Abstract
A neuropsychiatric study of individuals who underwent successful liver transplantation an average of 3 years previously was conducted to assess quality of life in terms of cognitive capacity and psychiatric status, as well as social and behavioral functioning. Compared with a control group of patients with Crohn’s disease, liver transplant patients did not differ on measures of intelligence, language, attention, concentration, spatial organization, memory, or learning. Performance on these diverse aspects of cognitive functioning was in the normal ranges for both groups when compared with normative or standardized test values. The control and liver transplant patients were not different from each other on measures of psychiatric status or social functioning; however, both groups exhibited some disruption of functioning in these two areas when contrasted with normative values. We conclude that relatively young individuals (mean age in this study, 27.8 years) do not exhibit debilitating long-term neuropsychiatric disability after liver transplantation, although some disturbance in social and psychiatric adjustment was observed.
Although liver transplantation is conducted in certain advanced chronic hepatic diseases that are refractory to all other medical interventions, there have been no follow-up investigations of the neuropsychiatric status of patients after successful transplantation. This lack of information is particularly disturbing because encephalopathy is a frequent sequela of chronic liver disease and is present in most liver transplant candidates. It is important, therefore, to determine whether liver transplantation, in addition to being a life-saving procedure, also can restore the individual to a normal quality of life in terms of social and behavioral functioning, emotional well-being, and cognitive capacity. Stated differently, it is critical to determine whether hepatic encephalopathy is fully reversible after successful liver transplantation.
There are several obvious reasons for conducting a comprehensive neuropsychiatric evaluation of patients after successful liver transplantation. Psychometric tests are able to detect the presence of cerebral dysfunction in the absence of overt clinical signs of encephalopathy.1 Moreover, these tests are known to be more sensitive indicators of central nervous system pathologic conditions than the electroencephalogram.2 In addition, certain neuropsychological indices are predictors of social and vocational adjustment, and thus can be used to either counsel or direct rehabilitation efforts after transplantation.3,4 Furthermore, behavioral, psychiatric, and emotional disturbances are common in prospective transplant patients with advanced liver disease, many of whom have hepatic encephalopathy. Because these latter disturbances can negatively influence the individual’s capacity to function behaviorally, as well as their social environment, the assessment of neuropsychiatric status after successful liver transplantation is of obvious importance in evaluating the holistic outcome of hepatic transplantation.
Methods
Patients
Ten patients who survived liver transplantation were compared with 10 control patients with established stable Crohn’s disease. The latter group was used for comparison to control for the nonspecific effects of chronic illness on the various test measures. The 10 transplant patients had had surgery an average of 36.30 months (SD = 42.19) before our evaluation. The average age and educational level was 27.80 (SD = 11.23) and 12.80 (SD = 2.62) years, respectively. None of the patients had a history of primary neurologic or psychiatric illness before the onset of liver disease. The duration of hepatic disease, measured as the time between first histopathologic diagnosis and date of transplantation, averaged 45.20 months (SD = 73.02).
The transplant patient group consisted of all individuals who came to Pittsburgh for annual postsurgical examination and agreed to submit to a comprehensive neuropsychiatric evaluation. No preselection criteria were utilized. Patients were consecutively admitted to this follow-up study as they became available. The small sample size is a result of the somewhat low long-term survival rate prior to the availability of the immunosuppressive drug cyclosporine, and the modest availability of persons who had undergone transplantation prior to 1981. Before transplantation, all patients had advanced liver disease; specifically, three each had primary biliary cirrhosis and postnecrotic cirrhosis, and one each had chronic active hepatitis, hepatoma, Wilson’s disease, and congenital hepatic fibrosis. No objective neuropsychiatric assessments were conducted prior to 1981, thereby preventing direct comparisons before and after surgery. However, latter conditions, particularly at or near the end stage, when the transplant is generally performed, are associated with significant neuropsychiatric disturbance consequential to chronic hepatic encephalopathy.
The patients with Crohn’s disease were all undergoing treatment at the time of this investigation, and disease activity level was stable. Average age and education level was 39.30 (s = 11.82) and 14.90 (s = 2.88) years, respectively. The duration of their illness, from the time of original diagnosis to the time of testing, averaged 63.56 months (SD = 73.02). As was the case for transplant patients, none of the patients with Crohn’s disease had a history of neurologic or psychiatric disturbance prior to their current illness. The patients with Crohn’s disease were chosen as controls, primarily because they had a gastrointestinal tract disease that is chronic in nature and can be debilitating during its active manifestations. For these reasons, although differing from transplant patients because Crohn’s disease is not life-threatening, their condition was sufficiency severe to enable evaluation of the nonspecific effects that a chronic illness exerts on neuropsychiatric status.
