Abstract
Objective
To design and implement a demonstration project to teach interprofessional teams how to recognize and engage in difficult conversations with patients.
Design
Interdisciplinary teams consisting of pharmacy students and residents, student nurses, and medical residents responded to preliminary questions regarding difficult conversations, listened to a brief discussion on difficult conversations; formed ad hoc teams and interacted with a standardized patient (mother) and a human simulator (child), discussing the infant's health issues, intimate partner violence, and suicidal thinking; and underwent debriefing.
Assessment
Participants evaluated the learning methods positively and a majority demonstrated knowledge gains. The project team also learned lessons that will help better design future programs, including an emphasis on simulations over lecture and the importance of debriefing on student learning. Drawbacks included the major time commitment for design and implementation, sustainability, and the lack of resources to replicate the program for all students.
Conclusion
Simulation is an effective technique to teach interprofessional teams how to engage in difficult conversations with patients.
Keywords: simulation, standardized patients, interprofessional teams, communication
INTRODUCTION
Graduates from health professional schools are expected to have competencies well beyond knowledge of drugs and diseases. A 2003 Institute of Medicine (IOM) report highlighted the need for health professional students to be educated to deliver patient-centered care, employ evidence-based practice, apply quality improvements, use informatics and practice in interdisciplinary teams as a way to improve patient safety.1 The 2007 Accreditation Council for Pharmacy Education (APCE) Accreditation Standards and Guidelines for the Professional Program in Pharmacy aligned the IOM report recommendations in terms of changes for pharmacy education.2 Specifically, the ACPE Standards state that graduates must be competent to deliver patient-centered care and to communicate and collaborate with patients, their caregivers, physicians, nurses, and other health care providers. Additionally, the Standards highlight the importance of students developing critical-thinking and problem-solving skills.
The Pharmaceutical Care section of the 2007 Center for the Advancement of Pharmaceutical Education (CAPE) Guidelines includes educational outcomes related to communication with patients, caregivers, and other health professionals. Specifically, the CAPE Guidelines state that students should develop competency in fostering collaborative relationships that embodies team-based care, demonstrates a caring and respectful attitude, and communicates information in a way that patients and healthcare professionals understand in order to communicate “clearly, accurately, compassionately, confidently, and persuasively.”3 The ACPE Standards encourage working with actual or simulated patients and health care professionals whenever possible during the instruction of effective communication skills.2
Simulation is an increasingly common part of pharmacy education, as evidenced by the number of articles in the Journal that describe the use of standardized patients and human simulators. Simulation is a broad term that includes computerized human models that replicate physiologic responses and disease states, live actors who role play during medical scenarios, and real health care providers who model positive and negative professional behavior in simulated learning environments. Simulation allows students to practice skills in a low-risk environment.4 Students interact with the simulators as they would with live patients, allowing them to practice and learn essential skills before caring for humans. Simulation allows students to develop competency in areas that may not be available consistently during advanced professional practice experiences (APPEs).5 It allows students to become more comfortable during difficult situations like dealing with angry patients, giving bad health news to patients, or asking patients personal questions. Interprofessional teams working together in simulated environments can learn about each other's scopes of practice and how to share information as they provide care for their patients. Simulation has been incorporated in professional practice laboratories and pharmacotherapy classes,6,7 and has been used to develop communication skills, physical assessment skills, and primary care skills; as an assessment at the end of an APPE; and to model interprofessional teams.8-11 Generally speaking, students like this form of education and describe improved knowledge and confidence in the area taught using simulation.
Fernandez used high fidelity simulators to teach hypertensive emergency care to teams of pharmacy students.12 Ninety percent of students stated that when compared to lectures, they learned clinical patient care better and 98% also found the course useful for their practice.
Westberg et al teamed pharmacy, medical, and nursing students to assess a standardized patient.4 Pre- and post-experience surveys found that students gained an appreciation for the others professions' patient care responsibilities and they also developed high-quality care plans.
