Abstract
A greater number of older adults now live with coronary heart disease (CHD). This poses a significant public health problem as older adults are at high risk for CHD-related mortality and morbidity. Overwhelming data support benefits of cardiac rehabilitation for secondary prevention, yet only a small portion of eligible older adults receive it. While many studies have examined factors that affect cardiac rehabilitation utilization among older adults, few interventions have aimed to improve their cardiac rehabilitation participation rates. A substantial body of evidence indicates an individual’s illness perceptions appear to play a pivotal role in health behavior and may be a promising target for intervention. Drawing from theoretic and empiric findings of Leventhal and others, a self-regulatory model is proposed that explicates how CHD perceptions of older adults may influence cardiac rehabilitation participation. The model may provide a useful guide for the development of effective interventions tailored to older adults.
Coronary heart disease (CHD) is a chronic disease that greatly impacts older Americans. The prevalence of CHD among adults who were 65 years of age or older between 2002 and 2003 was 21.9% for White, non-Hispanics; 17.4% for Black, non-Hispanics; and 14.3% for Hispanics. 1 The leading cause of mortality for men and women in the United States is CHD. Nearly 82% of those who die from CHD are 65 years of age or older. 2 Increased co-morbidities, greater disability, decreased health-related quality of life, and increased health care expenditures further characterize the CHD burden among older Americans. This burden will likely increase with the anticipated demographic shifts associated with increasing numbers and proportions of older Americans. 1 Thus, secondary prevention of CHD among older adults is identified as a significant area for the development of tailored interventions to decrease disease related burdens.
Cardiac rehabilitation is an effective secondary prevention measure for CHD among older adults.3–5 Benefits of cardiac rehabilitation participation for older adults include a 26–31% reduction in cardiac mortality risk, 6 cardiac risk factor modification, 7–9 improved quality of life and psychosocial well-being, 9,10 improved physical function, 9,11,12 and decreased health care expenditures due to lower rates of CHD related re-hospitalizations 13 for acute myocardial infarction (AMI) and myocardial revascularization procedures. 14,15
Acute myocardial infarction, angioplasty, stent, and coronary artery bypass graft (CABG) surgery are among acute CHD health threats that provide an opportunity for older adults to focus or re-focus their attention on secondary prevention of CHD. However, the participation of older adults in cardiac rehabilitation is low. Only 13% of eligible patients 80 years of age or older, 16 13.9% of AMI patients and 31% of CABG surgery patients who are 65 years of age or older participate in a cardiac rehabilitation program. 6 Older adults are between 1.5 and 2.0 times less likely to enter a cardiac rehabilitation program, as compared to younger adults. 11 Gender differences in cardiac rehabilitation utilization rates17 between men (higher) and women (lower) make participation even more unlikely among older adult women. Poor utilization of cardiac rehabilitation among older adults is concerning because they are at higher risk of CHD-related mortality and morbidity; therefore, cardiac rehabilitation benefits may be of even greater importance in this population. 5,11,18,19
There is a substantial body of research investigating the problem of poor cardiac rehabilitation utilization among adults. Taken together, findings show that an older adult’s decision concerning whether or not to participate in a cardiac rehabilitation program is complex and may be influenced by a variety of factors including age, gender, race and ethnicity, co-morbidities, social support, socioeconomic status, insurance status, depression, anxiety, role responsibilities, transportation issues, issues of provider non-referral, and the strength of the provider’s recommendation for the cardiac rehabilitation program. 6,17,20–22 There are many potential barriers to cardiac rehabilitation utilization; however, if an older adult does not perceive a personal need for cardiac rehabilitation, it is unlikely that he or she will be motivated to confront potential barriers.
Recent studies indicate the way in which older adults’ interpret their acute CHD illness (illness representation)23–26 may be a particularly influential factor, driving participation in cardiac rehabilitation.20,27,28 A perceived need for cardiac rehabilitation is likely influenced by acute CHD illness perceptions that are consistent with an expert model of CHD which emphasizes the chronic nature of the disease, and the need for continued secondary prevention efforts throughout the life-course. The Self-Regulation Model (Leventhal and colleagues)23,24,29–31 provides a framework for furthering a conceptual understanding of how the illness representations of older adults may influence cardiac rehabilitation behavior. The Self-Regulation Model seeks to understand individual patient’s illness perceptions as a key influencing factor for the selection of health behaviors within the patient’s personal, social, and ethno-cultural contexts. The Self-Regulation Model has been used to guide the development of interventions targeting other health behaviors and may provide a useful guide for the development of tailored interventions designed to improve older adult participation in cardiac rehabilitation.
Self-regulation theory
Leventhal and colleagues 23,24,29–31 suggest that individuals are active problem solvers whose health related behaviors are based upon, and then regulated or influenced by, the representations or beliefs they themselves generate about an illness.30 The basic premise of this model is that when confronted by a health problem, individuals are motivated to regulate or minimize their health-related risk and act to decrease health threats in ways consistent with their perceptions of them. Three recurring, self-regulating, stages guide an individual’s response to a health threat: 1) An active processing system generates cognitive representations of the health threat. The dynamic process is influenced by the individual’s personal, social, and ethno-cultural contexts, and thus highly individualized. 24,30,32 2) In response to the representation, a plan of action for coping with the problem is identified and activated. 3) The success of the coping procedure is appraised and forms the basis for subsequent modification. The appraisal feeds back and the self-regulating process may alter either the way the problem was initially represented and/or the selected coping strategy. Subject to appraisal within this process, representations are updated and, therefore, change over time. 30 This suggests there is potential to modify illness representations in a directed way to influence health behavior through an intervention.
