Abstract
Background There is a consensus that the large fluctuations in mortality seen in Russia in the past two decades can be attributed to trends in alcohol consumption. However, the precise mechanisms linking alcohol to mortality from circulatory disease remain unclear. It has recently been argued that a substantial number of such deaths currently ascribed to cardiovascular disorders are misclassified cases of acute alcohol poisoning.
Methods Analysis of routine mortality data and of a case–control study of mortality among working-age (25–54 years) men occurring in the Russian city of Izhevsk, west of the Ural mountains, 2003–05. Interviews were carried out with proxy informants for both the dead cases (N = 1750) and the controls (N = 1750) selected at random from a population register. Mortality was analysed according to indicators of alcohol problems.
Results Hazardous drinking was associated with an increased risk of death from circulatory diseases as a whole [odds ratio (OR) = 4.14, 95% confidence interval (CI) 3.23, 5.31] adjusted for age, smoking and education. The association with alcoholic cardiomyopathy was particularly strong (OR = 15.7, 95% CI 9.5, 25.9). Although there was no association with deaths from myocardial infarction (MI; OR = 1.17, 95% CI 0.59, 2.32), there was a strong association with the aggregate of all other ischaemic heart disease (IHD; OR = 4.04, 95% CI 2.79, 5.84). Stronger associations for each of these causes (other than MI) were seen with whether or not the man had drunk very heavily in the previous week. However, associations also remained when analyses were restricted to subjects with no evidence of recent heavy drinking, suggesting that misclassification of acute alcohol poisonings is unlikely to explain these overall associations.
Conclusion Taken as a whole, the available evidence suggests that the positive association of alcohol with increased cardiovascular disease mortality may be best explained as being the result of a combination of chronic and acute alcohol consumption resulting in alcohol-related cardiac disorders, especially cardiomyopathy, rather than being due to misclassification of acute alcohol poisoning. Further work is required to understand the mechanisms underlying the link between heavy alcohol consumption and deaths classified as being due to IHD (other than MI).
Keywords: Russia, alcohol, circulatory disease, acute alcohol poisoning, alcoholic cardiomyopathy, ischaemic heart disease
Introduction
Since the mid-1980s Russia has experienced pronounced mortality fluctuations, particularly among men, driven largely by deaths at working age.1–5 A substantial body of research has concluded that variations in alcohol consumption, particularly of spirits in intensive drinking binges, are likely to underlie these temporal changes.3,6–9 In turn, these variations in consumption have been influenced by the social and economic stresses arising from the transition from communism, as well as changes in supply and affordability of alcohol substances being drunk.10,11 However, there remains uncertainty around the relative importance of different biological mechanisms that may underlie the association between fluctuations in alcohol consumption and fluctuations in specific causes of death.
The most obvious cause of death associated with alcohol is acute alcohol poisoning. This has been and continues to be an important public health problem in Russia and other parts of the former Soviet Union,12,13 currently accounting for ∼4% of all deaths among working-age men in Russia. There is a wide range of other pathological mechanisms by which heavy drinking can lead to death. These include deaths from external causes resulting from intoxication (e.g. drowning, fire accidents, road traffic injury and suicide), deaths from tuberculosis,14 where immune function is impaired, perhaps as a consequence of concomitant malnutrition, deaths from pneumonia (often following aspiration of vomit) and deaths from cirrhosis and pancreatitis due to long-term end organ damage caused by the toxic effects of ethanol and its metabolites. All of these causes have shown clear fluctuations in Russia that were highly correlated with those of mortality from alcohol poisonings and of mortality as a whole.
Circulatory disease has also shown parallel fluctuations over time, with mortality rates broadly following those for more obviously alcohol-related causes. This has been apparent for both mortality from ischaemic heart as well as cerebrovascular disease.4 Among deaths from cardiovascular disease, alcoholic cardiomyopathy is one cause that is explicitly related to alcohol. This potentially very important cause of death has been often overlooked in previous work, largely because until 2005 it was not routinely tabulated as a cause of death in Russia in official mortality statistics.
A recent review of the link between circulatory disease and alcohol emphasized the variety of different mechanisms that underlie these associations.15 However, the pattern of fluctuations in ischaemic heart disease (IHD) mortality in Russia provides a challenge to the view that for this particular end point alcohol has a largely cardio-protective effect. Yet, as we have previously argued, there is a range of mechanisms that could explain the increased IHD risk associated with alcohol in the Russian context, not least the particularly adverse effects of heavy, episodic drinking of spirits, a phenomenon that is widespread in Russia and much less important in the West.16 This is supported by a recent analysis of time-series mortality data.17 However, a recent article in this journal concluded that the Russian trends in cardiovascular mortality are in fact due to deaths from acute alcohol poisoning being incorrectly classified as due to IHD.18
In this article, we report the results of a series of analyses of the association of circulatory disease mortality with alcohol in a case–control study conducted in Russia between 2003 and 2005. These are placed in the context of fluctuations in circulatory disease mortality in Russia over the past 25 years. Improved understanding of this phenomenon is a priority, not least because the very high rates of circulatory disease mortality in Russia importantly contribute to the extraordinarily low life expectancy, especially among men, which in 2008 was just under 62 years.
Methods
We present the findings of new analyses of a population-based case–control study undertaken in the city of Izhevsk, a city in European Russia with a typical demographic profile. As described in detail elsewhere,19,20 subjects were men aged 25–54 years resident in the city and living in households with at least one other person. Over a 24-month period in 2003–05, information about all deaths of male residents aged 25–54 years were notified to us by the registrar of deaths (ZAGS). Controls were live men selected from a 2002 population register, frequency matched to the age distribution of the cases. Interviews were sought with proxy informants (wife, daughter or other person living in the deceased’s household) for all the deaths (cases) and live controls. In total, we obtained 1750 proxy interviews for dead men and 1750 for live men, representing 62 and 57% proxy response rates, respectively.
The questionnaire covered a range of characteristics including alcohol consumption, smoking, socio-economic and demographic variables. For the purposes of this article, we defined a man as a hazardous drinker if over the previous year he was reported by his proxy informant to have one or more of the following behaviours:
drinking of non-beverage alcohols, such as alcohol-containing medicines and eau de colognes,21 the consumption of which we have previously shown is strongly associated with all-cause mortality;19
an average of twice-weekly or more occurrence of excessive drunkenness, hangover or going to sleep at night clothed because of being drunk;
having one or more episodes of zapoi. This is a Russian term used to describe a period of ≥2 days of continuous drunkenness when the person is withdrawn from normal social life.22
In this article, our definition of a hazardous drinker excluded the small number of men whose only problematic behaviour from the above list was an episode of zapoi in the previous week. This was to make it a clearer marker of chronic, longer-term hazardous drinking. However, we separately analysed associations with having had an episode of zapoi in the previous week, as this provided information about the acute effects on mortality of this binge drinking pattern.