Changes in pharmacy practice and health care as a whole, as outlined in the 2007-2008 Argus Commission Report and the Joint Commission of Pharmacy Practitioners 2015 Vision Statement, will result in deployment of pharmacists in even more direct patient care roles at a more personal level, increasing the need for pharmacists to conduct “difficult conversations” with patients.13,14 Even though simulation is discussed as an effective method for students to practice communication skills during difficult situations, there is little literature actually describing this process. Health professionals reported feeling better prepared and less anxious to initiate difficult conversations with patients and had a better understanding of patients, families, and the interprofessional team after participating in a 1-day workshop using standardized patients.15,16
The demonstration project described in this paper was undertaken to teach interprofessional team skills, with an emphasis on ad hoc teams. Ad hoc teams were defined as groups of professionals who come together, function as a team around a specific patient-care issue, and then disband. The project also taught interprofessional teams how to recognize challenging patient situations and engage in “difficult conversations.”
DESIGN
This demonstration project was designed in response to a 2007 request for proposals from the Association for Teaching Prevention and Research (ATPR), an organization focused on improving population health through promoting research in preventative medicine. ATPR also fosters interprofessional curriculum development for those disciplines engaged in disease prevention. ATPR funded teams of health professionals from health care systems and academic medical centers to attend the Institute for Interprofessional Prevention Education to refine their proposal on teaching disease prevention with experts in interprofessional education. ATPR also funded a subsequent project that resulted from the meeting. Social Sciences Institutional Review Board approval was obtained before the project was initiated.
Expected Outcomes and Learning Objectives
The project provided an opportunity for pharmacy students and residents, nursing students, and pediatric medical residents to learn, practice, and receive feedback on their skills in functioning in an ad hoc health care team and in engaging in difficult conversations with patients. The global outcomes included:
Educate healthcare providers to successfully assemble and function in an interprofessional ad hoc team.
Educate health care providers to identify and intervene in highly charged interpersonal situations such as difficult conversations.
Specific to this paper, upon completion of the program, participants were expected to be able to:
Identify areas of difficult conversations in patient care/professional practice.
Recognize signs and symptoms, diagnosis, treatment, and referral options for intimate partner violence.
Demonstrate competence while functioning as a member of an ad hoc interprofessional team engaged in difficult conversations.
The specific learning objectives were at the knowledge and application levels of Bloom's Taxonomy of Learning.
Educational Environment
Faculty members from the University of Missouri-Kansas City (UMKC) Schools of Pharmacy and Nursing and the Children's Mercy Hospital Emergency Department (CMH ED) designed the initial proposal. Once the project went into full development, the project team was expanded to include an additional CMH ED attending physician, 2 CMH ED nurses, the program director for the standardized patient program at the UMKC School of Medicine, and an intimate partner violence counselor from the Bridge program at Rose Brooks Center, a local domestic violence shelter. A social worker was available to assist students who were upset by the material covered during the difficult conversation portion of the program. The final project team represented the disciplines included on the interprofessional teams, content experts in the topics included in the difficult conversations, and the expertise needed to design and execute simulations using both high-fidelity human simulators and standardized patients.
The initial team attended the ATPR meeting in September 2007. A pre-pilot program was held in July 2008 to work out the timing and flow between didactic content and simulations and glitches in each scenario. The actual demonstration project was held over 2 evenings in September and October 2008. The project team met 2 to 4 times a month between the ATPR meeting and the demonstration in September 2008 to develop and refine the methodology and content.
Twelve volunteers participated in the project. They were recruited by e-mails sent to the target student population by their respective programs. Participants included 4 senior nursing students, 1 senior pharmacy student, 3 first-year pharmacy residents (PGY-1), 3 pediatric medical residents (PGY 1-3), and 1 pediatric emergency medicine fellow (PGY-4). Senior students/residents were solicited to avoid any negative impact on the learning caused by 1 discipline having significantly more clinical experience than another. Volunteers were awarded gift cards or earned clinical hours (nursing students) for their participation.
The project was completed in the jointly run UMKC School of Nursing/CMH Simulation Center. The center has several simulated medical/surgical patient rooms arranged around a classroom space and nurses' station. Two large rooms replicate an intensive care unit and emergency department trauma room. These rooms were equipped with beds, monitors, charts, resuscitation supplies, medication dosing guidelines, and mock medications. The rooms had windows to allow observers to watch and comment at a distance and not interfere with the scenario. S3010 Newborn HAL high fidelity human simulators (Gaumard Scientific, Miami, FL) were used during each simulation. The standardized patients were actors recruited from the UMKC School of Medicine Standardized Patient Program. Simulated charts were available for the child for hospital-based scenarios and for the mother and child for a scenario set in a family practice clinic. A faculty facilitator and team member who operated the simulator were present in each room during each simulation. Participants were allowed to ask the faculty facilitator questions. The simulation center's classroom was used for didactic sessions and large group debriefings. The overall goal was to provide a safe learning environment where students could give and receive feedback from peers and faculty members.
