Abstract
OBJECTIVE:
To contrast the efficacy of two exercise programs, segmental stabilization and strengthening of abdominal and trunk muscles, on pain, functional disability, and activation of the transversus abdominis muscle (TrA), in individuals with chronic low back pain.
DESIGN:
Our sample consisted of 30 individuals, randomly assigned to one of two treatment groups: segmental stabilization, where exercises focused on the TrA and lumbar multifidus muscles, and superficial strengthening, where exercises focused on the rectus abdominis, abdominus obliquus internus, abdominus obliquus externus, and erector spinae. Groups were examined to discovere whether the exercises created contrasts regarding pain (visual analogical scale and McGill pain questionnaire), functional disability (Oswestry disability questionnaire), and TrA muscle activation capacity (Pressure Biofeedback Unit = PBU). The program lasted 6 weeks, and 30‐minute sessions occurred twice a week. Analysis of variance was used for inter‐ and intra‐group comparisons. The significance level was established at 5%.
RESULTS:
As compared to baseline, both treatments were effective in relieving pain and improving disability (p<0.001). Those in the segmental stabilization group had significant gains for all variables when compared to the ST group (p<0.001), including TrA activation, where relative gains were 48.3% and ‐5.1%, respectively.
CONCLUSION:
Both techniques lessened pain and reduced disability. Segmental stabilization is superior to superficial strengthening for all variables. Superficial strengthening does not improve TrA activation capacity.
Keywords: Chronic Low Back Pain, Pressure Biofeedback Unit, Segmental Stabilization, Muscle Strength, Transversus Abdominis
INTRODUCTION
Chronic low back pain (CLBP) is defined as back pain lasting more than 12 weeks,1 and it affects more than 50% of the general population. It is estimated that over 70% of adults have at least one episode of low back pain during their lifetimes.2 Prevalence is higher in young, economically active adults in South American populations;3 indeed, low back pain is the second most common reason for absenteeism from work, and one of the most common reasons for medical consultation.4
One important risk factor for low back pain is weakness of superficial trunk and abdominal muscles,5-9 and strengthening of these muscles is often associated with significant improvements of CLBP, as well as with decreased functional disability.10-15 Another independent risk factor for CLBP is the weakness and lack of motor control of deep trunk muscles, such as the lumbar multifidus (LM) and transversus abdominis (TrA) muscles.16,17 Ferreira et al.18 and Hodges et al.19 demonstrated that the TrA had insufficient control and speed of muscle contraction delayed in individuals with CLBP.
Kinesiotherapeutic protocols addressing both the superficial and the deep muscles seem to be effective in the treatment of CLBP.20-22 Most clinical protocols combine different exercises and techniques, making it difficult to isolate the efficacy of specific strategies.10,11 This is of great clinical importance and needs to be further clarified through research. Therefore, in this study, we compared the efficacy of SS exercises with strengthening of abdominal and trunk muscles (ST) on pain, functional capacity, and TrA activation capacity in individuals with CLBP.
Our hypothesis was that the lumbar stabilization would be more efficient than the muscle strength in the improvement of chronic low back pain.
METHODS
Subjects
Our sample was selected from a list of patients being seen at the Department of Orthopedics, University Hospital, Sao Paulo University. We made 162 calls, and performed 35 evaluations. Four patients were excluded for rheumatologic disorders and one for surgical reasons. Therefore, the sample consisted of 30 patients (four men and 11 women in each group) with non‐specific CLBP. They were randomized by means of opaque envelopes to one of two treatment groups: SS and ST. Inclusion criteria were: low back pain for more than 3 months (pain felt between T12 and the gluteal fold), patients willing and able to participate in an exercise program safely and without cognitive impairments that would limit their participation. Exclusion criteria were history of back surgery, rheumatologic disorders, spine infections and spine exercise training in the 3 months before the onset of the study. This study was approved by the Ethics Committee of the University Hospital (Protocol 700/06) and of the School of Medicine (Protocol 1249/06), University of São Paulo. Participants signed informed consent forms.
