Abstract
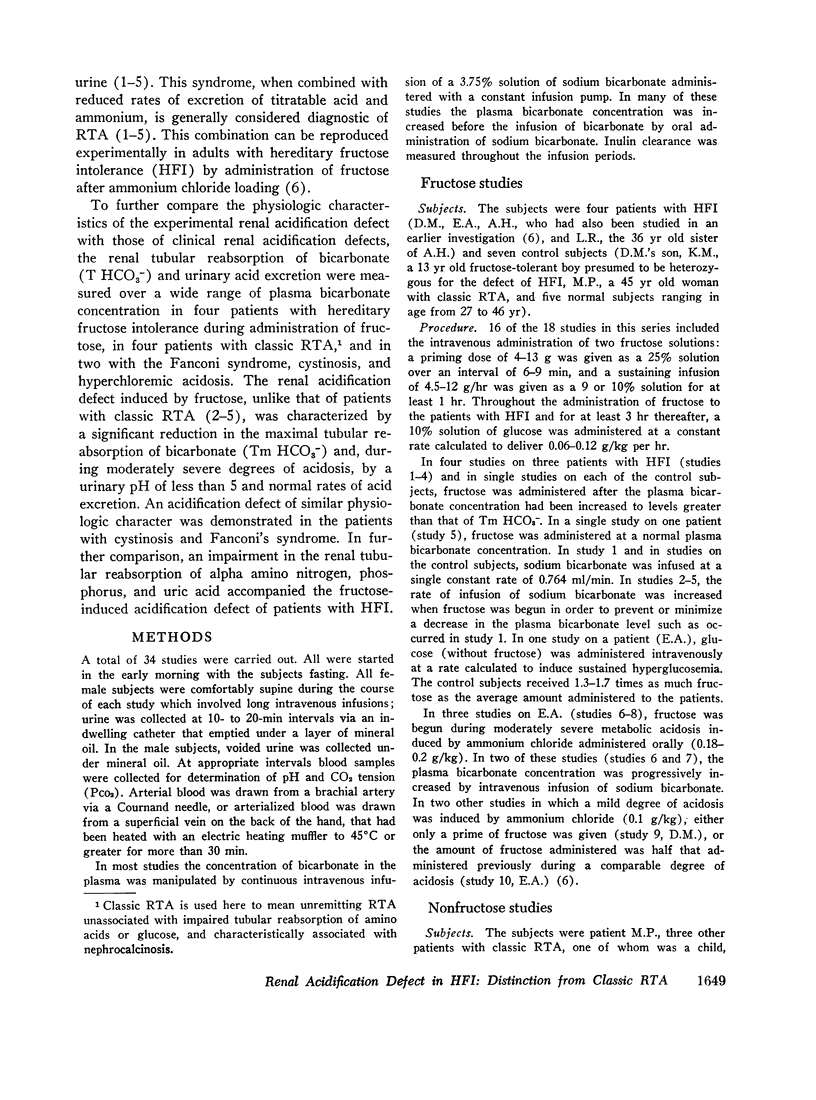