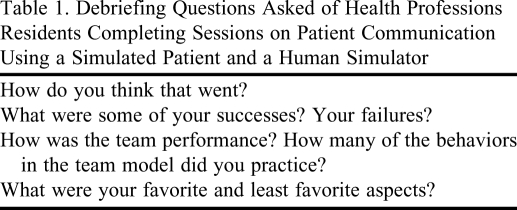
Pedagogy/Andragogy
The program was a mixture of teacher-focused and learner-focused activities. The teacher-focused activities were brief didactic sessions that provided content and a framework of understanding about scopes of practice and team functions (first night of program) and difficult conversations, intimate partner violence and suicide (second night of the program). The majority of time was spent in learner-focused activities where students independently completed brief readings and self-assessments before the 2 sessions, or observed or participated in scenarios. The debriefings that followed the scenarios allowed participants to actively share their feelings and reactions to the simulation in which they had just participated. The participants, under faculty guidance, reflected on their own experiences and learned from each other's experiences during these brief discussions. Table 1 lists the initial debriefing questions asked after the scenarios. More specific questions relating to individual scenarios were asked after the general questions. Students spent about 1 hour of preparation time before each class session. During the actual program, about 75% of the time was dedicated to scenarios or debriefings. The combination of a human simulator and a standardized patient was chosen to further enhance the authenticity of delivering care in a pediatric setting. Also, there was no literature found combining the use of these 2 modalities in simulation-based education, so the project was able to implement a novel approach to learning.
Table 1.
Debriefing Questions Asked of Health Professions Residents Completing Sessions on Patient Communication Using a Simulated Patient and a Human Simulator
Content
The program was delivered during two 4-hour sessions held 3 weeks apart. The first session focused on orientating the participants to the human simulator and standardized patients and learning about scopes of practice and ad hoc team function. The results of this session will be reported in a separate publication. The second night focused on ad hoc team function during difficult conversations.
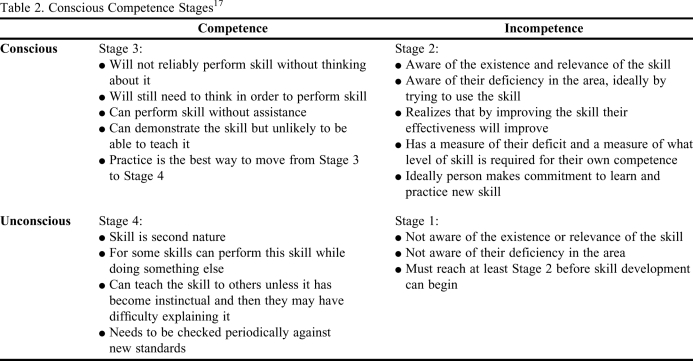
The Conscious Competence Learning Model and Matrix underpinned the projects' design and assessment methods. The model is most commonly applied in the business world and it describes how personal learning and change occurs. The model operates under the premise that people apply what they learn from training when they become aware that they need and can benefit from the training experience. As learners progress from stage to stage, they feel like the “lights came on” or some other feeling of awakening. In this learning model, the learners or trainees generally begin at Stage 1, “unconscious incompetent,” and pass through a series of stages with the goal to attain Stage 4, “unconscious competence.”17 Students used this matrix (Table 2) as the measure of their competence in various domains of engaging in difficult conversations with patients (Table 3). The goal was for participants to move forward at least 1 stage on the matrix. The project team felt this goal was achievable after a short training program and could also impart meaningful change for participants as they moved forward in their career.
Table 2.
