Abstract
Objective
To compare patient-reported and observer-rated shared decision making (SDM) use for colorectal cancer (CRC) screening and evaluate patient, physician and patient-reported relational communication factors associated with patient-reported use of shared CRC screening decisions.
Methods
Study physicians are salaried primary care providers. Patients are insured, aged 50-80 and due for CRC screening. Audio-recordings from 363 primary care visits were observer-coded for elements of SDM. A post-visit patient survey assessed patient-reported decision-making processes and relational communication during visit. Association of patient-reported SDM with observer-rated elements of SDM, as well as patient, physician and relational communication factors were evaluated using generalized estimating equations.
Results
70% of patients preferred SDM for preventive health decisions, 47% of patients reported use of a SDM process, and only one of the screening discussions included all four elements of SDM per observer ratings. Patient report of SDM use was not associated with observer-rated elements of SDM, but was significantly associated with female physician gender and patient-reported relational communication.
Conclusion
Inconsistencies exist between patient reports and observer ratings of SDM for CRC screening.
Practice Implications
Future studies are needed to understand whether SDM that is patient-reported, observer-rated or both are associated with informed and value-concordant CRC screening decisions.
1. Introduction
Shared decision making (SDM) has garnered much attention in recent years and its use is now advocated by the United States Preventive Services Task Force (USPSTF) when making screening and chemoprevention recommendations to patients [1]. The justification for doing so is predicated on the assumption that patient-physician partnership is needed to ensure that decisions about preventive services take into consideration the needs, values and preferences of the patient [1]. This is particularly true in the case of colorectal cancer (CRC) screening where multiple effective and recommended screening modalities exist [2, 3].
However, providing a clear and concise definition of SDM has proven difficult and has led to inconsistent measurement of the concept [4-7]. When studying communication content and function, one commonly used definition consistent with that advocated by the USPSTF is that proposed by Charles, et al. [8] where shared decision making is characterized by four necessary components: (1) both the physician and patient are involved in the treatment decision-making process; (2) both the physician and patient share information with each other; (3) both the physician and the patient take steps to participate in the decision-making process by expressing treatment preferences; and (4) a treatment decision is made and both the physician and patient agree on the treatment to implement. Yet, there is evidence that SDM may be defined differently by patients [8-10].
The primary aims of this study are: 1) to evaluate the concordance between patient preferences for SDM and its use in practice for CRC screening decision making, and 2) to evaluate the concordance between patient-reported use of a shared decision and observer-ratings of the presence of the four necessary components of SDM as defined by Charles et al. [8] in the context of colorectal cancer screening decision making. We also explore patient and physician characteristics as well as relational communication factors associated with patient reports of a shared CRC screening decision.
2. Methods
2.1 Study Setting and Participants
Physician and patient samples were drawn from the universe of primary care physicians and patients in a large, integrated health system located in southeast Michigan. Eligible physician participants were family and general internal medicine physicians practicing within the health system’s salaried multi-specialty medical group. The medical group staffs a large teaching hospital and 26 ambulatory care clinics located in Detroit and its surrounding suburbs. Physicians were recruited for participation via email and personal telephone calls by the study principal investigator (JEL).
Patient participants were insured, aged 50 to 80 years and due for colorectal cancer screening at the time of a scheduled routine annual physical exam with a study participating physician between February 2007 and June 2009. Patients were recruited for participation via a letter of study introduction followed by telephone contact. Study participation included completion of a pre-visit telephone survey, audio-recording of the scheduled office visit and completion of a brief post-visit survey. Those verbally agreeing to study participation completed a brief telephone survey and were asked to arrive at their scheduled appointment approximately 15 minutes early to enable completion of informed consent. All aspects of the research protocol were approved by the medical group’s institutional review board (IRB).
2.2 Data Sources and Measures
2.2.1 Patient Surveys and Measures of Patient Perceptions
A structured pre-visit telephone survey was administered at the time of subject recruitment. The survey was used to confirm study eligibility and solicit information on patient preferences for colorectal cancer screening modality attributes as well as preferences for types of information and decision making processes when making preventive health decisions [11]. The survey also included questions regarding the patient’s socio-demographic characteristics (age, gender, race, education, household income and employment status) and a number of other patient-reported factors [12-17].