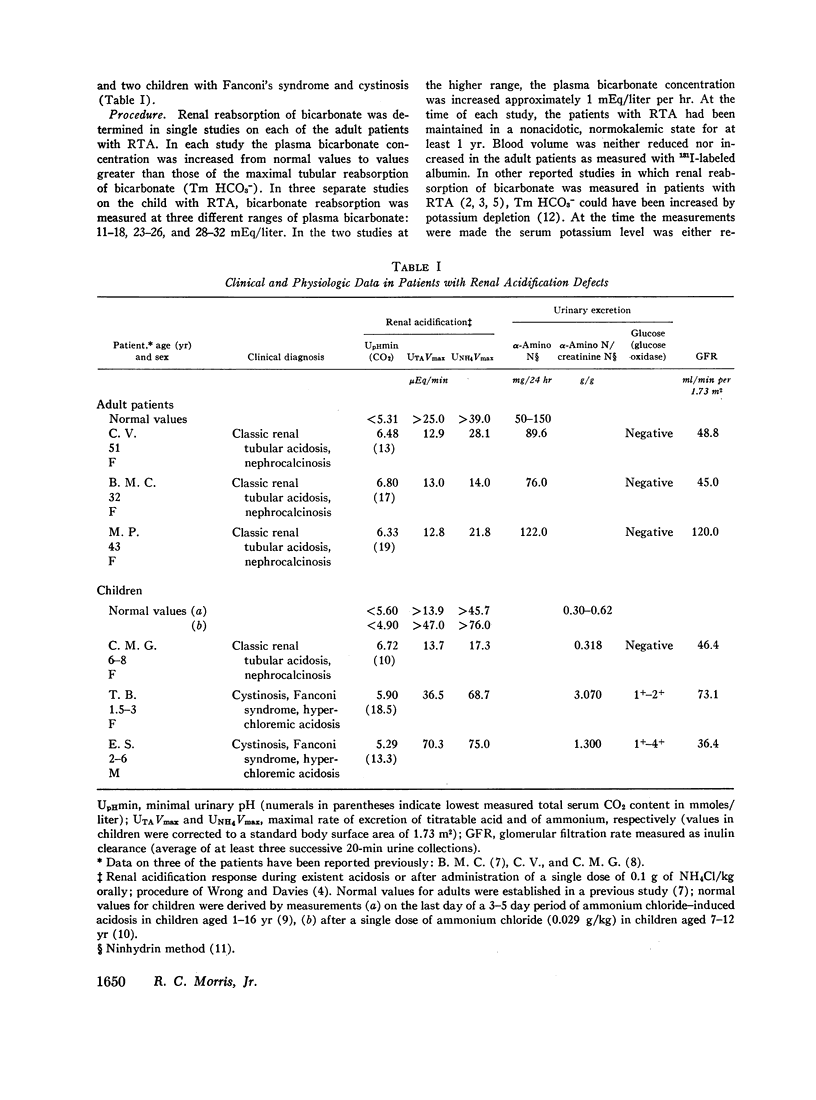
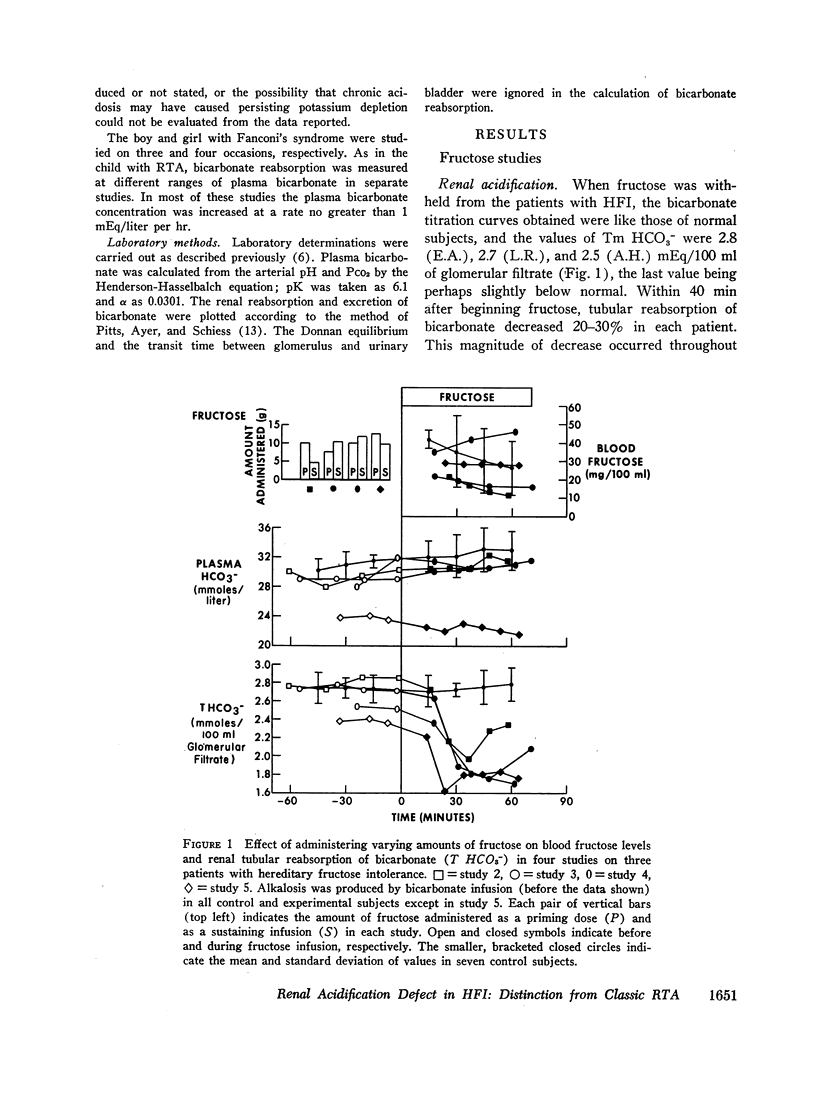
