Abstract
OBJECTIVE:
We aim to compare selective spinal anesthesia and general anesthesia with regard to postoperative recovery and fast‐track eligibility in day surgeries.
MATERIALS AND METHOD:
Sixty geriatric outpatient cases, with ASA II‐III physical status and requiring short‐duration transurethral intervention, were enrolled in the study. The cases were split into 2 groups: as general anesthesia (Group GA) and selective spinal anesthesia (Group SSA). Group GA (n = 30) received propofol 2 mg kg‐1 (until loss of eyelash reflex), remifentanil induction 0.5‐1 µg kg‐1, and laryngeal mask. Maintenance was achieved by 4‐6% desflurane in 60% N2O and 40% O2 along with remifentanil infusion at 0.05 µg /kg‐1 /min‐1. Drugs were discontinued after the withdrawal of the ureteroscope, and extubation was carried out with 100% O2. Group SSA (n = 30) received 0.5% spinal anesthesia via L4‐5 space by 0.5% hyperbaric bupivacaine 5 mg. Anesthesia preparation time, time to surgical anesthesia level, postoperative fast‐tracking, and time to White‐Song recovery score of 12, were noted. In the operating room, we evaluated hemodynamics, nausea/vomiting, surgeon and patient satisfaction with anesthesia, perioperative midazolam‐fentanyl administration, postoperative pain, and discharge time.
RESULTS:
Anesthesia preparation time, length of surgery, anesthesia‐related time in the operating room, time to sit, and time to walk were significantly low in Group GA (p<0.05), whereas time to fast‐track eligibility, length of stay in the PACU, discharge time, and other parameters were similar in both of the groups.
CONCLUSION:
While anesthesia preparation time, length of surgery, start time of surgery, time to sit, and time to walk were shorter in the General Anesthesia group, time to fast‐track eligibility, phase 1 recovery time, and discharge time were similar among patients subjected to selective spinal anesthesia.
Keywords: Selective spinal anesthesia, General anesthesia, Postoperative recovery, Fast‐track, Geriatri
INTRODUCTION
At the beginning of the 20th century, an age of over 50 was a contraindication for surgery; however, the ever‐improving health conditions have made more complicated and difficult interventions feasible, thereby producing a growing number of geriatric patients.1,2
Although advanced age does not constitute a contraindication for outpatient anesthesia and surgical procedures alone, morbidity and mortality associated with anesthesia shows a higher rate among elderly compared with young adults.2 Novel procedures and techniques are investigated in order to ensure fast and safe operations and discharges.2
Urologic interventions are performed endoscopically or as open surgery, and the majority of those procedures are conducted on geriatric patients. The aim to perform operations rapidly and discharge the patients as soon as possible increases the significance of the anesthesia technique. The anesthesia should be chosen based on its side effects and risk factors by the patient, surgeon, and the anesthesiologist.3
Currently, fast‐tracking patients to early recovery is a growing tendency in order to reduce the complications, shorten the hospital stay, decrease the costs, and increase patient circulation. Fast‐track surgery describes the use of multimodal preoperative rehabilitation programs that target early discharge from the hospital and a faster return to routine daily life and activities. While a successful fast‐track surgery program comprises multifactorial elements, such as pre‐ and post‐operative nursing, preoperative preparation, postoperative analgesia, and prevention of nausea/vomiting, anesthesiologists are the key factors in a fast‐track surgery program.2,4-6
Some studies report that selective spinal anesthesia provides considerably more rapid early phase recovery and ability to ambulate compared with general anesthesia.6-8
Therefore, in the present study, we aimed to compare the effects of selective spinal anesthesia with hyperbaric bupivacaine 5mg and general anesthesia, including an induction with propofol + remifentanil and a maintenance with desflurane, over recovery and fast‐tracking eligibility among geriatric patients in day surgeries.