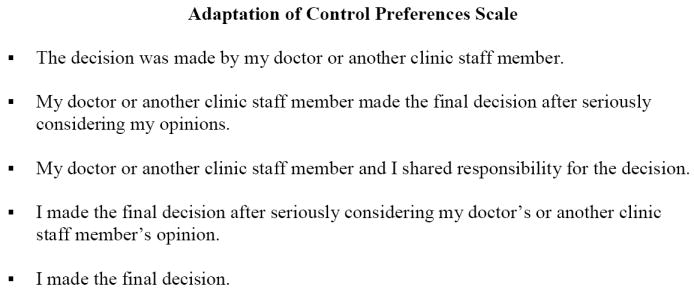
Upon completion of the office visit, patients were asked to complete a brief post-visit survey. This survey was structured and interviewer administered, and included questions adapted from Degner’s Control Preferences Scale [11] to collect the patient’s perceptions of the decision-making process used during the visit for five preventive health services (including colorectal cancer screening) [Figure 1]. From the colorectal cancer screening specific item, we constructed a variable that reflected whether or not the patient reported the colorectal cancer decision-making process that occurred during the visit as shared or not. Only those patients who reported that the responsibility for the decision had been shared by both physician and patient were coded as shared, all other responses were coded as not shared. The post-visit survey also included 20 items from the Relational Communication Scale which uses Likert items ranging from one to seven to assess patient perceptions of relational communication [18].
Fig. 1. Adaptation of Degner’s Control Preferences Scale.
2.2.2 Office Visit Audio-recordings and Observer-rated Measures of Communication
Office visits were audio-recorded for task-oriented communication using a small digital recording device. All recordings were transcribed prior to coding. Members of the research team developed a structured coding form based upon a priori identified concepts in addition to using a grounded approach to identify emerging themes. Coders then used forms that enabled response capture via scanning technology. The coding form included, among other things, items consistent with Charles et al.’s four elements of shared decision making [8]. Three trained research assistants coded the visits by listening to the audio-recordings while following the associated transcript. Inter-rater reliability was assessed by having approximately 10% of the recordings (n=44) coded by all 3 research assistants. Cohen’s Kappas for the four elements of SDM ranged from .48 (element 1) to .86 (element 2). Because of the modest Kappa for element 1, we recoded each visit for this element using a consensus coding approach across three coders. Results are presented for codes derived using this consensus process for element 1. Cohen’s Kappas for the remaining elements ranged from .60 (element 4) to .86 (element 2).
2.2.3 Physician Characteristics
Physician characteristics were available via health system records and included age, gender, race, and specialty certification (family medicine or general internal medicine).
2.3 Statistical Methods
The association of patient-reported SDM and coder-rated task-oriented elements of SDM was assessed using univariate logistic regression. Similarly, differences in patient characteristics, physician characteristics, and relational communication factors, by patient-reported use of a SDM process, were also assessed using univariate logistic regression. Finally, a multivariable logistic regression model was fit to assess the association of each of these factors and observer-rated SDM content simultaneously with patient-reported use of SDM. An exploratory factor analysis was used to summarize items from the Relational Communication Scale for inclusion in the multivariable model. Scale reliability from the parameters of the factor model was estimated with Omega (Ω=.93) [19]. Due to the skewness of item distribution, we used the robust maximum likelihood estimator. All logistic regression models were fit using generalized estimating equation methods to account for non-independence of patients seen by the same physician.
3. Results
3.1 Sample characteristics
Seventy-seven physicians agreed to study participation (47% physician participation rate) and 500 patients agreed to study participation (44% patient participation rate). Table 1 compares physician participants and non-participants, and patient participants and non-participants. Physician participants did not differ from non-participants in terms of age or gender, but physician participants were more likely to be of African American race (16% vs. 3%) or a practicing family medicine physician (45% vs. 29%) compared to physician non-participants. Patient participants did not differ from patient non-participants in terms of race, or marital status, however they were significantly younger (58 years of age vs. 60 years of age) and tended more likely to be female (66% vs. 60%).
Table 1.
