Abstract
Objective
To assess students' attitudes and confidence about type 2 diabetes mellitus and diabetes self-management education before and after participation in Living With Diabetes Week simulation.
Design
Third-year pharmacy students took part in diabetes lectures, interactive laboratory sessions, and a week-long simulation of life as a patient with diabetes in the Clinical Assessment course. Pre-/postintervention survey instruments and experimental and control group comparisons were completed assessing attitudes and confidence relating to knowledge about diabetes.
Assessment
The understanding that diabetes has a psychosocial impact, patient autonomy is necessary, and the seriousness of the disease increased. Students' confidence in their diabetes self-management education skills also increased.
Conclusion
The Living With Diabetes Week simulation changed pharmacy students' attitudes toward patients with diabetes and increased confidence in diabetes education skills.
Keywords: diabetes, attitude, assessment, simulation
INTRODUCTION
The American Diabetes Association recommends that patients with diabetes receive medical care from a physician-coordinated team, which often includes a pharmacist.1 This team should recognize diabetes self-management education as a critical component of diabetes care.1 Pharmacists can play an integral role in providing diabetes self-management education to patients. Adequate preparation and training of pharmacy students is critical to ensuring that patients receive optimal diabetes care.
A traditional diabetes curriculum consisting of lectures and laboratory sessions provides students with background knowledge and exposure to basic diabetes education skills. However, students may not fully comprehend the challenges that patients with diabetes face routinely, and they may not be confident in their skills to provide diabetes self-management education. Diabetes-related attitudes of health care professionals may be inappropriate and can lead to negative outcomes for patients.2 Therefore, it is important to foster positive attitudes toward caring for patients with diabetes and increase students' understanding of the impact of the disease on daily living.
This study consisted of incorporating a nontraditional component of a week-long simulation of living as a patient with type 2 diabetes into the traditional curriculum of the Clinical Assessment course at the South Carolina College of Pharmacy (SCCP). The Clinical Assessment course delivered to students in the third year of the doctor of pharmacy (PharmD) program was designed to provide interactive learning techniques to promote improved competencies. The curricular content of the course was based on the Center for the Advancement of Pharmacy Education (CAPE) outcomes, specifically including: providing patient-centered care, providing population-based care, and promotion of public health improvement.3 The diabetes segment of the course specifically sought to enable students to assess a patient's past and current medical history and variables to develop a pharmacotherapy regimen that is supported by evidenced-based goals, therapeutic endpoints, and therapeutic monitoring.4,5 The goal of implementing nontraditional instruction methods within the diabetes segment of the Clinical Assessment course was to influence students' attitudes toward caring for patients with diabetes and enhance understanding of the daily challenges patients with diabetes face. In addition, it was included to increase students' confidence in providing patients and caregivers diabetes self-management education, and understanding solutions for medication nonadherence.5,6 Furthermore, the nontraditional instruction methods support the Accreditation Council for Pharmacy Education (ACPE) Guidelines for the development of critical thinking and problem-solving skills through simulations and other practice-based exercises.7
Implementation of nontraditional diabetes curriculum using active learning and practice-based exercises improved pharmacy students' knowledge and skills in the management of diabetes.8-10 Most of the published literature highlights advanced diabetes care courses and training and certificate programs. These programs incorporated a diabetes simulation into their program, but they did not evaluate the impact of the simulation alone. In contrast to our project, which evaluated a single simulation in a required course and in a large sample of students, many of the publications assessing a nontraditional curriculum consisted of small sample sizes and optional enrollment in the programs.