Apart from information from proxy interviews for each case and control, we obtained information about whether or not each man had been previously registered at the city’s Narcology Dispensary, the main treatment facility for alcohol problems. This information, obtained for all subjects regardless of whether or not an interview was carried out, was abstracted from clinical records blind to case–control status. As 99% of registrations among men aged 25–54 years had an alcohol-related diagnosis, this provided information on alcohol problems free of observer and recall bias.
In summary, therefore, in these analyses we had three measures of alcohol problems: registration with the narcology dispensary, hazardous drinking and whether or not the man had an episode of zapoi in the previous week. These three markers may be seen as lying along a distal–proximal axis with respect to recent drinking behaviour. Registration with the narcology dispensary is the most distal, being a measure of a tendency to heavy and problematic drinking at some point in the past. Indeed some men who were previously registered had abstained in the previous year. The marker of hazardous drinking we used was a composite of different types of drinking behaviour and consequences thereof in the past year. Although strongly predicting whether or not a man had drunk recently, it was more a measure of chronic rather than recent heavy drinking. However, a proxy report of zapoi in the past week is a direct measure of recent (proximal) acute exposure to alcohol, although it did not include men who had had recent drinking binges that had lasted <2 days.
Deaths were coded to the 10th Revision of the International Classification of Diseases (ICD) by the certifying doctor, pathologist or forensic specialist. Of the deaths for which we have proxy interviews, 69% had cause of death determined at forensic autopsy. For the vast majority of these, we obtained data on blood alcohol concentration (BAC) (g/l) as determined at forensic autopsy.
Logistic regression was used to estimate the strength of association of factors with mortality, with all analyses being conducted using STATA 11. In all models age was included in six 5-year categories. Education, smoking and marital status were treated as potential confounders and were introduced into models as categorical variables.
To place these results in a broader context, we also examined routine mortality data from Russia for the years 1980–2007, taking into account the introduction of ICD10 for cause-of-death coding in 1999. This was accompanied by gradual changes in the practice of certifying underlying cause of death.
Ethical approval for the case–control study was obtained from the committees of the Izhevsk Medical Academy and the London School of Hygiene & Tropical Medicine.
Results
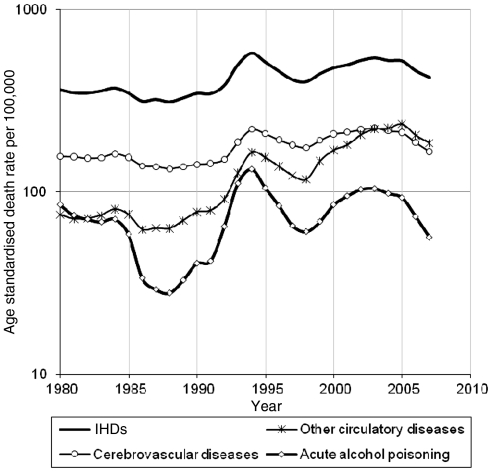
Circulatory disease mortality in Russia has shown substantial temporal fluctuations since the mid-1980s, which have been particularly pronounced at working ages.3,4Figure 1 shows these trends divided into three categories: IHD, cerebrovascular disease and other circulatory conditions. These three groups show a very similar pattern of fluctuation, although the residual group of other circulatory diseases has superimposed upon it an upward trend. Figure 1 also shows a very similar pattern for the trend in acute alcohol poisonings.
Figure 1.
Age-standardized death rates (per 100,000) for selected causes of circulatory disease in Russia since 1980–2007, for men aged 35–69 years
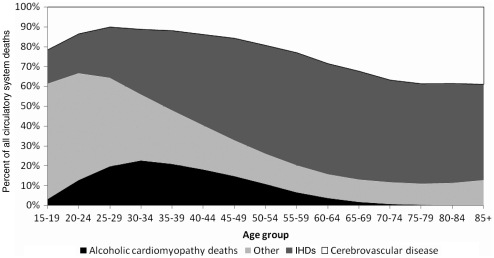
The ‘other’ category of circulatory disease mortality shown in Figure 1 includes deaths from alcoholic as well as non-alcoholic cardiomyopathies. As discussed further below, alcoholic cardiomyopathy is a well-known consequence of long-term heavy drinking. However, it is only since 2005 that routinely available mortality data for Russia have shown mortality rates for cardiomyopathies as a separate category. Previously, they were aggregated into broader cause of death categories in the Russian cause of death classification. However, alcoholic cardiomyopathy constitutes a substantial part of this ‘other’ cardiovascular disease group, particularly below the age of 50 years (Figure 2).
Figure 2.
Cause-specific components of all deaths from circulatory system disorders by age among men, Russia, 2005
Distribution of deaths by cause and autopsy status
Within the Izhevsk study, the distribution of circulatory disease deaths among men aged 25–54 years is shown in Table 1. These deaths constitute one-third of the 1750 deaths from all causes that had proxy interviews.19 Within the group of circulatory disease deaths, IHD deaths comprised 45%, cardiomyopathies 32% and cerebrovascular disease 18%. These figures are broadly consistent with the national picture shown in Figure 2.
Table 1.
Blood alcohol concentrations determined at forensic autopsy by cause of death, men aged 25–54 years, Izhevsk, Russia, 2003–05
| Cause of death | ICD10 codes | Total number of deathsa | Percentage (number) subject to forensic autopsy | Mean BAC g/l (N) | Percentage with BAC >2.5 g/l | Percentage with BAC ≥4 g/l |
|---|---|---|---|---|---|---|
| Circulatory disease | I00–I99 | 573 | 71.7 (411) | 0.97 (401) | 17.0 | 5.0 |
| IHD | I20–25 | 258 | 76.7 (198) | 0.80 (197) | 13.2 | 4.1 |
| MI | I21, I22, I25.2 | 66 | 43.9 (29) | 0.55 (28) | 0.0 | 0.0 |
| Other IHD | Remainder I20–I25 | 192 | 88.0 (169) | 0.84 (169) | 15.4 | 4.7 |
| Alcoholic cardiomyopathy | I42.6 | 121 | 95.9 (116) | 1.45 (111) | 27.0 | 8.1 |
| Other cardiomyopathy | Remainder I42 | 61 | 93.4 (57) | 0.96 (57) | 15.8 | 3.5 |
| Cerebrovascular disease | I60–I69 | 100 | 25.0 (25) | 0.14 (21) | 0.0 | 0.0 |
| Haemorrhagic stroke | I61 | 45 | 40.0 (18) | 0.09 (15) | 0.0 | 0.0 |
| Occlusive stroke | I63 | 21 | 4.8 (1) | – (0) | – | – |
| Other cerebrovascular disease | Remainder I60–I69 | 34 | 17.6 (6) | 0.27 (6) | 0.0 | 0.0 |
| Other circulatory disease | Remainder I00–I99 | 33 | 45.5 (15) | 1.00 (15) | 20.0 | 6.7 |
| Acute alcohol poisoning | X45 | 95 | 97.9 (93) | 4.30 (93) | 94.6 | 55.9 |
| All causes | – | 1750 | 69.1 (1209) | 1.39 (1140) | 23.8 | 8.2 |
aThese are deaths with proxy interviews.