Comparison of Physician and Patient Study Participants and NonParticipants
| Physician | Participants (N=77) | Non-Participants (N=86) | P-values |
|---|---|---|---|
| Mean Age in Years (sd) | 48 (9) | 49 (9) | 0.62 |
| Female (%) | 57 | 49 | 0.35 |
| Race (%) | |||
| African American | 16 | 3 | <0.01 |
| White | 55 | 47 | |
| Other | 29 | 50 | |
| Specialty (%) | 0.04 | ||
| General Internist | 55 | 71 | |
| Family Medicine | 45 | 29 | |
| Patient | Participants (N=500) | Non-Participants (N=510) | P-values |
| Mean Age in Years (sd) | 58(8) | 60 (8) | <0.01 |
| Female (%) | 66 | 60 | 0.05 |
| Race (%) | |||
| African American | 27 | 23 | 0.33 |
| White | 66 | 70 | |
| Other | 7 | 7 | |
| Married (%) | 70 | 72 | 0.53 |
All p-values for tests of proportions were calculated using Fisher’s Exact tests.
P-values for tests of means were calculated using Student’s t-tests.
The 500 study attended visits resulted in 485 audible recordings. Among these, 363 visits among 62 physicians are included here. Excluded were visits for which it was determined there was no talk regarding colorectal cancer screening (n=39), the patient was not eligible for (n=17) or already scheduled for colorectal cancer screening (n=11), presented with symptoms (n=1) or did not answer the survey questions regarding SDM (n=54). The mean age of physicians (N=62) was 49 years of age (sd=8.6). Seventy percent were general internal medicine physicians and 30% family medicine physicians. Fifty-six percent were female, and 48% were white, 17% African American, and 34% were of another race. The average number of audio-recorded visits per physician was 7.5 patients, (range 2-20, sd=4.8).
The mean age of patients (N=363) was 58 years of age (sd=7.8). Sixty-three percent of the patient sample was female. Sixty-five percent reported they were white, 28% African American, and 7% reported being of another race. Almost three-quarters of the sample (73%) reported attending college, 23% reported having a high school diploma, and 4% reported having less than a high school diploma. Sixty-four percent indicated they were employed at the time of study participation, and 55% reported earning a combined household income of more than $60,000 per year.
3.2 Patient Preferences for SDM
At the time of the pre-survey, 70% of patients indicated a preference to share responsibility with their doctor when making preventive health decisions. Eighteen percent indicated a preference to make the decision themselves or after considering input from their doctor and 12% indicated a preference to delegate decision making responsibility to their doctor either completely or after their doctor considered their input.
After the visit, less than half of patients (47%) reported that they shared responsibility with their doctor when making a CRC screening decision. Thirty-six percent reported making the decision and 17% reported their doctor making the decision. Overall, while 49% of patients reported a colorectal cancer screening decision making process consistent with their preferences, 32% of patients reported being involved in the decision more than they preferred and 19% less than they preferred.
3.3 Comparison of Observer-rated and Patient-reported SDM for Colorectal Cancer
Although 47% of patients reported that they shared responsibility with their doctor when making the CRC screening decision, only one of the patient-physician discussions of colorectal cancer screening was coded by observers as including all four elements of SDM (Table 2). Despite there being only one visit that included all four elements, each element was identified as in use, albeit to varying degrees. Observers coded less than half of the colorectal cancer discussions as including involvement of both the physician and patient (element 1) and approximately a third as having both patients and physicians sharing information (element 2). Treatment preferences (element 3) were rarely discussed (3%) and articulation of an agreement regarding the screening plan (element 4) was only slightly less rare (7%). When evaluating the association of patient-reported SDM with each of the four observer-rated elements of SDM, we found no statistically significant association (Table 2).
Table 2.
Use of a Shared Colorectal Screening Decision-making Process by Patient Report and Observer Ratings.
| All Visits N=363 | Patient Reported Shared Decision Making Experience N=171 | No Patient Reported Shared Decision Making Experience N=192 | p values | |
|---|---|---|---|---|
|
Observer-Rated SDM |
||||
| Element 1: MD and patient involved in DM process |
40% | 38% | 43% | 0.22 |
| Element 2: MD and patient share information |
29% | 31% | 28% | 0.31 |
| Element 3: MD and patient express treatment preferences |
4% | 3% | 4% | 0.59 |
| Element 4: MD and patient agree on treatment |
7% | 5% | 8% | 0.25 |
| Contained all 4 Elements | <1% | 1% | 0% | N/A |
3.4 Patient, Physician and Relational Communication Characteristics Associated with Patient-reported Use of a Shared Decision-making Process
When unadjusted comparisons are made, patients who reported sharing the CRC screening decision-making responsibility did not differ in terms of socio-demographic characteristics when compared to those who did not (Table 3). But prior to adjustment for other factors, patients who reported sharing decision-making responsibility with their physicians were significantly more likely to have seen a female physician and significantly more likely to have seen an African American physician—all but 3 of whom were women in the study sample (Table 4).
