than your hip, mark not applicable (N/A). | ||||||
| No difficulty at all | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A | |
| Standing for 15 minutes | ||||||
| Getting into and out of an average car | ||||||
| Putting on socks and shoes | ||||||
| Walking up steep hills | ||||||
| Walking down steep hills | ||||||
| Going up 1 flight of stairs | ||||||
| Going down 1 flight of stairs | ||||||
| Stepping up and down curbs | ||||||
| Deep Squatting | ||||||
| Getting into and out of a bath tub | ||||||
| Sitting for 15 minutes | ||||||
| Walking initially | ||||||
| Walking approximately 10 minutes | ||||||
| Walking 15 minutes or greater | ||||||
| Because of your hip how much difficulty do you have with: | ||||||
| No difficulty at all | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A | |
| Twisting/ pivoting on involved leg | ||||||
| Rolling over in bed | ||||||
| Light to moderate work (standing, walking) | ||||||
| Heavy work (push/pulling, climbing, carrying) | ||||||
| Recreational activities | ||||||
| How would you rate your current level of function during your usual activities of daily living from 0 to 100 with 100 being your level of function prior to your hip problem and 0 being the inability to perform any of your usual daily activities? | ||||||
| __ ____ _____.0% | ||||||
| HOS - Sports Subscale | ||||||
| Because of your hip how much difficulty do you have with: | ||||||
| No difficulty at all | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A | |
| Running one mile | ||||||
| Jumping | ||||||
| Swinging objects like a golf club | ||||||
| Landing | ||||||
| Starting and stopping quickly | ||||||
| Cutting / lateral movements | ||||||
| Low impact activities like fast walking | ||||||
| Ability to perform activity with your normal technique | ||||||
| Ability to participate in your desired sport as long as your would like | ||||||
| How would you rate your current level of function during your usual sports related activities from 0 to 100 with 100 being your level of function prior to your hip problem and 0 being the inability to perform any of your usual daily activities? | ||||||
| __ ____ _____.0% | ||||||
| Overall, how would you rate your current level of function? | ||||||
| Normal Nearly normal Abnormal Severely Abnormal | ||||||
REFERENCES
- 1. Wood DG, Packham I, Trikha SP, et al. Avulsion of the proximal hamstring origin. J Bone Joint Surg Am. 2008;90:2365–74 [DOI] [PubMed] [Google Scholar]
- 2. Sarimo J, Lempainen L, Mattila K, et al. Complete proximal hamstring avulsions: A series of 41 patients with operative treatment. Am J Sport Med. 2008;36(6):1110–1115 [DOI] [PubMed] [Google Scholar]
- 3. Hernesman SC, Hoch AZ, Vetter CS, et al. Foot drop in a marathon runner from chronic complete hamstring tear. Clin J Sport Med. 2003;13(6):365–368 [DOI] [PubMed] [Google Scholar]
- 4. Street CC, Burks RT. Chronic complete hamstring avulsion causing foot drop. Am J Sport Med. 2000;28(4):574–576 [DOI] [PubMed] [Google Scholar]
- 5. Takami H, Takahashi S, Ando M. Late sciatic nerve palsy following avulsion of the biceps femoris muscle from the ischial tuberosity. Arch Orthop Trauma Surg. 2000;120:352–354 [DOI] [PubMed] [Google Scholar]
- 6. Carmody C, Prietto C. Entrapment of the sciatic nerve as a late sequela of injury to the hamstring muscles. J Bone Joint Surg Am. 1995;77A(7):1100–1102 [DOI] [PubMed] [Google Scholar]
- 7. Orava S, Kujala UM. Rupture of the ischial origin of the hamstring muscles. Am J Sport Med. 1995;23(6):702–705 [DOI] [PubMed] [Google Scholar]
- 8. Miller A, Stedman GH, Beisaw NE, et al. Sciatica caused by an avulsion fracture of the ischial tuberosity. J Bone Joint Surg Am. 1987;69A(1):143–145 [PubMed] [Google Scholar]
- 9. Martin RL, Kelly BT, Philippon MJ. Evidence of validity for the Hip Outcome Score (HOS). Combined Sections Meeting of the American Physical Therapy Association, New Orleans, LA, February 25, 2005 [Google Scholar]
- 10. Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004;34:116–125 [DOI] [PubMed] [Google Scholar]
- 11. Butler DS. The Sensitive Nervous System. Adelaide, Australia: Noigroup Publications, 2000 [Google Scholar]
- 12. Mason DL, Dickens VA, Vail A. Rehabilitation for hamstring injuries. Cochrane database of systematic reviews. 2007. Issue 1. Art. No.: CD004575. DOI: 10.1002/14651858.CD004575.pub2. [DOI] [PubMed] [Google Scholar]
- 13. Turl SE, George KP. Adverse neural tension: A factor in repetitive hamstring strain? J Orthop Sports Phys Ther. 1998;27(1):16–21 [DOI] [PubMed] [Google Scholar]
- 14. Kornberg C, Lew P. The effect of stretching neural structures on grade one hamstring injuries. J Orthop Sports Phys Ther. 1989;13:481–487 [DOI] [PubMed] [Google Scholar]
- 15. Heiderscheit BC, Sherry MA, Silder A, et al. Hamstring strain injuries: Recommendations for diagnosis, rehabilitation and injury prevention. J Orthop Sports Phys Ther. 2010;40(2):67–81 [DOI] [PMC free article] [PubMed] [Google Scholar]