A total of 7 out of 10 deaths from all causes combined, and from circulatory diseases as a whole, were subject to forensic autopsy, whereas almost all of the deaths certified as due to acute alcohol poisoning had been subject to forensic autopsy (Table 1). There was, however, considerable variation in this proportion by type of circulatory disease. Although occlusive stroke was rarely certified as a cause among those subject to forensic autopsy, alcoholic cardiomyopathy was almost exclusively certified by forensic specialists. Myocardial infarction (MI) deaths were almost equally likely to be certified at forensic autopsy or elsewhere, although nearly 9 out of 10 deaths from other forms of IHD were determined at forensic autopsy. Detailed information was available on results of a subset of forensic autopsies undertaken on cases, including 69 of 258 deaths attributed to IHD and 36 of 121 attributed to alcoholic cardiomyopathy. Fifty-three (77%) of those attributed to IHD had evidence of coronary artery obstruction [7 (>75% obstructed); 8 (50–75%); 38 (<50%)] compared with only 13 (36%) of those attributed to alcoholic cardiomyopathy, of which 9 were <50% obstructed and 4 were 50–75%. Only one case attributed to IHD had histological evidence of cardiomyopathy.
Cause-specific variation in blood alcohol concentrations at autopsy
Blood alcohol concentrations found at forensic autopsy varied considerably by cause (Table 1). They were by definition particularly high for acute alcohol poisoning deaths, with almost all having BAC levels >2.5 g/l and the majority ≥4 g/l—usually regarded as a fatal concentration. In contrast, less than 1 in 10 of any of the circulatory system disease deaths shown in Table 1 had BACs of ≥4 g/l. Alcoholic cardiomyopathy showed the highest BAC levels of any of the circulatory system deaths, although deaths from each type of cerebrovascular disease had zero or very low levels. Among the IHD deaths, BAC levels were very low for deaths certified as being due to MIs but were moderately raised for other forms of IHD.
The prevalence of selected indicators of heavy or problematic alcohol drinking by cause of death are shown in Table 2 for all deaths and separately for deaths subject to forensic autopsy with zero or low BAC levels. Among controls the prevalence of narcology dispensary registration was 4.1%, of hazardous drinking was 13.1% and of zapoi in the last week 2.6%. Among the cases (deaths), narcology dispensary registration was notably high for alcoholic cardiomyopathy and acute alcohol poisoning. This is consistent with the high prevalence of proxy reported hazardous drinking for both of these causes, and of zapoi in the week prior to death. In contrast, those dying from MI had a low prevalence of all three of these indicators of heavy or problematic drinking. Deaths from other forms of IHD had prevalences of these adverse alcohol behaviour indicators that were intermediate between MI on the one hand, and alcoholic cardiomyopathy and acute alcohol poisoning on the other. Similar cause-specific patterns were seen for the subset of deaths with zero or low levels of BAC at forensic autopsy. This suggests that the factors driving the cause-specific variation in the prevalence of alcohol problems were independent of whether or not potentially lethal BAC levels were found at forensic autopsy.
Table 2.
Percentage prevalence of alcohol problems by cause of death, men aged 25–54 years, Izhevsk, Russia, 2003–05
| Cause of death |
All deaths |
Deaths with BAC ≤2.5 g/l at forensic autopsya |
||||
|---|---|---|---|---|---|---|
| Registered with narcology dispensary | Hazardous drinkerb (proxy report) | Zapoi in previous week (proxy report) | Registered with narcology dispensary | Hazardous drinkerb (proxy report) | Zapoi in previous week (proxy report) | |
| Circulatory disease | 16.2 (93) | 43.5 (224) | 20.8 (118) | 18.3 (61) | 47.6 (140) | 23.2 (76) |
| IHD | 11.6 (30) | 37.4 (86) | 14.5 (37) | 12.9 (22) | 40.0 (60) | 15.4 (26) |
| MI | 4.5 (3) | 21.3 (13) | 10.6 (7) | 10.7 (3) | 28.0 (7) | 17.9 (5) |
| Other IHD | 14.1 (27) | 43.2 (73) | 15.8 (30) | 13.3 (19) | 42.4 (53) | 14.9 (21) |
| Alcoholic cardiomyopathy | 32.2 (39) | 72.6 (77) | 50.0 (60) | 34.6 (28) | 62.9 (44) | 43.2 (35) |
| Other cardiomyopathy | 13.1 (8) | 40.7 (22) | 16.9 (10) | 14.6 (7) | 39.5 (17) | 15.2 (7) |
| Cerebrovascular disease | 14.0 (14) | 29.5 (28) | 10.0 (10) | 19.0 (4) | 65.0 (13) | 38.1 (8) |
| Haemorrhagic stroke | 8.9 (4) | 44.2 (19) | 22.2 (45) | 20.0 (3) | 78.6 (11) | 53.3 (8) |
| Occlusive stroke | 19.0 (4) | 20.0 (4) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| Other cerebrovascular disease | 17.6 (6) | 15.6 (5) | 0.0 (0) | 16.7 (1) | 33.3 (2) | 0.0 (0) |
| Other circulatory disease | 6.1 (2) | 36.7 (11) | 3.1 (1) | 0.0 (0) | 54.6 (6) | 0.0 (0) |
| Acute alcohol poisoning | 27.4 (26) | 74.7 (62) | 42.1 (40) | 20.0 (1) | 60.0 (3) | 40.0 (2) |
| All causes | 16.7 (292) | 58.4 (747) | 22.0 (381) | 18.6 (869) | 54.7 (416) | 26.2 (224) |
| Total number of all- cause deaths | 1750 | 1542 | 1734 | 869 | 761 | 856 |
Figures in parentheses are numerators for percentages. Denominators vary within cause because of missing data.
aRestricted to deaths subject to forensic autopsy.
bHazardous drinker defined as proxy report of one or more of the following in the past year: drinking non-beverage alcohol or one or more episodes of zapoi (excluding those who only had an episode of zapoi in previous week), or twice weekly or more occurrence of excessive drunkenness, hangover or going to sleep at night because of being drunk.
