In Clinical orthotopic liver transplantation (OLT), one of the more important factors that influence prognosis in the postoperative period is the extent of liver injury resulting from harvesting, preservation, and reperfusion of the donor organ.1
Agents that either enhance the reparative process or protect the liver from cellular damage are referred to as “hepatotrophic.” Cyclosporine A (CyA), a powerful immunosuppressive agent used clinically to prevent allograft rejection, has been shown to possess significant hepatotrophic action in the rat studied after partial hepatectomy.2–5 Recently, FK 506, an even more powerful new immunosuppressive agent, bas been shown to possess similar if not greater hepatotrophic activity.5
The purpose of the present study was to examine the efficacy of FK 506 in ameliorating the hepatic injury associated with experimental ischemia and reperfusion in rats.
MATERIALS AND METHODS
Male Lewis rats weighing 200–300 g were used for all of the experiments. A 60-minute period of total ischemia of the right lateral lobe of the liver was induced by occluding the right portal vein and hepatic artery using microvascular clamps under metofane inhalation anesthesia. This technique avoids occlusion of the left portal vein and the left hepatic artery during the ischemic period which, were they occluded, would result in splanchnic pooling of blood which can be lethal.6 Immediately after reperfusion, the nonischemic median and left lateral lobes of the liver were excised using the method of Higgins and Anderson.7
