Abstract
Background
Our objective was to examine the effect of antenatal peer support on rates of breastfeeding initiation.
Methods
We performed a systematic review of randomized controlled trials, quasi-randomized trials and cohort studies with concurrent controls. We searched the Cochrane Library, MEDLINE, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), the National Research Register and the British Nursing Index from inception or from 1980 to 2009. We carried out study selection, data abstraction and quality assessment independently and in duplicate. We defined high-quality studies as those that minimized the risk of at least three of the following types of bias: selection, performance, measurement and attrition bias. We calculated risk ratios (RRs) and 95% confidence intervals (CIs) for individual studies and undertook separate meta-analyses for high-quality trials of universal peer support and targeted peer support. We did not include low-quality studies.
Results
We selected 11 studies, which involved 5445 women in total. Seven of these studies (involving 4416 women in total) evaluated universal peer support, and four studies (involving 1029 women in total) targeted antenatal peer support. In the three high-quality studies of universal peer support, all involving low-income women, the relative risk for not initiating breastfeeding was 0.96 (95% CI 0.76–1.22). In the three high-quality studies of antenatal peer support that targeted women considering breastfeeding, the relative risk for not initiating breastfeeding was 0.64 (95% CI 0.41 – 0.99).
Interpretation
Universal antenatal peer support does not appear to improve rates of breastfeeding initiation, but targeted antenatal peer support may be beneficial. This effect may be related to context, however, so any new peer-support program should undergo concurrent high-quality evaluation.
Breastfeeding confers numerous benefits for mother and infant,1–3 yet many women still do not initiate breastfeeding.4 The World Health Organization recommends exclusive breastfeeding to six months,5 and national governments have implemented initiatives to increase initiation rates.6,7 Peer support has been examined as one intervention to increase breastfeeding rates, but there have been few high-quality randomized controlled trials (RCTs) examining initiation. One systematic review8 (published in 2000) concluded, based only on two nonrandomized studies, that antenatal peer support had a positive effect on breastfeeding initiation. Another9 (published in 2005 and updated in 2007) included only RCTs but excluded those whose primary purpose was to affect duration. Based only on one RCT, that review concluded that peer support is likely to result in improvements in initiation of breastfeeding among low-income women where baseline breastfeeding rates are low. These weaknesses in the available evidence make recommendations uncertain. Despite this uncertainty, antenatal peer support for breastfeeding is being incorporated into routine maternity care in some parts of the world.10
Antenatal peer support can be provided as a universal service or targeted to women who are considering breastfeeding. Although trials have made this distinction, previous reviews have not. New evidence has become available, and it appears appropriate to re-examine antenatal peer support through a systematic review. The purpose of our review was to assess the effectiveness of antenatal peer support, as either a universal or a targeted service, including all studies that examined breastfeeding initiation using concurrent controls.
Methods
A protocol was developed prospectively to conduct the review, using widely recommended methods.11
Literature search
The following bibliographic databases and resources were searched: British Nursing Index (1981–2008), the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (1982–2008), the Cochrane Library, EMBASE (1980–2008), MEDLINE (1950–2008) and Current Controlled Trials. Reference lists of retrieved articles were manually searched. An updated search was carried out in January 2009 in MEDLINE (1950–2009) (Appendix 1, available at www.cmaj.ca/cgi/content/full/cmaj.091729/DC1).
Inclusion criteria
Citations and papers were selected using an inclusion–exclusion form (Appendix 2, available at www.cmaj.ca/cgi/content/full/cmaj.091729/DC1). We included studies in which the participants were pregnant women, peer-support intervention was provided in the antenatal period irrespective of whether it was also provided in the immediate postnatal period, any comparator was used, breastfeeding initiation was reported, and the study design was either an RCT, quasi-randomized or cohort study with concurrent control. Peer support was defined as support offered by women who had themselves breastfed, who were usually from the same socioeconomic background and locality as the women they were supporting and who had received appropriate training. Peer supporters could be either voluntary or in receipt of basic remuneration or money for expenses.10 Universal peer support was described as that offered to all women, and targeted peer support as that offered only to women who were considering breastfeeding. For the purposes of this review, breastfeeding initiation was defined as any attempt to breastfeed, even if only once. Nonrandomized studies were included to explore the full spectrum of evidence, given that many studies on this subject are nonrandomized.