As might be expected, cases with a proxy report of zapoi in the week before death had appreciably higher mean BAC levels compared with those who did not (1.85 vs 1.20 g/l) and a higher prevalence of the potentially fatal level of ≥4 g/l (14.8 vs 5.5%).
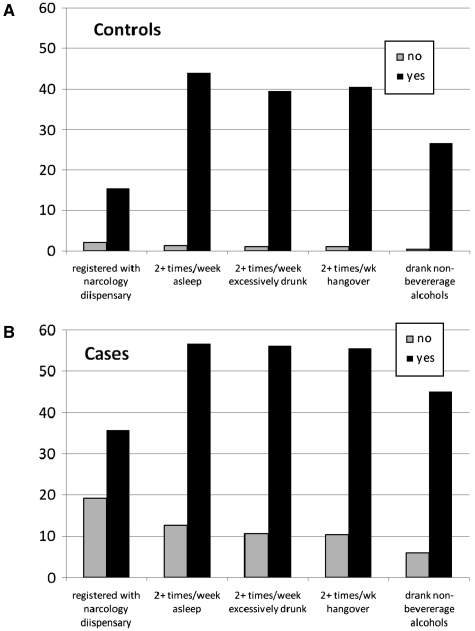
Registration with the narcology dispensary and the indicators of hazardous and heavy drinking used in this article relate to chronic alcohol problems extending over at least a year before interview. However, these markers of chronic problems are inevitably confounded with whether the man had an episode of heavy drinking (zapoi) in the week before death (or interview for the controls). This is shown in Figure 3, where indicators of problem drinking are strongly associated having had a recent episode of zapoi.
Figure 3.
Percentage of controls (A) and cases (B) (deaths from all causes) with proxy reports of other indicators of problem drinking in previous year according to whether or not they had an episode of zapoi in the week before interview/death
Association of problem drinking with cause-specific mortality
The strength of associations of cause-specific mortality (adjusted for age, smoking and education) with three binary indicators of alcohol problems are shown in Table 3. Alcoholic cardiomyopathy and acute alcohol poisoning show similar, very high ORs with each of the three alcohol variables. In contrast, MI shows little evidence of an association with any of the alcohol variables. However, the larger aggregate of all other types of IHD deaths, shows moderately raised ORs. Haemorrhagic stroke shows elevated ORs for hazardous drinking and zapoi within the past week, although no evidence of an association with narcology dispensary registration.
Table 3.
Cause-specific mortality ORs by type of alcohol problem adjusted for education and smoking
| Cause of death |
Registered with narcology dispensary |
Hazardous drinkera (proxy report) |
Zapoi in previous week (proxy report) |
|||
|---|---|---|---|---|---|---|
| OR (95% CI) | Cases | OR (95% CI) | Cases | OR (95% CI) | Cases | |
| Circulatory disease | 3.71 (2.52–5.47) | 72/414 | 4.14 (3.23–5.31) | 213/273 | 9.62 (6.2–14.91) | 97/389 |
| IHD | 2.54 (1.50–4.31) | 25/194 | 3.04 (2.17–4.24) | 82/137 | 4.70 (2.64–8.39) | 28/191 |
| MI | 0.62 (0.14–2.66) | 2/57 | 1.17 (0.59–2.32) | 12/47 | 2.03 (0.66–6.28) | 4/55 |
| Other IHD | 3.26 (1.88–5.64) | 23/137 | 4.04 (2.79–5.84) | 70/90 | 5.85 (3.18–10.7) | 24/136 |
| Alcoholic cardiomyopathy | 10.42 (6.05–17.9) | 31/67 | 15.7 (9.5–25.94) | 72/26 | 40.5 (23.0–71.4) | 51/47 |
| Other cardiomyopathy | 2.86 (1.05–7.79) | 5/46 | 3.84 (2.05–7.18) | 21/30 | 7.87 (3.31–18.7) | 9/42 |
| Cerebrovascular disease | 2.45 (1.16–5.17) | 10/80 | 2.05 (1.24–3.40) | 27/63 | 3.02 (1.28–7.11) | 8/82 |
| Haemorrhagic stroke | 0.82 (0.19–3.56) | 2/38 | 3.72 (1.90–7.27) | 18/22 | 6.89 (2.8–16.99) | 8/32 |
| Occlusive stroke | 4.72 (1.23–18.2) | 3/15 | – | 4/14 | – | 0/18 |
| Other cerebrovascular disease | 4.61 (1.58–13.5) | 5/27 | 0.93 (0.34–2.54) | 5/27 | – | 0/32 |
| Other circulatory disease | 0.61 (0.08–4.70) | 1/27 | 3.43 (1.51–7.81) | 11/17 | 1.18 (0.15–9.38) | 1/27 |
| Acute alcohol poisoning | 6.79 (3.62–12.8) | 18/60 | 18.9 (10.7–33.3) | 58/20 | 33.63 (18.1–62.4) | 34/44 |
| All causes | 4.03 (2.93–5.54) | 220/1226 | 5.46 (4.50–6.61) | 698/748 | 11.41 (7.78–16.7) | 316/1130 |
Cases: the number of cases with/without particular drinking behaviour. 95% CI, 95% confidence interval.
aHazardous drinker defined as proxy report of one or more of the following in the past year: drinking non-beverage alcohol or one or more episodes of zapoi (excluding those who only had an episode of zapoi in previous week), or twice weekly or more occurrence of excessive drunkenness, hangover or going to sleep at night because of being drunk.
For most causes in Table 3, the highest ORs were for having zapoi in the previous week. This was particularly pronounced for deaths attributed to acute alcohol poisoning and alcoholic cardiomyopathy. For acute alcohol poisoning, this is not surprising as a heavy episode of drinking in the period immediately prior to death is a necessary condition for the diagnosis of this cause.
A proportion of the men who were classified as being hazardous drinkers did not have an episode of heavy drinking in the week prior to death/interview. The association of mortality with indicators of problem drinking in this subgroup provides an indication of the hazards of chronic alcohol problems. In Table 4 we have restricted analyses to cases and controls where there was no proxy report of an episode of zapoi in the week before death. Moreover, we have only included cases with BAC levels at forensic autopsy that were ≤2.5 g/l. Results for subcategories of cerebrovascular disease and acute alcohol poisoning are not tabulated because there were few or zero deaths meeting these criteria.
Table 4.