Procedures
Test Measures
A comprehensive neuropsychiatric examination, consisting of tests of cognitive or neuropsychological capacity, psychiatric illness, and personality and social adjustment, was conducted on each patient. The neuropsychological battery was comprised of tests of intelligence, attention, learning, memory, psychomotor skills, language, and perceptual-spatial ability. The specific tests are listed in Table I, and discussions of their reliability, validity, standardization, and scoring criteria can be found in standard reference texts.5,6
Table 1.
Neuropsychological measures from tests on transplant patients and patients with Crohn’s disease
| Capacity/measure | Transplant patients |
Crohn’s disease |
Normal value | ||
|---|---|---|---|---|---|
| X̄ | SD | X̄ | SD | ≥ | |
| Verbal intelligence (IQ) | |||||
| Peabody Picture Vocabulary test | 96.00 | 15.91 | 99.00 | 15.81 | 100 |
| Nonverbal intelligence (IQ) | |||||
| Raven’s Progressive Matrices | 113.38 | 9.78 | 113.50 | 13.21 | 100 |
| Attention and concentration | |||||
| Digit span forward | 6.90 | 1.29 | 7.22 | 0.97 | 7 |
| Digit span backward | 4.80 | 1.03 | 4.78 | 1.30 | 5 |
| Mental control | 7.90 | 1.10 | 7.90 | 0.99 | 8 |
| Learning and memory | |||||
| Logical memory (immediate) | 17.11 | 8.22 | 19.40 | 6.65 | 18 |
| Logical memory (delayed) | 13.44 | 6.73 | 13.10 | 6.40 | 13 |
| Figural memory (immediate) | 11.20 | 2.97 | 10.40 | 2.76 | 11 |
| Figural memory (delayed) | 12.30 | 2.16 | 10.40 | 3.89 | 10 |
| Paired associates (immediate) | 25.90 | 3.51 | 17.75 | 2.06 | 18 |
| Paired associates (delayed) | 9.50 | 0.71 | 9.20 | 1.14 | 9 |
| Supraspan (digit span + 1)* | 2.60 | 1.35 | 2.22 | 1.72 | 2 |
| Perceptual-motor | |||||
| Finger tapping | 97.30 | 14.03 | 81.80 | 12.71 | 95 |
| Purdue pegboard | 38.20 | 5.86 | 29.22 | 2.95 | 38 |
| Star tracing—time | 36.20 | 9.59 | 43.90 | 25.02 | 36 |
| —errors* | 4.30 | 4.86 | 1.30 | 1.49 | 2 |
| Symbol Digit Modalities | 46.60 | 10.93 | 53.50 | 6.45 | 53 |
| Spatial | |||||
| Block design | 20.20 | 3.97 | 21.30 | 5.87 | 21 |
| Tactual performance—seconds | 838.22 | 296.65 | 835.40 | 297.01 | 900 |
| —memory | 7.78 | 1.09 | 7.70 | 1.49 | 7 |
| —location | 4.11 | 2.89 | 4.90 | 2.28 | 4 |
| Trailmaking test* | 113.38 | 47.98 | 88.67 | 46.79 | 130 |
| Language | |||||
| Boston Diagnostic Aphasia examination | |||||
| Fluency | 22.40 | 5.25 | 23.80 | 5.98 | 20 |
| Confrontation naming | 104.70 | 0.95 | 103.70 | 1.70 | 105 |
| Responsive naming | 30.00 | 0.00 | 29.90 | 0.32 | 30 |
| Token test | 11.90 | 1.85 | 12.30 | 0.82 | 10 |
Higher score indicates poorer performance.
Personality and psychopathologic characteristics were evaluated with the MMPI and the 16PF. The MMPI is a 566-item true-false questionnaire that contains 10 clinical scales and three validity scales.7 The clinical scales are hypochondriasis (Hs), depression (D), hysteria (Hy), psychopathic-deviate (Pd), masculinity-femininity interests (Mf), paranoia (Pa), psychasthenia (Pt), schizophrenia (Sc), mania (Ma), and social introversion (Si). The validity scales assess the attitudinal bias of the person answering the questions and, in so doing, determine if the person is answering deceptively (L scale), emphasizing negative aspects of their current emotional state (F scale), or stressing only the positive aspects of their present state (K scale).