No language restrictions were applied. Potentially relevant citations were identified through a comprehensive electronic search. Inclusion and exclusion criteria were applied to all citations, and hard copies of potentially relevant papers were obtained and assessed for relevance (L.I., K.J.). When there was uncertainty, it was resolved by consulting coauthors (K.S.K. and C.M.).
Data extraction and assessment of study quality
Data were extracted on participants, intervention, type of peer support (universal or targeted), outcome, study type, methods, results and quality (L.I. and K.J.). A tool12,13 was adapted to assess the risk of bias in both experimental and observational studies (Appendix 3, available at www.cmaj.ca/cgi/content/full/cmaj.091729/DC1). The tool classified study quality into high, medium or low for selection, performance, measurement and attrition bias based on descriptions of the study design, execution and analysis. Studies rated as having the same level of quality in two or more of the four categories were considered to be of that quality overall.
Data synthesis
The data were tabulated and studies were categorized according to whether they had involved universal or targeted peer support. Risk ratios (RRs) with 95% confidence intervals (CIs) were used where available or were calculated from the other measures of effect reported. When pooling studies, it is important to choose a summary statistic that is likely to be constant across settings. Although trials typically report the proportions initiating breastfeeding, it is more likely that the relative risk of not initiating breastfeeding would be constant across settings where initiation rates vary (i.e., that an effective intervention would cause a greater number of women to breastfeed in a setting where rates are low than where few women do not breastfeed). Therefore, for the purposes of meta-analysis, we have pooled the RR of failure to initiate breastfeeding and have redefined it as the absolute number of additional women initiating breastfeeding.
Meta-analysis was only considered for studies without a high risk of bias. We derived the RRs of not initiating breast-feeding and 95% CIs. We explored heterogeneity among the included studies both qualitatively, by comparing their characteristics, and quantitatively, using the χ2 test of heterogeneity and the I2 statistic. Where appropriate, we combined results from included studies for each outcome to give an overall estimate of the treatment effect. For cluster trials, we computed the design effect from data presented in the reports (intraclass correlation coefficients and cluster-adjusted estimates) and adapted the standard errors of the relative risk to make appropriate allowance for clustering.14 Where intraclass correlation coefficients were not reported, we computed a design effect using mean intraclass correlation coefficients from the trials in which they were available.
Results
Identification of the literature
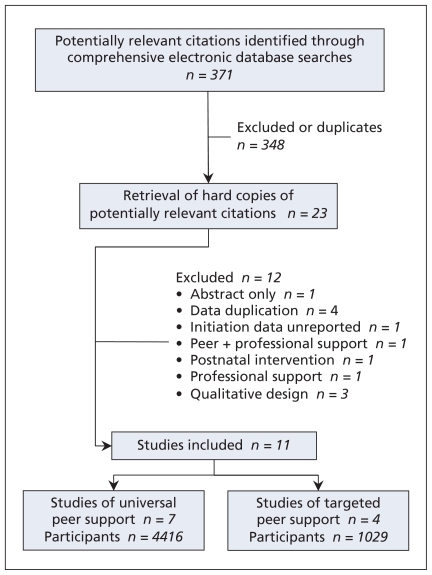
In the primary search, 371 citations were identified, of which 348 were excluded because of irrelevance or duplication. Of 23 studies assessed in full, 12 were excluded, leaving 11 for review (Figure 1). Of these studies, seven15–21 involved an intervention of universal peer support and four22–25 involved targeted peer support (Tables 1 and 2). All control groups received routine maternity care as practised in their respective regions.