Cause-specific mortality ORs for deaths with BAC at forensic autopsy ≤2.5 g/l by type of alcohol problem restricted to those who were reported by proxies as not having an episode of zapoi in the previous week, adjusted for education and smoking
| Cause of death |
Registered with narcology dispensary |
Hazardous drinkera (proxy report) |
||
|---|---|---|---|---|
| OR (95% CI) | Cases | OR (95% CI) | Cases | |
| Circulatory disease | 3.05 (1.89–4.92) | 32/211 | 3.33 (2.38–4.67) | 78/138 |
| IHD | 2.16 (1.15–4.06) | 15/124 | 2.70 (1.76–4.16) | 40/84 |
| MI | 1.53 (0.34–6.97) | 2/21 | 1.05 (0.34–3.27) | 4/18 |
| Other IHD | 2.27 (1.17–4.42) | 13/103 | 3.18 (2.01–5.03) | 36/66 |
| Alcoholic cardiomyopathy | 8.11 (3.71–17.7) | 11/30 | 4.29 (2.07–8.89) | 15/19 |
| Other cardiomyopathy | 3.69 (1.34–10.2) | 5/35 | 2.89 (1.33–6.29) | 11/25 |
| Cerebrovascular disease | 2.31 (0.27–19.6) | 1/10 | 7.10 (2.02–24.9) | 6/5 |
| All causes | 3.80 (2.62–5.50) | 87/513 | 4.78 (3.71–6.15) | 218/307 |
Cases: the number of cases with/without particular drinking behaviour. 95% CI, 95% confidence interval.
aHazardous drinker defined as proxy report of one or more of the following in the past year: drinking non-beverage alcohol or one or more episodes of zapoi (excluding those who only had an episode of zapoi in previous week), or twice weekly or more occurrence of excessive drunkenness, hangover or going to sleep at night because of being drunk.
The pattern of mortality by cause seen in Table 4 is very similar to that shown in Table 3, although, in general, the ORs are a little smaller. Alcoholic cardiomyopathy still shows notably strong associations with the two alcohol variables, although the OR for hazardous drinking is much reduced compared with Table 3. Mortality from the aggregates of all causes and all circulatory diseases continue to show robust associations. As in Table 3, deaths ascribed to MI do not show any association, while those in the category of other IHD continue to show moderately strong associations with alcohol problems. These results suggest that long-term hazardous drinking is also associated with substantial increases in mortality from cardiovascular disease independent of any acute hazards associated with recent episodes of heavy drinking.
Discussion
We have found that mortality from all causes, circulatory disease and acute alcohol poisoning are strongly associated with markers of alcohol problems: registration with the alcohol treatment service (narcology dispensary), proxy report of hazardous drinking over the preceding year and proxy reports of whether or not an extended binging drinking episode (zapoi) occurred in the previous week. There is striking variation in the magnitude of these effects between causes and as well as across markers. This latter variation is informative about the contribution of chronic versus acute effects of alcohol on mortality, and leads us to conclude that, depending upon cause of death, both chronic as well as acute effects of alcohol drinking are implicated in risk of circulatory disease death.
These results are based on a case–control study using proxy informants. The strengths and weaknesses of this design and this particular study have been discussed in detail elsewhere.19,20 One of the main issues of concern is the validity of information from proxy interviews. However, the questions on alcohol were chosen to identify easily observable behaviours and characteristics (e.g. hangover) rather than to provide quantitative estimates of usual amount drunk, which are more difficult for a proxy to observe directly. Nevertheless, it is possible that proxy responses may be affected by the fact of death for the cases relative to the controls. It is reassuring therefore, that the pattern of cause-specific variation of ORs for narcology registration (based on medical records) is very similar to that observed for hazardous drinking and recent zapoi (based on proxy interview).
The difference in magnitude of ORs between zapoi in the previous week and hazardous drinking is unlikely to be explained by differential recall, as both are derived from proxy interview.
Alcohol poisoning
This cause of death has one of the strongest associations with our markers of alcohol problems. As one would anticipate, the vast majority of deaths attributed to this cause had BAC levels at autopsy that were >2.5 g/l, with over half having fatal levels of ≥4 g/l. However, it is clear that there are other deaths in the study with high BAC levels which were not attributed to acute alcohol poisoning. The process by which this causal attribution is made at forensic autopsy involves a balanced judgement drawing in other findings at autopsy beyond that of BAC.
The primary mechanism assumed to underlie deaths from this cause is ethanol-induced paralysis of the respiratory centre of the brain.23,24 This results in fatal respiratory and/or circulatory failure. However, unless these events are observed directly by a trained informant, alcohol poisoning is almost impossible to establish with certainty post mortem. In particular, it is almost impossible to distinguish it from coincident fatal arrhythmia. It is generally determined by exclusion of other more identifiable causes when moderate or high ethanol concentrations have been found in the blood and (often) in urine. A BAC level of ≥5.0 g/l is regarded as very likely to be fatal. However, lethal concentrations determined at autopsy have been described as ranging from 2.3 to 4.0 g/l,24 with thresholds varying by sex, age and drinking history.25
Assignment of acute alcohol poisoning as the underlying cause of death is most problematic when BAC at autopsy is between 2.5 and 4.5 g/l. Because alcohol is rapidly cleared from the blood,26 these relatively high concentrations will nearly always have been the result of consumption of large volumes of ethanol in the hours immediately preceding death. However, such a heavy drinking bout is most likely to occur among those with a history of regular heavy drinking rather than being an isolated and atypical event in the person’s biography. Chronic patterns of heavy drinking induce end-organ damage including fatty liver and cirrhosis, alcoholic cardiomyopathy and oesophageal varices, some or all of which may be found at autopsy. The forensic specialist will need to consider the macroscopic and histological evidence, as well as what was known at the time of autopsy about pre-existing illness, before deciding whether the underlying cause of death was indeed alcohol poisoning.
The conclusion to be drawn from this is that for deaths with moderate or high BAC levels at autopsy, establishing a definitive cause of death is a matter of judgement, and possibly medical tradition. Whether a death is attributed to acute poisoning per se or to the frequently coexisting alcohol-induced end-organ damage is a difficult line to draw. This will inevitably result in some element of misclassification of sudden deaths, especially for those with BAC levels 2.5–4.5 g/l.
IHD
IHD is the largest single category of circulatory disease mortality in this study. Of these, only one-quarter (26%) were coded to MI. This is substantially lower than the corresponding proportion (43%) for the same age group England and Wales in 2008.27 Overall, IHD shows a moderately strong association with indicators of problem drinking. However, what is striking is that the mortality from MI does not show any association with our alcohol variables. In contrast, the residual category of ‘other’ IHD shows moderately strong associations, even in the subset of men who did not have an episode of zapoi in the previous week and where the deaths had low or zero BAC levels at autopsy. Unlike most other deaths in this analysis, a much smaller proportion of MI deaths was certified at forensic autopsy and had a prior registration with the narcology dispensary. However, even those certified at forensic autopsy had very low or zero BAC levels and only one of those for whom we had detailed autopsy data had histological evidence of cardiomyopathy. All of this suggests that these are sudden deaths where there was little, if any, indication of a history of heavy drinking, where the diagnosis of MI may have been uncomplicated by any alcohol-induced comorbidities.