Prior to the hepatic ischemia, the rats were assigned to one of three different experimental groups (10 rats each). In group I (controls), 0.5 mL of saline solution was administered IV via the inferior vena cava (IVC) 30 minutes after the initiation of the ischemia. In groups 2 and 3, 0.3 mg kg of FK 506 were injected IV 30 minutes after and 24 hours before the initiation of the hepatic ischemia, respectively.
In a second experiment, five rats in groups 1 and 3 were killed at 24-hour intervals, from time 0 (end of the surgical procedure) to 72 hours after the operation. Immediately before killing, blood samples were obtained from each rat for the purpose of measuring serum levels of alanine aminotransferase (ALT) and lactate dehydrogenase (LDH). At the same time, a portion of the previously ischemic right hepatic lobe was freeze-clamped in liquid nitrogen for determination of its adenosine triphosphate (ATP) content.
All data are reported as mean values ± SEM. Comparisons between the means for each group were performed using Student’s t test. The chi-square test with the Yates correction was used to compare the proportions of surviving rats between groups. A P value of <.05 was considered to be statistically significant.
RESULTS
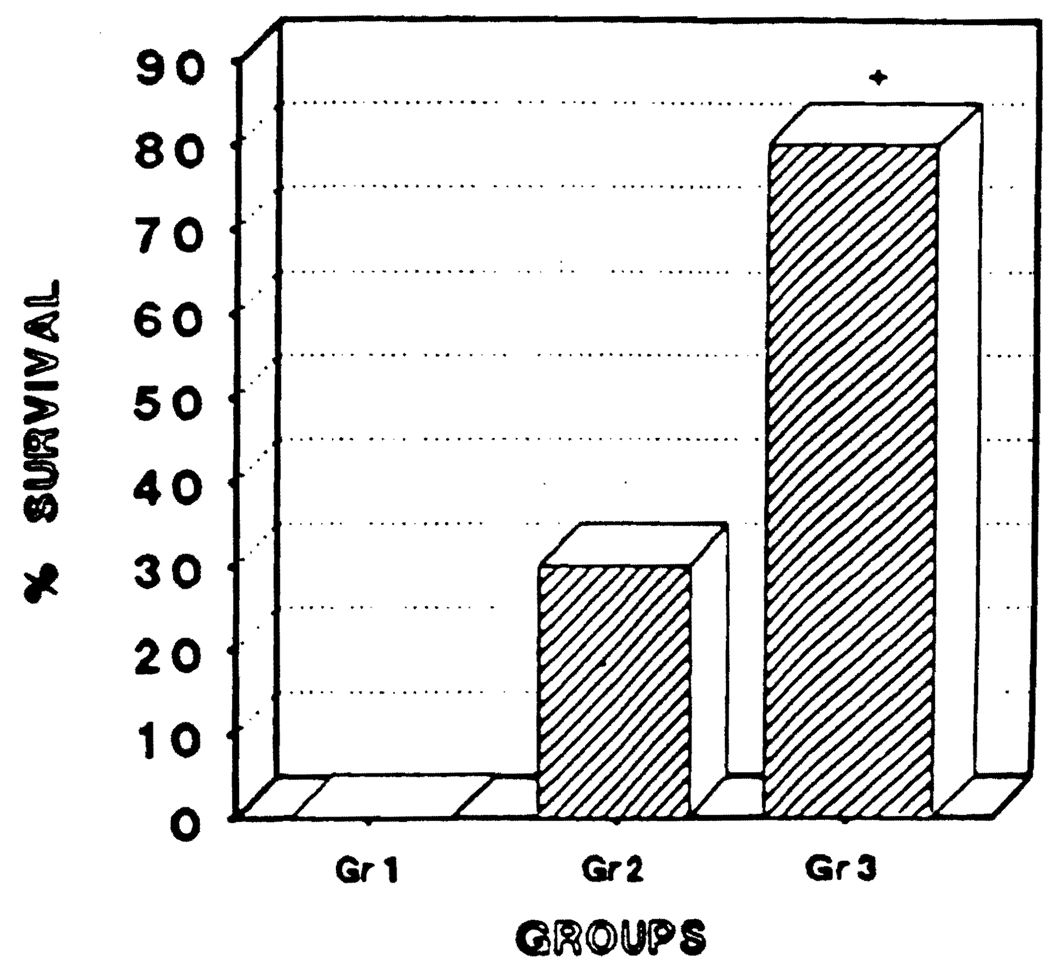
The control rats (100%) died within 72 hours after the initiation of the ischemia. The 10-day survival rates for the rats in groups 2 and 3 were, respectively, 30% and 80% (P < .01) (Fig 1).
Fig 1.
Percent survival at 10 days of the animals studied (+ = P < .01).
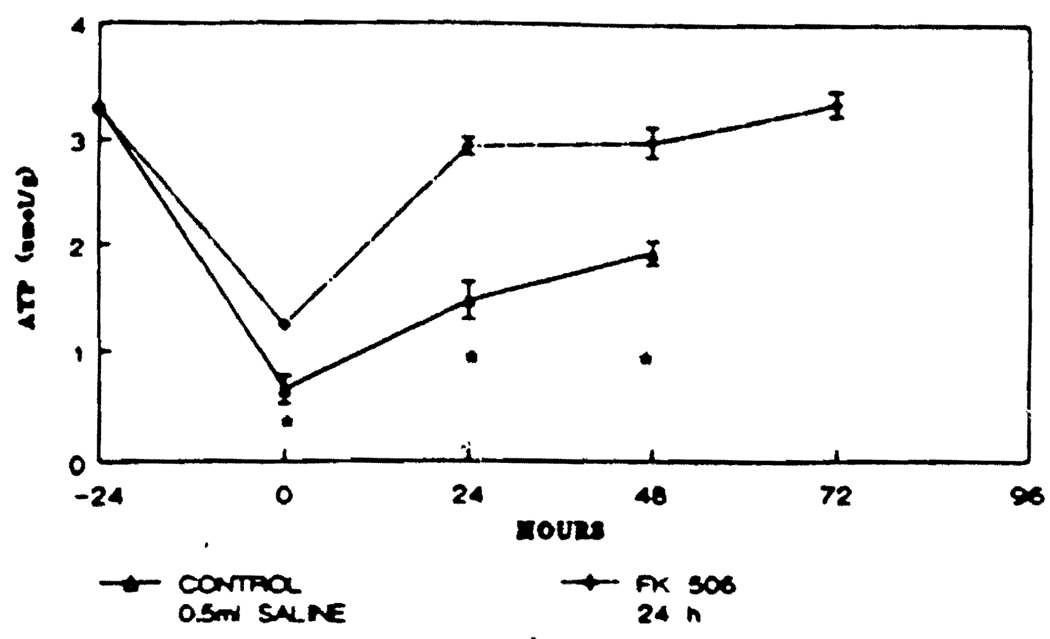
FK 506 pretreatment significantly increased the hepatic ATP content at each time interval considered with respect to the control group (P < .05). In the FK 506 pretreatment group, the hepatic ATP content returned to preischemic values (3–3.5 µumol/g) within 24 hours and was maintained at that level thereafter (Fig 2).
Fig 2.