MATERIAL AND METHOD
Sixty geriatric cases (age > 65 years) with ASA 2‐3 physical status and requiring short‐duration transurethral intervention, were enlisted in the study after obtaining the ethics committee approval and informed consent from the patients. The ones having a body mass index >32, having a history of allergy against the study drugs or demonstrating contraindication for spinal or general anesthesia, were excluded from the study. Moreover, apart from the anesthesia method, because of influence on discharge time, patients who developed surgical complications during the perioperative period were excluded from the study as well.
The cases were selected in this prospective, randomized study by use of computer‐generated randomization tables and split into two groups: General Anesthesia (Group GA) and Selective Spinal Anesthesia (Group SSA).
Each patient was monitored for electrocardiography, noninvasive arterial blood pressure, and pulse oxymetry. Peripheral IV line was opened with a 20G cannula and crystalloid infusion was started at 5 ml/kg/h. In all the patients, heart rate, mean arterial pressure (MAP), and oxygen saturation (SpO2) were recorded before the operation; after the anesthesia; during the operation at 1, 3, 5, 10, 15, and 20 minutes, followed by measurements every 10 minutes; during the extubation; and after the extubation at 5, 10, and 20 minutes.
Anesthesia induction in Group GA (n = 30) was performed by delivery of propofol 2 mg kg‐1 (until the disappearance of eyelash reflex) and 0.5‐1 µg kg‐1 remifentanil (within 60 seconds) before applying the laryngeal mask. Anesthesia maintenance was achieved with administration of 4‐6% desflurane and 40% O2 and 60% N2O. During the operation, 0.05 µg /kg‐1 /min‐1 remifentanil infusion was also employed. End‐tidal CO2 concentration was 32‐36 mmHg, and the respiration of the patient was supported with mechanical ventilation. The characteristics of mechanical ventilation are synchronized intermittent mandatory ventilation (SIMV), 8 ml/kg tidal volume, and 11 min/breath. In cases where hypertension and tachycardia surpassed 20% of the control values and could not be controlled, remifentanil dose was elevated by 50%. Drugs used for the maintenance of anesthesia were completely discontinued after the removal of the ureteroscope, and 100% O2 ventilation was started while extubation was performed upon restoration of the respiration. Patients were evaluated with the White‐Song recovery scoring system in the recovery room every 5 minutes.9 They were allowed to go to the ward service when they demonstrated a score above 12, showed no dizziness, and appeared to be able to sit down.
Group SSA (n = 30) received spinal anesthesia at the sitting position by means of 0.5% hyperbaric bupivacaine, 5 mg via the midline approach method from the L4‐5 space. Local anesthetic was delivered without aspirating the CSF and patients were kept waiting (a maximum of 10 minutes) until reaching the anesthesia level of T10. Patients with perioperative requirements were administered midazolam 0.03 mg/kg and fentanyl 0.25 µg /kg IV. Sensory block was evaluated with a pin‐prick test, whereas motor block was assessed with the Bromage scale. Among those cases, times to surgical anesthesia level, along with sensory and motor block levels, were recorded. After the end of the surgery, sensory and motor blocks were evaluated every 20 minutes until patients were referred to the service. The interval between Phase I recovery time and referral to service was noted. Based on the White‐Song recovery score, patients were referred to the service when the score dropped below 12, the sensory block decreased below T12 level, complete restoration of motor block was achieved, and patients were able to sit.
Patients were asked aboud their nausea/vomiting history and the ones with more than two risk factors (female, nonsmoker, history of postoperative nausea/vomiting [PONV] or movement disorder), were subjected to prophylactic dexamethasone 5 mg IV after the induction and a 5‐HT3 NT antagonist (ondansetron 4 mg) IV after the end of the surgery. In treatment of PONV, metoclopramide 10 mg IV for patients with prophylaxis and ondansetron 4 mg IV for those without prophylaxis were applied.