Our findings are consistent with a cohort study conducted in Novosibirsk 1985–98 of men aged 25–64 years on entry.28 This found that men who drank heavily on a regular basis had a 2-fold increased risk of death from circulatory disease, with a suggestion of a similar effect for IHD. However, the authors comment in their discussion that they did not find such an increased risk for non-fatal MIs, which were almost certainly ascertained using MONICA criteria. This is consistent with our failure to find an association for fatal MIs. Similar results were reported in a very large case–control study of deaths aged 15–74 years in the 1990s in three industrial cities of western Siberia with predominantly European Russian populations.8 Again, the pattern was found of an association of heavy drinking with IHD deaths (excluding MI) but not with acute MI itself.
There is a substantial body of evidence that moderate alcohol drinking has a positive (protective) effect upon blood lipid profile and appears to be associated with a reduced risk of coronary artery disease.15 The numbers of deaths from MI in our study may be insufficient to be able to detect this protective effect. However, the challenge is to understand the nature of the moderately strong increased risk of mortality from ‘other’ IHD that we and others have found. This diagnosis will be given in cases of sudden death associated with alcohol that may involve other pathologies other than infarcts. We have previously reviewed evidence that both acute drinking episodes in moderate or heavy drinkers and withdrawal in heavy drinkers are associated with an increased risk of heart failure and arrhythmia.16 These deaths may well be ascribed to ‘other’ IHD. In addition, these ‘other’ IHD deaths could be secondary to undiagnosed and undetected dilated cardiomyopathies.
Alcoholic cardiomyopathy
Alcoholic cardiomyopathy deaths comprised 20% of all circulatory system deaths in this study. We have found that this cause of death was as strongly associated with markers of alcohol problems as acute alcohol poisoning, particularly zapoi in the previous week. In addition, like acute alcohol poisoning, the cause of 95% of these deaths were determined at forensic autopsy. However, these two causes differed in that only one-quarter of the alcoholic cardiomyopathy deaths had BAC levels >2.5 g/l compared with acute alcohol poisoning where 95% had these levels. Moreover, alcoholic cardiomyopathy showed strong associations with alcohol problem indicators even among men who did not have an episode of zapoi in the previous week and had BAC levels at death of ≤2.5 g/l. This restriction ensures that there were almost no deaths that could be misclassified cases of acute alcohol poisoning in the subset.
Our findings with respect to cardiomyopathy are consistent with clinical studies which suggest that heavy alcohol drinking over a prolonged number of years is associated with dilated cardiomyopathy, which in turn leads to a substantial mortality due to arrhythmia and heart failure.15,29,30 These are likely to present as sudden deaths. Importantly, there is some evidence that abstinence reduces case fatality among those suffering from alcoholic cardiomyopathy.31 This may partly explain why there appears to be particularly strong acute as well as chronic effect of alcohol on risk of death from this cause. However, it is possible that some of the deaths from this cause with high BACs (≥4 g/l) are misclassified acute alcohol poisonings, although they make up only 5% of the total.
To our knowledge, no other epidemiological studies of the association of alcohol with alcoholic cardiomyopathy in Russia have been published. This is almost certainly because until the middle of the 2000s, this cause was not separately coded by ZAGS, the institution responsible for registering and certifying deaths in Russia.
Cerebrovascular disease
Just under one in five of the deaths from circulatory disease in this study were classified as due to cerebrovascular disease, of which almost half were haemorrhagic strokes. This compares with 31% of stroke deaths being haemorrhagic in men aged 25–54 years in England and Wales in 2008.27 Only one-quarter of deaths classified as due to cerebrovascular disease were subject to forensic autopsy, and none of these had BAC levels >2.5 g/l. Nevertheless, haemorrhagic stroke in particular was strongly associated with recent zapoi, although not with previous registration with the narcology dispensary.
The Novosibirsk cohort study28 failed to find an association of stroke with binge drinking, although as in our study, they only had 100 deaths from this cause in total. The recent large case–control study from western Siberia8 did find some evidence of a positive association with amount drunk on single occasions, but this effect was weaker than for IHD, as was indeed the case in our study.
Our finding of an association of alcohol with cerebrovascular disease is consistent with the broader literature.32 Mechanisms include the hypertensive effects of drinking alcohol33 as well as the impairment of coagulation specific to binge drinking,16 both of which persist for several days after an acute drinking episode. Haemorrhagic stroke is particularly strongly linked to heavy alcohol drinking, probably through both the acute pressor effects of alcohol on blood pressure as well as through its impact on clotting mechanisms.15 These effects may be acute and transient, which could explain the particularly strong association of haemorrhagic stroke with recent zapoi that we found, consistent with a recent suggestion that binge drinking may be particularly hazardous.34
Misclassification of cause of death
As already discussed above, the determination of cause of death at autopsy when there are moderate or high levels of BAC is not straightforward, and is a process that will inevitably result in some misclassification. However, a recent article in this journal18 took the possibility of misattribution of cause to its limits by arguing that ‘alcohol poisoning’ was the main cause of the fluctuations in mortality in Russia in the past two decades. This view was based on an analysis of routine Russian mortality data together with a study of forensic autopsy deaths from the city of Barnaul in the Altai region of Siberia between 1990 and 2004. This misclassification argument crucially hinges upon the observation that in their Barnaul forensic autopsy series there was a substantial proportion of circulatory disease deaths with potentially lethal BAC levels: among men aged 35–69 years 14% had BAC levels of ≥4.0 g/l . The majority of these deaths were from the category of ‘other’ IHD, of which over 15% had BAC ≥4.0 g/l, whereas only 3% of MI deaths had such high BAC levels.
Our own Izhevsk data show much lower shares of BAC ≥4.0 g/l than those in the Barnaul data. While our data agree with those from Barnaul, in that MI deaths are far less likely to have elevated BAC that ‘other’ IHD deaths (although both are at much lower levels in our study), we believe that the authors over-interpret the significance of a raised BAC among deaths from ‘other’ IHD. They assume that deaths with high BAC levels must, by definition, be due to acute alcohol poisoning. But as discussed above, this is not necessarily the case. High BAC levels at autopsy in many cases coexist with end-organ damage due to chronic, long-term alcohol drinking. Although some of these ‘other’ IHD deaths may indeed be due to acute toxic effects per se, many will be due to these comorbidities, or indeed be the result of an interaction of the two: i.e. acutely high BAC against a background of damage caused by long-term heavy drinking. Our analyses, in fact, go further by showing that the association of alcohol problems with increased risk of death from ‘other’ IHD is not dependent upon high BAC or recent heavy drinking episodes, as this association is still apparent when analyses exclude persons with these characteristics. As already discussed, misclassification may be an issue, but it may be due to deaths from alcohol-induced heart failure and arrhythmia being misattributed to IHD.