The 16PF, consisting of 266 items, was designed to evaluate personality in persons who are not suffering from a pronounced psychiatric disorder.8 Unlike the MMPI, the 16PF is concerned with assessing normal personality functioning, although a marked deviation from normality, if obtained on any scale, may indicate important maladjustment. The 16 bipolar personality dimensions assessed with this instrument are: reserved/outgoing, less intelligent/more intelligent, affected by feelings/stable, humble/assertive, sober/happy-go-lucky, expedient/conscientious, shy/venturesome, tough minded/tender minded, trusting/suspicious, practical/imaginative, forthright/astute, self-assured/apprehensive, conservative/experimenting, group dependent/self-sufficient, self-conflict/controlled, and relaxed/tense.
The effects of illness on the individual’s capacity to perform everyday activities was assessed with the Sickness Impact Profile.9 This self-report scale quantifies impairment in social interaction, ambulation, sleep and rest, eating, work, home management, mobility, body care and movement, communication, recreation and pastimes, alertness, and emotional behavior. Physical dysfunction, psychosocial dysfunction, and total dysfunction scores also are obtained.
Statistical analysis
The liver transplant and control groups were compared with each other across each measure using Student’s t test for independent samples. This comparison determines if patients who underwent liver transplantation are distinguishable in terms of their cognitive, psychiatric, and social functioning abilities from patients who have a chronic illness that is not known to be associated with primary neurological sequelae and who have not undergone transplant surgery. A p value of <0.05 was considered significant.
Results
The results of the neuropsychological tests are presented in Table I. The two groups did not differ from each other on measures of verbal and nonverbal intelligence (Peabody Picture Vocabulary Test and Raven’s Progressive Matrices, respectively). However, the transplant patients were significantly better at learning the associations on a 10-item list of word pairs than were the patients with Crohn’s disease (t = 6.736, P < 0.001). Recall accuracy of the word pair associations tested one-half hour later was the same for both groups. Similarly, on two of the perceptual-motor tests, the transplant patients performed significantly better than did the control group of patients with Crohn’s disease. The transplant patients exhibited faster finger-tapping speed than did the control patients (t = 2.592, p < 0.01). The transplant patients also performed better than the medical controls in perceptual-motor speed, as measured by the Purdue Pegboard (t = 4.34, p < 0.001).
In contrast, the two groups did not differ in attention and concentration capacities. The transplant patients could repeat strings of digits both in a forward and backward sequence, recite the alphabet, perform serial additions, and count backward as competently and as rapidly as the controls with Crohn’s disease. Similarly, immediate and delayed recall of verbal passages (logical memory) and pictorial figures (figural memory) did not differentiate the two groups. On another test of learning ability, the supraspan digit test, there was no difference between the two groups in the number of trials it took to learn a sequence of digits that exceeded their digit span by one number.
No differences between groups were noted on the Star Drawing Test, another perceptual-motor test. The transplantation patients and controls performed comparably on the time it took to draw a line along the one-quarter inch boundary; the number of errors committed completing the task was also comparable. In addition, no group differences were observed in the ability to sequentially match symbols with numbers of the Symbol Digit Modalities Test.
Tests of spatial organization also failed to discriminate between the two groups. Specifically, no differences were noted either in their ability to copy patterns with blocks on the Block Design Test, or in their ability, when blindfolded, to rapidly place geometric blocks in a formboard, as measured by the Tactual Performance Test. In addition, the groups did not differ in recall of the number of block shapes and their location on the formboard after the task was completed.
Language capacities, measured by subtests of the Boston Diagnostic Aphasia Examination, were almost identical in the transplant patients and controls. Confrontation naming, requiring the naming of common objects, and responsive naming, involving answering a variety of questions, were similar in the two groups. The two groups also did not differ in the ability to repeat simple or complex phrases after the examiner. Fluency, or speed of verbal output, also was not different in the two groups. Moreover, comprehension was the same for both groups, as measured by the Token Test.
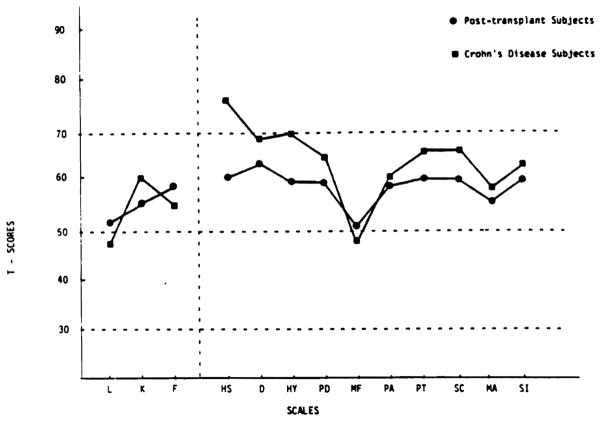
The MMPI profiles for the transplant patients and controls are presented in Fig. 1. Comparisons between the two groups revealed a significant difference only on the hypochondriasis scale (t = 2.67, p < 0.01); patients with Crohn’s disease scored in the more pathologic direction.