Although representation of an illness is highly individualized and varies across disease entity, it is characterized by five distinct, inter-related attributes: 1) disease identity, perceived symptoms and labels for the illness; 2) timeline, perceived course of the illness as acute, chronic, or cyclical in nature; 3) cause, perceived risk factors for the illness; 4) controllability, perceived controllability or cure of the illness through personal or treatment efforts; and 5) consequence, perceived effects of the illness. 23–26
The Self-Regulation Model has been tested and supported across a wide range of patient illness populations, age groups, and ethno-cultural contexts. Diabetes, human immunodeficiency syndrome, chronic obstructive pulmonary disease, hypertension, cancer, rheumatoid arthritis, fibromyalgia, asthma, and chronic pain are some examples of patient illness populations to which the self-regulation model has been applied.25,33–43 Young adults, middle-aged adults, and older adults have participated in research studies that have tested this model. Additionally, the self-regulation model has been applied in African American, Chinese, Japanese, and Latino ethno-cultural contexts.44–47 Self-regulation theory has guided the development of representational interventions which have successfully influenced selected patient health behaviors including but not limited to antiretroviral adherence,35,36 cancer related symptom management,38 and advanced care planning.48 The wide applicability of this model with emphasis on understanding individual patient’s illness perceptions as an influencing factor on subsequent health behaviors lend itself to usefulness in examining the problem of poor cardiac utilization among older adults following acute CHD events and guiding the development of tailored interventions for this at risk population.
Self-regulation theory, older adults, and cardiac rehabilitation
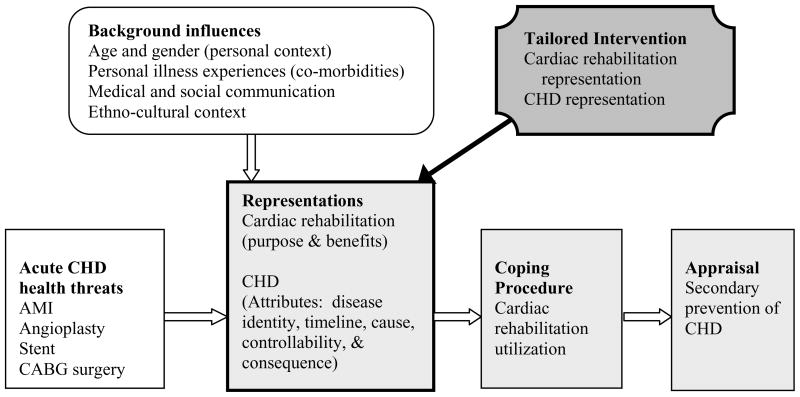
Considered within a self-regulation framework, an older adult’s participation in cardiac rehabilitation will depend upon his or her representation of CHD in relation to perceptions of the purpose and personal benefits of cardiac rehabilitation. 27,49,50 Cardiac rehabilitation utilization can be understood as one of the coping behaviors or procedures that may be selected by the older adult in response to his or her representations of the acute CHD health threat. The success of the coping procedures (cardiac rehabilitation or other coping response) will be appraised and subsequent self-regulating processes adjusted accordingly (see Figure 1).
Figure 1.
Self-regulatory model of cardiac rehabilitation utilization
Patient representations of CHD and cardiac rehabilitation will thus influence whether or not, or the extent to which an older adult will elect to participate in a cardiac rehabilitation program. 27,50 Older CHD patients who understand the role of cardiac rehabilitation and perceive it as being a potentially important or personally necessary coping strategy are more likely to participate. Conversely, older adults will be less likely to participate when they have inaccurate, skeptical, or negative perceptions about CHD and cardiac rehabilitation. 50 For example, the older adult may perceive cardiac rehabilitation as more appropriate for younger patients or have concerns about attendance barriers or the exercise component of the program. A variety of such representations across the five illness representation attributes may curtail older adults’ selection of cardiac rehabilitation as a means to cope with an acute CHD health threat as described below.