Table 3.
Patient Characteristics by Patient-reported Use of a Shared Decision-Making Process for Colorectal Cancer Screening.
| Patient Characteristic | No SDM N= 192 | SDM N= 171 | p-value | |
|---|---|---|---|---|
| Mean Age in Years (Std Dev) | 58.5 (8.1) | 58.4 (7.5) | 0.65 | |
| Female (%) | 62% | 64% | 0.26 | |
| Race (%) | African American | 28% | 29% | 0.60 |
| White | 66% | 64% | ||
| Other | 7% | 7% | ||
| Education (%) | Less Than HS Diploma | 4% | 4% | 0.70 |
| HS Diploma/GED | 25% | 22% | ||
| Some College or More | 71% | 74% | ||
| Household Income (%) | < $20,000 | 6% | 7% | 0.48 |
| $20-$60,000 | 36% | 40% | ||
| > $60,000 | 58% | 53% | ||
| Employment (%) | Employed/Working for pay | 66% | 62% | 0.63 |
| Unemployed/Retired/Homemaker | 34% | 38% | ||
Table 4.
Physician Characteristics by Patient-reported Use of a Shared Decision-Making Process for Colorectal Cancer Screening.
| Physician Characteristic | No SDM (N= 193) | SDM (N= 171) | P value | |
|---|---|---|---|---|
| Mean Age in Years (Std Dev) | 49.9 (7.7) | 49.2 (7.5) | 0.13 | |
| Female (%) | 51% | 61% | <0.01 | |
| Race (%) | African American | 37% | 59% | 0.02 |
| White | 20% | 16% | ||
| Other | 43% | 25% | ||
| Specialty (%) | Family Medicine | 32% | 30% | 0.80 |
| Internal Medicine | 68% | 70% | ||
Patients who reported sharing CRC screening decision making responsibility were in general more likely to report that the relational communication with their physician during the visit was positive. As illustrated in Table 5, eleven of the twenty relational communication scale items were significantly associated with the patient reporting the use of a shared colorectal cancer screening decision-making process. Results from the exploratory factor analysis indicated that there was one 10-item factor underlying the item responses (RMSEA =.076; CFI=.906, TLI=.878) The ten items included: my doctor (1) was interested in talking to me; (2) seemed to care if I liked him/her; (3) was sincere; (4) wanted me to trust him/her; (5) was willing to listen to me; (6) was open to my ideas; (7) was honest in communicating with me; (8) seemed nervous in my presence; (9) was comfortable interacting with me; and (10) wanted to cooperate with me. As the factor score estimates for this item were also significantly associated with patient reports of sharing the colorectal cancer decision making responsibility with their physician (p<0.05), for multivariable modeling, the factor score estimates were used as a latent variable measuring relational communication as reported by the patient.
Table 5.
Patient reported Relational Communication by Patient-reported Use of a Shared Decision-Making Process for Colorectal Cancer Screening.
