Abstract
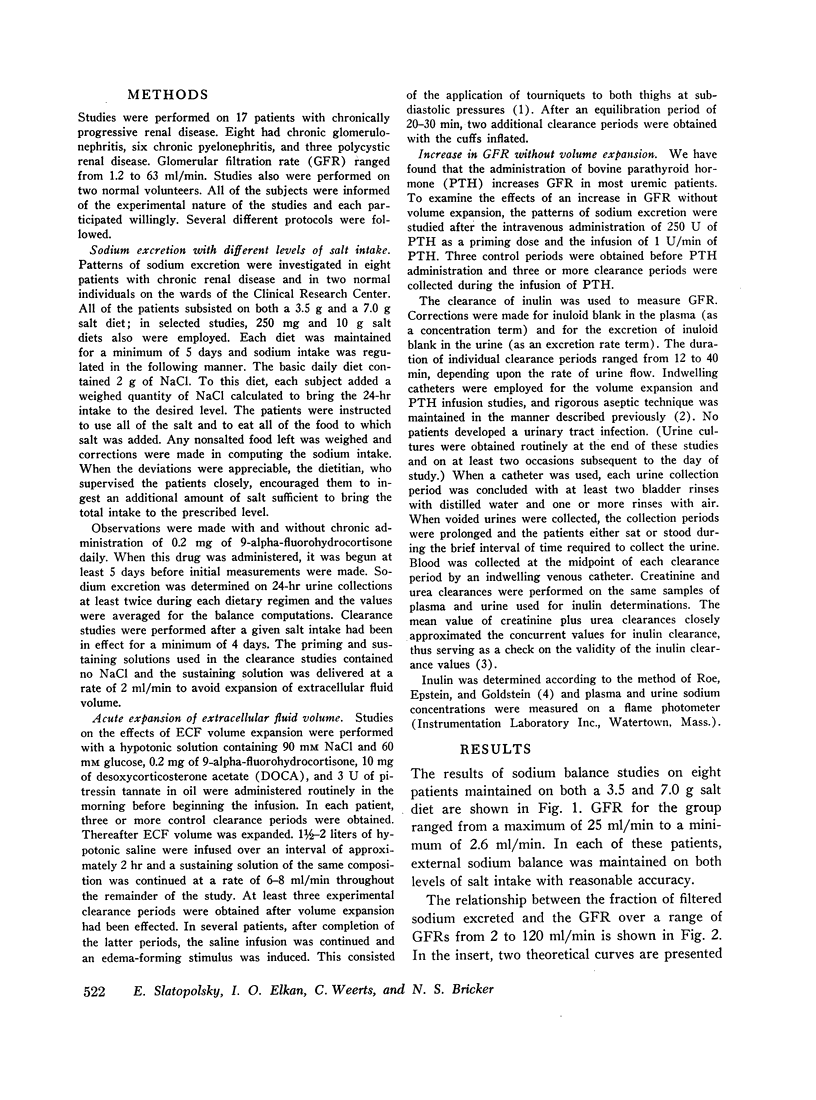
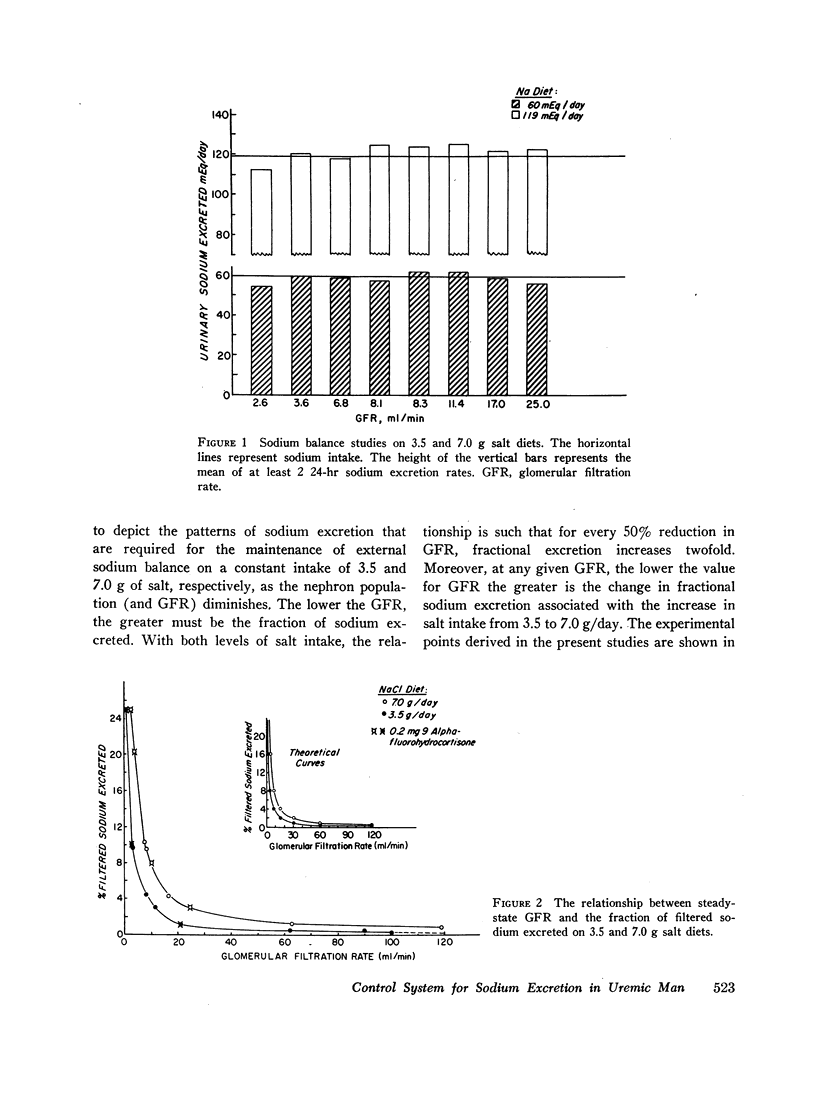
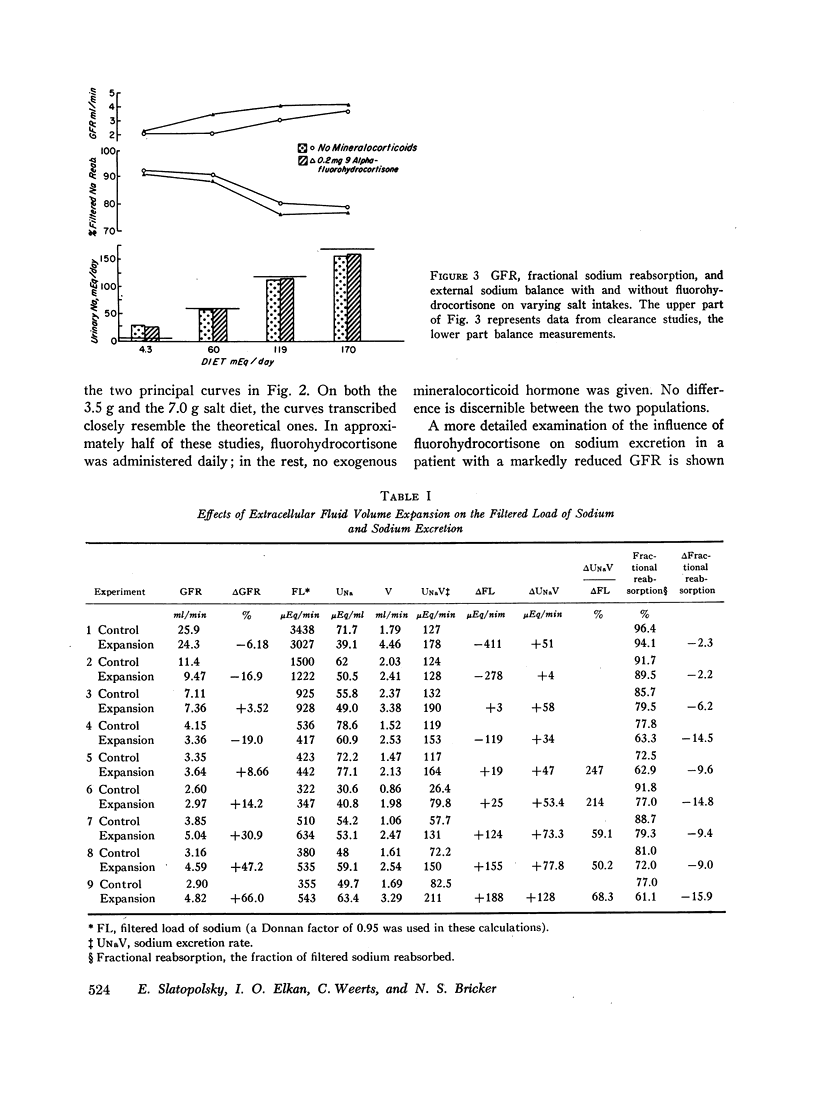
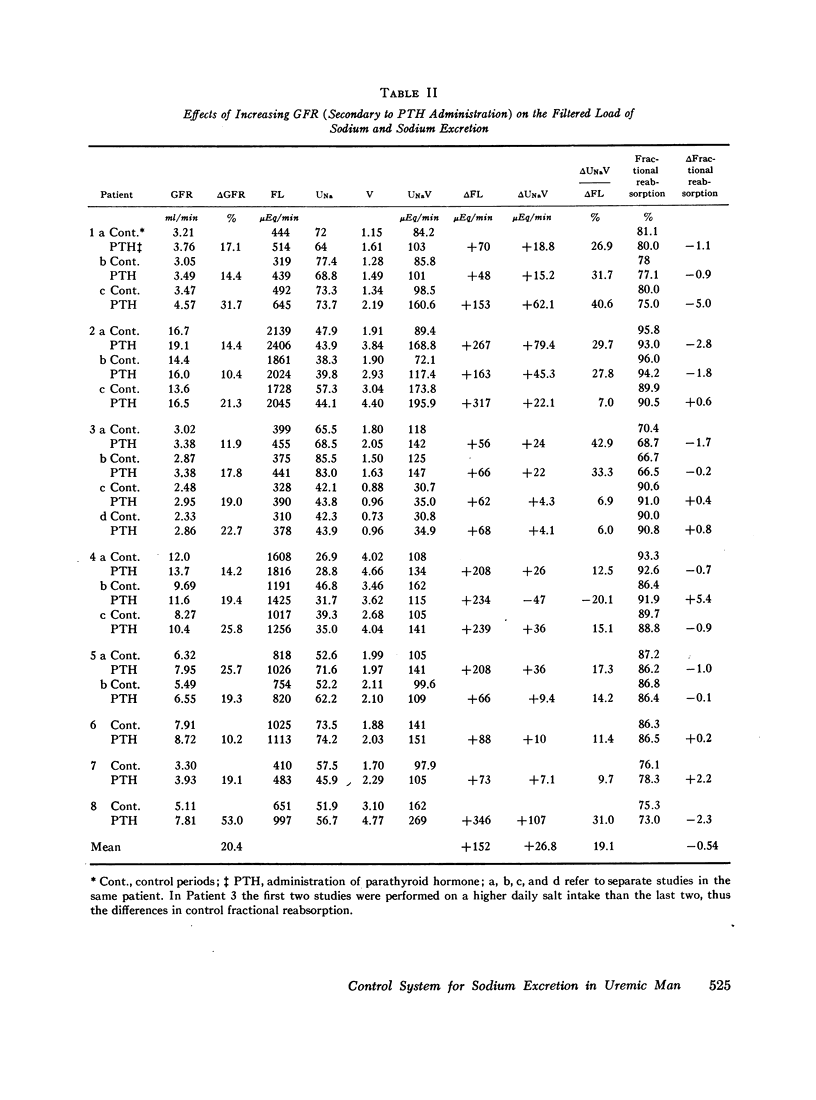
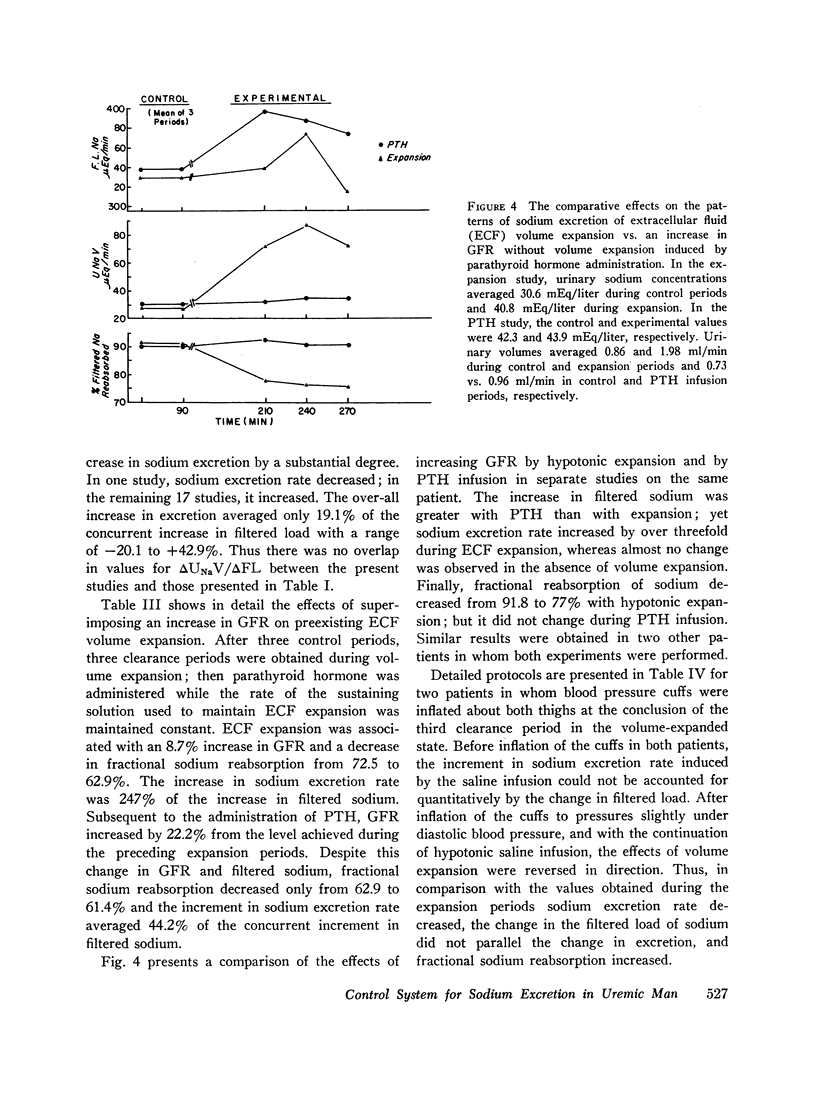
Sodium excretion was studied in a group of patients with chronic renal disease, (a) on constant salt intakes of varying amounts with and without mineralocorticoid hormone administration and, (b) after acute extracellular fluid volume expansion. The lower the steady-state glomerular filtration rate (GFR), the greater was the fraction of filtered sodium excreted on both a 3.5 and 7.0 g salt diet; and the lower the GFR, the greater was the change in fractional excretion in the transition from the 3.5 to the 7.0 g salt diet. This regulatory capacity did not appear to be influenced by mineralocorticoid hormone administration. After acute expansion of extracellular fluid (ECF) volume, the increment in sodium excretion exceeded the concomitant increment in filtered sodium in six of nine studies and in the remaining three studies, the