Fig. 1.
MMPI profiles of liver transplant patients and patients with Crohn’s disease. The population norm is 50, and a score > 70 is pathognomonic.
The profiles for the transplant patients and the medical control group from the 16PF are presented in Fig. 2. The two groups were not significantly different on any of the personality scales.
Fig. 2.
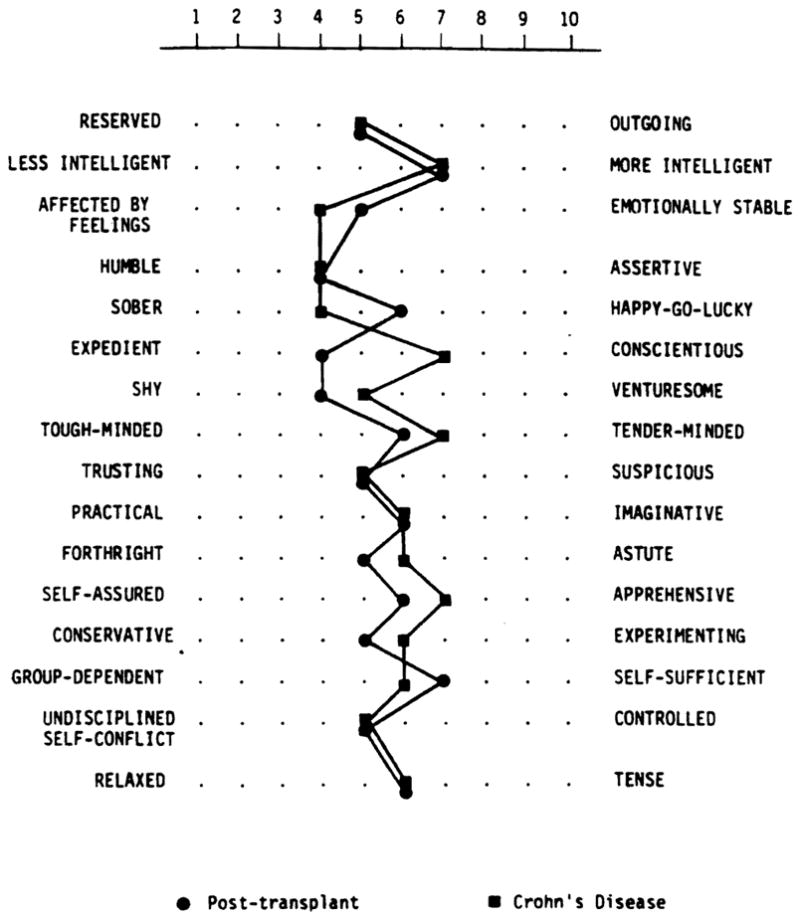
The 16PF profiles of liver transplant patients and patients with Crohn’s disease. A score of 5 is the population mean for each of the personality traits.
The Sickness Impact Profiles for both groups are presented in Fig. 3. None of the scales discriminated between transplant patients and patients with Crohn’s disease.
Fig. 3.
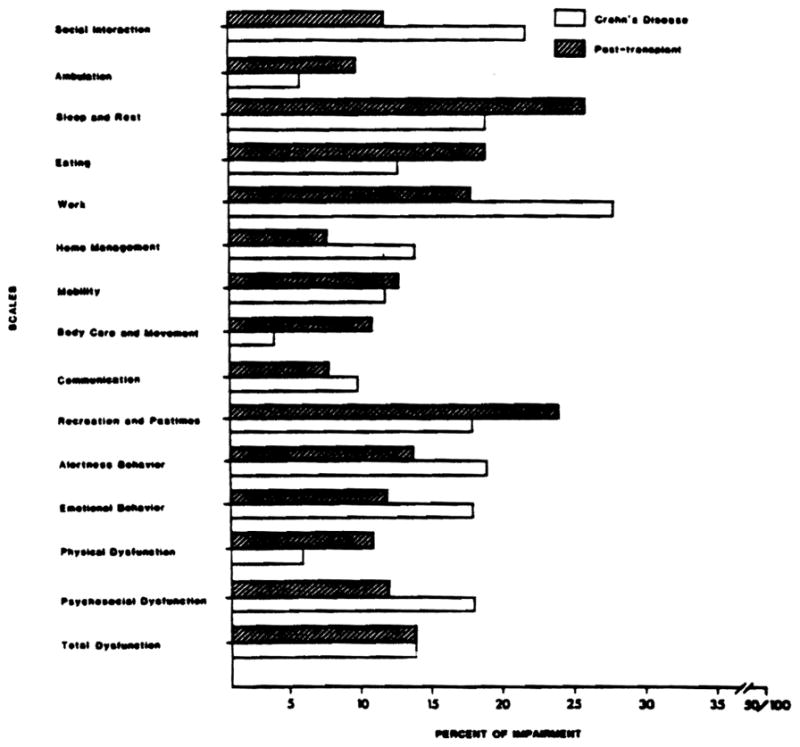
Sickness Impact Profiles of liver transplant patients and patients with Crohn’s disease. The higher the score, the greater the impact of illness on daily functioning.