Assessments
Participants were assessed at baseline and at the end of the treatment by an investigator (physiotherapist) who was blinded to the randomization, the severity of pain, functional disability, and TrA activation capacity.
Pain
Pain was assessed using a visual analogical scale (VAS) and the McGill pain questionnaire.23 The VAS consists of a 10‐cm line, with the left extremity indicating “no pain” and the right extremity indicating “unbearable pain.” Participants were asked to use the scale to indicate their current level of pain. Higher values suggest more intense pain. The McGill pain questionnaire consists of a list of 78 pain descriptors organized into 4 major classes (sensory, affective, evaluative, and miscellaneous) and 20 subclasses, each made up of at least 2 and at most 6 words, to which are assigned intensity values.
Functional Disability
Functional disability was estimated by the Oswestry disability questionnaire,24 a functional scale assessing the impact of low back pain on daily activities. Other questionnaires are available for the measurement of the evaluation of low‐back pain, but McGill and Oswestry were considered the most appropriate in the context of this project.26,27 The score is calculated by the addition of the values assigned for each of the 10 individual questions and is used to categorize disability as: mild or no disability (0‐20%); moderate disability (21%‐40%); severe disability (41% to 60%); incapacity (61% to 80%); restricted to bed (81% to 100%).
Transversus Abdominis Activation Capacity
TrA activation capacity was assessed by using the Stabilizer Pressure Biofeedback Unit (PBU, Chattanooga Group, Australia). The PBU consists of a combined gauge/inflation bulb connected to a pressure cell. It is a simple device that registers changing pressure in an air‐filled pressure cell allowing body movement, especially spinal movement, to be detected during exercise. The gauge contains 16.7 × 24 cm of inelastic material. The pressure cell measures from 0‐200 mmHg, with a precision of 2 mmHg. Changes in body position modify the pressure, and they are registered by the sphygmomanometer.25 The device was placed on the TrA (above the anterior superior iliac spines) while participants were in ventral decubitus over a rigid surface. The depression of the abdominal muscles over the spinal cord typically decreases the pressure by 4‐10 mmHg.20 Before individuals were asked to contract the muscle, the device was inflated to a pressure of 70 mmHg. The participants were instructed to draw the lower stomach gently off the pressure sensor without moving the back or the hips and to sustain it for 10 seconds, measured by a stop watch.
Interventions
Interventions were conducted over 6 weeks, twice per week, each session lasting 30 minutes. Sessions were supervised by the investigator, and participants were instructed to report any adverse event, whether it was related to the exercises or not. Groups were instructed not to participate in any other physical program during the study and not to exercise while at home. In the segmental stabilization (SS) group, exercises focused on the TrA and LM muscles according to the protocol proposed by Richardson et al.17,28 In the superficial strengthening (ST) group, exercises focused on the rectus abdominis (RA), abdominus obliquus internus (OI), abdominus obliquus externus (OE), and erector spinae (ES).29
Three series of 15 repetitions were done for each exercise (Table 1).
Table 1.
Treatment protocol in the segmental stabilization and superficial strengthening groups.
| Segmental Stabilization17,26 | |
| Strengthening of the Tranversus abdominis (TrA) and lumbar multifidus (LM) |
|
| Superficial strengthening27 | |
| Strengthening of the rectus abdominis (RA), external and internal obliquus (EO and IO) and erector spinae (ES) |
|
Statistical Analysis
Sample size was calculated assuming a power of 80% to detect a 30% improvement in pain (VAS), with a standard deviation of 2 points and a significance level of 5%. The required sample would be 10 patients per group.
The relative gain with treatment was calculated with the following equation: 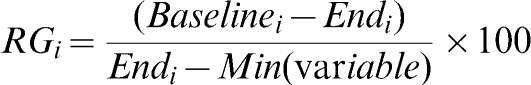
ANOVA One Way was used for inter‐group and intra‐group comparisons. For TrA activation, the binomial test was used.
Analyses were done using Minitab 14 and 15 for Windows. The significance level was established at 5%.
RESULTS
Sample Characterization
Demographic data are presented in Table 2. No significant differences were seen for age, weight, height, and body mass index.