Figure 1.
Identification of relevant literature on antenatal peer support to improve rates of breastfeeding initiation.
Table 1.
Characteristics of studies involving universal peer support
| Study | Methods | Participants and setting | Intervention | Outcomes | Results | Quality* |
|---|---|---|---|---|---|---|
| MacArthur et al.16 |
|
|
Routine AN care + 2 AN support sessions with PC (24–38 wk + 32–34 wk) | Primary outcome: BF initiation |
|
|
| Muirhead et al.19 |
|
|
|
BF initiation + duration (up to 6 wk) |
|
|
| Morrow et al.18 |
|
|
|
|
|
|
| Caulfield et al.15 |
|
|
|
BF initiation + continuation to 7–10 days PN |
|
|
| McInnes et al.17 |
|
|
PC (2 AN + 2 PN sessions) | Infant feeding intention, BF initiation + BF duration (to 6 wk) |
|
|
| Shaw et al.21 |
|
|
PC (1 AN session + PN as required) | BF initiation on hospital discharge + BF duration |
|
|
| Schafer et al.20 |
|
|
AN + PN PC | BF initiation + BF duration |
|
|
Note: AN = antenatal, BF = breastfeeding, GP = general practice, PC = peer counsellor or counselling, PN = postnatal, RCT = randomized controlled trial, WIC = Women, Infants and Children programme.
1 = selection bias, 2 = performance bias, 3 = measurement bias, 4 = attrition bias.
Table 2.
Characteristics of studies involving targeted peer support
| Study | Methods | Participants and setting | Intervention | Outcomes | Results | Quality* |
|---|---|---|---|---|---|---|
| Chapman et al.23 |
|
|
AN early intrapartum, PN PC | BF initiation, BF rates at 1, 3 and 6 mo |
|
|
| Graffy et al.24 |
|
|
|
|
|
|
| Anderson et al.22 |
|
|
PC + routine care: 3 AN home visits, daily in-patient visits + 9 PN home visits | Exclusive BF status at hospital discharge, 1, 2 + 3 mo PN |
|
|
| Kistin et al.25 |
|
|
AN PC if possible and PN PC by telephone | BF initiation exclusively and duration |
|
|
Note: AN = antenatal, BF = breastfeeding, NICU = neonatal intensive care unit, PC = peer counsellor or counselling, PN = postnatal, RCT = randomized controlled trial, WIC = Women, Infants and Children programme.
1 = selection bias, 2 = performance bias, 3 = measurement bias, 4 = attrition bias.
Quality of the studies
The quality of the 11 included studies varied. Six16,18,19,22–24 of the seven RCTs were classified as high-quality overall, with three involving targeted and three involving universal peer support. The remaining RCT15,17 was of medium to low quality, and involved universal peer support. The four remaining studies were observational and classified as being of medium to low quality, with one involving targeted and three involving universal peer support.17,20,21,25
Study settings
Six of the 11 studies were undertaken in the United States,15,20,23–25 one in Mexico18 and four in the United Kingdom (two in Scotland17,19 and two in England16,24). The populations in all studies predominantly comprised low-income women.
Intensity of the interventions
All studies included both antenatal and postnatal peer support in their interventions. Differences in the intensity of the interventions are shown in Table 3, which lists the number and venue of intended antenatal support contacts and compliance in terms of actual contacts and population coverage. The two US-based RCTs of targeted peer support22,23 also included daily in-hospital peer support starting within 24 hours after birth, which may have had an additional effect on initiation rates.
Table 3.