The suggestion that acute alcohol poisoning may be responsible for the fluctuations in Russian mortality over the past few decades is thus based on weaker evidence than the Barnaul study authors presupposed. There are however, a few more general problems relating to their claim of misclassification that need to be mentioned. For Russia as a whole, age-standardized death rates at ages 35–69 years by IHD (excluding acute MI) and alcohol poisoning during the period 1980–2007 are indeed closely correlated (r = 0.86, P < 0.001). We may assume, for sake of argument, that, as suggested by the Barnaul team, 50% of deaths actually due to alcohol poisoning are mistakenly classified as ‘other’ IHD and reallocate these deaths accordingly. Experiments with distributions of the reallocated deaths, showed that the minimum of the correlation between the remaining cardiovascular deaths and accidental poisoning by alcohol is reached when the reallocated deaths are distributed by age exactly as deaths from the alcohol poisonings. But even in this case, the association is reduced only marginally (r = 0.74, P < 0.001). Hence, the misclassification proposed can, at best, only explain a very small proportion of the observed association between IHD and acute alcohol poisoning.
Over the same calendar period, age-standardized death rates at ages 35–69 years by cerebrovascular disorders are highly correlated with alcohol poisoning (r = 0.86, P < 0.001). This correlation cannot be explained in terms of misclassification of acute alcohol poisoning as both in Izhevsk and Barnaul studies there were almost no deaths with BAC ≥4.0 g/l.
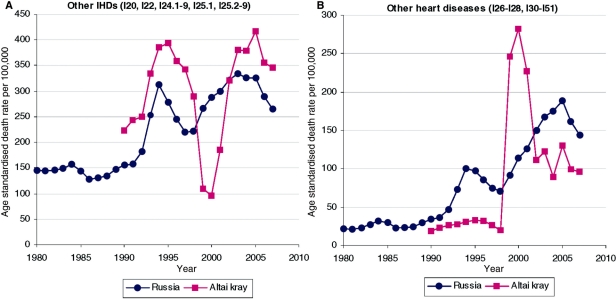
Finally, we have some observations about certain very specific features of mortality in the Altai kray region of Russia, in which Barnaul is located, which lead us to believe that mortality trends there may not be representative of the whole of Russia. It seems that Altai Kray faced particular difficulties with the introduction of the ICD10 system in 1999 and its associated practice of direct coding by physicians instead of statisticians. Figure 4 shows how this transition was associated with an abrupt drop in mortality from other IHDs and a symmetrical abrupt jump in mortality from other (non-ischaemic) heart diseases in the region, but not in Russia as a whole. The artificial exchange between the two causes of death in Altai Kray lasted 3 years, from 1999 to 2001, and then both causes returned to levels consistent with previous trends.
Figure 4.
Trends in age standardised death rates (per 100000) from (a) other iscahemic heart disease, and (b) other heart diseases in Altai Kray and the Russian Federation, 1980–2007, men aged 35–69 years
In summary, we have shown that circulatory disease mortality is strongly related to markers of heavy, problematic drinking in Russia. We have identified for the first time the importance of deaths from alcoholic cardiomyopathy a component of this association. Alcohol-induced changes to architecture of the heart predispose the individual to acute episodes of arrhythmias. Our findings of a relationship with stroke deaths (hemorrhagic stroke in particular) are not surprising and are consistent with the literature. However, the main outstanding puzzle remains as to why the risk of dying from IHD (excluding MI) is associated with heavy alcohol consumption. Contrary to some suggestions, any misclassification of acute alcohol poisoning is insufficient to explain these associations, although misclassification of cardiomyopathies or more subtle alcohol-induced changes in cardiac function may be involved. Further research is required to explore the underlying mechanisms and to resolve how far alcohol-related deaths from circulatory disease in Russia are due to chronic versus acute effects, or indeed their interaction. Resolution of these issues has a significance beyond Russia, as it will throw new light upon the link between heavy alcohol consumption and cardiovascular disease elsewhere.
Funding
The Wellcome Trust supports aspects of the authors’ work on the effects of alcohol on Russian health.
Conflict of interest: None declared.
KEY MESSAGES.
It is accepted that alcohol is likely to play a substantial role in explaining the huge fluctuations in working-age mortality, including that from circulatory disease, seen among men in Russia over the past 25 years.
Mechanisms underlying these associations are unclear, although it has been suggested that misclassification of acute alcohol poisoning might be important.
This article provides the first individual-level analysis of the effects of both chronic hazardous drinking and short-term acute episodes of heavy drinking on circulatory disease mortality.
Our results suggest that deaths from alcoholic cardiomyopathies, overlooked in previous research, are important. Moreover, misclassification of deaths due to the impact of chronic hazardous drinking on heart structure and function (as in cardiomyopathies) is likely to be more important than misclassification of acute alcohol poisonings.