Anesthesia preparation time was recognized to be the duration between the assuming of the proper position by patients and the end of the 10‐minute period required for achieving complete block in Group SSA, whereas it was noted to be the duration between the start of drug delivery for induction and connection of the patient to the respiratory device in Group GA. Time to fast‐tracking eligibility was noted to be the interval between the removal of the cystoscope and the time to a White‐Song score of 12. In the operating room, anesthesia‐related time was the total of LMA duration and the times required for achievement of extubation and orientation, whereas it was the duration starting with spinal anesthesia and ending with the establishment of complete block in group SAA. Patient and surgeon satisfaction along with the quality of motor block, were evaluated during this period, as well. Moreover, delivery of preoperative agents such as midazolam or fentanyl and use of other drugs for therapeutic reasons were noted. Time to walk, time to discharge eligibility, and time of first urination, were calculated relative to the removal time of cystoscope. Discharge criteria were having no nausea, vomiting, and hemorrhage; absence of pain or presence of mild pain; and being able to walk. The patients were not required to perform their first urination prior to the discharge; however, if they were still in the hospital and had no catheter, their time of first urination was recorded. Symptoms such as nausea/vomiting, headache, back pain, considerable weariness, dysuria, transient neurologic symptoms, postdural headache, and other pains during the postoperative period and the day after, were investigated, evaluated and treated accordingly.
Postoperative pain was evaluated with a visual analogue scale (VAS; 0: no pain, 10: severe pain) and the values at postoperative 1, 5, 10, 20, 40, 60, 80, and 120 minutes were recorded. VAS scores above 7 were evaluated as severe pain and treated with tramadol 100 mg. VAS scores higher than 3 and lower than 7 were recognized as moderate pain and treated with paracetamol 1000 mg IV.
Home discharge criteria were stable vital signs, absence of PONV, no or minimal pain (VAS < 4), no hemorrhage, and being able to walk. Discharge times were noted.
Statistical analysis was carried out with the SPSS 12 statistical package. Categorical data were expressed as frequencies and percentages: intergroup comparisons of those values were done with a Chi‐square test. Noncategorical data were expressed as median and standard deviation values, and intergroup comparisons were performed with the Mann‐Whitney U test, whereas intragroup comparisons were done with the Wilcoxon Sign test. P<0.05 was recognized as significant. By taking alpha as 0.05, the power value was found to be 0.79. The power value was evaluated with the G‐power 3.1 package program. On the basis of previous studies alpha as 0.05 and beta as 0.8 revealed that 30 patients per group would be required for detecting achievement of fast tract eligibility.10
RESULTS
There was no statistically significant difference between the age, height, weight, gender, and ASA physical status of patients (Table 1).
Table 1.
Demographic data.
| Group GA (n = 30) | Group SSA (n = 30) | p | |
| Height (cm) | 169.7±7.3 | 170.5±7.6 | 0.550 |
| Weight (kg) | 76.4±11.8 | 76.0±12.5 | 0.900 |
| Age (year) | 65.8±11.9 | 70.0±9.6 | 0.112 |
| Gender (M/F) | 27/3 | 25/5 | 0.855 |
| ASA (2/3) | 9/21 | 13/17 | 0.650 |
Intergroup analysis revealed statistically significant lower anesthesia preparation time, length of surgery, anesthesia‐related time in the operating room, time to sit, and time to walk in Group GA, whereas similar values were shown with Group SSA regarding time to fast‐track eligibility, length of stay in the PACU, and discharge time (Table 2).
Table 2.
Intergroup analysis of parameters associated with time.