Conscious Competence Stages17
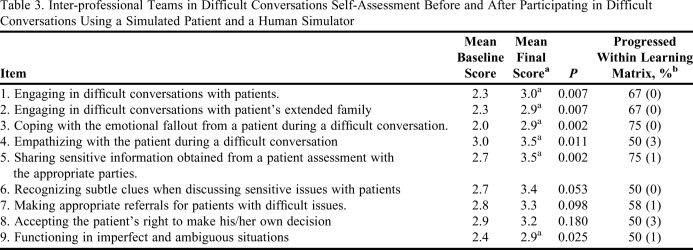
Table 3.
Inter-professional Teams in Difficult Conversations Self-Assessment Before and After Participating in Difficult Conversations Using a Simulated Patient and a Human Simulator
Rating scale used: 4 = I can perform this skill as second nature (automatically without thought or effort); 3 = I can perform this skill reliably and without assistance, but I have to think in order to do it; 2 = I am aware of the existence of this skill, but I am not effective in performing it; 1 = I am currently unaware of the existence of or relevance of this skill.
aSignificant change from pre-test to post-test as measured by Wilcoxan Signed Ranks Test
b % of total group that moved up one level on matrix (# rated 4 on pretest)
The scenarios were designed by the project team in consultation with the director of the standardized patient program. Each scenario incorporated an interprofessional team with 1 representative from each profession to treat the child and interact with the mother. Participants were not assigned specific responsibilities in caring for the child. They naturally assumed their roles within their own scopes of practice. Another interprofessional team observed the scenario through a window outside the treatment room. Team membership switched with each scenario in order to model ad hoc teams. By switching between participant and observer roles, students had different ways to learn and to contribute to the learning of others during debriefings. A human simulator (the child) and a standardized patient (the mother) were used to model a situation where a mother had a sick child who needed attention. The child was the presenting patient, whereas the mother exhibited the signs and symptoms of intimae partner violence or suicidal thinking, precipitating the difficult conversation. Although the standardized patient acting as the mother maintained the same role for all 3 scenarios, the health care setting in which she and her child were seen and the child's presenting problem changed with each scenario.
The program was as follows:
Physician-facilitator led a 20-minute discussion on difficult conversations, including specific examples and strategies to minimize discomfort and discord.
Scenario 1: Standardized mother and simulated baby. The child was being discharged from the hospital after a stay for respiratory illness. The discharge was delayed as the child had a new onset fever. The mother exhibited symptoms of intimate partner violence. Each health professional came into the room independently to work within their scope of practice for the discharge. They decided on their own whether to meet as a team or not prior to discharge.
Teams switched membership and roles (participant or observer).
Scenario #2: Same as Simulation #1 except the signs of intimate partner violence in the mother were more obvious. The mother pulled up her sleeves to show bruises on her arms. Her partner called and asked when she would be ready to leave. She was very distressed as she spoke to him on the phone.
Small and large group debriefings were conducted.
The Rose Brooks Center counselor provided information on intimate partner violence recognition and referral.
The pharmacist-facilitator led a 20-minute discussion on difficult conversations in the context of suicidal thinking.
Teams switched membership and roles (participant or observer).
Scenario #3: Mother and child were at their family medicine clinic getting follow-up after the baby's hospitalization. The baby had become ill again and might need to be re-hospitalized. Mom was stressed and intimated suicidal thinking. Each student worked within his/her scope of practice to care for the mother in a clinic setting. The participants decided on their own whether to meet and discuss her care as a team.
Small and large group debriefings were conducted.
Participants wrote at least 3 statements about difficult conversations, completed a self-assessment on difficult conversations, and evaluated the program.
This program used 5 of Issenberg's 10 features of effective learning18 in the methodology, including providing feedback (debriefing sessions), repetitive practice (students were involved with 6 scenarios over the 2 sessions and the roles played by the standardized mother and simulated child remained the same, just the setting in which they received care and the reason for the visit changed), multiple learning strategies (didactic and active learning), controlled environment (simulators, standardized patients and social workers), and defined outcomes.