Disease identity attribute
The potential for erroneous symptom interpretation during an acute CHD health threat is great among older adults, as symptom interpretation can be a challenging task. Older adults may inaccurately attribute CHD associated symptoms to the discomfort of normal aging, as they are more likely to experience an increased number of symptoms from age-related changes in the biological self, and a milder, atypical CHD symptom presentation. 51–53 Sex-related differences in the clinical presentation of an acute CHD health threat further complicate symptom interpretation for older adult women as women are more likely to experience atypical CHD symptoms in addition to chest pain, as compared to men.54 Chronic disease burdens among older adults also complicate symptom interpretation through increased symptom experience. 52 For example, when an older adult has known chronic disease, such as gastroesophageal reflux disease, the experience of CHD associated “chest pain” may be inaccurately attributed to the older adult’s occasional “heart burn”. Symptom interpretation may also be potentially inaccurate for older adults who have experienced a prior AMI, as they may not have increased knowledge of typical or atypical AMI symptom presentations. 55 Thus, older adults who inaccurately attribute their CHD associated symptoms to normal aging or other chronic disease processes are less likely to participate in cardiac rehabilitation. 28
Timeline attribute
Cardiac rehabilitation programs emphasize the chronic nature of CHD, and the personal need for continued secondary prevention efforts throughout the life-course. 4 A perception of CHD as a chronic illness is consistent with scientific evidence and the mission of cardiac rehabilitation. Older adults, however, are more likely to perceive CHD as an acute illness, as compared to younger adults. 53 The perception of CHD as having an acute rather than chronic timeline among older adults is especially likely among those who are experiencing an initial AMI event or CABG surgery. 56–58 The acute cardiac event is perceived as a short-term problem that will be resolved following recovery from the event, rather than as a symptom of a chronic disease (CHD). 56,57 For example, CABG surgery may be regarded as a mechanism to “fix” the health threat. 59 Healthcare professionals may contribute to the potential for older adults to perceive their CHD as only acute in nature when they select words to describe the patient’s disease and present circumstance that can be misunderstood to mean there is no longer a health concern. Examples of words or phrases that might incorrectly communicate this type of message would include “we’ve fixed your heart,” “solved your problem,” “took care of it,” or “you’re fine now”. While an interventional measure may have addressed an acute cardiac crisis, it is important to emphasize to patients and their families/support person(s) the continued presence of a chronic disease process that requires a commitment to secondary prevention efforts. Failing to emphasize the efficacy of cardiac rehabilitation as a secondary prevention measure for CHD through a strong recommendation of the program to patients or through patient referral to the program may also contribute to an acute perception of CHD among patients. When older adults inaccurately perceive CHD solely as acute, their attention is focused on immediate recovery from the acute CHD health threat. The need for cardiac rehabilitation may be dismissed or minimized, as the CHD problem is perceived to be eradicated with interventional or surgical treatment.
Cause attribute
Patients may not have awareness or knowledge of the cause of a cardiac event or recognize the underlying, progressive nature of the CHD process. 46,49,60–62 When an acute CHD event is perceived by an older adult as an isolated episode, instead of a progressive, chronic disease, the older adult may search for a “trigger” or single cause (e.g. aging) and not consider the cumulative effect of multiple cardiac risk factors on the development of CHD over the life-course. 49,63
Patient causal attributions are often inconsistent with documented personal cardiac risk factors. 46,49,61,62,64 Hypertension, hyperlipidemia, and smoking are risk factors for CHD that are often unrecognized as modifiable causes of an acute CHD event by older adults with these documented risks. 61,62 Older adults are more prone to identify aging and less apt to identify lifestyle behaviors (e.g., stress or inactivity) as factors contributing to their acute CHD health threat. 53 These factors may contribute to the potential for older adult CHD patients to have causal attributions for CHD that are inconsistent with a perceived need for cardiac rehabilitation utilization. Without an accurate and complete personal cardiac risk factor profile, cardiac rehabilitation utilization may be perceived as unnecessary.
Controllability attribute
The controllability attribute of the CHD representation indicates whether or not patients believe their CHD can be controlled or cured. This attribute includes perceptions of personal and treatment controllability. Patients who have a strong perception of personal controllability believe their individual efforts at managing CHD will help to control the progression of the disease. Patients who have a strong perception of treatment controllability believe that the treatments prescribed by their health care provider (s) will have a positive impact on the progression of the disease. For example, a CHD patient with strong personal and treatment controllability may believe that adhering to an aerobic exercise program (personal controllability), following a cardiac diet (personal controllability), and taking prescribed medications (treatment controllability) to control high blood pressure will control the progression of CHD.
Research has demonstrated that older adults are more likely to perceive CHD as less controllable, as compared to younger adults. 53,58,65 Patients with CHD who perceive less personal and treatment controllability are less likely to participate in cardiac rehabilitation. 20,28,66,67 The perceived controllability of CHD may be influenced by the patient’s causal attribution. 68 If the causal attribute is medically inaccurate, this may promote further inaccuracy within the controllability attribute and create a personal circumstance where a perceived need for cardiac rehabilitation is unlikely. For instance, if a patient believes his/her CHD resulted from the aging process, despite having uncontrolled high blood pressure and current smoking behavior, the patient may perceive CHD as not controllable, even though addressing these two modifiable cardiac risk factors through secondary prevention efforts would likely have significant impact on the progression of the disease. Thus, inaccuracy in one’s causal attributions have the potential to promote inaccuracy in one’s perception of whether or not anything can be done to help control CHD progression.
Consequence attribute
Finally, older adults with CHD who perceive less disease severity and fewer severe consequences are less likely to attend cardiac rehabilitation. 20,67 Older adults with lower perceived severity of their CHD during hospitalization for an AMI or CABG surgery have been found to be less likely to attend cardiac rehabilitation. 22 Patients who minimize CHD-related consequences are more likely to only make moderate changes in daily activities and lifestyle after the acute CHD event. 57 While a perception of less disease severity and fewer severe consequences may assist CHD patients in coping with the emotional threat of a CHD event, it may also result in the lack of cardiac rehabilitation participation and secondary prevention efforts.
Summary, discussion, and implications for intervention
Interventions that effectively promote cardiac rehabilitation utilization and prevent cardiac disease related disability among the growing population of older adults are critically needed. While at high risk for CHD-related morbidity and mortality, few older adults participate in cardiac rehabilitation programs despite the well established benefits. Available evidence demonstrates an individual’s representation of CHD and cardiac rehabilitation plays a pivotal role in rehabilitation attendance and may be a promising target for interventions tailored to older adults.