| Relational Communication Scale Items+ | No SDM (N=192) | SDM (N= 171) | P value |
|---|---|---|---|
| 1. My doctor was interested in talking to me. | 6.2 (1.7) | 6.6 (1.3) | <0.01 |
| 2. My doctor seemed to care if I liked him/her. | 5.6 (1.8) | 6.1 (1.5) | <0.01 |
| 3. My doctor was sincere. | 6.4 (1.5) | 6.7 (1.1) | 0.03 |
| 4. My doctor wanted me to trust him/her. | 6.2 (1.5) | 6.5 (1.2) | 0.01 |
| 5. My doctor was willing to listen to me. | 6.5 (1.4) | 6.7 (1.0) | 0.04 |
| 6. My doctor was open to my ideas. | 6.2 (1.5) | 6.6 (1.0) | <0.01 |
| 7. My doctor was honest in communicating with me. | 6.5 (1.5) | 6.8 (1.0) | 0.03 |
| 8. My doctor was comfortable interacting with me. | 6.4 (1.6) | 6.8 (0.9) | <0.01 |
| 9. My doctor tried to control the interaction. | 2.3 (1.8) | 1.9 (1.6) | <0.01 |
| 10. My doctor wanted to cooperate with me. | 6.1 (1.6) | 6.4 (1.3) | 0.03 |
| 11. My doctor wanted to stick to the main purpose of the interaction. | 3.9 (2.4) | 3.5 (2.4) | 0.11 |
| 12. My doctor felt very tense talking to me. | 6.5 (1.3) | 6.7 (0.8) | 0.02 |
| 13. My doctor created a sense of distance between us. | 6.4 (1.4) | 6.5 (1.4) | 0.66 |
| 14. My doctor acted bored by our conversation. | 6.7 (1.1) | 6.7 (1.1) | 0.86 |
| 15. My doctor seemed nervous in my presence. | 6.6 (1.3) | 6.8 (0.8) | 0.06 |
| 16. My doctor made the interaction very formal. | 3.1 (2.3) | 3.2 (2.5) | 0.77 |
| 17. My doctor attempted to persuade me. | 3.1 (2.3) | 2.7 (2.2) | 0.10 |
| 18. My doctor didn’t attempt to influence me. | 3.7 (2.4) | 3.5 (2.5) | 0.60 |
| 19. My doctor tried to gain my approval. | 3.8 (2.2) | 3.9 (2.4) | 0.69 |
| 20. My doctor did not treat me as an equal. | 6.4 (1.5) | 6.5 (1.5) | 0.34 |
Items scored on a 7 point Likert scale with 1=strongly disagree to 7=strongly agree. Items 12 – 15 & 20 reverse coded for analyses.
The results from the multivariable logistic regression model are reported in Table 6. The model included socio-demographic characteristics of the patient and physician as well as physician specialty (i.e., family vs. general internal medicine) and the relational communication 10-item factor. We also include binary measures reflective of patient-physician race and gender concordance. As illustrated in the table, only two of the variables assessed were significantly associated with patient reports of a shared colorectal cancer screening decision after adjusting for factors simultaneously: female physician gender and patient-reported positive relational communication.
Table 6.
Patient, Physician and Relational Communication Factors Associated with Patient Reports of a Shared Decision-making Process for Colorectal Cancer Screening: Multivariable Logistic Regression Results (N=326).
| Odds Ratio (95% CI) | P value | |
|---|---|---|
| Patient and Physician Socio-demographic Characteristics | ||
| Patient Age | 0.10 (0.9-1.0) | 0.84 |
| Patient Female Gender | 1.14 (0.9-2.0) | 0.67 |
| Patient Race | ||
| African American | 1.0 | |
| White | 1.22 (0.7 – 1.9) | 0.40 |
| Other | 1.14 (0.6 – 2.0) | 0.85 |
| Patient Education | ||
| Less than High School Diploma | 1.16 (0.3-4.8) | 0.84 |
| High School Diploma | 1.0 | |
| Some College or More | 1.10 (0.7-1.8) | 0.69 |
| Patient Income | ||
| <$20,000 | 1.23 (0.5-3.1) | 0.67 |
| $20,000 - $60,000 | 1.0 | |
| >$60,000 | 0.79 (0.5-1.4) | 0.41 |
| Patient Unemployed Status | 1.36 (0.7-2.5) | 0.32 |
| Physician Male Gender | 0.57 (0.4-0.9) | <0.02 |
| Physician Race | ||
| African American | 1.0 | |
| White | 0.89 (0.5-1.5) | 0.65 |
| Other | 0.74 (0.4-1.3) | 0.29 |
| Physician Age in Years | 0.99 (0.9, 1.0) | 0.32 |
| General Internal Medicine | 0.99 (0.7-1.4) | 0.96 |
| Family Medicine | 1.0 | |
| Physician-Patient Race Concordance | 0.86 (0.6-1.2) | 0.40 |
| Physician-Patient Gender Concordance | 0.88 (0.5-1.6) | 0.66 |
| Observer-rated Elements of SDM | ||
| Element 1: MD and patient involved in DM process | 0.76 (0.5-1.2) | 0.27 |
| Element 2: MD and patient share information | 1.01 (0.6-1.6) | 0.98 |
| Element 3: MD and patient express treatment preferences | 0.60 (0.2-1.8) | 0.37 |
| Element 4: MD and patient agree on treatment | 0.77 (0.3-2.0) | 0.60 |
| Relational Communication | ||
| Relational Communication Latent Factor Score | 1.33 (1.0-1.7) | 0.03 |
4. Discussion & Conclusion
4.1 Discussion
Despite 70% of patients indicating at the time of the pre-visit survey that they prefer a shared decision-making process when making preventive health decisions, only 47% of patients reported after their visit that the colorectal cancer screening decision was in fact shared with their physician. Furthermore, when established criteria for shared decision making [9] are used, only one colorectal cancer screening discussion was coded as containing all the necessary elements for shared decision making. These findings are consistent with those of others who have highlighted differences between patient preferences for SDM and the decision making process used [8-10] as well as differences in patient perceptions and observer-ratings of SDM, [8, 9, 20-22] although, to our knowledge, our study is the first to do so in the context of the colorectal cancer screening decision. As prior research has also found better outcomes with a match between patient preferences for and patient-reported decisional involvement [8, 23], it seems important to strive for such concordances in practice. Yet, as many of the methods used to study SDM reflect professional criteria--and not patient perceptions—our ability to understand when such concordances exist is currently limited as is our ability to understand how to improve decision making processes in a manner that is consistent with patient preferences for SDM.