Table 2.
Patient's clinical and demographic data, according to group.
| Features | SS group (n = 15) | ST group (n = 15) | p |
| Mean age (yrs) | 42.07 (8.15) | 41.73 (6.42) | 0.902* |
| Weight (Kg) | 74.61 (16.26) | 73.60 (12.26) | 0.849* |
| Height (cm) | 1.67 (0.11) | 1.65 (0.08) | 0.542* |
| BMI (cm/Kg2) | 26.40 (4.47) | 26.92 (3.64) | 0.725* |
| Pain | |||
| 12 to 24 months | 4 (26.66%) | 6 (40%) | |
| More than 24 months | 11 (73.44%) | 9 (60%) | |
p value for t Test
Pre‐and Post‐Treatment Results
Table 3 displays results found in those randomized to SS training. All variables significantly improved with treatment (p<0.001). The highest relative gain was for pain (99%). Contraction of the TrA improved by 48.3%.
Table 3.
Pain, functional disability and contraction of TrA mean values of SS group at pre‐ and post‐treatment evaluations, and p values.
| Segmental Stabilization (n = 15) | ||||
| Pre‐treat | Post‐treat | Relative gain | P | |
| Pain‐VAS (0‐10 cm)# | ||||
| Mean(SD) | 5.94 (1.56) | 0.06 (0.16) | 99% | <0.001* |
| Pain‐McGill (0‐67)# | ||||
| Mean(SD) | 35.00 (7.76) | 3.20 (4.00) | 92% | <0.001* |
| Sensory (0‐34)# | ||||
| Mean(SD) | 18.20 (4.43) | 1.73 (2.99) | 93% | <0.001* |
| Affective (0‐17)# | ||||
| Mean(SD) | 8.07 (2.43) | 0.33 (0.62) | 97% | <0.001* |
| Functional disability (0‐45)# | ||||
| Mean(SD) | 17.07 (3.99) | 1.80 (1.26) | 90% | <0.001* |
| Contraction of TrA‐UBP (4 to‐10mmHg)# | ||||
| Mean(SD) | ‐0.67 (1.95) | ‐5.33 (1.23) | 48.32% | <0,001* |
statistically significant difference; pre‐treat = before treatment; post‐treat = immediately after treatment
Normal range
Table 4 displays the results for the ST group. All variables significantly improved with treatment (p<0.001), with the exception of TrA contraction (p = 0.99). The highest relative gain was for pain (61%). Functional disability improved by 52% to no or mild disability. However, TrA contraction had negative gains (worsening ‐5.1%).
Table 4.
Pain, functional disability and contraction of TrA mean values of ST group at pre‐ and post‐treatment evaluations, and p values.
| Superficial Strengthening (n = 15) | ||||
| Pre‐treat | Post‐treat | Relative gain | p | |
| Pain‐VAS (0‐10 cm)# | ||||
| Mean(SD) | 6.49 (1.48) | 2.89 (1.45) | 55% | <0.000* |
| Pain‐McGill (0‐67)# | ||||
| Mean(SD) | 37.67 (7.33) | 19.8 (7.93) | 48% | <0.000* |
| Sensory (0‐34)# | ||||
| Mean(SD) | 20.20 (3.55) | 11.27 (4.58) | 43% | <0.000* |
| Affective (0‐17)# | ||||
| Mean(SD) | 9.40 (3.29) | 3.60 (1.99) | 61% | <0.000* |
| Functional disability‐ Oswestry (0‐45)# | ||||
| Mean(SD) | 17.27 (3,84) | 8.40 (3,13) | 52% | <0,000* |
| Contraction of TrA‐ UBP (4 to ‐10mmHg)# | ||||
| Mean(SD) | ‐0.40 (1,35) | 0.00 (1,57) | ‐5.11% | 0,99 |
statistically significant difference; pre‐treat = before treatment; post‐treat = immediately after treatment
Normal range
Intragroup Comparisons
Table 5 contrasts the results seen in each group. The SS group yielded significantly higher gains in all variables when compared to the ST group (p<0.001).