| Group GA (n = 30) | Group SSA (n = 30) | p | |
| Length of surgery (min) | 19.0±10.2 | 29.3±12.4 | 0.001 |
| Anesthesia preparation time (min) | 4.3±1.7 | 11.7±5.8 | 0.000 |
| Anesthesia‐related time in the operating room (min) | 7.9±3.1 | 14.0±3.7 | 0.000 |
| Time to fast‐track eligibility (min) | 7.7±5.6 | 5.6±5.4 | 0.130 |
| Length of stay in the postoperative care unit (PACU) (min) | 21.7±8.1 | 23.3±12.5 | 0.970 |
| Time to sit (min) | 16.9±10.3 | 34.6±17.1 | 0.000 |
| Time to walk (min) | 39.5±32.9 | 60.9±19.7 | 0.007 |
| Discharge time (min) | 131.9±34.7 | 111.7±51.7 | 0.116 |
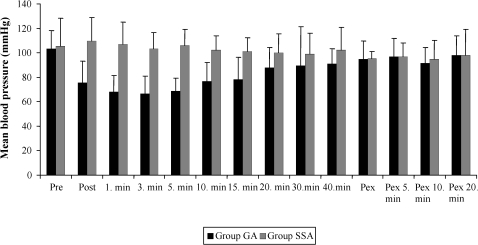
Intergroup analysis showed statistically significantly lower mean blood pressure values in Group GA during induction and at 1, 3, 5, 10, and 30 minutes of post‐induction (Fig. 1).
Figure 1.
Average changes in blood pressure.
Pre: preinduction, Post:postinduction, Pex: post‐extubation
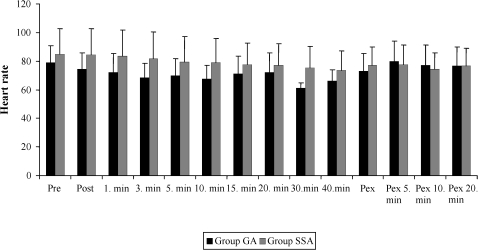
Also, intergroup analysis revealed statistically significantly lower heart rates in Group GA during induction and at 1, 3, 5, 10, and 30 minutes of post‐induction (Fig. 2).
Figure 2.
Average changes in heart rate.
Pre: preinduction, Post:postinduction, Pex: post‐extubation
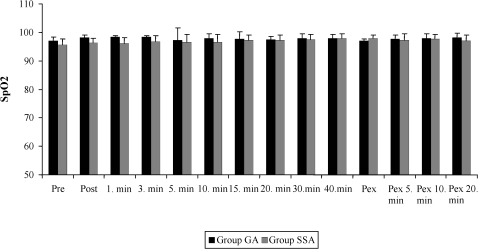
Moreover, in the intergroup comparisons, SpO2 values were statistically significantly lower in Group SSA during the induction and at 1, 3, 5, and 10 minutes post‐induction (Fig. 3).
Figure 3.
Distribution of SpO2 over time.
Pre: preinduction, Post:postinduction, Pex: post‐extubation
In Group SAA, motor block was good in 39.1% of patients, whereas it was moderate in 52.2% of patients. Again in Group SAA, during the perioperative period 72.7% of patients were delivered midazolam and 12.1% received fentanyl, whereas during the postoperative period, 3% of the patients required tramadol and 15.2% needed paracetamol. However, in group GA, 13% of patients required tramadol and 39% needed paracetamol. During the early postoperative period, median VAS was 2 in Group SSA and 3 in Group GA. Nausea/vomiting prophylaxis was required by only 3% of patients in Group SAA. In the phase I recovery unit, nausea/vomiting treatment was applied to 3% of Group SSA and 8.7% of Group GA. Weariness was determined in 56.5% of Group GA and 6.7% of Group SAA. Headache was present in 6.1% of Group SSA and 13% of Group GA. While only 9.1% of patients in Group SSA demonstrated dysuria, the rate was 39.1% in Group GA. Patient satisfaction with anesthesia was very good in 85.2% and moderate in 14.8% of Group SSA patients, whereas it was very good in 75% and moderate in 25% of Group GA patients. Patients of both groups were satisfied with the anesthesia methods and demanded the same methods in the future. Satisfaction with surgery was very good in 88.9% and moderate in 11.1% of Group SSA, whereas it was very good in 91.7% and moderate in 8.3% of Group GA patients (Table 3).
Table 3.