In this study, the Living With Diabetes Week incorporated into a required course, Clinical Assessment, sought to integrate traditional and nontraditional active-learning techniques for diabetes education. All third-year pharmacy students participated in instructional methods of lecture and laboratory sessions. In addition to the traditional methods, an experimental group, including all pharmacy students on 1 campus, also participated in the intervention, which was the Living With Diabetes Week simulation. The objective of this project was to determine the change in students' attitudes about type 2 diabetes and impact on students' confidence in diabetes self-management education skills by integrating the intervention of a Living With Diabetes Week simulation into the curriculum. Study objectives were assessed using an anonymous online validated survey instrument.11
DESIGN
By incorporating lecture and active-learning techniques in the Living With Diabetes Week, students were exposed to various learning methods with an emphasis on a pedagogical curriculum.12 Students also self-reflected on the human dimension of diabetes as they lived with the disease for an entire week.13 Specific learning objectives of the Living With Diabetes Week included: (1) demonstrate specific diabetes self-management tasks (eg, insulin injection, carbohydrate counting); (2) understand the importance of goal-setting and patient autonomy in diabetes management; (3) appreciate the psychosocial impact of diabetes; (4) recognize the importance of training health care professionals in diabetes self-management education; (5) explain the seriousness of diabetes and its influence on daily lifestyle choices; and (6) understand the influence of tight glucose control and the medication and lifestyle factors that impact it. By attaining these learning objectives, the instructors anticipated that students' attitudes toward diabetes would be influenced and students' confidence in diabetes self-management education skills would increase.
SCCP encompasses 2 campuses (University of South Carolina campus in Columbia, SC, and Medical University of South Carolina campus in Charleston, SC), which offer the same curriculum on both campuses using distance education. The 2 groups of students on the 2 campuses are similar and served as the unblinded experimental and control groups for this study. The student group located on the USC campus were not able to participate in the Living With Diabetes simulation due to legal policies prohibiting self-injections on their campus; thus, they served as a control group. This control group was deemed an equal educational intervention as evidenced by similar student demographics, performance on diabetes examinations, and exposure to the same instructors and courses.
The Living With Diabetes Week was developed as part of the diabetes segment of the Clinical Assessment course that is a requirement in the spring of the third year of the PharmD program. Prior to the diabetes curriculum in this course, all students were provided lectures about diabetes mellitus in a separate course in the fall (pharmacotherapy series). The required traditional instructive and laboratory sessions in the Clinical Assessment course were delivered using distance education between the 2 campuses with both groups of students (experimental and control groups) participating. The laboratory exercises were identical but were taught separately on each campus. Both campuses incorporated faculty members who were certified diabetes educators for the laboratory instruction. Each site used a mix of full-time faculty members, pharmacy residents, and fourth-year pharmacy students to facilitate the stations and the objective structured learning experiences (OSLEs).
All third-year pharmacy students at SCCP were included (n = 187). One hundred-ten third-year pharmacy students on the USC campus participated in the traditional instructive lectures and the laboratory sessions only (no participation in the living with diabetes simulation); therefore, they served as the control group. Seventy-seven third-year pharmacy students on the MUSC campus participated in the lectures, the laboratory sessions, and the Living With Diabetes Week; therefore, they served as the experimental group. Institutional Review Board approval was obtained prior to implementation of the diabetes curriculum.
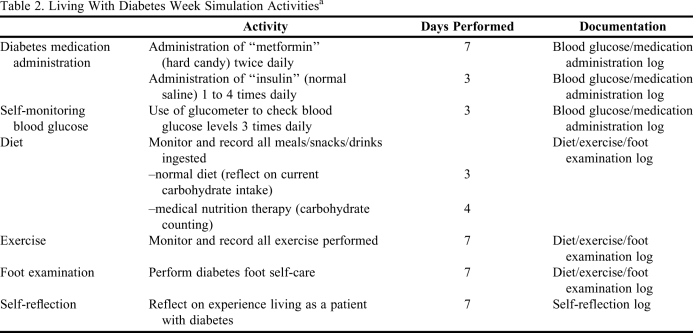
The activities in the diabetes segment of the Clinical Assessment course for all students on both campuses are highlighted in Table 1. In addition, students on the MUSC campus (experimental group) participated in the nontraditional Living With Diabetes Week which occurred at home between classroom and laboratory sessions. They performed common self-care tasks related to diabetes. All students in the experimental group were required to participate in the simulation and were provided with necessary instructions and supplies. In addition, the students were provided with a “diabetes diary” consisting of several logs to record when self-care tasks were performed. Students were asked also to reflect on their daily experiences including the human dimension of diabetes and its psychosocial impact and influence on daily life. Details of the Living With Diabetes Week are included in Table 2.