In fact, we know little about how patients define what constitutes a shared decision. What is clear from results here is that a patient’s perception of ‘sharing’ in responsibility for the CRC screening decision is not related to the quality of the decision making process as defined by the four elements of SDM outlined by Charles and colleagues [8]. Instead, the more positive the relational communication the patient reported as occurring during the visit, the more likely the patient was to report that they shared in the CRC screening decision. Central to the measure of relational communication used here are the concepts of receptivity and trust. Therefore, it seems that some intrinsic relationship may exist between patient perceived receptivity/trust and SDM. Interestingly, interpersonal trust between patient and physician has been defined in the literature as, “expertise, caring and communication,” factors that are not explicit components of the observer determined definition of SDM used here [24]. Furthermore, patients appear to demonstrate more trust for physicians who are competent, committed, open and informative, also attributes that are not explicitly considered in established professional criteria for SDM [25, 26]. From our results, it would appear that trust via its role in relational communication maybe central to how patients conceptualize the notion of SDM in the context of colorectal cancer screening decision making.
Epstein and Street [26] have recently suggested that relational communication is synonymous with fostering healing relationships, responding to emotions, exchanging information and making decisions. Perhaps from patients’ perspectives, SDM has more to do with being heard than the actual content of the words exchanged. When asked for their perspective on SDM, African American patients with diabetes do not highlight the need for deliberations within the clinical encounter, but do describe the importance of (1) being able to “tell their story,” (2) being presented with care options and their physician’s recommendation, and (3) the ability to select and act upon this recommendation [5]. They also acknowledge their ability to follow their physician’s recommendation, agree/disagree openly with their physician, or decide whether or not to adhere once home all represent ways to ‘share’ in the decision making process.
Among all of the patient characteristics and physician characteristics examined for an association with patient reports of a shared decision-making process, only seeing a female physician was significantly associated with patients’ greater likelihood of reporting that a shared decision occurred. It remains unclear exactly what it is that occurs during visits with female physicians that leads patients to be more likely to label colorectal cancer screening decisions made during office visits as shared. However, there is evidence that patient trust is higher with female physicians [27], and that female physicians have been found to engage in more socio-emotional talk [28, 29] and be more likely to facilitate partnership and patient participation in the medical exchange as well as to spend more time with their patients [30, 31].
4.2 Conclusion
In summary, we found a lack of concordance between both patient preferences for SDM and the CRC screening decision making processes used in practice as well as between patient reports of sharing in the CRC screening decision and observer-ratings of the use of SDM when based on professionally established SDM criteria. Although we did not find an association between the task-oriented conversation generally considered to be consistent with a shared decision-making process, we did find that patients who reported positive relational communication with their physician were more likely to report sharing in the CRC screening decision. While the results here point to the importance of relational communication in patient perceptions of a shared colorectal cancer screening decision, there maybe task-oriented communication not evaluated here that is also associated with patient perceptions of SDM.
4.3 Limitations
These data were drawn from a single health care organization and the degree to which these findings are generalizable to other healthcare contexts is not known. Furthermore, although the sample size of over 350 patients and 60 physicians is quite large by qualitative research standards, such a sample size precludes the addition of other potentially important factors in the multivariable model. These include other aspects of conversation content such as the use of patient and physician questioning or the types of specific information shared.