Discussion
The results of this investigation indicate that patients who survived liver transplantation an average of 3 years are not impaired on measures of neuropsychological capacity when compared either with a control group with a chronic disease or with population norms. On measures of psychiatric status and social functioning, they also were not substantially different from the control group; however, when contrasted with normative population values, the transplant patients presented a profile of moderate anxiety, somatic distress and concern, frustration, depression, worry, and social withdrawal. Routines of everyday living also are somewhat disrupted, as indicated by the finding that their condition negatively affects sleep and rest, eating and appetite, work capacity, and recreation and pastimes. Impairments of ≥20% were observed in each of these scales, when a score at or near 0% would be normal.
This investigation, the first examination of neuropsychiatric status of patients who have undergone successful liver transplantation, indicates that the long-term prognosis, at least for young adults, is positive. Whether neuropsychiatric disturbances would persist in older individuals cannot be determined from our data, although findings on the relationship between age and the reversibility of encephalopathy, reported by Victor et al.,10 suggests that this may be the case.
Also, it should be pointed out that the control group was on average approximately 7 years older than the transplant group, a factor that certainly could have obscured the results of the neuropsychological assessment and contributed to the superior performance of the transplant patients on three of the cognitive tests. Thus, the generally good neuropsychiatric outcome of the transplant patients may be attributable, in part, to the youth of the sample. Additional research, utilizing a larger sample and encompassing a wider age range, needs to be conducted before definitive conclusions can be drawn regarding the long-term neuropsychiatric outcome of liver transplantation.
Acknowledgments
Supported in part by Grant RO1 AM32556-01 from the National Institutes of Health, and by a grant from the Gastroenterological Medical Research Foundation of Southwestern Pennsylvania.
Abbreviations
- MMPI
Minnesota Multiphasic Personality Inventory
- 16PF
Sixteen Personality Factors Questionnaire
References
- 1.Gilberstadt S, Gilberstadt H, Zieve L, et al. Psychomotor performance deficits in cirrhotic patients without overt encephalopathy. Ann Int Med. 1950;140:519–521. [PubMed] [Google Scholar]
- 2.Rikkers L, Jenko P, Rudman D, Freides D. Subclinical hepatic encephalopathy: Detection, prevalence and relationship to nitrogen metabolism. Gastroenterology. 1978;75:462–469. [PubMed] [Google Scholar]
- 3.Meaton R, Chalune G, Lehman R. Using neuropsychological and personality tests to assess the likelihood of patient employment. J Nerv Ment Dis. 1978;166:408–416. doi: 10.1097/00005053-197806000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Diller L, Gordon W. Rehabilitation and clinical neuropsychology. In: Filskov S, Boll T, editors. Handbook of clinical neuropsychology. New York: John Wiley & Sons Inc; 1981. pp. 702–733. [Google Scholar]
- 5.Buros O. The seventh mental measurements yearbook. Highland Park, NJ: Gryphon Editions Ltd; 1972. [Google Scholar]
- 6.Lezak M. Neuropsychological assessment. New York: Churchill-Livingstone Inc; 1978. [Google Scholar]
- 7.Dahlstrom W, Welsh G, Dalhstrom L. An MMPI handbook: Research applications. Minneapolis: University of Minnesota Press; 1975. [Google Scholar]
- 8.Cattell R, Eber H, Tatsoaka M. Handbook for the Sixteen Personality Factor Questionnaire. Champaign, IL: Institute for Personality and Ability Testing; 1970. [Google Scholar]
- 9.Gibson B, Bergner M, Bobbitt R, Carter W. The Sickness Impact Profile: Final development and testing. Seattle, WA: Center for Health Service Research, University of Washington; 1979. [Google Scholar]
- 10.Victor M, Adams R, Cole M. The acquired (non-Wilsonian) type of chronic hepatocerebral degeneration. Medicine. 1965;44:342–396. doi: 10.1097/00005792-196509000-00001. [DOI] [PubMed] [Google Scholar]