Characteristics of interventions in all included studies
| Study | Intervention n (n with initiation data) | Peer supporters, no. | Contact venue or method | Contacts per woman, proposed no. | Contacts per woman, actual no. | Coverage by peers, % |
|---|---|---|---|---|---|---|
| Universal peer support | ||||||
| MacArthur et al.16 | 1140 (1083) | 11 | Clinic or home | 2 | 2 received by 42% | 74 |
| Muirhead et al.19 | 112 (112) | 12 (2 per mother) | “Visited” | At least 1 | “Limited” | NS |
| Morrow et al.18 | 96 (95) | 3 | Home | 1 or 2, depending on intervention group | NS | NS |
| Caulfield et al.15 | Not defined (242) | NS | Home or telephone | 1 (interested women followed up ≥ 3 times) | NS | NS |
| McInnes et al.17 | 474 (449) | 7 | “Visited” | ≥ 2 breastfeeding awareness events in community | 1 | 71 |
| Shaw et al.21 | 156 (156) | 7 | Telephone, clinic, home, hospital | Based on need after questionnaire | 1 | 81 |
| Schafer et al.20 | 143 (72) | 94 | Home, clinic, telephone | NS | NS | 100 |
| Targeted peer support | ||||||
| Chapman et al.23 | 113 (90) | 3 | Home | At least 1 (additional if deemed necessary) | 1 | 53 |
| Graffy et al.24 | 363 (350) | 28 | Home and telephone | 1 | 1 received by 80% | 80 |
| Anderson et al.22 | 90 (63) | 2 | Home | 3 | 3 received by 89% | 89 |
| Kistin et al.25 | 59 (55) | NS | Telephone only | Talk to women “if possible” antenatally | NS | NS |
Note: NS = not stated.
Universal peer support
Randomized controlled trials
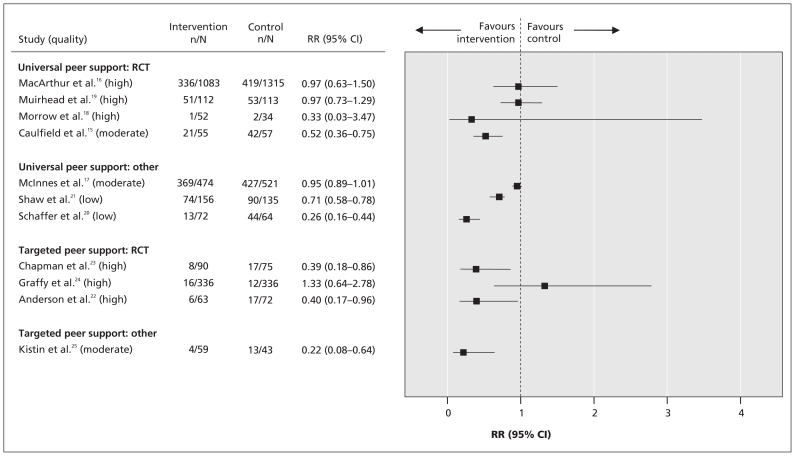
Three cluster RCTs15,16,18 and one individual RCT19 investigated universal peer support. Morrow and colleagues,18 in a cluster RCT in Mexico, reported no significant difference in breastfeeding initiation rates between the control group and two intervention groups. Intervention group one (involving two antenatal peer-counselling visits) had an initiation rate of 100%, and intervention group two (involving one visit) had an initiation rate of 98%, compared with 94% for the control group (with no peer counselling). The cluster RCT in the United Kingdom by MacArthur and colleagues16 also showed no difference in initiation rates between intervention and control groups (intervention 69.0%, control 68.1%; cluster-adjusted RR for noninitiation 0.97, 95% CI 0.63–1.50). A cluster RCT by Caulfield and colleagues15 in the United States reported breastfeeding initiation rates from four clusters (i.e., three intervention clusters relative to control) of 62% with peer-counselling only versus 26% for controls (RR 0.52, 95% CI 0.36–0.75). An individual RCT carried out in Scotland by Muirhead and colleagues19 reported no significant difference in breastfeeding initiation rates (intervention 54.5%, control 53.1%; RR 0.97, 95% CI 0.73–1.29). The pooled analysis showed no significant effect of universal peer support on non-initiation of breastfeeding (RR 0.96, 95% CI 0.76–1.22; χ2 for heterogeneity 0.81, p = 0.67; I2 0.0%) (Appendix 4, available at www.cmaj.ca/cgi/content/full/cmaj.091729/DC1). Only the three high-quality RCTs16,18,19 were pooled, with the fourth15 excluded because of methodologic weaknesses.