When older adults experience acute CHD health threats, there is a great potential for the construction of CHD representations that will limit participation in cardiac rehabilitation. An older adult may, for example, attribute CHD associated symptoms to normal aging or other known chronic disease(s) (disease identity), instead of recognizing them as part of the progression of CHD. The experience of angioplasty, stent placement, or CABG surgery may be perceived as a treatment that “fixed” the CHD (timeline) so that it is no longer a concern. When the benefits of an outpatient cardiac rehabilitation program are presented, the older adult may not perceive it as being personally necessary. Because CHD is perceived as an isolated event that has been “fixed”, the older adult may not identify personal modifiable cardiac risk factors (causal attribution). The older adult perceives the CHD problem as having been resolved, and therefore, cardiac rehabilitation seems unnecessary, as there is no perceived chronic disease to manage (controllability). The potential negative consequences of CHD have been avoided, because the treatment was successful. The CHD was caught in time (consequences).
Research is needed to determine whether such inaccuracies, skeptical or negative representations of CHD can be positively modified to improve this at risk population’s participation in cardiac rehabilitation programs. The prior example illustrated potential misperceptions as targets for tailored intervention within the five representational attributes: 1) disease identity: erroneous symptom interpretation; 2) timeline: only acute in nature; 3) cause: inaccurate and incomplete CHD attributions; 4) controllability: perceptions of less disease controllability; and 5) consequences: perceptions of less disease severity and fewer consequences of CHD. Self-regulation provides a useful framework for understanding how several key representational attributes interact to influence cardiac rehabilitation utilization and may be a useful guide for the development of tailored interventions to promote cardiac rehabilitation participation among older adults.
Considered within a self-regulation model, a cardiac rehabilitation utilization intervention would be tailored according to the older adult’s representations of CHD and cardiac rehabilitation and reinforce secondary prevention efforts. The desired outcome of such an intervention is to increase participation in cardiac rehabilitation. The initial, essential, step in the intervention process is the assessment of the older adult’s representations of CHD and cardiac rehabilitation. The Revised Illness Perception Questionnaire69 and the Brief Illness Perception Questionnaire70 are two reliable and valid instruments that provide a feasible method for assessing an older adult’s CHD representation in the clinical setting. An assessment of the older adult’s CHD representation would elicit beliefs specific to the five attributes previously discussed (disease identity, timeline, cause, controllability, and consequence) while an assessment of the cardiac rehabilitation representation would elicit beliefs about the perceived purpose and personal benefits of cardiac rehabilitation, including information related to program content, the purpose of aerobic exercise, and explicit barriers to attendance,49 which may be different according to gender. The older adult’s representations provide the frame in which the cardiac rehabilitation utilization intervention content is tailored to the individual. While the cardiac rehabilitation utilization intervention may be designed to address multiple content areas related to CHD and cardiac rehabilitation programs, only the content that applies to the individual’s CHD and cardiac rehabilitation representations would be presented as intervention content. Further, the intervention content is delivered in a bi-directional manner. Representational beliefs that are consistent with cardiac rehabilitation utilization and secondary prevention efforts would be reinforced. Well-established CHD or cardiac rehabilitation representational beliefs that are inconsistent with cardiac rehabilitation utilization and secondary prevention efforts would be challenged with alternative, new information. An opportunity to clarify any logistical concerns about the cardiac rehabilitation program would be provided. This may include a discussion of barriers to access a cardiac rehabilitation program such as: deprivation,71 distance from home,72 lower income or less education, 73 rural living, 74 and transportation.75 The primary purpose of the intervention would be to encourage the older adult to adopt CHD and cardiac rehabilitation representational beliefs that are consistent with cardiac rehabilitation utilization and secondary prevention of CHD to promote cardiac rehabilitation participation.
Research is needed to determine the most advantageous time and mechanisms for delivery of a representational cardiac rehabilitation utilization intervention. Donovan and colleagues’76,77 have conceptualized and tested a representational approach to patient education which seems to be efficacious across a variety of patient populations. Key elements and goals of this representational approach to patient education include the following: 1) representational assessment; 2) identifying and exploring gaps, errors, and confusion; 3) creating conditions for conceptual change; 4) introducing replacement information; 5) summary; 6) goal setting and planning; and 7) follow-up contact to review goals and strategies.77 This approach could be used to design a clinically feasible, tailored cardiac rehabilitation and CHD representational intervention that could be delivered during hospitalization for an acute CHD event, or post-discharge, prior to post-interventional or surgical clearance for cardiac rehabilitation participation. The intervention could be delivered in a single session or in multiple sessions. The delivery modality could be in person, via telephone, or through the internet. It has been suggested that follow-up telephone contact with CHD patients after discharge to encourage cardiac rehabilitation utilization, answer patient questions, and clarify any misconceptions regarding the purpose and benefits of cardiac rehabilitation programs may be beneficial in promoting cardiac rehabilitation enrollment.78 The intervention could also be designed to include the older adult’s significant other or the key individual who will be assisting the older adult during recovery. The tailored intervention may also present alternative options for cardiac rehabilitation program delivery (e.g., educational modules,79 home-based programs,80 use of the internet,81 or telemedicine82 to further encourage older adult participation.
Improving cardiac rehabilitation participation rates among older adults is an important health care initiative. Theoretical and empiric work based upon self-regulation theory have identified the importance of an older adult’s illness representation on his or her cardiac rehabilitation utilization following an acute CHD event. Research is needed to determine the most advantageous mechanisms for delivery of representational interventions to promote cardiac rehabilitation participation among a population at high risk for CHD-related mortality and morbidity. The proposed self-regulatory model of cardiac rehabilitation utilization may serve as a useful guide for the development of effective interventions, tailored to older adult CHD patients.