Table 5.
Mean Gain (difference of before and after in each group), and p value.
| Mean(SD) | ST (n = 15) | SS (n = 15) | p |
| Pain‐VAS (cm) | 3.6(1.56) | 5.8(1.61) | <0.001* |
| Pain‐McGill | 17.87(6.73) | 31.8(6.06) | <0.001* |
| Sensory | 8.9(5.05) | 16.4(2.90) | <0.001* |
| Affective | 5.8(2.59) | 7.73(2.18) | <0.001* |
| Functional disability ‐Oswestry | 8.86(2.82) | 15.26(3.43) | <0.001* |
| Contraction of TrA‐ UBP (mmHg) # | ‐0.40(1.60) | 4.66(2.22) | <0.001# |
statistically significant difference (Anova one‐way)
statistically significant difference (Binomial test)
DISCUSSION
The aim of this study was to compare the efficacy of SS and ST exercises in the relief of CLBP symptoms. Both treatments were effective in relieving pain and in decreasing functional impairment, but only the SS treatment improved TrA muscle activation.
The PBU test has been validated by imaging19 and electromyography, 17 tests that are considered to be the gold‐standard measurements of TrA performance. These tests demonstrated that individuals with low back pain have an impaired ability to depress the abdominal wall. Hides et al.30 suggested that the TrA is important in sustaining the spinal cord and that its conditioning is accompanied by functional improvement.
The SS group exercised the TrA and LM muscles. On average, participants had optimal depression of the abdominal wall, as measured by the PBU, with a gain of 48.3% with the program, findings that are similar to those obtained by Cairms et al.31
Ferreira et al.18 and Teyhen et al.32 also suggested that TrA exercising improves muscle activation in individuals with low back pain. According to Jull and Richardson 30 and Richardson et al.,31 normal PBU responses range from ‐4 to ‐10 mmHg; for Hodges et al.,19 mean normal values were around ‐5,82 mmHg.
For pain, the SS technique yielded impressive improvements (99% when measured by the VAS and 90% by the McGill questionnaire); functional disability improved by 90%. Our findings are supported by other studies,21,22 where SS translated into pain and functional capacity improvements. The better results of the SS group may be explained by the fact that this technique addressed two muscles primarily affected by low back pain. Hides16 identified selective atrophy of the LM after the first episode of back pain; the atrophy was unlikely to revert without specific training, and the lower muscular stability predisposed an individual to further episodes of low back pain. In individuals with low back pain, the TrA has decreased anticipatory capacity, meaning that it has reduced segmental protective function.19 Richardson et al.17 suggested that both muscles are primary stabilizers of the lumbar segment, minimizing compressive forces on spinal structures.
The ST group performed exercises that aimed to strengthen the superficial muscles of the abdomen and trunk. The regimen yielded significant pain and functional capacity improvements, which were also demonstrated by other studies.10,11 Rodacki et al.33 suggested that abdominal exercises are associated with low back pain improvement, since during abdominal contraction the pressure on the intervertebral disks was decreased as a consequence of the increased intra‐abdominal pressure. However, no improvements on TrA capacity of activation were observed. Cairms et al.31 found that individuals with a history of but no current low back pain had impairments in TrA contraction. Accordingly, pain remission does not necessarily translate into improved muscle activation capacity.
The better improvement in all variables yielded by the SS relative to ST may be explained by the hierarchical structure of the muscular control system. According to Bergmark,34 two systems are important. The local system is formed by the deep muscles directly involved with the joints, and their primary function is stabilizing the segments, avoiding articular micro‐movements. These muscles do not normally perform joint movements, which makes contracting them more difficult, and this is exacerbated by pain. The second system is formed by the superficial muscles, which secondarily stabilize the spinal cord, further minimizing compressive forces. The main function of this system is to generate and control axial movements, and it makes little contribution to segmental stability.