Nonrandomized controlled studies
In a quasi-randomized study examining universal peer support in Scotland, McInnes and colleagues17 observed that women in the intervention group were more likely to initiate breastfeeding than those in the control group (23% v. 20%) and that this finding was significant only when adjusted for confounding variables that included socio-economic deprivation. Two nonrandomized studies, both US-based,20,21 showed a difference in breastfeeding initiation rates with universal peer support. Schafer and colleagues20 reported that 82% of women initiated breastfeeding in the intervention group versus 31% in the control group (RR 0.26, 95% CI 0.16–0.44). Shaw and colleagues21 reported that women in the intervention group were significantly more likely to initiate breast-feeding (53%) than those in the control group (33%) (RR 0.71, 95% CI 0.58–0.78).
The results of all of the included studies of universal peer support are shown in Figure 2.
Figure 2.
Forest plot of the effect of antenatal peer support on noninitiation of breastfeeding. Values less than 1.0 favour intervention. CI = confidence interval, RR = risk ratio.
Targeted peer support
Randomized controlled trials
In three RCTs22–24 evaluating targeted peer support (two22,23 in the United States, one24 in the United Kingdom) the study populations included only women who were considering breast-feeding. Both US-based trials reported a significant increase in breastfeeding initiation rates in the intervention groups compared with the control groups (91% v. 77% [RR for noninitiation 0.39, 95% CI 0.18–0.86]23 in one trial and 90% v. 76% [RR for noninitiation 0.40, 95% CI 0.17–0.96] in the other.22 These trials involved predominantly low-income Hispanic women who were considering breastfeeding. In their UK-based RCT, Graffy and colleagues24 reported no difference in initiation rates between intervention (95%) and control (96%) groups. The pooled analysis of these three RCTs22–24 showed a significant reduction in breastfeeding noninitiation with targeted peer support (RR 0.64, 95% CI 0.41–0.99, p = 0.04) (Appendix 4, available at www.cmaj.ca/cgi/content/full/cmaj.091729/DC1). However, there was significant heterogeneity (χ2 for heterogeneity 6.44, p = 0.04, I2 69.0%).
Nonrandomized controlled studies
One small cohort study25 with concurrent control in the United States by Kistin and colleagues reported a significant difference in the rate of breastfeeding initiation with targeted peer support (intervention 93%, control 70%; RR for noninitiation 0.22, 95% CI 0.08–0.64).
The results of all of the studies of targeted peer support are shown in Figure 2.
Interpretation
This systematic review found, from high-quality RCT evidence,16,18,19 that universal antenatal peer support did not reduce rates of breastfeeding noninitiation. Targeted antenatal peer support might have an effect, based on two small RCTs involving Hispanic women in the United States22,23 and one nonrandomized US study.25 In a setting where 75 of 100 women choose to breastfeed, providing targeted peer support would cause an additional 9 to initiate breastfeeding.
Explanation and comparison with other studies
Our findings may have been influenced by the intensity of the interventions, underlying breastfeeding rates and breastfeeding information provided to control groups. The interventions were generally similar, although in one trial,17 community breastfeeding awareness events also took place, and one trial used only telephone peer support.25
All study designs included additional postnatal peer support for breastfeeding women, so it was not possible to determine the sole effect of antenatal peer support on the duration or exclusivity of breastfeeding. The designs of two RCTs included daily peer support while in hospital after birth,22,23 which may have contributed to the significant results reported by both. It is therefore difficult to identify accurately whether antenatal peer support alone can improve initiation or whether a combination of antenatal and very early postnatal support is required.