Table 1.
Diabetes Curriculum for a Clinical Assessment Coursea
Duration: 14 days including weekends.
bSee Table 2 for details of the intervention.
Table 2.
Living With Diabetes Week Simulation Activitiesa
Experimental group (MUSC students) participated in the intervention; control group (USC students) did not participate in these activities due to campus policies.
EVALUATION AND ASSESSMENT
Students' attitudes regarding diabetes and their confidence in diabetes self-management education skills were assessed using a 40-item anonymous survey instrument administered through SurveyMonkey (SurveyMonkey, Inc, Palo Alto, CA). The first 33 questions of the survey instrument consisted of the Diabetes Attitude Scale (DAS-3) (Michigan Diabetes Research and Training Center, Ann Arbor, MI), 11 and the final 7 questions assessed confidence in diabetes education skills. Students answered survey questions using a 5-point Likert scale with 1 = strongly agree to 5 = strongly disagree. The DAS-3 is a validated assessment tool that can be used as a general measure of diabetes-related attitudes of health care workers and patients, and is suitable for the evaluation of professional education programs. The DAS-3 is the most appropriate instrument to measure directly the attitudes toward diabetes. Questions on the DAS-3 fall into 5 distinct subscales and measure the following attitudes: need for special training to provide diabetes care; seriousness of type 2 diabetes; value of tight glucose control; psychosocial impact of diabetes; and patient autonomy. The subscales measured on the DAS-3 directly correspond to the specific learning objectives of the Living With Diabetes Week.
To strengthen the results, the Living With Diabetes Week simulation was assessed in 2 ways. First, the survey instrument was administered to students in the experimental group prior to the start of the 2-week diabetes segment (preintervention), and the same survey instrument was administered again within 7 days after completion of the diabetes segment and the Living With Diabetes Week simulation (postintervention). Furthermore, the postintervention survey instrument completed by the experimental group was compared with survey results of students in the control group who did not participate in the Living With Diabetes Week simulation. The survey instrument was administered to students in the control group during the same timeframe as the postintervention survey instrument.
The Living With Diabetes Week intervention had 2 study objectives that were assessed using 2 study groups (preintervention vs. postintervention and experimental group vs. control group). The change in students' attitudes toward patients with diabetes was the primary objective measured. The secondary objective measured was the change in students' confidence in diabetes self-management education skills.
Statistical analysis was performed using Statistical Analysis Software 9.0 (SAS Institute Inc, Cary, NC). Students completing more than half of the survey instrument were included in the analysis. Preintervention and postintervention survey results were analyzed using a dependent student t test. The second statistical analysis comparing the experimental and control groups was performed using an independent student t test.
Preintervention vs. Postintervention Analysis
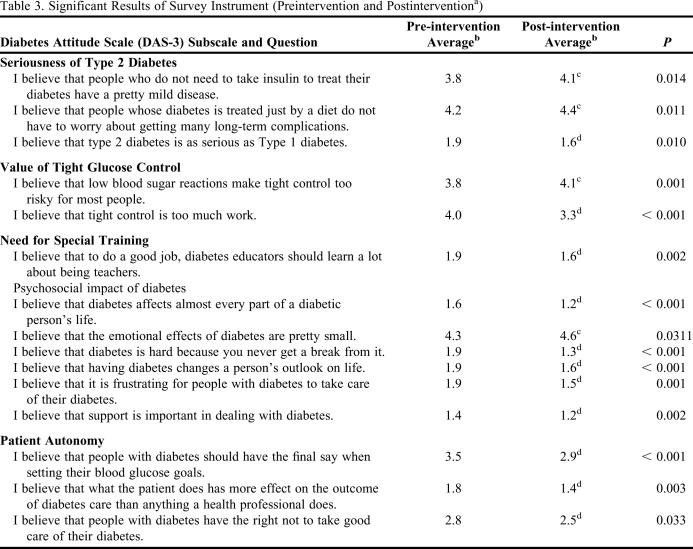
Of the 77 students included in the experimental group, 65 completed more than half of both survey instruments and were included in the data analysis, representing an 84% response rate. There was a significant difference in responses to 16 of the 33 questions representing the DAS-3 portion of the survey instrument (Table 3) and all 7 of the questions assessing students' confidence in diabetes education skills.