Post‐operative clinical findings.
| Group SAA (30) | Group GA (30) | |
| Motor block Good | 39.1% | |
| Moderate | 52.2% | _ |
| Bad | 8.7% | |
| Midazolam treatment | 72.7% | |
| Fentany treatment | 12.1% | ‐ |
| Tramadol treatment | 3% | 13% |
| Paracetamol treatment | 15.2% | 39% |
| Median VAS | 2 | 3 |
| Nausea/vomiting prophylaxis | 3% | ‐ |
| Nausea/vomiting treatment (Phase I recovery unit) | 3% | 8.7% |
| Weariness | 6.7% | 56.5% |
| Headache | 6.1% | 13% |
| Dysuria | 9.1% | 39.1% |
| Patient satisfaction | ||
| Very good | 85.2% | 75% |
| Moderate | 14.8% | 25% |
| Bad | 0 | 0 |
| Satisfaction with surgery | ||
| Very good | 88.9% | 91.7% |
| Moderate | 11.1% | 8.3% |
| Bad | 0 | 0 |
DISCUSSION
In the present study, in which we investigated the effects of two different anesthesia techniques over recovery and discharge processes among elderly patients, the general anesthesia group which was subjected to propofol‐remifentanil infusion + desflurane maintenance, demonstrated shorter anesthesia preparation time, length of surgery, start time of surgery, time to sit, and time to walk; however, time to fast‐track eligibility, phase I recovery time, and discharge time were similar with the results of the selective spinal anesthesia patients. However, hemodynamic parameters were observed to be more stable in the SSA group.
In the present study, we compared the general anesthesia achieved by propofol + remifentanil induction and desflurane maintenance, with selective spinal anesthesia achieved with hyperbaric bupivacaine 5 mg, among day surgery patients undergoing short‐duration transurethral intervention. Anesthesia preparation time was 4.3 ± 1.7 minutes and anesthesia‐related time in the operating room was 7.9 ± 3.1 minutes among the general anesthesia patients. Anesthesia preparation time and anesthesia‐related time in the operating room were 11.7 ± 5.8 and 14.0 ± 3.7 minutes in the SSA group, respectively.
Koltka et al.11 conducted a study on day surgery by using propofol + remifentanil for induction and desflurane inhalation for maintenance. Time to surgical anesthesia level was found to be 7 (5‐25) minutes which was consistent with our result.
Zohar et al.10 reported that spinal anesthesia by a combination of bupivacaine 4 mg + fentanyl 20 µg achieved adequate analgesia among elderly patients undergoing transurethral intervention. The patients also showed hemodynamic stability and a good recovery profile. The same authors reported that a combination of bupivacaine 5 mg + fentanyl 20 µg considerably prolonged the length of stay in the PACU.12 Koltka et al. 11 employed 5 mg hyperbaric bupivacaine in patients undergoing unilateral anesthesia and reported the time to surgical anesthesia level as 16 (9‐25) minutes. In the current study, considering the time of spinal anesthesia, anesthesia preparation time was closer to those values in the selective spinal anesthesia group.
Anesthesia preparation time and anesthesia‐related time in the operating room were higher in selective spinal anesthesia patients. In order to benefit from the advantages of regional anesthesia in transurethral interventions, block level should reach the T10 level. In the study of Zohar et al., the time to onset of sensory block at the T10 level was found to be 4.8±2.4 minutes in spinal anesthesia, including the combination of bupivacaine 5 mg and fentanyl 20 µg.10 In our study, unlike in the studies mentioned above, we used hyperbaric bupivacaine 5 mg, and the level of block was elevated by making the patients assume a half‐sitting position. When required, additional sedatives and analgesics were applied. Perioperative sedative was given to 72.7% of the patients, whereas only 12.1% required analgesics. Such an elevated requirement of sedative may have arisen from the lack of preoperative sedation. By use of hyperbaric bupivacaine 5 mg, the median block level has been reported to be T8(T4‐T12), while the length of anesthesia and the percentage of patients evaluating the anesthesia as adequate have been noted to be 123±7 minutes and 73%, respectively.13
Patient satisfaction with the anesthetic method was noted to be very good by 85.2%. Therefore, we believe that, despite long anesthesia preparation time and anesthesia‐related time in the operating room, short‐duration transurethral intervention can be performed with bupivacaine 5 mg without using additional opioid in the spinal anesthesia.