The studies in the meta-analysis of targeted peer support had significant heterogeneity. This heterogeneity may have resulted from provision in the two US-based trials of in-hospital postnatal peer support, which may have affected initiation rates.22,23 The study by Graffy and colleagues24 was located in the United Kingdom, where baseline rates of breastfeeding initiation are not high. At recruitment, however, all but 2% of women in the intervention group and 4% of those in the control group had already decided to breastfeed; therefore, “considering breast-feeding” may have been interpreted differently in this study. The primary outcome, which was any breastfeeding at six weeks, showed no difference between trial groups. Only the trial by Chapman and colleagues23 stated breastfeeding initiation as a primary outcome; thus, the focus of the interventions in the other two trials22,24 may have been more on exclusivity of breast-feeding.
Unlike the RCTs, all of the nonrandomized trials reported a significant effect. Except for that of the trial by Caulfield and colleagues,15 the interventions used in the nonrandomized studies do not appear to have been more intensive than those in the RCTs. The much lower underlying rate of breastfeeding initiation among participants in the non-RCTs may explain this finding, although this explanation was not true for the trial by Kistin and colleagues.25 The effect is probably better explained by higher levels of selection and attrition biases.
Limitations
This review has some limitations. The quality of the included studies varied. All but one of the RCTs were rated as high-quality overall, but the nonrandomized studies were of lower quality. This difference was taken into account by inclusion of only the high-quality trials in the meta-analyses. Data for the outcome measure of breastfeeding initiation were collected using different methods. The majority of the studies relied on self-reporting by participants (either by completion of a questionnaire17,19–21,24 or by interview15,18,22,23,25). Only one study used hospital data to report rates of initiation.16 The largest trial was in the United Kingdom16 and reported data on 2398 women. By comparison, the other RCTs reported data for between 12718 and 64424 women. The nonrandomized studies included between 20720 and 92617 women, and most were subject to high rates of loss to follow-up.
The intensity of the interventions varied, both in planned and actual contacts between peer supporters and participants, varying from one (in most) to three.22 Coverage ranged from 53%23 to 100%,20 but this was not always reported.15,18,19,25 There was insufficient information given to determine whether a relation existed between intensity of antenatal peer support and initiation of breastfeeding. Routine advice about breastfeeding provided antenatally to controls was generally poorly described, but it appeared to have been mainly clinic-based and written information.
Three RCTs, although not designating breastfeeding initiation as a primary or secondary outcome,18,19,22,24 reported this measure. Exclusion of these results would not have changed the interpretation of findings.
In two RCTs,18,24 control rates of breastfeeding initiation were very high, allowing little scope for improvement from intervention. One of the two trials, which evaluated universal peer support, took place in Mexico,18 where almost all women initiate breastfeeding (hence the higher baseline rate). There, continuation and exclusivity are problems, and these out-comes did improve with intervention. The other trial, which evaluated targeted peer support, was in the United Kingdom,24 where the rate of breastfeeding initiation is under 70%. In the trial population, however, this rate was over 95%; thus, only women who had already nearly decided to breastfeed were recruited. This study’s primary outcome of breastfeeding at six weeks, however, showed no effect.
Conclusion
Universal antenatal peer support appears to be ineffective at increasing rates of breastfeeding initiation when provided in the form of one or two instances of contact between peer supporter and pregnant woman, with strong evidence of this conclusion from the United Kingdom.16,19 There may be a significant increase in rates of initiation of breastfeeding when antenatal peer support is targeted at women who are considering breastfeeding, but evidence of this effect was found only among low-income Hispanic women in the United States. Owing to differences in community rates of breastfeeding and levels of breastfeeding support included in routine care in the included studies, the findings of this review may have limited generalizability. When peer support is introduced as an intervention to improve rates of breastfeeding initiation, there should be concurrent, high-quality evaluation to determine its effectiveness. Future research might focus on more intensive interventions and on the combination of antenatal and immediate postpartum breastfeeding support.
Supplementary Material
Footnotes
Funding: No external funding was received for this study.