References
- 1.Meslé F, Shkolnikov V. La mortalité en Russie: une crise sanitaire en deux temps. Revue d'études comparitives Est-Ouest. 1995;4:9–24. [Google Scholar]
- 2.Meslé F, Shkolnikov V, Vallin J. Brusque montée des morts violentes en Russie. Population. 1996;3:780–90. [Google Scholar]
- 3.Leon DA, Chenet L, Shkolnikov VM, et al. Huge variation in Russian mortality rates 1984–94: artefact, alcohol, or what? Lancet. 1997;350:383–88. doi: 10.1016/S0140-6736(97)03360-6. [DOI] [PubMed] [Google Scholar]
- 4.Shkolnikov V, McKee M, Leon DA. Changes in life expectancy in Russia in the mid-1990s. Lancet. 2001;357:917–21. doi: 10.1016/S0140-6736(00)04212-4. [DOI] [PubMed] [Google Scholar]
- 5.Men T, Brennan P, Boffetta P, et al. Russian mortality trends for 1991–2001: analysis by cause and region. BMJ. 2003;327:964. doi: 10.1136/bmj.327.7421.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shkolnikov VM, Nemtsov A. The anti-alcohol campaign and variations in Russian mortality. In: Bobadilla J-L, Costello C, Mitchell F, editors. Premature Death in the New Independent States. Washington: National Academy Press; 1997. pp. 239–61. [Google Scholar]
- 7.McKee M, Shkolnikov V, Leon DA. Alcohol is implicated in the fluctuations in cardiovascular disease in Russia since the 1980s. Ann Epidemiol. 2001;11:1–6. doi: 10.1016/s1047-2797(00)00080-6. [DOI] [PubMed] [Google Scholar]
- 8.Zaridze D, Brennan P, Boreham J, et al. Alcohol and cause-specific mortality in Russia: a retrospective case–control study of 48,557 adult deaths. Lancet. 2009;373:2201–14. doi: 10.1016/S0140-6736(09)61034-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leon DA, Shkolnikov VM, McKee M. Alcohol and Russian mortality: a continuing crisis. Addiction. 2009;104:1630–6. doi: 10.1111/j.1360-0443.2009.02655.x. [DOI] [PubMed] [Google Scholar]
- 10.Leon DA, Shkolnikov VM. Social stress and the Russian mortality crisis. JAMA. 1998;279:790–91. doi: 10.1001/jama.279.10.790. [DOI] [PubMed] [Google Scholar]
- 11.Stuckler D, King L, McKee M. Mass privatisation and the post-communist mortality crisis: a cross-national analysis. Lancet. 2009;373:399–407. doi: 10.1016/S0140-6736(09)60005-2. [DOI] [PubMed] [Google Scholar]
- 12.Treml VG. Death from alcohol poisoning in the USSR. Soviet Studies. 1982;34:487–505. [Google Scholar]
- 13.Stickley A, Leinsalu M, Andreev E, et al. Alcohol poisoning in Russia and the countries in the European part of the former Soviet Union, 1970–2002. Eur J Pub Health. 2007;17:444–9. doi: 10.1093/eurpub/ckl275. [DOI] [PubMed] [Google Scholar]
- 14.Lonnroth K, Williams BG, Stadlin S, et al. Alcohol use as a risk factor for tuberculosis—a systematic review. BMC Pub Health. 2008;8:289. doi: 10.1186/1471-2458-8-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klatsky AL. Alcohol and cardiovascular health. Physiol Behav. 2009;100:76–81. doi: 10.1016/j.physbeh.2009.12.019. [DOI] [PubMed] [Google Scholar]
- 16.McKee M, Britton A. The positive relationship between alcohol and heart disease in Eastern Europe: potential physiological mechanisms. J R Soc Med. 1998;91:402–7. doi: 10.1177/014107689809100802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ramstedt M. Fluctuations in male ischaemic heart disease mortality in Russia 1959–1998: assessing the importance of alcohol. Drug Alcohol Rev. 2009;28:390–95. doi: 10.1111/j.1465-3362.2009.00059.x. [DOI] [PubMed] [Google Scholar]
- 18.Zaridze D, Maximovitch D, Lazarev A, et al. Alcohol poisoning is a main determinant of recent mortality trends in Russia: evidence from a detailed analysis of mortality statistics and autopsies. Int J Epidemiol. 2009;38:143–53. doi: 10.1093/ije/dyn160. [DOI] [PubMed] [Google Scholar]
- 19.Leon DA, Saburova L, Tomkins S, et al. Hazardous alcohol drinking and premature mortality in Russia: a population based case-control study. Lancet. 2007;369:2001–9. doi: 10.1016/S0140-6736(07)60941-6. [DOI] [PubMed] [Google Scholar]
- 20.Tomkins S, Shkolnikov V, Andreev E, et al. Identifying the determinants of premature mortality in Russia: overcoming a methodological challenge. BMC Pub Health. 2007;7:343. doi: 10.1186/1471-2458-7-343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gil A, Polikina O, Koroleva N, et al. Availability and characteristics of nonbeverage alcohols sold in 17 Russian cities in 2007. Alcohol Clin Exp Res. 2009;33:79–85. doi: 10.1111/j.1530-0277.2008.00813.x. [DOI] [PubMed] [Google Scholar]
- 22.Treml V. Soviet and Russian statistics on alcohol consumption and abuse. In: Bobadilla J-L, Costello C, Mitchell F, editors. Premature Death in the New Independent States. Washington, DC: National Academy Press; 1997. pp. 220–38. [PubMed] [Google Scholar]
- 23.Poikolainen K. Alcohol Poisoning Mortality in Four Nordic Countries. Vol. 28. Helsinki, Finland: The Finnish Foundation for Alcohol Studies. Alcohol Research in the Northern Countries, 1977; [Google Scholar]
- 24.Jones AW, Holmgren P. Comparison of blood-ethanol concentration in deaths attributed to acute alcohol poisoning and chronic alcoholism. J Forensic Sci. 2003;48:874–79. [PubMed] [Google Scholar]
- 25.Lahti RA, Vuori E. Fatal alcohol poisoning: medico-legal practices and mortality statistics. Forensic Sci Int. 2002;126:203–9. doi: 10.1016/s0379-0738(02)00057-9. [DOI] [PubMed] [Google Scholar]
- 26.Helander A. Biological markers in alcoholism. J Neural Transm Suppl. 2003;66:15–32. doi: 10.1007/978-3-7091-0541-2_2. [DOI] [PubMed] [Google Scholar]
- 27.Office for National Statistics. Mortality Statistics. Deaths Registered in 2008. DR_08. London: ONS, DR; 2009. [Google Scholar]
- 28.Malyutina S, Bobak M, Kurilovitch S, et al. Relation between heavy and binge drinking and all-cause and cardiovascular mortality in Novosibirsk, Russia: a prospective cohort study. Lancet. 2002;360:1448–54. doi: 10.1016/S0140-6736(02)11470-X. [DOI] [PubMed] [Google Scholar]
- 29.Piano MR. Alcoholic cardiomyopathy: incidence, clinical characteristics, and pathophysiology. Chest. 2002;121:1638–50. doi: 10.1378/chest.121.5.1638. [DOI] [PubMed] [Google Scholar]
- 30.Djousse L, Gaziano JM. Alcohol consumption and heart failure: a systematic review. Curr Atheroscler Rep. 2008;10:117–20. doi: 10.1007/s11883-008-0017-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fauchier L, Babuty D, Poret P, et al. Comparison of long-term outcome of alcoholic and idiopathic dilated cardiomyopathy. Eur Heart J. 2000;21:306–14. doi: 10.1053/euhj.1999.1761. [DOI] [PubMed] [Google Scholar]
- 32.Reynolds K, Lewis B, Nolen JD, et al. Alcohol consumption and risk of stroke: a meta-analysis. JAMA. 2003;289:579–88. doi: 10.1001/jama.289.5.579. [DOI] [PubMed] [Google Scholar]
- 33.Chen L, Davey Smith G, Harbord RM, et al. Alcohol intake and blood pressure: a systematic review implementing a Mendelian randomization approach. PLoS Med. 2008;5:e52. doi: 10.1371/journal.pmed.0050052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sundell L, Salomaa V, Vartiainen E, et al. Increased stroke risk is related to a binge drinking habit. Stroke. 2008;39:3179–84. doi: 10.1161/STROKEAHA.108.520817. [DOI] [PubMed] [Google Scholar]