Hides et al.16 found that even after pain remission in patients with low back pain, proper deep muscle reestablishment often did not happen and that specific physical therapy focusing on those muscles was necessary. Snijders et al.35 postulated that the co‐contraction of the TrA and LM muscles is the basis of the lumbo‐sacral biomechanic stability and that these muscles act by reducing the compressive overloads, attenuating or eradicating pain perception. According to Norris,36 the rectus abdominis is the most important trunk flexor, while the obliquus muscles support flexion but also rotation, and lateral inclination as well as providing secondary stability during exercise.37
Our findings suggest that both protocols are of clinical utility in the improvement of chronic low back pain.
CONCLUSIONS
Segmental stabilization and strengthening exercises effectively reduce pain and functional disability in individuals with chronic low back pain. Segmental stabilization but not strengthening improves TrA muscle activation capacity. Improvement in all variables was superior in the segmental stabilization group opposed to the strengthening group.
LIMITATIONS OF THE STUDY
Limitations of the study were that there were no intermediate and long‐term follow up examinations. Moreover, biopsychosocial factors were not observed in this study.
clinicaltrials.gov registration number: NCT01124201
Figure 1.
The test of the abdominal drawing in action in a prone position, monitoring the contraction of TrA with pressure biofeedback unit.
REFERENCES
- 1. Rozemberg S. Chronic low back pain: Definition and treatment. Rev Prat. 2008;15;58:265–72. [PubMed] [Google Scholar]
- 2. Lawrence JP, Greene HS, Grauner JN. Back pain in athletes. J Am Acad Orthop Surg. 2006;14:726–35. doi: 10.5435/00124635-200612000-00004. [DOI] [PubMed] [Google Scholar]
- 3. De Vitta A. A lombalgia e suas relações com o tipo de ocupação com a idade e o sexo. Rev Bras Fisioter. 1996;1:67–72. [Google Scholar]
- 4. Ebenbichler GR, Oddsson LIE, Kollmitzer J, Erim Z. Sensory‐motor control of the lower back: Implications for rehabilitation. Med Sci Sports Exerc. 2001;33:1889–98. doi: 10.1097/00005768-200111000-00014. 10.1097/00005768‐200111000‐00014 [DOI] [PubMed] [Google Scholar]
- 5. Bayramoglu M, Akman MN, Kilinç S, Çetin N, Yavuz N, Özker R. Isokinetic measurement of trunk muscle strength in women with chronic low back pain. Am J Phys Med Rehabil. 2001;80:650–5. doi: 10.1097/00002060-200109000-00004. 10.1097/00002060‐200109000‐00004 [DOI] [PubMed] [Google Scholar]
- 6. Danneels LA, Vanderstraeten GG, Cambier DC, Witvrouw EE, Cuyper HJ. CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur Spine J. 2000;9:266–72. doi: 10.1007/s005860000190. 10.1007/s005860000190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hodges PW, Moseley GL, Gabrielsson A, Gandevia SC. Experimental muscle pain changes feed forward postural responses of the trunk muscles. Exp Brain Res. 2003;151:262–71. doi: 10.1007/s00221-003-1457-x. 10.1007/s00221‐003‐1457‐x [DOI] [PubMed] [Google Scholar]
- 8. Barr KP, Griggs M, Cadby T. Lumbar stabilization: A review of core concepts and current literature, part 2. Am J Phys Med Rehabil. 2007;86:72–80. doi: 10.1097/01.phm.0000250566.44629.a0. 10.1097/01.phm.0000250566.44629.a0 [DOI] [PubMed] [Google Scholar]
- 9. Shirado O, Kaneda K, Ito T. Trunk muscle strength during concentric and eccentric contraction: A comparison between healthy subjects and patients with low back pain. J Spinal Disord. 1992;5:175–82. doi: 10.1097/00002517-199206000-00005. 10.1097/00002517‐199206000‐00005 [DOI] [PubMed] [Google Scholar]