Previously published at www.cmaj.ca
Competing interests: Christine MacArthur, Kate Jolly, Lucy Ingram and Khalid Khan are coauthors of one of the studies included in this review.16 No competing interests declared by Jonathan Deeks.
Contributors: Christine MacArthur conceived the study. Lucy Ingram, Kate Jolly and Khalid Khan designed the study protocol, and Lucy Ingram designed and carried out the searches. Lucy Ingram and Kate Jolly screened the initial references for retrieval and extracted the data. Kate Jolly performed the meta-analyses, and Jonathan Deeks provided advice on statistical methodology. Lucy Ingram interpreted the data with input from Kate Jolly, Christine MacArthur and Khalid Khan. Lucy Ingram and Kate Jolly drafted the manuscript, and Khalid Khan, Jonathan Deeks and Christine MacArthur critically reviewed it. All of the authors approved the final version of the manuscript submitted for publication.
This article has been peer reviewed.
REFERENCES
- 1.Horta BL, Bahl R, Martines J, et al. Evidence on the long-term effects of breastfeeding: systematic reviews and meta-analyses. Geneva: World Health Organization; 2007. [(accessed 2010 May 12)]. Available: http://whqlibdoc.who.int/publications/2007/9789241595230_eng.pdf. [Google Scholar]
- 2.Ip S, Chung M, Raman G, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Rockville (MD): Agency for Healthcare Research and Quality; 2007. [(accessed 2010 May 12)]. Evidence report no. 153. Available: www.ahrq.gov/downloads/pub/evidence/pdf/brfout/brfout.pdf. [Google Scholar]
- 3.Kramer MS, Kakuma R. The optimal duration of breastfeeding. A systematic review. Adv Exp Med Biol. 2004;554:63–77. doi: 10.1007/978-1-4757-4242-8_7. [DOI] [PubMed] [Google Scholar]
- 4.Bolling K, Grant C, Hamlyn B, et al. Infant feeding survey 2005. London (UK): The Information Centre; 2007. [(accessed 2010 May 12)]. Available: www.ic.nhs.uk/webfiles/publications/ifs06/2005%20Infant%20Feeding%20Survey%20(final%20version).pdf. [Google Scholar]
- 5.Kramer MS, Kakuma R. The optimal duration of exclusive breastfeeding. Geneva: World Health Organization; 2002. [(accessed 2010 May 12)]. Available: www.who.int/nutrition/topics/optimal_duration_of_exc_bfeeding_review_eng.pdf. [Google Scholar]
- 6.Department of Health. Improvement, expansion and reform — the next three years: priorities and planning framework 2003–2006. London (UK): The Stationary Office; 2002. [(accessed 2010 May 12)]. Available: www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4070202.pdf. [Google Scholar]
- 7.Canadian Pediatric Society, Dietitians of Canada and Health Canada. Nutrition for healthy term infants. Ottawa (ON): Minister of Public Works and Government Services; 2005. [(accessed 2010 May 12)]. Available: www.hc-sc.gc.ca/fn-an/pubs/infant-nourrisson/nut_infant_nourrisson_term-eng.php. [Google Scholar]
- 8.Fairbank L, O’Meara S, Renfrew MJ, et al. A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding. Health Technol Assess. 2000;4:1–171. [PubMed] [Google Scholar]
- 9.Dyson L, McCormick FM, Renfrew MJ. Interventions for promoting the initiation of breastfeeding. Cochrane Database Syst Rev. 2005:CD001688. doi: 10.1002/14651858.CD001688.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Dyson L, Renfrew MJ, McFadden A, et al. Promotion of breastfeeding initiation and duration. Evidence into practice briefing. London (UK): National Institute for Health and Clinical Excellence; 2006. [(accessed 2010 May 12)]. Available: www.breastfeedingmanifesto.org.uk/doc/publication/EAB_Breastfeeding_final_version_1162237588.pdf. [Google Scholar]