We applied the White‐Song scoring system and waited for the patients to reach a fast‐tracking score of 12. In terms of time to the White‐Song score of 12, there was no statistically significant difference between the Group GA and the Group SSA patients; however, it was shorter among the SSA cases. The length of stay in the PACU was similar in both of the groups.
In day surgery, fast‐tracking eligibility following general anesthesia has taken on increasing importance. Transfer of patients directly from the operating room to the recovery room, where less invasive monitoring is applied, results in considerable financial gains. Freidman et al.12 investigated fast‐tracking eligibility among elderly patients undergoing short‐duration urological surgery, and found that recovery time with desflurane was 8.7+3.2 minutes and the time to a fast‐tracking score of 14 was 22±23 minutes. Koltka et al. delivered desflurane and fentanyl to their patients and found the recovery time to be 8 (5‐20) minutes. One study compared combinations of sevoflurane and desflurane with fentanyl and desflurane according to different recovery scores in day surgeries. In patients who received desflurane and remifentanil, the median fast‐tracking score at 5 and 10 minutes after extubation was 12. This value was 7.7±5.6 minutes among the general anesthesia group of our study, and it was similar to the value found by this study. Koltka et al. described the time to recovery as 0 minutes in spinal anesthesia patients. In the current study, this time was shorter compared with the general anesthesia patients; however, it was different from the one found by Koltka et al. Elderly patients show particular sensitivity to drug interactions. Intraoperative usage of midazolam (0.5‐2 mg) may induce moderate or deep sedation in a dose‐dependent way, which might have a negative effect on the recovery.11
Zohar et al.10 found the exit time from the PACU with bupivacaine 5 mg and fentanyl 20 µg to be 105±39 minutes. In the present study, exit time from the PACU was 2.7±8.1 minutes for Group GA and 23.3±12.5 minutes for Group SSA.
In order to ensure safe home discharge after day surgery, guidelines have been issued.15,16 Vital signs should be stable for at least 1 hour. The patient should demonstrate flawless time and space orientation as well as self‐consciousness. Moreover, the patient should be able to receive fluids orally, urinate, wear one's clothes, and walk without help. Koltka et al. found the discharge time to be 110 (75‐230) minutes in Group GA and and 120 (75‐240) minutes in Group SSA. Ben‐David et al. 17 reported the time to sit after delivery of bupivacaine 5 mg to be 140±6 minutes; time to urination, 163± 8 minutes; and discharge time, 181±8 minutes. In the present study, time to sit was 16.9±10.3 minutes in the Group GA patients, whereas it was 34.6±17.1 minutes in the Group SSA patients. Time to walk was 39.5±32.9 in Group GA and 60.9±19.7 in Group SSA patients. Discharge time was found to be 13.9±34.7 and 111.0±57.5 minutes in the Group GA and Group SSA patients, respectively. While the times to sit and time to walk were longer in the SSA patients, discharge time was shorter and was consistent with the discharge time found by Koltka et al. The reason behind the difference from the values given by Ben‐David et al. may be differing maximal block levels.
Cardiac and pulmonary problems have been demonstrated to increase among elderly patients who received transurethral intervention. Opioid‐induced chest wall rigidity occurs more frequently in the elderly, especially with remifentanil. This risky effect can result in increased recovery time for arterial saturation. Perioperative hypotension is more frequent and more severe in the elderly than in the young. Vasopressor drugs, such as dopamine and norepinephrine, can be used to control hypotension. Therefore, applying a stable anesthesia that would minimize the hemodynamic changes in those patients is important. General anesthesia has been noted to cause more hemodynamic changes compared with regional anesthesia in patients undergoing TURP; therefore, regional anesthesia is recommended.18,19 In the current study, among patients who received general anesthesia, particularly within the first 15 minutes after the induction, we observed blood pressure changes reaching the level of 30%, whereas stable hemodynamics were noted in patients who received selective spinal anesthesia. We believe that selective spinal anesthesia is a more appropriate method because it is associated with more stable hemodynamics.