Acknowledgments
Fellowship support was provided for Carrie Keib by the U.S. National Institutes of Health, NINR 5 F31 NR008971
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Carrie N. Keib, Cedarville University, Department of Nursing, Cedarville, OH 45314.
Nancy R. Reynolds, Yale University, School of Nursing, New Haven, CT 06536.
Karen L. Ahijevych, The Ohio State University, College of Nursing, Columbus, OH 43210.
References
- 1.Centers for Disease Control and Prevention, The Merck Company Foundation. The State of Aging and Health in America 2007. 2007 [Google Scholar]
- 2.American Heart Association. Heart Disease and Stroke Statistics-2009 Update. 2009 [Google Scholar]
- 3.Wenger NK, Froelicher ES, Smith LK, et al. Cardiac rehabilitation as secondary prevention. Agency for Health Care Policy and Research and National Heart, Lung, and Blood Institute. Clin Pract Guidel Quick Ref Guide Clin. 1995;17(17):1–23. [PubMed] [Google Scholar]
- 4.American Association of Cardiovascular & Pulmonary Rehabilitation. Guidelines for cardiac rehabilitation and secondary prevention programs. 4. Champaign, IL: Human Kinetics; 2004. p. 280. [Google Scholar]
- 5.Williams MA, Fleg JL, Ades PA, et al. Secondary prevention of coronary heart disease in the elderly (with emphasis on patients > or =75 years of age): an American Heart Association scientific statement from the Council on Clinical Cardiology Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention. Circulation. 2002;105(14):1735–1743. doi: 10.1161/01.cir.0000013074.73995.6c. [DOI] [PubMed] [Google Scholar]
- 6.Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116(15):1653–1662. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- 7.Leon AS, Franklin BA, Costa F, et al. Cardiac rehabilitation and secondary prevention of coronary heart disease: an American Heart Association scientific statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2005;111(3):369–376. doi: 10.1161/01.CIR.0000151788.08740.5C. [DOI] [PubMed] [Google Scholar]
- 8.Ades PA. Cardiac rehabilitation and secondary prevention of coronary heart disease. N Engl J Med. 2001;345(12):892–902. doi: 10.1056/NEJMra001529. [DOI] [PubMed] [Google Scholar]
- 9.Pasquali SK, Alexander KP, Peterson ED. Cardiac rehabilitation in the elderly. Am Heart J. 2001;142(5):748–755. doi: 10.1067/mhj.2001.119134. [DOI] [PubMed] [Google Scholar]
- 10.Milani RV, Lavie CJ. Prevalence and effects of cardiac rehabilitation on depression in the elderly with coronary heart disease. Am J Cardiol. 1998;81(10):1233–1236. doi: 10.1016/s0002-9149(98)00121-0. [DOI] [PubMed] [Google Scholar]
- 11.Lavie CJ, Milani RV, Littman AB. Benefits of cardiac rehabilitation and exercise training in secondary coronary prevention in the elderly. J Am Coll Cardiol. 1993;22(3):678–683. doi: 10.1016/0735-1097(93)90176-2. [DOI] [PubMed] [Google Scholar]
- 12.Dolansky MA, Moore SM. Effects of cardiac rehabilitation on the recovery outcomes of older adults after coronary artery bypass surgery. J Cardiopulm Rehabil. 2004;24(4):236–244. doi: 10.1097/00008483-200407000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Ades PA, Huang D, Weaver SO. Cardiac rehabilitation participation predicts lower rehospitalization costs. Am Heart J. 1992;123(4 Pt 1):916–921. doi: 10.1016/0002-8703(92)90696-s. [DOI] [PubMed] [Google Scholar]
- 14.Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116(10):682–692. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 15.Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005;143(9):659–672. doi: 10.7326/0003-4819-143-9-200511010-00010. [DOI] [PubMed] [Google Scholar]
- 16.Evenson KR, Rosamond WD, Luepker RV. Predictors of outpatient cardiac rehabilitation utilization: the Minnesota Heart Surgery Registry. J Cardiopulm Rehabil. 1998;18(3):192–198. doi: 10.1097/00008483-199805000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Caulin-Glaser T, Blum M, Schmeizl R, Prigerson HG, Zaret B, Mazure CM. Gender differences in referral to cardiac rehabilitation programs after revascularization. J Cardiopulm Rehabil. 2001;21(1):24–30. doi: 10.1097/00008483-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Wenger NK. Rehabilitation of the coronary artery disease patient: capturing patients. Am J Cardiol. 1997;80(8B):66H–68H. doi: 10.1016/s0002-9149(97)00824-2. [DOI] [PubMed] [Google Scholar]
- 19.Wenger NK. Current status of cardiac rehabilitation. J Am Coll Cardiol. 2008;51(17):1619–1631. doi: 10.1016/j.jacc.2008.01.030. [DOI] [PubMed] [Google Scholar]
- 20.Cooper AF, Jackson G, Weinman J, Horne R. Factors associated with cardiac rehabilitation attendance: a systematic review of the literature. Clin Rehabil. 2002;16(5):541–552. doi: 10.1191/0269215502cr524oa. [DOI] [PubMed] [Google Scholar]