EVALUATION AND ASSESSMENT
Evaluation Data
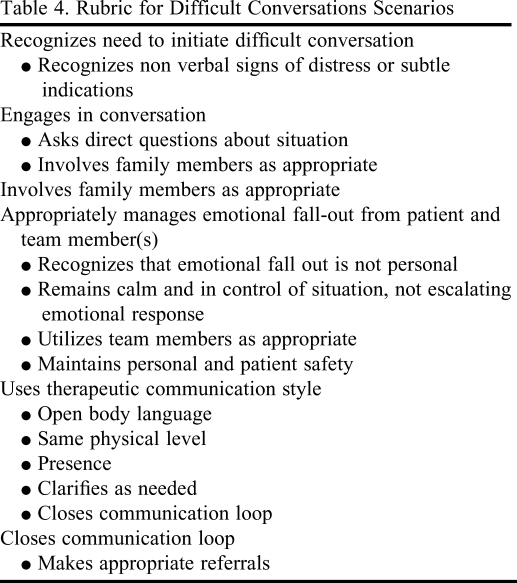
Participants completed the following activities outside of class before the first session: the Inter-professional Teams in Difficult Conversations Self-Assessment (Table 3) and the directed questions on past difficult conversations. The Self-Assessment was repeated at the end of the second session, before participants left the simulation center. They were also asked to write 3 statements that they believed about difficult conversations at the end of the second session. The accuracy of the 3 statements was determined by comparing them to the content delivered earlier in the evening by 1 of the faculty members. Students' performance within the actual simulations was assessed using a rubric completed by faculty observers (Table 4). Student satisfaction with the program was evaluated by a separate survey instrument administered at the end of the session (Table 5). Participants completed directed questions on difficult conversations before the program. Their responses were the basis for the program introduction. Students described a range of conversations that they found difficult. The most commonly cited difficult conversations were around death and dying. They also listed medical mistakes, team conflict, and patients questioning or refusing care as challenging. The participants felt helpless, sad or depressed, uneasy, stressed, and/or incompetent, but also sympathetic when they encountered these situations. Reasons included their own difficulty in admitting mistakes, difficulty dealing with their own emotions or the emotions of others, and the challenges of having to make decisions under time restraints. Finally, they said they would handle the situations by listening to the other party, encouraging patients to speak freely and ask questions, positioning themselves at the same physical level as the patient when speaking, consulting with the team, relying on previous experience, and offering comfort.
Table 4.
Rubric for Difficult Conversations Scenarios
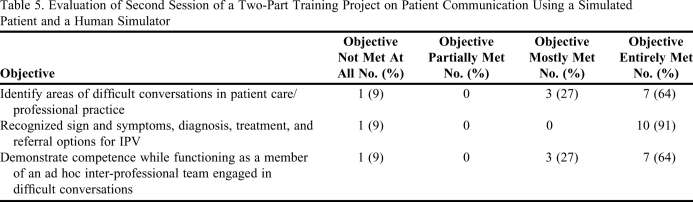
Table 5.
Evaluation of Second Session of a Two-Part Training Project on Patient Communication Using a Simulated Patient and a Human Simulator
The Wilcoxon signed rank test was used to compare whether a significant change occurred in the pre- and postintervention test or each question on the Inter-Professional Teams in Difficult Conversations Survey (Table 3). For all items, at least 50% of students moved 1 stage higher in the matrix. Increases in scores were found for all items, although the change was only significant for questions 1-5 and 9.
Although faculty members used a rubric (Table 4) to guide the debriefing and there was quantitative data on performance on the individual simulations, the survey had not been validated and interrater reliability training was not completed before the session, so the results were not reported. The majority of participants indicated that the program “mostly met” or “entirely met” the stated learning objectives (Table 5).
The 3 statements that students wrote about difficult conversations at the end of the program were reviewed by the faculty member who led that discussion. He rated the statements as accurate or not accurate relative to the content and discussion held during the didactic session. Nine of 11 (82%) students listed 3 accurate statements, 1 (9%) listed 2 accurate statements, 1 (9%) listed 1 accurate statement, and 1 did not provide any statements.
When evaluating the program, students said the course was thought provoking and led to self-reflection. They found debriefing to be a positive process and the feedback allowed them to see how to better approach patient situations similar to those in the scenarios in the future. They liked combining the standardized patient with the patient simulator as it helped them to realize that an encounter should not focus solely on the identified patient and that they needed to be sensitive to caregivers' needs as well. They liked the simulation laboratory facilities, the pacing of activities, and the opportunity to learn about each other's scopes of practice. They also felt they better understood what to do when confronted with difficult conversations. The Rose Brooks Center counselor, the realistic experiences, learning with other disciplines, and team building were all viewed favorably. Students expressed a desire to engage in additional simulation scenarios as they found them to be the most beneficial method of learning to communicate with patients and other health care providers.