Hepatic ATP content in the animals studied. Points represent mean values and bracket represent SEM (* = P < .05).
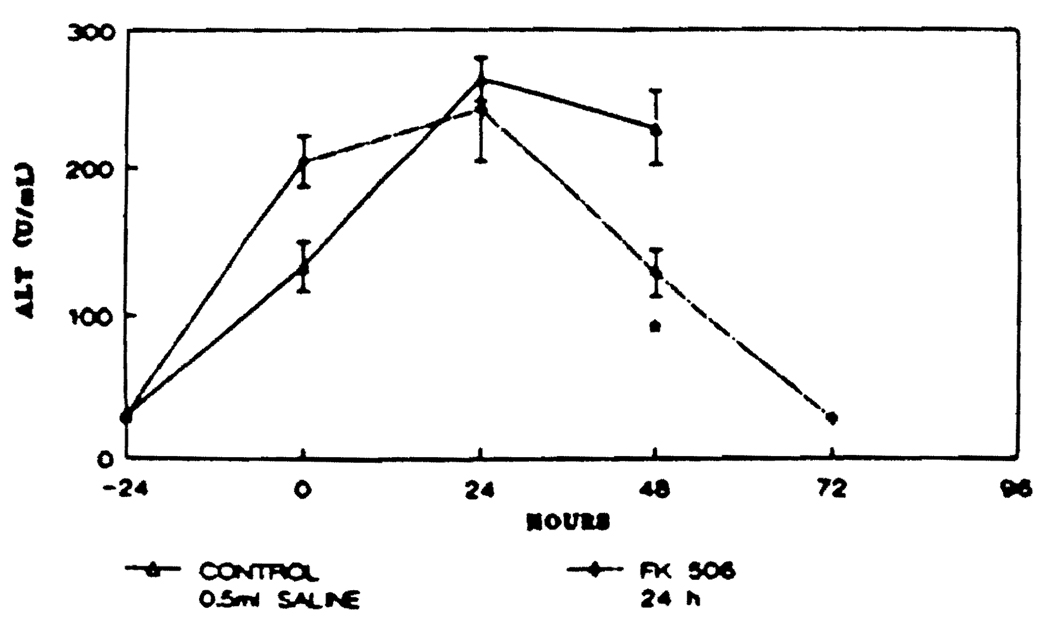
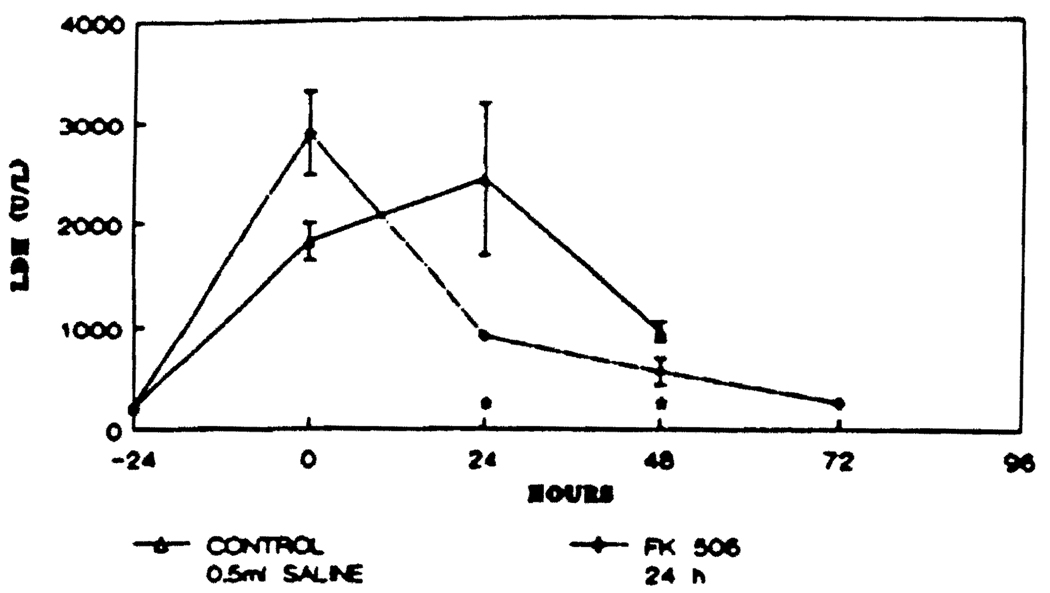
In both the control and the FK 506 pretreatment groups, an increase in the level of ALT was observed at time 0 and at 24 hours postoperatively but declined thereafter. When the peak values were compared between groups, the ALT level was significantly lower in the rats pretreated with FK 506 than in the control rats at 48 hours postoperatively (P < .05). Moreover, the ALT level in the FK 506-pretreated rats reached the normal range (preischemic) at 72 hours postischemia (Fig 3). Finally, the LDH level was significantly lower in the FK 506-pretreated rats compared with the levels seen in the control rats at 24 and 48 hours postischemia (P < .05) (Fig 4).