- 21.Evenson KR, Fleury J. Barriers to outpatient cardiac rehabilitation participation and adherence. J Cardiopulm Rehabil. 2000;20(4):241–246. doi: 10.1097/00008483-200007000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Ades PA, Waldmann ML, McCann WJ, Weaver SO. Predictors of cardiac rehabilitation participation in older coronary patients. Arch Intern Med. 1992;152(5):1033–1035. [PubMed] [Google Scholar]
- 23.Leventhal H, Benyamini Y, Brownlee S, et al. Illness Representations: Theoretical Foundations. In: Petrie KJ, Weinman JA, editors. Perceptions of Health and Illness: Current Research and Applications. Amsterdam: Harwood Academic Publishers; 1997. pp. 19–45. [Google Scholar]
- 24.Diefenbach MA, Leventhal H. The Common-Sense Model of Illness Representation: Theoretical and Practical Considerations. Journal of Social Distress and the Homeless. 1996;5(1):11–38. [Google Scholar]
- 25.Meyer D, Leventhal H, Gutmann M. Common-sense models of illness: the example of hypertension. Health Psychol. 1985;4(2):115–135. doi: 10.1037//0278-6133.4.2.115. [DOI] [PubMed] [Google Scholar]
- 26.Lau RR, Hartman KA. Common Sense Representations of Common Illnesses. Health Psychology. 1983;2(2):167–185. doi: 10.1037//0278-6133.8.2.195. [DOI] [PubMed] [Google Scholar]
- 27.French DP, Cooper A, Weinman J. Illness perceptions predict attendance at cardiac rehabilitation following acute myocardial infarction: a systematic review with meta-analysis. J Psychosom Res. 2006;61(6):757–767. doi: 10.1016/j.jpsychores.2006.07.029. [DOI] [PubMed] [Google Scholar]
- 28.Whitmarsh A, Koutantji M, Sidell K. Illness perceptions, mood and coping in predicting attendance at cardiac rehabilitation. Br J Health Psychol. 2003;8(Pt 2):209–221. doi: 10.1348/135910703321649178. [DOI] [PubMed] [Google Scholar]
- 29.Leventhal H, Meyer D, Nerenz DJ. The Common-Sense Representations of Illness Danger. In: Rachman S, editor. Contributions to Medical Psychology and Health. New York: Pergamon; 1980. pp. 7–30. [Google Scholar]
- 30.Leventhal H, Nerenz DR, Steele DJ. Illness Representation and Coping With Health Threats. IV. Hillsdale, New Jersey: Lawrence Erlbaum Associates, Inc; 1984. pp. 219–252. [Google Scholar]
- 31.Cameron LD, Leventhal H. The self-regulation of health and illness behaviour. New York: Routledge; 2003. [Google Scholar]
- 32.Leventhal H, Diefenbach M, Leventhal EA. Illness Cognition: Using Common Sense to Understand Treatment Adherence and Affect Cognition Interactions. Cognitive Therapy and Research. 1992;16:143–163. [Google Scholar]
- 33.Lawson VL, Bundy C, Lyne PA, Harvey JN. Using the IPQ and PMDI to predict regular diabetes care-seeking among patients with Type 1 diabetes. Br J Health Psychol. 2004;9(Pt 2):241–252. doi: 10.1348/135910704773891078. [DOI] [PubMed] [Google Scholar]
- 34.Paschalides C, Wearden AJ, Dunkerley R, Bundy C, Davies R, Dickens CM. The associations of anxiety, depression and personal illness representations with glycaemic control and health-related quality of life in patients with type 2 diabetes mellitus. J Psychosom Res. 2004;57(6):557–564. doi: 10.1016/j.jpsychores.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 35.Reynolds NR. The problem of antiretroviral adherence: a self-regulatory model for intervention. AIDS Care. 2003;15(1):117–124. doi: 10.1080/0954012021000039815. [DOI] [PubMed] [Google Scholar]
- 36.Reynolds NR, Testa MA, Su M, et al. Telephone support to improve antiretroviral medication adherence: a multisite, randomized controlled trial. J Acquir Immune Defic Syndr. 2008;47(1):62–68. doi: 10.1097/QAI.0b013e3181582d54. [DOI] [PubMed] [Google Scholar]
- 37.Ross S, Walker A, MacLeod MJ. Patient compliance in hypertension: role of illness perceptions and treatment beliefs. J Hum Hypertens. 2004;18(9):607–613. doi: 10.1038/sj.jhh.1001721. [DOI] [PubMed] [Google Scholar]
- 38.Ward S, Donovan H, Gunnarsdottir S, Serlin RC, Shapiro GR, Hughes S. A randomized trial of a representational intervention to decrease cancer pain (RIDcancerPain) Health Psychol. 2008;27(1):59–67. doi: 10.1037/0278-6133.27.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaptein AA, Scharloo M, Fischer MJ, et al. Illness perceptions and COPD: an emerging field for COPD patient management. J Asthma. 2008;45(8):625–629. doi: 10.1080/02770900802127048. [DOI] [PubMed] [Google Scholar]
- 40.Graves H, Scott DL, Lempp H, Weinman J. Illness beliefs predict disability in rheumatoid arthritis. J Psychosom Res. 2009;67(5):417–423. doi: 10.1016/j.jpsychores.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 41.van Ittersum MW, van Wilgen CP, Hilberdink WK, Groothoff JW, van der Schans CP. Illness perceptions in patients with fibromyalgia. Patient Educ Couns. 2009;74(1):53–60. doi: 10.1016/j.pec.2008.07.041. [DOI] [PubMed] [Google Scholar]