Table 3.
Significant Results of Survey Instrument (Preintervention and Postinterventiona)
Results only reported for DAS-3 questions; all questions regarding student confidence were significant (see text for details).
bResponses based on the following scale: 1 = strongly agree, 2 = agree, 3 = neutral, 4 = disagree, 5 = strongly disagree.
cFor this item, higher score favored using an intervention.
dFor this item, lower score favored using an intervention.
The majority of the differences found on the DAS-3 portion of the survey results involved attitudes related to the psychosocial impact of diabetes and belief in patient autonomy regarding management of their disease state. There was a significant difference on all questions involving the psychosocial impact of diabetes. The results of the postintervention survey instrument revealed that students' confidence in diabetes education skills increased. Students' confidence significantly increased in response to all 7 questions. The greatest increase occurred regarding confidence in glucometer use and counseling patients on diabetes medications, including how to administer insulin, after students completed the Living With Diabetes simulation (all p values < 0.001).
The written comments in the self-reflection logs reported similar changes in attitudes regarding diabetes as those found on the survey results. In addition, students also reflected on increased confidence in their diabetes self-management education skills because they had experience “living with the disease.” The majority of students' comments involved a greater appreciation of how difficult and demanding it was to be a patient with diabetes.
Experimental vs. Control Group Analysis
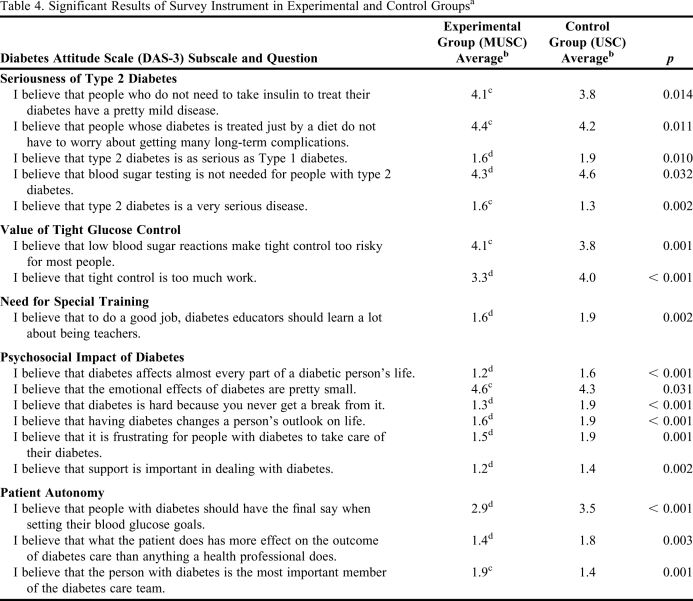
Of the 77 students included in the experimental group, 68 completed more than half of the postintervention survey instrument and were included in the data analysis. This represented an 88% response rate. Of the 110 students included in the control group (USC campus), 57 completed more than half of the postintervention survey instrument and were included in the data analysis, representing a 52% response rate. There was a significant difference between the groups in responses to 17 of the 33 questions representing the DAS-3 portion of the survey results (Table 4) and all of the questions assessing students' confidence in diabetes self-management education skills.
Table 4.
Significant Results of Survey Instrument in Experimental and Control Groupsa
Results only reported for DAS-3 questions; all questions regarding student confidence were significant (see text for details).
b1 = strongly agree, 2 = agree, 3 = neutral, 4 = disagree, 5 = strongly disagree
cFor this item, higher score favored using an intervention.
dFor this item, lower score favored using an intervention.