4.4 Practice Implications
As currently conceptualized, SDM in the context of CRC screening is neither used in practice nor reflective of patients’ perceptions of SDM. Given that SDM processes are recommended [1], tend to be preferred by patients [32, 33], and associated with improved patient satisfaction and behavioral outcomes such as adherence to evidence-based care and improvements in functional status [8, 26, 34], it seems critical to better understand how patients conceptualize SDM in the context of colorectal cancer screening and more generally. Furthermore, there is a need to clarify whether SDM that is patient-reported, observer-rated or both is associated with informed and value concordant CRC screening decisions. Without a better understanding of this desired concept, our ability to understand how to improve decision making in a manner consistent with patient preferences will remain elusive. In the meantime, improving relational communication and building trusting relationships may lead patients to perceive greater participation in the CRC screening decision.
Acknowledgments
With our gratitude and appreciation to Levent Dumenci for his assistance with the factor analysis and the research assistant team: Kelly McCormick, Emily Rose, Cindy Chidi and Max Kendall for their diligence and continued hard work, and two anonymous reviewers for their thoughtful suggestions.
Role of funding: This work was supported by a grant from the National Institutes of Health. The funding source had no involvement in data collection, analysis, or the preparation of this manuscript.
Footnotes
Conflict of Interest The authors state no actual or potential conflict of interest, including financial, personal or organizational.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sheridan SL, Harris RP, Woolf SH. Shared decision making about screening and chemoprevention: a suggested approach from the U.S. Preventive Services Task Force. Am J Prev Med. 2004;26:56–66. doi: 10.1016/j.amepre.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 2.US Preventive Services Task Force. Screening for CRC: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149:627–37. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 3.Levin B, Lieberman DA, McFarland B, Andrews KS, Brooks D, Bond J, Dash C, Giardiello FM, Glick S, Johnson D, Johnson CD, Levin TR, Pickhardt PJ, Rex DK, Smith RA, Thorson A, Winawer SJ American Cancer Society CRC Advisory Group; US Multi-Society Task Force; American College of Radiology Colon Cancer Committee. Screening and surveillance for the early detection of CRC and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on CRC, and the American College of Radiology. Gastroenterology. 2008;134:1570–95. doi: 10.1053/j.gastro.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Makoul G, Clayman M. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60:301–12. doi: 10.1016/j.pec.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Peek ME, Quinn MT, Gorawara-Bhat R, Odoms-Young A, Wilson SC, Chin MH. How is shared decision-making defined among African-Americans with diabetes? Patient Educ Couns. 2008;72:450–8. doi: 10.1016/j.pec.2008.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elwyn G, Edwards A, Kinnersley P. Shared decision-making in primary care: the neglected second half of the consultation. Brit J Gen Pract. 1999;49:477–82. [PMC free article] [PubMed] [Google Scholar]
- 7.Coulter A. Partnerships with patients: the pros and cons of shared clinical decision-making. J Health Serv Res Policy. 1997;2:112–21. doi: 10.1177/135581969700200209. [DOI] [PubMed] [Google Scholar]
- 8.Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1997;49:651–61. doi: 10.1016/s0277-9536(99)00145-8. [DOI] [PubMed] [Google Scholar]
- 9.Street RL., Jr Analyzing communication in medical consultations: do behavioral measures correspond to patients’ perceptions? Med Care. 1992;30:976–88. doi: 10.1097/00005650-199211000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Saba G, Wong S, Schillinger D, Fernandez A, Somkin C, Wilson C, Grumbach K. Shared decision making and the experience of partnership in primary care. Ann Fam Med. 2006;4:54–62. doi: 10.1370/afm.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Degner LF, Kristjanson LJ, Bowman D, Sloan JA, Carriere KC, O’Neil J, Bilodeau B, Watson P, Mueller B. Information needs and decisional preferences in women with breast Cancer. JAMA. 1997;277:1485–92. [PubMed] [Google Scholar]