DISCUSSION
This demonstration project was the first attempt for 3 programs within UMKC to partner in a program that teaches and assesses interprofessional skill development. The assessments were not designed to assign a grade or score, but to demonstrate whether participants improved their knowledge and advanced along the Conscious Competence Matrix. Assessment also included measures of student satisfaction with the experience and self-assessment as to whether students gained knowledge and experience about engaging in difficult conversations with patients. Overall, faculty members considered it to be a success because of the participants' favorable reaction and the many lessons they learned through the design and implementation of the program. The goal that all participants move up 1 level on the Conscious Competence Learning Matrix was not met, although improvement was seen in the majority of students. A portion of participants ranked themselves high at baseline, so movement up the scale was difficult. Since the main measure was self-rated as opposed to a more objective evaluation by a faculty member, it is unclear whether these students were competent at baseline or overestimated their ability. Future programs will include more content and experiences in the areas where students did not improve, such as recognizing subtle clues from patients when discussing challenging issues. The programming appeared to impart knowledge to the participants since at least half of the students improved their rating by 1 level on every question, 75% were able to state 3 accurate comments about difficult conversations, and the majority felt the program objectives were met. The results were encouraging as the students liked the teaching methods and learned new skills that they could not have achieved from lectures alone. The goal of the sessions was to provide an educational experience over and above what students received in their regular educational programs and that was achieved. Students usually do not gain experience with difficult conversations until they are faced with a real life situation. Using standardized patients and human simulators helped the students gain confidence and experience when the stakes were relatively low, unlike when they are working with an actual family who just received bad news about their loved one.
The drawbacks to this project were similar to those described in papers about other simulation projects in health care education.4,7,10,12 The first was the major time commitment required to design the program. Some of the project team had significant experience in using simulators for training within their own profession, but none in using simulators in an interprofessional environment. None of the core team had significant experience with using standardized patients, so outside expertise from the school of medicine's standardized patient program was brought in to design that part of the program.
Active-learning strategies were heavily emphasized because advanced level students were more likely to attain the program objectives by “doing” followed by reflection and feedback rather than by passive listening. Also the sessions were held in the evening after a full day of work, so active learning was essential to maintain the learner's attention. If this program were implemented on a broader scale, it likely would need to be offered in the daytime—a challenge given the conflicting schedules across the schools.
There was no existing model or theoretical framework on which to base the ad hoc team portion of the project. The project team spent many months reviewing the medical and business literature to find a theoretical framework for ad hoc team function in health care with limited success. Finally, after consulting with the project coordinators at ATPR, the Conscious Competence model was selected to show whether the content resulted in learning gains in awareness. The challenges in finding this model slowed down project implementation.
Another challenge was the cost and sustainability of the project. The project team participated out of personal interest and the substantial time commitment was in addition to their normal workload. In order for the project to be sustained, time allotted for interprofessional simulation education would have to be built into their ongoing responsibilities. The resources necessary to conduct this project with a full class of pharmacy, nursing, and medical students would be challenging to obtain, especially in the current economic climate, so the lessons learned from the project will be used to look at realistic ways to use simulation in interprofessional teams so more students can benefit.
Overall, the project was a success, as faculty gained experience in designing interprofessional educational programs using 2 types of simulation. Additionally, a new use for simulation showed promise as students gained confidence in dealing with “difficult patient situations” before they face them in real practice. Finally, the project brings the reality of implementing intensive active-learning strategies to the attention of the university administration who can determine where it fits as a priority within and across the health professional schools to identify resources to create a sustainable program.
SUMMARY
A demonstration project was designed to teach members of interprofessional teams how to better engage in difficult patient conversations regarding intimate partner violence and suicide. Scenarios using both human simulators and standardized patients provided an active-learning environment, and debriefing and self-reflection further enhanced the participants' skill development. The results were positive, as participants demonstrated both knowledge and skill enhancement using the assessment tools and they were satisfied with the program. The project team gained many valuable lessons in designing interprofessional educational programs using different simulation methods and also experienced some of the common challenges in using simulation as a teaching tool. The team will use these lessons as they move simulation-based education at UMKC into future student experiences.