- 42.Kaptein AA, Hughes BM, Scharloo M, et al. Illness perceptions about asthma are determinants of outcome. J Asthma. 2008;45(6):459–464. doi: 10.1080/02770900802040043. [DOI] [PubMed] [Google Scholar]
- 43.Foster NE, Bishop A, Thomas E, et al. Illness perceptions of low back pain patients in primary care: what are they, do they change and are they associated with outcome? Pain. 2008;136(1–2):177–187. doi: 10.1016/j.pain.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 44.Webb MS, Gonzalez LO. The burden of hypertension: mental representations of African American women. Issues Ment Health Nurs. 2006;27(3):249–271. doi: 10.1080/01612840500502742. [DOI] [PubMed] [Google Scholar]
- 45.Jayne RL, Rankin SH. Application of Leventhal’s self-regulation model to Chinese immigrants with type 2 diabetes. J Nurs Scholarsh. 2001;33(1):53–59. doi: 10.1111/j.1547-5069.2001.00053.x. [DOI] [PubMed] [Google Scholar]
- 46.Fukuoka Y, Dracup K, Kobayashi F, Ohno M, Froelicher ES, Hirayama H. Illness attribution among Japanese patients with acute myocardial infarction. Heart Lung. 2004;33(3):146–153. doi: 10.1016/j.hrtlng.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 47.Cabassa LJ, Lagomasino IT, Dwight-Johnson M, Hansen MC, Xie B. Measuring Latinos’ perceptions of depression: a confirmatory factor analysis of the Illness Perception Questionnaire. Cultur Divers Ethnic Minor Psychol. 2008;14(4):377–384. doi: 10.1037/a0012820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Song MK, Ward SE, Happ MB, et al. Randomized controlled trial of SPIRIT: an effective approach to preparing African-American dialysis patients and families for end of life. Res Nurs Health. 2009;32(3):260–273. doi: 10.1002/nur.20320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cooper AF, Jackson G, Weinman J, Horne R. A qualitative study investigating patients’ beliefs about cardiac rehabilitation. Clin Rehabil. 2005;19(1):87–96. doi: 10.1191/0269215505cr818oa. [DOI] [PubMed] [Google Scholar]
- 50.Cooper AF, Weinman J, Hankins M, Jackson G, Horne R. Assessing patients’ beliefs about cardiac rehabilitation as a basis for predicting attendance after acute myocardial infarction. Heart. 2007;93(1):53–58. doi: 10.1136/hrt.2005.081299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Prohaska TR, Keller ML, Leventhal EA, Leventhal H. Impact of symptoms and aging attribution on emotions and coping. Health Psychol. 1987;6(6):495–514. doi: 10.1037//0278-6133.6.6.495. [DOI] [PubMed] [Google Scholar]
- 52.Leventhal EA, Crouch M. Are There Differences in Perceptions of Illness Across the Lifespan? In: Petrie KJ, Weinman JA, editors. Perceptions of Health and Illness: Current Research and Applications. Amsterdam: Harwood Academic Publishers; 1997. pp. 77–102. [Google Scholar]
- 53.Aalto AM, Heijmans M, Weinman J, Aro AR. Illness perceptions in coronary heart disease. Sociodemographic, illness-related, and psychosocial correlates. J Psychosom Res. 2005;58(5):393–402. doi: 10.1016/j.jpsychores.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 54.Dey S, Flather MD, Devlin G, et al. Sex-related differences in the presentation, treatment and outcomes among patients with acute coronary syndromes: the Global Registry of Acute Coronary Events. Heart. 2009;95(1):20–26. doi: 10.1136/hrt.2007.138537. [DOI] [PubMed] [Google Scholar]
- 55.Tullmann DF, Dracup K. Knowledge of heart attack symptoms in older men and women at risk for acute myocardial infarction. J Cardiopulm Rehabil. 2005;25(1):33–39. doi: 10.1097/00008483-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 56.Lau-Walker M. Relationship between illness representation and self-efficacy. J Adv Nurs. 2004;48(3):216–225. doi: 10.1111/j.1365-2648.2004.03190.x. [DOI] [PubMed] [Google Scholar]
- 57.Brink E, Karlson BW, Hallberg LR. Readjustment 5 months after a first-time myocardial infarction: reorienting the active self. J Adv Nurs. 2006;53(4):403–411. doi: 10.1111/j.1365-2648.2006.03737.x. [DOI] [PubMed] [Google Scholar]
- 58.Gump BB, Matthews KA, Scheier MF, Schulz R, Bridges MW, Magovern GJS. Illness representations according to age and effects on health behaviors following coronary artery bypass graft surgery. J Am Geriatr Soc. 2001;49(3):284–289. doi: 10.1046/j.1532-5415.2001.4930284.x. [DOI] [PubMed] [Google Scholar]
- 59.Keller C. Seeking normalcy: the experience of coronary artery bypass surgery. Res Nurs Health. 1991;14(3):173–178. doi: 10.1002/nur.4770140303. [DOI] [PubMed] [Google Scholar]
- 60.Martin R, Johnsen EL, Bunde J, et al. Gender differences in patients’ attributions for myocardial infarction: implications for adaptive health behaviors. Int J Behav Med. 2005;12(1):39–45. doi: 10.1207/s15327558ijbm1201_6. [DOI] [PubMed] [Google Scholar]