increment in excretion averaged 59% of the Δ filtered load (i.e., only 41% of the increase in filtered sodium was reabsorbed). During saline loading, the decrease in fractional reabsorption of sodium tended to vary inversely with the steady-state GFR, although all patients received approximately the same loading volume. When an edema-forming stimulus was applied during saline infusion, the natriuretic response was aborted and the lag time was relatively short. When GFR and the filtered load of sodium were increased without volume expansion, the Δ sodium excretion averaged only 19% of the Δ filtered load; moreover, changes in fractional sodium reabsorption were considerably smaller than those observed during saline loading. The data implicate the presence of a factor other than GFR and mineralocorticoid changes in the modulation of sodium excretion in uremic man.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- DE WARDENER H. E., MILLS I. H., CLAPHAM W. F., HAYTER C. J. Studies on the efferent mechanism of the sodium diuresis which follows the administration of intravenous saline in the dog. Clin Sci. 1961 Oct;21:249–258. [PubMed] [Google Scholar]
- EARLEY L. E., FRIEDLER R. M. CHANGES IN RENAL BLOOD FLOW AND POSSIBLY THE INTRARENAL DISTRIBUTION OF BLOOD DURING THE NATRIURESIS ACCOMPANYING SALINE LOADING IN THE DOG. J Clin Invest. 1965 Jun;44:929–941. doi: 10.1172/JCI105210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FITZHUGH F. W., Jr, McWHORTER R. L., Jr, ESTES E. H., Jr, WARREN J. V., MERRILL A. J. The effect of application of tourniquets to the legs on cardiac output and renal function in normal human subjects. J Clin Invest. 1953 Nov;32(11):1163–1170. doi: 10.1172/JCI102840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleeman C. R., Okun R., Heller R. J. The renal regulation of sodium and potassium in patients with chronic renal failure (CRF) and the effect of diuretics on the excretion of these ions. Ann N Y Acad Sci. 1966 Nov 22;139(2):520–539. doi: 10.1111/j.1749-6632.1966.tb41226.x. [DOI] [PubMed] [Google Scholar]
- Lindheimer M. D., Lalone R. C., Levinsky N. G. Evidence that an acute increase in glomerular filtration has little effect on sodium excretion in the dog unless extracellular volume is expanded. J Clin Invest. 1967 Feb;46(2):256–265. doi: 10.1172/JCI105528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubowitz H., Slatopolsky E., Shankel S., Rieselbach R. E., Bricker N. S. Glomerular filtration rate. Determination in patients with chronic renal disease. JAMA. 1967 Jan 23;199(4):252–256. doi: 10.1001/jama.199.4.252. [DOI] [PubMed] [Google Scholar]
- Rieselbach R. E., Shankel S. W., Slatopolsky E., Lubowitz H., Bricker N. S. Glucose titration studies in patients with chronic progressive renal disease. J Clin Invest. 1967 Feb;46(2):157–163. doi: 10.1172/JCI105518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultze R. G., Slatopolsky E., Tall B., Walker W., Levy M., Bricker N. S. The regulation of sodium excretion in uremia: a new dimension in the characterization of "third factor". Trans Assoc Am Physicians. 1966;79:322–329. [PubMed] [Google Scholar]