- 11.Higgins J, Green S, editors. Cochrane handbook for systematic reviews of interventions, version 5.0.2. The Cochrane Collaboration; 2009. [(accessed 2010 May 12)]. [updated September 2009] Available: www.cochrane-handbook.org. [Google Scholar]
- 12.Kidney E, Winter HR, Khan KS, et al. Systematic review of effect of community-level interventions to reduce maternal mortality. BMC Pregnancy Childbirth. 2009;9:2. doi: 10.1186/1471-2393-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality of both randomised and nonrandomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deeks JJ, Higgins J, Altman DG. Analysing and presenting results. In: Higgins J, Green S, editors. Cochrane handbook for systematic reviews of interventions 4.2.6. Chichester (UK): John Wiley & Sons, Ltd; 2006. [update September 2006] [Google Scholar]
- 15.Caulfield LE, Gross SM, Bentley ME, et al. WIC-based interventions to promote breastfeeding among African-American women in Baltimore: effects on breastfeeding initiation and continuation. J Hum Lact. 1998;14:15–22. doi: 10.1177/089033449801400110. [DOI] [PubMed] [Google Scholar]
- 16.MacArthur C, Jolly K, Ingram L, et al. Antenatal peer support workers and breastfeeding initiation: a cluster randomised controlled trial. BMJ. 2009;338:b131. doi: 10.1136/bmj.b131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McInnes RJ, Love JG, Stone DH. Evaluation of a community-based intervention to increase breastfeeding prevalence. J Public Health Med. 2000;22:138–45. doi: 10.1093/pubmed/22.2.138. [DOI] [PubMed] [Google Scholar]
- 18.Morrow AL, Guerrero ML, Shults J, et al. Efficacy of home-based peer counselling to promote exclusive breastfeeding: a randomised controlled trial. Lancet. 1999;353:1226–31. doi: 10.1016/S0140-6736(98)08037-4. [DOI] [PubMed] [Google Scholar]
- 19.Muirhead PE, Butcher G, Rankin J, et al. The effect of a programme of organised and supervised peer support on the initiation and duration of breastfeeding: a randomised trial. Br J Gen Pract. 2006;56:191–7. [PMC free article] [PubMed] [Google Scholar]
- 20.Schafer E, Vogel MK, Viegas S, et al. Volunteer peer counselors increase breastfeeding duration among rural low-income women. Birth. 1998;25:101–6. doi: 10.1046/j.1523-536x.1998.00101.x. [DOI] [PubMed] [Google Scholar]
- 21.Shaw E, Kaczorowski J, Shaw E, et al. The effect of a peer counseling program on breastfeeding initiation and longevity in a low-income rural population. J Hum Lact. 1999;15:19–25. doi: 10.1177/089033449901500108. [DOI] [PubMed] [Google Scholar]
- 22.Anderson AK, Damio G, Young S, et al. A randomized trial assessing the efficacy of peer counseling on exclusive breastfeeding in a predominantly Latina low-income community. Arch Pediatr Adolesc Med. 2005;159:836–41. doi: 10.1001/archpedi.159.9.836. [DOI] [PubMed] [Google Scholar]
- 23.Chapman DJ, Damio G, Young S, et al. Effectiveness of breastfeeding peer counseling in a low-income, predominantly Latina population: a randomized controlled trial. Arch Pediatr Adolesc Med. 2004;158:897–902. doi: 10.1001/archpedi.158.9.897. [DOI] [PubMed] [Google Scholar]
- 24.Graffy J, Taylor J, Williams A, et al. Randomised controlled trial of support from volunteer counsellors for mothers considering breastfeeding. BMJ. 2004;328:26. doi: 10.1136/bmj.328.7430.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kistin N, Abramson R, Dublin P. Effect of peer counselors on breastfeeding initiation, exclusivity, and duration among low-income urban women. J Hum Lact. 1994;10:11–5. doi: 10.1177/089033449401000121. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.