ACKNOWLEDGEMENTS
The authors thank the following individuals for their aid in designing and executing the scenarios: Amy Altergott, RN, BSN, CPN, Coordinator, Center for Excellence in Pediatric Resuscitation; Gabriel Bailey, RN, BSN, Technical Coordinator, Center for Excellence in Pediatric Resuscitation; and Rochelle D. Wilson, MBA, Research Assistant, UMKC School of Nursing.
REFERENCES
- 1. Institute of Medicine of the national Academies. Quality Chasm Series. Health Professionals Education. A Bridge to Quality. Washington, DC: The National Academies Press; 2003, http://www.nap.edu/openbook.php?record_id=10681.
- 2. Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Programs in pharmacy Leading to the Doctor of Pharmacy Degree. Chicago, IL 2006. http://www.acpe-accredit.org/deans/standards.asp Accessed July 21, 2010.
- 3. American Association of Colleges of Pharmacy, Center for the Advancement of Pharmaceutical Education (CAPE), Advisory Panel on Educational Outcomes. Educational Outcomes, revised version 2004. http://www.aacp.org/resources/education/APPI/Pages/default.aspx. Accessed July 21, 2010.
- 4.Westberg SM, Adams J, Thiede K, Stratton TP, Bumgardner MA. An interprofessional activity using standardized patients. Am J Pharm Educ. 2006;70 doi: 10.5688/aj700234. Article 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lane JL, Slavin S, Ziv A. Simulation in medical education: a review. Simulation Gaming. 2001;32:297–314. [Google Scholar]
- 6.Austin Z, Gregory PAM. Evaluating the accuracy of pharmacy students self-assessment skills. Am J Pharm Educ. 2007;71(5) doi: 10.5688/aj710589. Article 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seybert AL, Kobulinsky LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Phar Educ. 2008;72(2) doi: 10.5688/aj720237. Article 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rickels NM, Tieu P, Myers L, Galal S, Chung V. The impact of a standardized patient program on student learning of communication skills. Am J Pharm Educ. 2009;73(1) doi: 10.5688/aj730104. Article 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Monaghan MS, Gardner SF, Schneider EF, Grady AR, McKay AB. Using standardized patients to teach physical assessment skills to pharmacists. Am J Pharm Educ. 1997;61(3):266–271. [Google Scholar]
- 10.Austin Z, Dolovich L, Lau E, et al. Teaching and assessing primary care skills: the family practice simulator model. Am J Pharm Educ. 2005;69(4) Article 68. [Google Scholar]
- 11.Weathermon RA, Erbele S, Marifan M. Use of standardized patients as an assessment tool at the end of an ambulatory care rotation. Am J Pharm Educ. 2000;64(2):109–113. [Google Scholar]
- 12.Fernandez R, Parker D, Kalus JS, Miller D, Compton S. Using a human patient simulation mannequin to teach interdisciplinary team skills to pharmacy students. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710351. Article 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wells BG, Beck DE, Draugalis JR, et al. Report of the 2007-2008 Argus Commission: What future awaits beyond pharmaceutical care? Am J Pharm Educ. 2008;72(Suppl) Article S8. [Google Scholar]
- 14. Future Vision of Pharmacy Practice, Joint Commission of Pharmacy Practitioners November 10, 2004; http://www.ascp.com/advocacy/coalitions/jcpp.cfm Accessed July 21, 2010.
- 15.Browning DM, Solomon MZ. Relational learning in pediatric palliative care: transformative education and the culture of medicine. Child Adolesc Psychiatr Clin N Am. 2006;15(3):795–815. doi: 10.1016/j.chc.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Browning DM, Meyer EC, Truong RD, Solomon MZ. Difficult conversations in health care: cultivating relational learning to address the hidden curriculum. Acad Med. 2007;82(9):905–13. doi: 10.1097/ACM.0b013e31812f77b9. [DOI] [PubMed] [Google Scholar]
- 17. Conscious competence learning model. http://www.businessballs.com/consciouscompetencelearningmodel.htm.
- 18.Issenberg SB, McGaghie WC, Petrusa ER, Gordon DL, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]