The majority of the differences in responses to the DAS-3 portion of the survey involved changes in attitudes about the psychosocial impact of diabetes, the seriousness of diabetes, and the belief in patient autonomy regarding management of their disease state. Similar to the preintervention and postintervention analysis, there was a significant difference on all questions involving the psychosocial impact of diabetes. A greater percentage of students in the experimental group had confidence in all of the aspects of diabetes education skills assessed. The greatest difference in confidence occurred regarding making recommendations to other health care providers about diabetes management (p < 0.0001), using a blood glucose diary to make recommendations for changes in diabetes medication management (p = 0.002), and in the overall ability to provide appropriate education to patients with diabetes (p = 0.0003).
DISCUSSION
This study demonstrated that including the Living With Diabetes Week simulation within a traditional diabetes curriculum changed students' attitudes regarding diabetes and improved students' confidence in diabetes self-management education skills. Therefore, this study adds to the evidence that nontraditional diabetes education is important to ensure that pharmacy students are adequately prepared to provide diabetes patient care and education. In addition, this study demonstrated that a nontraditional activity like the Living With Diabetes simulation can have positive influence on students' attitudes related to diabetes and increase their understanding of the challenges patients with the disease face daily. This study may impact colleges and schools of pharmacy curriculum, and implementation of similar programs should be considered.
Limited studies have reported that a nontraditional diabetes curriculum can benefit pharmacy students.8-10 These complex programs involving role-playing as a patient with diabetes have demonstrated positive effects. Only 1 other study has published findings specific to a living with diabetes simulation/role-playing experience; however, this was using a type 1 diabetes regimen.14 The majority of previous studies involved elective courses that included limited numbers of students, involved multiple exercises, and did not address specifically the “living with diabetes” exercise. In contrast to these previous studies reported in the literature, this study involved the assessment of the Living With Diabetes Week simulation alone rather than as part of a larger program.
A strength of this study was the use of a validated survey instrument to determine changes in students' attitudes. Using this survey instrument is a summative approach to attitudinal assessment and is reported in the literature as the gold standard of diabetes attitude data collection. Overall, a large number of students were included in this study and student survey response rates were high, thereby increasing the representativeness of the survey results. This study also adds to the body of literature because outcomes were compared in 2 ways and showed similar positive results, both within the experimental group (pre-/postintervention), and between the experimental and the control group. In addition, the simulation was incorporated into a required course that was delivered via distance education on 2 campuses, thus representing a design strength because other reports of similar activities were offered only in elective courses where the positive impact on students was limited. Furthermore, institutions may be able to implement more easily a Living With Diabetes Week simulation within the traditional diabetes education curriculum rather than implementing a more complex diabetes elective course, thereby benefitting more students. Our results demonstrate that this simple diabetes simulation is effective in changing students' attitudes and improving confidence related to diabetes. Prior to implementation, institutions should verify with administrators the availability of diabetes supplies and compliance with university policies and procedures for injections, (for example student self-injections were allowed on the MUSC campus; however, some universities require a signed consent form).
While our study has many strengths and adds to the literature by differing from or expanding on outcomes previously reported, it is not without limitations. While all students in the experimental group were expected to participate, compliance with the simulation activities was not formally assessed. The study design included a control group defined by campus location, which may be a limitation because the students were not randomized. However, in a required course, a randomized control study is difficult because students need similar experiences on all campuses. In addition, the survey instrument was not administered to students in the control group prior to the diabetes lecture/laboratory sessions; this group is assumed to have similar baseline survey results as the experimental group. The lower response rate of the students in the control group may have influenced the results. The timing of administering the survey instruments may also be a limitation, as the long-term effects of the Living With Diabetes Week simulation on students' attitudes and confidence towards diabetes cannot be assessed. Although the majority of the survey results are significant, determining the educational significance is difficult. Furthermore, we did not collect outcomes related to actual student knowledge and behavior in delivering diabetes education, although this was not the objective of this study. Fortunately, reinforcement typically occurs during advanced pharmacy practice experiences. Collecting these outcomes will be important and future assessment may be warranted.