VAS values in patients who received selective spinal anesthesia were lower than in those who underwent general anesthesia, and they required less postoperative analgesia. Nausea/vomiting rates were similar in both groups. More than 80% of selective spinal anesthesia patients developed motor block, and 39.1% of general anesthesia patients exhibited dysuria. Weariness following anesthesia and surgery was higher in Group GA. Side effects are also important factors that influence discharge. In particular,post spinal headache, which can occur after spinal anesthesia, affects discharge negatively. We observed headache following spinal anesthesia in one of our patients.
In conclusion, selective spinal anesthesia achieved by hyperbaric bupivacaine in patients undergoing short‐duration transurethral intervention elevates the anesthesia preparation time and anesthesia‐related time in the operating room, while keeping patients from sitting and walking early. Nonetheless, we believe that it accelerates fast‐tracking and discharge compared with general anesthesia, and provides more stable hemodynamics. Therefore, selective spinal anesthesia is a preferable anesthesia method for fast‐tracking among elderly patients.
REFERENCES
- 1. Mulroy MF, McDonald SB. Regional anesthesia for outpatient surgery. Anesthesiol Clin North America. 2003;21:289–303. doi: 10.1016/s0889-8537(02)00071-8. 10.1016/S0889‐8537(02)00071‐8 [DOI] [PubMed] [Google Scholar]
- 2. Kuusniemi KS, Pihlajamäki KK, Pitkänen MT, Helenius HY, Kirvelä OA. The use of bupivacaine and fentanyl for spinal anesthesia for urologic surgery. Anesth Analg. 2000;91:1452–6. doi: 10.1097/00000539-200012000-00029. 10.1097/00000539‐200012000‐00029 [DOI] [PubMed] [Google Scholar]
- 3. Fredman B, Sheffer O, Zohar E, Paruta I, Richter S, Jedeikin R, White PF. Fast‐track eligibility of geriatric patients undergoing short urologic surgery procedures. Anesth Analg. 2002;94:560–4. doi: 10.1097/00000539-200203000-00015. 10.1097/00000539‐200203000‐00015 [DOI] [PubMed] [Google Scholar]
- 4. Song D, Joshi GP, White PF. Fast‐track eligibility after ambulatory anesthesia: a comparison of desflurane, sevoflurane, and propofol. Anesth Analg. 1998;86:267–73.5. doi: 10.1097/00000539-199802000-00009. 10.1097/00000539‐199802000‐00009 [DOI] [PubMed] [Google Scholar]
- 5. Wong J, Marshall S, Chung F, Sinclair D, Song D, Tong D. Spinal anesthesia improves the early recovery profile of patients undergoing ambulatory knee arthroscopy. Can J Anaesth. 2001;48:323–5. doi: 10.1007/BF03014965. 10.1007/BF03014957 [DOI] [PubMed] [Google Scholar]
- 6. Vaghadia H. Spinal anaesthesia for outpatients: controversies and new techniques. Can J Anaesth. 1998;45:R64–75. doi: 10.1007/BF03019208. 10.1007/BF03019208 [DOI] [PubMed] [Google Scholar]
- 7. Stewart AV, Vaghadi H, Collins L, Mitchell GW. Small‐dose selective spinal anaesthesia for short‐duration outpatient gynaecological laparoscopy: recovery characteristics compared with propofol anaesthesia. Br J Anaesth. 2001;86:570–2. doi: 10.1093/bja/86.4.570. 10.1093/bja/86.4.570 PMID:11573635. [DOI] [PubMed] [Google Scholar]