- 61.Murphy B, Worcester M, Higgins R, Le Grande M, Larritt P, Goble A. Causal attributions for coronary heart disease among female cardiac patients. J Cardiopulm Rehabil. 2005;25(3):135–43. doi: 10.1097/00008483-200505000-00002. quiz 144–5. [DOI] [PubMed] [Google Scholar]
- 62.Zerwic JJ, King KB, Wlasowicz GS. Perceptions of patients with cardiovascular disease about the causes of coronary artery disease. Heart Lung. 1997;26(2):92–98. doi: 10.1016/s0147-9563(97)90068-6. [DOI] [PubMed] [Google Scholar]
- 63.French D, Maissi E, Marteau TM. The purpose of attributing cause: beliefs about the causes of myocardial infarction. Soc Sci Med. 2005;60(7):1411–1421. doi: 10.1016/j.socscimed.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 64.Cameron LD, Petrie KJ, Ellis C, Buick D, Weinman JA. Symptom experiences, symptom attributions, and causal attributions in patients following first-time myocardial infarction. Int J Behav Med. 2005;12(1):30–38. doi: 10.1207/s15327558ijbm1201_5. [DOI] [PubMed] [Google Scholar]
- 65.Grace SL, Krepostman S, Brooks D, et al. Illness perceptions among cardiac patients: relation to depressive symptomatology and sex. J Psychosom Res. 2005;59(3):153–160. doi: 10.1016/j.jpsychores.2005.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cooper A, Lloyd G, Weinman J, Jackson G. Why patients do not attend cardiac rehabilitation: role of intentions and illness beliefs. Heart. 1999;82(2):234–236. doi: 10.1136/hrt.82.2.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mitoff PR, Wesolowski M, Abramson BL, Grace SL. Patient-provider communication regarding referral to cardiac rehabilitation. Rehabil Nurs. 2005;30(4):140–146. doi: 10.1002/j.2048-7940.2005.tb00097.x. [DOI] [PubMed] [Google Scholar]
- 68.Petrie KJ, Weinman JA. Illness Representations and Recovery from Myocardial Infarction. In: Petrie KJ, Weinman JA, editors. Perception of Illness and Health. Amsterdam: Harwood Academic Publishers; 1997. pp. 441–461. [Google Scholar]
- 69.Moss-Morris R, Weinman J, Petrie KJ, Horne R, Cameron LD, Buick D. The Revised Illness Perception Questionnaire (IPQ-R) Psychology and Health. 2002;17(1):1–16. [Google Scholar]
- 70.Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60(6):631–637. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 71.Doolan-Noble F, Broad J, Riddell T, North D. Cardiac rehabilitation services in New Zealand: access and utilisation. N Z Med J. 2004;117(1197):U955. [PubMed] [Google Scholar]
- 72.Grace SL, Evindar A, Kung T, Scholey P, Stewart DE. Increasing access to cardiac rehabilitation: automatic referral to the program nearest home. J Cardiopulm Rehabil. 2004;24(3):171–174. doi: 10.1097/00008483-200405000-00006. [DOI] [PubMed] [Google Scholar]
- 73.Tod AM, Lacey EA, McNeill F. ‘I’m still waiting…’: barriers to accessing cardiac rehabilitation services. J Adv Nurs. 2002;40(4):421–431. doi: 10.1046/j.1365-2648.2002.02390.x. [DOI] [PubMed] [Google Scholar]
- 74.King KM, Humen DP, Smith HL, Phan CL, Teo KK. Predicting and explaining cardiac rehabilitation attendance. Can J Cardiol. 2001;17(3):291–296. [PubMed] [Google Scholar]
- 75.Jones LW, Farrell JM, Jamieson J, Dorsch KD. Factors influencing enrollment in a cardiac rehabilitation exercise program. Can J Cardiovasc Nurs. 2003;13(1):11–15. [PubMed] [Google Scholar]
- 76.Donovan HS, Ward S. A representational approach to patient education. J Nurs Scholarsh. 2001;33(3):211–216. doi: 10.1111/j.1547-5069.2001.00211.x. [DOI] [PubMed] [Google Scholar]
- 77.Donovan HS, Ward SE, Song MK, Heidrich SM, Gunnarsdottir S, Phillips CM. An update on the representational approach to patient education. J Nurs Scholarsh. 2007;39(3):259–265. doi: 10.1111/j.1547-5069.2007.00178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Heid HG, Schmelzer M. Influences on women’s participation in cardiac rehabilitation. Rehabil Nurs. 2004;29(4):116–121. doi: 10.1002/j.2048-7940.2004.tb00327.x. [DOI] [PubMed] [Google Scholar]
- 79.Redfern J, Ellis E, Briffa T, Freedman SB. Modular prevention of heart disease following acute coronary syndrome (ACS) BMC Cardiovasc Disord. 2006;6:26. doi: 10.1186/1471-2261-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jolly K, Taylor RS, Lip GY, Stevens A. Home-based cardiac rehabilitation compared with centre-based rehabilitation and usual care: a systematic review and meta-analysis. Int J Cardiol. 2006;111(3):343–351. doi: 10.1016/j.ijcard.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 81.Zutz A, Ignaszewski A, Bates J, Lear SA. Utilization of the internet to deliver cardiac rehabilitation at a distance: a pilot study. Telemed J E Health. 2007;13(3):323–330. doi: 10.1089/tmj.2006.0051. [DOI] [PubMed] [Google Scholar]
- 82.Schwaab B. Telemedicine in cardiac rehabilitation--a literature review and critical appraisement. Rehabilitation. 2007;46(5):276–282. doi: 10.1055/s-2007-985167. [DOI] [PubMed] [Google Scholar]