- 10. Liddle SD, Baxter GD, Gracey JH. Exercice and chronic low back pain: What works? Pain. 2004;107:176–90. doi: 10.1016/j.pain.2003.10.017. 10.1016/j.pain.2003.10.017 [DOI] [PubMed] [Google Scholar]
- 11. Hayden JA, van Tulder MW, Malmivaara A, Koes BW. Meta‐analysis: Exercice therapy for nonspecific low back pain. Ann Intern Med. 2005;142:765–75. doi: 10.7326/0003-4819-142-9-200505030-00013. [DOI] [PubMed] [Google Scholar]
- 12. Carpenter DM, Nelson BW. Low back strengthening for the prevention and treatment of low back pain. Med Sci Sports Exerc. 1999;31:18–24. doi: 10.1097/00005768-199901000-00005. 10.1097/00005768‐199901000‐00005 [DOI] [PubMed] [Google Scholar]
- 13. Leggett S, Mooney V, Matheson LN, Nelson B, Dreisinger T, Zytveld JV, Vie L. Restorative exercise for clinical back pain. A prospective two‐center study with one year follow‐up. Spine. 1999;24:889–98. doi: 10.1097/00007632-199905010-00010. 10.1097/00007632‐199905010‐00010 [DOI] [PubMed] [Google Scholar]
- 14. Takemasa R, Yamamoto H, Tani T. Trunk muscle strength and effect of trunk muscle exercises for patients with chronic low back pain. The differences in patients with and without organic lumbar lesions. Spine. 1995;20:2522–30. doi: 10.1097/00007632-199512000-00012. 10.1097/00007632‐199512000‐00012 [DOI] [PubMed] [Google Scholar]
- 15. Calmels P, Jacob JF, Fayolle‐Minon I, Charles C, Bouchet JP, Rimaud D, et al. Étude comparative entre technique isocinétique et kinésithérapie classique chez le lombalgique chronique. Résultats préliminaires. Ann Readapt Med Phys. 2004;47:20–7. doi: 10.1016/j.annrmp.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 16. Hides JA, Richardson CA, Jull GA. Multifidus muscle recovery is not automatic following resolution of acute first‐episode low back pain. Spine. 1996;21:2763–9. doi: 10.1097/00007632-199612010-00011. 10.1097/00007632‐199612010‐00011 [DOI] [PubMed] [Google Scholar]
- 17.Richardson C, Hodges P, Hides J. Therapeutic exercise for lumbopelvic stabilization: a motor control approach for the treatment and prevention of low back pain. 2nd ed. London: Churchill Livingstone; 2004. [Google Scholar]
- 18. Ferreira PH, Ferreira ML, Maher CG, Refshauge K, Herbert R, Hodges PW. Changes in recruitment of transversus abdominis correlate with disability in people with chronic low back pain. Br J Sports Med. doi: 10.1136/bjsm.2009.061515. published online 26 May 2009;doi:10.1136/bjsm.2009.061515. [DOI] [PubMed] [Google Scholar]
- 19. Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain: A motor control evaluation of transversus abdominis. Spine. 1996;21:2640–50. doi: 10.1097/00007632-199611150-00014. 10.1097/00007632‐199611150‐00014 [DOI] [PubMed] [Google Scholar]
- 20.Richardson C, Jull G, Hodges PW, Hides JA. Therapeutic Exercise for Spinal Segmental Stabilization in Low Back Pain: Scientific Basis and Clinical Approach. 1a ed. Sydney: Churchill Livingstone; 1999. [Google Scholar]
- 21. O'Sullivan PB, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine. 1997;22:2959–67. doi: 10.1097/00007632-199712150-00020. 10.1097/00007632‐199712150‐00020 [DOI] [PubMed] [Google Scholar]
- 22. Hides JA, Jull GA, Richardson CA. Long‐term effects of specific stabilizing exercises for first‐episode low back pain. Spine. 2001;26:E243–8. doi: 10.1097/00007632-200106010-00004. 10.1097/00007632‐200106010‐00004 [DOI] [PubMed] [Google Scholar]