- 8. Lennox PH, Chilvers C, Vaghadia H. Selective spinal anesthesia versus desflurane anesthesia in short duration outpatient gynecological laparoscopy: a pharmacoeconomic comparison. Anesth Analg. 2002;94:565–8. doi: 10.1097/00000539-200203000-00016. 10.1097/00000539‐200203000‐00016 table of contents. PMID: 11867376. [DOI] [PubMed] [Google Scholar]
- 9. White PF, Song D. New criteria for fast‐tracking after outpatient anesthesia: a comparison with the modified Aldrete's scoring system. Anesth Analg. 1999;88:1069–72. doi: 10.1097/00000539-199905000-00018. 10.1097/00000539‐199905000‐00018 [DOI] [PubMed] [Google Scholar]
- 10. Zohar E, Noga Y, Rislick U, Leibovitch I, Fredman B. Intrathecal anesthesia for elderly patients undergoing short transurethral procedures: a dose‐finding study. Anesth Analg. 2007;104:552–4. doi: 10.1213/01.ane.0000255329.55037.cd. 10.1213/01.ane.0000255329.55037.cd [DOI] [PubMed] [Google Scholar]
- 11. Koltka K, Abdülkerimov V, Küçükay S, Şentürk M, Pembeci K. Diz Atraskopilerinde Unilateral Spinal Anestezi ve Genel Anestezi Uygulamalarının Derlenme Özellikleri Açısından Karşılaştırılması. TARD. 2008;36:310–6. [Google Scholar]
- 12. Fredman B, Sheffer O, Zohar E, Paruta I, Richter S, Jedeikin R, et al. Fast‐track eligibility of geriatric patients undergoing short urologic surgery procedures. Anesth Analg. 2002;94:560–4. doi: 10.1097/00000539-200203000-00015. 10.1097/00000539‐200203000‐00015 [DOI] [PubMed] [Google Scholar]
- 13. Moemen ME. Selective spinal anaesthesia. EgJ Anaesth. 2003;19:99–106. [Google Scholar]
- 14. Liu SS, McDonald SB. Current issues in spinal anesthesia. Anesthesiology. 2001;94:888–906. doi: 10.1097/00000542-200105000-00030. 10.1097/00000542‐200105000‐00030 [DOI] [PubMed] [Google Scholar]
- 15. Korttila K. Recovery from outpatient anaesthesia:factors affecting outcome. Anaesthesia. 1995;50(Suppl):22–8. doi: 10.1111/j.1365-2044.1995.tb06186.x. 10.1111/j.1365‐2044.1995.tb06186.x [DOI] [PubMed] [Google Scholar]
- 16. Marshall SI, Chung F. Discharge criteria and complications after ambulatory surgery. Anesth Analg. 1999;88:508–17. doi: 10.1097/00000539-199903000-00008. 10.1097/00000539‐199903000‐00008 [DOI] [PubMed] [Google Scholar]
- 17. Ben‐David B, DeMeo PJ, Lucyk C, Solosko D. A comparison of minidose lidocaine‐fentanyl spinal anesthesia and local anesthesia/propofol infusion for outpatient knee arthroscopy. Anesth Analg. 2001;93:319–25. doi: 10.1097/00000539-200108000-00016. 10.1097/00000539‐200108000‐00016 2nd contents page. [DOI] [PubMed] [Google Scholar]
- 18. Ozmen S, Koşar A, Soyupek S, Armağan A, Hoşcan MB, Aydin C. The selection of the regional anaesthesia in the transurethral resection of the prostate (TURP) operation. Int Urol Nephrol. 2003;35:507–12. doi: 10.1023/b:urol.0000025616.21293.6c. 10.1023/B:UROL.0000025616.21293.6c [DOI] [PubMed] [Google Scholar]
- 19. Dobson PM, Caldicott LD, Gerrish SP, Cole JR, Channer KS. Changes in haemodynamic variables during transurethral resection of the prostate: comparison of general and spinal anaesthesia. Br J Anaesth. 1994;72:267–71. doi: 10.1093/bja/72.3.267. 10.1093/bja/72.3.267 [DOI] [PubMed] [Google Scholar]