- 12.Pinsky PF, Kramer BS, Reding D, Buys S. Reported family history of cancer in the prostate, lung, colorectal, and ovarian cancer screening trial. Am J Epidemiol. 2003;157:792–99. doi: 10.1093/aje/kwg043. [DOI] [PubMed] [Google Scholar]
- 13.Vernon SW. Development and validation of an instrument to measure factors related to colorectal cancer screening adherence. Cancer Epidemiol Biomarkers Prev. 1997;6:825–32. [PubMed] [Google Scholar]
- 14.Solomon LS, Hays RD, Zaslavsky AM, Ding L, Cleary PD. Psychometric properties of a group-level consumer assessment of health plans study (CAHPS) instrument. Med Care. 2005;43:53–60. [PubMed] [Google Scholar]
- 15.Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 16.Flocke S. Measuring attributes of primary care: development of a new instrument. J Fam Pract. 1997;45:64–74. [PubMed] [Google Scholar]
- 17.Allen JP, Wilson VB, editors. Assessing alcohol problems: A guide for clinicians and researchers. 2. National Institute of Alcohols Abuse and Alcoholism. US Department of Health and Human Services. Public Health Service. National Institutes of Health; 2003. [Google Scholar]
- 18.Burgoon JK, Hale JL. Validation and measurement of the fundamental themes of relational communication. Commun Monogr. 1987;54:19–41. [Google Scholar]
- 19.McDonald RP. Test theory: A unified treatment. New Jersey: Lawrence Erlbaum Associates; 1999. [Google Scholar]
- 20.Entwistle VA, Skea ZC, O’Donnell MT. Decisions about treatment: interpretations of two measures of control by women having a hysterectomy. Soc Sci Med. 2001;53:721–32. doi: 10.1016/s0277-9536(00)00382-8. [DOI] [PubMed] [Google Scholar]
- 21.Entwistle VA, Watt IS, Gilhooly K, Bugge C, Haites N, Walker AE. Assessing patients’ participation and quality of decision-making: insights from a study of routine practice in diverse settings. Patient Educ Couns. 2004;55:105–13. doi: 10.1016/j.pec.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 22.Bradley JG, Zia MJ, Hamilton N. Patient preferences for control in medical decision making: a scenario-based approach. Fam Med. 1996;28:496–501. [PubMed] [Google Scholar]
- 23.Lanz PM, Janz NK, Fagerlin A, Schwartz K, Lakhani I, Salem B, Katz S. Satisfaction with surgery outcomes and the decision process in a population-based sample of women with breast cancer. Health Serv Res. 2005;40:745–67. doi: 10.1111/j.1475-6773.2005.00383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kraetschmer N, Sharpe N, Urowitz S, Deber R. How does trust affect patient preferences for participation in decision-making? Health Expect. 2004;7:317–26. doi: 10.1111/j.1369-7625.2004.00296.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salkeld G, Solomon M, Short L, Butow PN. A matter of trust—patient’s views on decision-making in colorectal cancer. Health Expect. 2004;7:104–14. doi: 10.1111/j.1369-7625.2004.00257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Epstein RM, Street RL., Jr . Patient-centered communication in cancer care: promoting healing and reducing suffering. National Cancer Institute, NIH Publication No. 07-6225; Bethesda, MD: 2007. [Google Scholar]
- 27.Derose KP, Hays RD, McCaffrey DF, Baker DW. Does physician gender affect satisfaction of men and women visiting the emergency department? J Gen Intern Med. 2001;16:218–26. doi: 10.1046/j.1525-1497.2001.016004218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee YY, Lin JL. Trust but Verify: The interactive effects of trust and autonomy preferences on health outcomes. Health Care Anal. 2009;17:244–60. doi: 10.1007/s10728-008-0100-1. [DOI] [PubMed] [Google Scholar]
- 29.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288:756–64. doi: 10.1001/jama.288.6.756. [DOI] [PubMed] [Google Scholar]
- 30.Roter DL, Hall JA. Why physician gender matters in shaping the physician-patient relationship. J Womens Health. 1998;7:1093–97. doi: 10.1089/jwh.1998.7.1093. [DOI] [PubMed] [Google Scholar]
- 31.Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, Ford DE. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282:583–9. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 32.Coulter A. Patient information and shared decision-making in cancer care. Brit J Cancer. 2003;89:S15–16. doi: 10.1038/sj.bjc.6601080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carlsen B, Aakvik A. Patient involvement in clinical decision making: the effect of GP attitude on patient satisfaction. Health Expect. 2006;9:148–57. doi: 10.1111/j.1369-7625.2006.00385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stewart MA. Effective physician-patient communication and health outcomes: A review. Can Med Assoc J. 1995;152:1423–1433. [PMC free article] [PubMed] [Google Scholar]