- 23. Varoli FK, Pedrazzi V. Adapted version of the McGill pain questionnaire to Brazilian Portuguese. Braz Dent J. 2006;17:328–35. doi: 10.1590/s0103-64402006000400012. 10.1590/S0103‐64402006000400012 [DOI] [PubMed] [Google Scholar]
- 24. Vigatto R, Alexandre NM, Filho HR. Development of a Brazilian Portuguese version of the Oswestry Disability Index. Spine. 2007;32:481–6. doi: 10.1097/01.brs.0000255075.11496.47. 10.1097/01.brs.0000255075.11496.47 [DOI] [PubMed] [Google Scholar]
- 25. Maciel SC, Jennings F, Jones A, Natour J. The development and validation of a Low Back Pain Knowledge Questionnaire ‐ LKQ. Clinics. 2009;64:1167–75. doi: 10.1590/S1807-59322009001200006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Furtado R, Jones A, Furtado RN, Jennings F, Natour J. Validation of the Brazilian‐Portuguese version of the Gesture Behavior Test for patients with non‐specific chronic low back pain. Clinics. 2009;64:83–90. doi: 10.1590/S1807-59322009000200004. 10.1590/S1807‐59322009000200004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anonymous. Stabilizer pressure biofeedback. Operating Instructions. Brisbane: Chattanooga Pacific; 2002. [Google Scholar]
- 28. Richardson C, Jull G. Muscle control‐pain control. What exercises would you prescribe? Manual Therapy. 1995;1:2–10. doi: 10.1054/math.1995.0243. 10.1054/math.1995.0243 [DOI] [PubMed] [Google Scholar]
- 29.Kisner C, Colby L. Exercícios terapêuticos: Fundamentos etécnicas. 3a ed. São Paulo: Manole; 2000. [Google Scholar]
- 30. Hides J, Wilson S, Stanton W, McMahon S, Keto H, McMahon K, et al. An MRI investigation into the function of the transversus abdominis muscle during “drawing‐in” of the abdominal wall. Spine. 2006;31:175–8. doi: 10.1097/01.brs.0000202740.86338.df. 10.1097/01.brs.0000202740.86338.df [DOI] [PubMed] [Google Scholar]
- 31. Cairms MC, Harrison K, Wright C. Pressure biofeedback: A useful tool in the quantification of abdominal muscular dysfunction? Physiother. 2000;86:127–38. 10.1016/S0031‐9406(05)61155‐8 [Google Scholar]
- 32. Teyhen DS, Miltenberger CE, Deiters HM, Del Toro YM, Pulliam JN, Childs JD, et al. The use of ultrasound imaging of the abdominal drawing‐in maneuver in subjects with low back pain. J Orthop Sports Phys Ther. 2005;35:346–55. doi: 10.2519/jospt.2005.35.6.346. [DOI] [PubMed] [Google Scholar]
- 33. Rodacki CLN, Rodacki ALF, Ugrinowitsch C, Zielinski D, Costa RB. Spinal unloading after abdominal exercises. Clin Biomech. 2008;23:8–14. doi: 10.1016/j.clinbiomech.2007.08.022. 10.1016/j.clinbiomech.2007.08.022 [DOI] [PubMed] [Google Scholar]
- 34. Bergmark A. Stability of lumbar spine: A study in mechanical engineering. Acta Orthop Scand. 1989;230:1–54. doi: 10.3109/17453678909154177. [DOI] [PubMed] [Google Scholar]
- 35. Snijders CJ, Ribbers MT, de Bakker HV, Stoeckart R, Stam HJ. EMG recordings of abdominal and back muscles in various standing postures: Validation of a biomechanical model on sacroiliac joint stability. J Eletromyogr Kinesiol. 1998;8:205–14. doi: 10.1016/s1050-6411(98)00005-4. 10.1016/S1050‐6411(98)00005‐4 [DOI] [PubMed] [Google Scholar]
- 36. Norris CM. Abdominal muscle training in sport. Br J Sports Med. 1993;27:19–27. doi: 10.1136/bjsm.27.1.19. 10.1136/bjsm.27.1.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mirka G, Kelaher D, Baker A, Harrison A, Davis J. Selective activation of the external oblique musculature during axial torque production. Clin Biomech. 1997;12:172–80. doi: 10.1016/s0268-0033(97)00061-2. 10.1016/S0268‐0033(97)00061‐2 [DOI] [PubMed] [Google Scholar]