Fig 3.
Serum ALT levels in the animals studied. Points represent mean values and brackets represent SEM (* = P < .05).
Fig 4.
Serum LDH levels in the animals studied. Points represent mean values and brackets represent SEM (* = P < 0.05).
DISCUSSION
In this model, a 70% hepatectomy involving the median and left lateral hepatic lobes is performed immediately after a 60-minute period of total ischemia of the right lateral lobe of the liver. Subsequent survival of the rats is dependent upon the ability of the residual ischemic right lobe of the liver to regenerate and recover from the ischemic injury.
Previous experiments have shown that the hepatic content of DNA and the mitotic activity in the liver of the rat after a 70% hepatectomy increase significantly as a result of CyA exposure, and even more markedly following exposure to FK 506.5 Furthermore, in the dog Eck-fistula model, CyA has been shown to prevent hepatocellular atrophy and to increase the low rate of hepatocyte hyperplasia characteristic of the model. The effect of an infusion of FK 506 at a much lower dose in this model was similar.8
The possibility of a link between the immune system and hepatic regeneration has been suggested.5,9,10 It is conceivable that ischemic hepatic injury may activate a cytotoxic autoimmune reaction against hepatocytes and other cells present in the liver, as a consequence of an induced structural alteration of the liver cell membrane caused by ischemia, and thereby impair the ability of liver cells to regenerate.11 It is equally possible that the hepatotrophic qualities of FK 506 and CyA are independent from immunosuppression as has been discussed by Starzl et al.12 A biochemical mechanism is supported by our demonstration of a faster and more complete restoration of hepatic ATP. We conclude that FK 506 pretreatment maintains the hepatic ATP content and reduces the extent of necrosis following hepatic ischemia. These actions may allow the liver to regenerate and recover from the ischemic injury.
Acknowledgments
This work was supported in part by grants from the NIDDK 32556, 39789, and NIAAA 06601.
REFERENCES
- 1.Starzl TE, Iwatsuki S, Van Thiel DH, et al. Hepatology. 1982;2:614. doi: 10.1002/hep.1840020516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Makowka L, Svanas G, Esquival C, et al. Surg Forum. 1986;37:352–354. [PMC free article] [PubMed] [Google Scholar]
- 3.Kim YI, Calne RY, Nagassue N. Surg Gynecol Obstet. 1988;166:317. [PubMed] [Google Scholar]
- 4.Kahn D, Lai HS, Romovacek H, et al. Transplant Proc. 1988;20:850–852. [PMC free article] [PubMed] [Google Scholar]
- 5.Francavilla A, Barone M, Todo S, et al. Lancet. 1989;2:1248. doi: 10.1016/s0140-6736(89)91853-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meer C, Kley GA, Valkenburg PW. Circ Shock. 1976;3:191. [Google Scholar]
- 7.Higgins GM, Anderson RM. Arch Pathol. 1931;12:186. [Google Scholar]
- 8.Mazzafero V, Scotti-Foglieni CL, Porter KA, et al. Transplant Proc. 1990;22:93. [PMC free article] [PubMed] [Google Scholar]
- 9.Sakai A, Pfefferman R, Kountz SL. Surg Gynecol Obstet. 1976;43:914. [PubMed] [Google Scholar]
- 10.Flye MW, Yu S. Transplantation. 1990;49:581. doi: 10.1097/00007890-199003000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Kawano K, Kim Y, Kaketani K, et al. Transplantation. 1989;48:759. doi: 10.1097/00007890-198911000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Starzl TE, Porter KA, Mazzaferro V, et al. Transplantation. doi: 10.1097/00007890-199101000-00010. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]