SUMMARY
This study involved including a week-long simulation of living the life of a patient with type 2 diabetes within a traditional diabetes curriculum with the goal of changing students' attitudes toward diabetes and increasing confidence in diabetes self-management education. Pre-/postintervention, experimental, and control groups were used to assess students' attitudes related to diabetes. Implementation of the Living With Diabetes Week simulation changed pharmacy students' attitudes toward patients with diabetes. Specifically, it increased pharmacy students' beliefs in the psychosocial impact of diabetes, and the belief that patients with diabetes should have autonomy regarding treatment of their disease state. Furthermore, implementation of the Living With Diabetes Week simulation increased pharmacy students' confidence in diabetes self-management education skills.
ACKNOWLEDGEMENTS
We would like to thank Maryann Delea and Dristin Delea for their input into the publication of this manuscript.
REFERENCES
- 1.American Diabetes Association. Standards of medical care in diabetes-2009. Diabetes Care. 2009;32(Supp1):S13–S49. [Google Scholar]
- 2.Department of Health. Report of the National Commission on Diabetes to Congress of the United States. Vol. 3, Part 5. Washington, DC: US Government Printing Office; 1975. Education, and Welfare. NIH publication 76-1024;5-13. [Google Scholar]
- 3. American Association of Colleges of Pharmacy, Center for the Advancement of Pharmaceutical Education. http://accp.org/resources/education/Pages/ CAPEEducationalOutcomes.aspx. Accessed June 30, 2010.
- 4. American Association of Colleges of Pharmacy, Center for the Advancement of Pharmaceutical Education. Anatomy, physiology, and pathophysiology supplemental educational outcomes based on CAPE 2004. http://www.aacp.org/resources/education/Documents/anatomyphysiologypathophysiologyDEC06.pdf. Accessed June 30, 2010.
- 5. American Association of Colleges of Pharmacy, Center for the Advancement of Pharmaceutical Education. Pharmacy practice supplemental educational outcomes based on CAPE 2004. http://www.aacp.org/resources/education/Documents/PharmacyPracticeDEC006.pdf. Accessed June 30, 2010.
- 6. American Association of Colleges of Pharmacy, Center for the Advancement of Pharmaceutical Education. Social and administrative sciences supplemental educational outcomes based on CAPE 2004. http://www.aacp.org/resources/education/Documents/SocialandAdminDEC06.pdf. Accessed June 30, 2010.
- 7. Accreditation Council for Pharmacy Education. Accreditation standards. http://www.acpe-acredit.org/deans/standards.asp. Accessed June 30, 2010.
- 8.Johnson JF, Chesnut RJ, Tice BP. An advanced diabetes care course as a component of a diabetes concentration. Am J Pharm Educ. 2003;67(1) Article 21. [Google Scholar]
- 9.Odegard PS, LaVigne LL, Ellsworth A. A diabetes education program for pharmacy students. Am J Pharm Educ. 2002;66(4):391–395. [Google Scholar]
- 10.Ryan GJ, Foster KT, Unterwagner W, Jia H. Impact of a diabetes certificate program on PharmD students' knowledge and skills. Am J Pharm Educ. 2007;71(5) doi: 10.5688/aj710584. Article 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson RM, Fitzgerald JT, Funnell MM, Gruppen LD. The third version of the diabetes attitude scale. Diabetes Care. 1998;21(9):1403–1407. doi: 10.2337/diacare.21.9.1403. [DOI] [PubMed] [Google Scholar]
- 12.Hailikari T, Katajavouri N, Lindblom-Ylanee S. The relevance of prior knowledge in learning and instructional design. Am J Pharm Educ. 2008;72(5) doi: 10.5688/aj7205113. Article 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Conner ML. Andragogy and pedagogy. Ageless Learner, 1997-2004. http://agelesslearner.com/introsandragogy.html. Accessed June 30, 2010.
- 14.Westburg SM, Bumgardner MA, Brown MC, Frueh J. Impact of an elective diabetes course on student pharmacists' skills and attitudes. Am J Pharm Educ. 2010;74(3) doi: 10.5688/aj740349. Article 49. [DOI] [PMC free article] [PubMed] [Google Scholar]