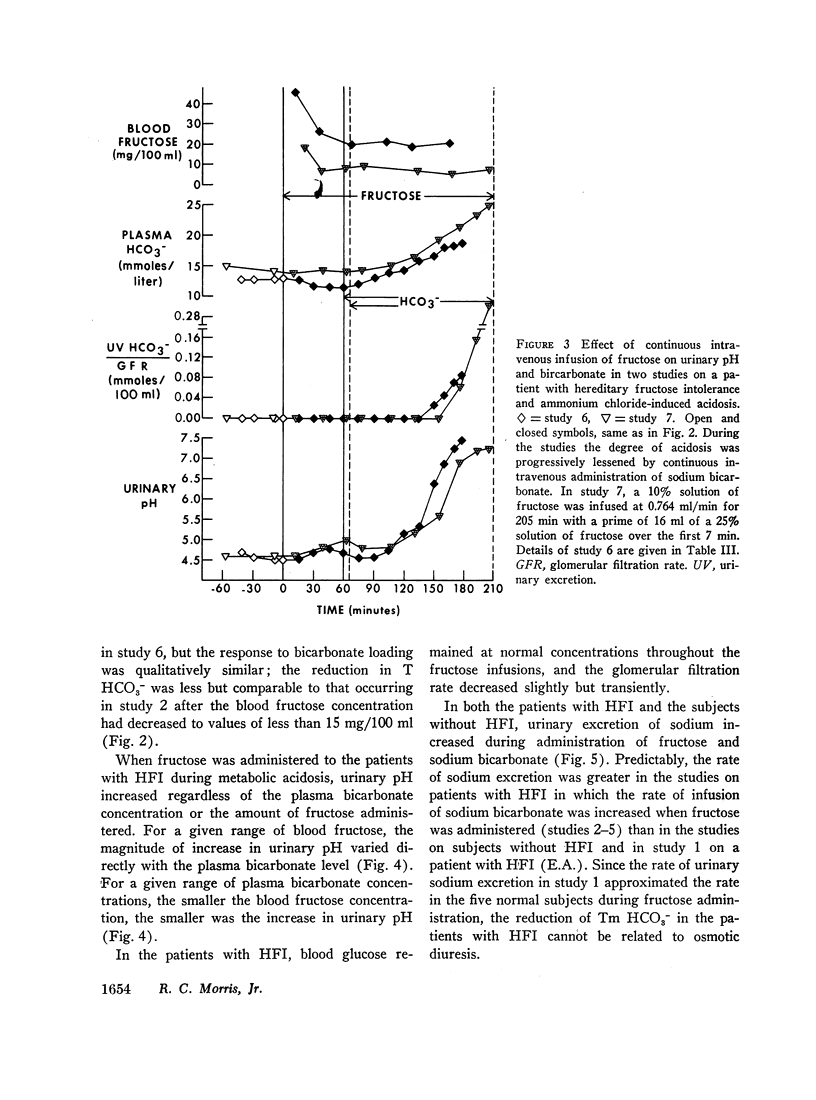
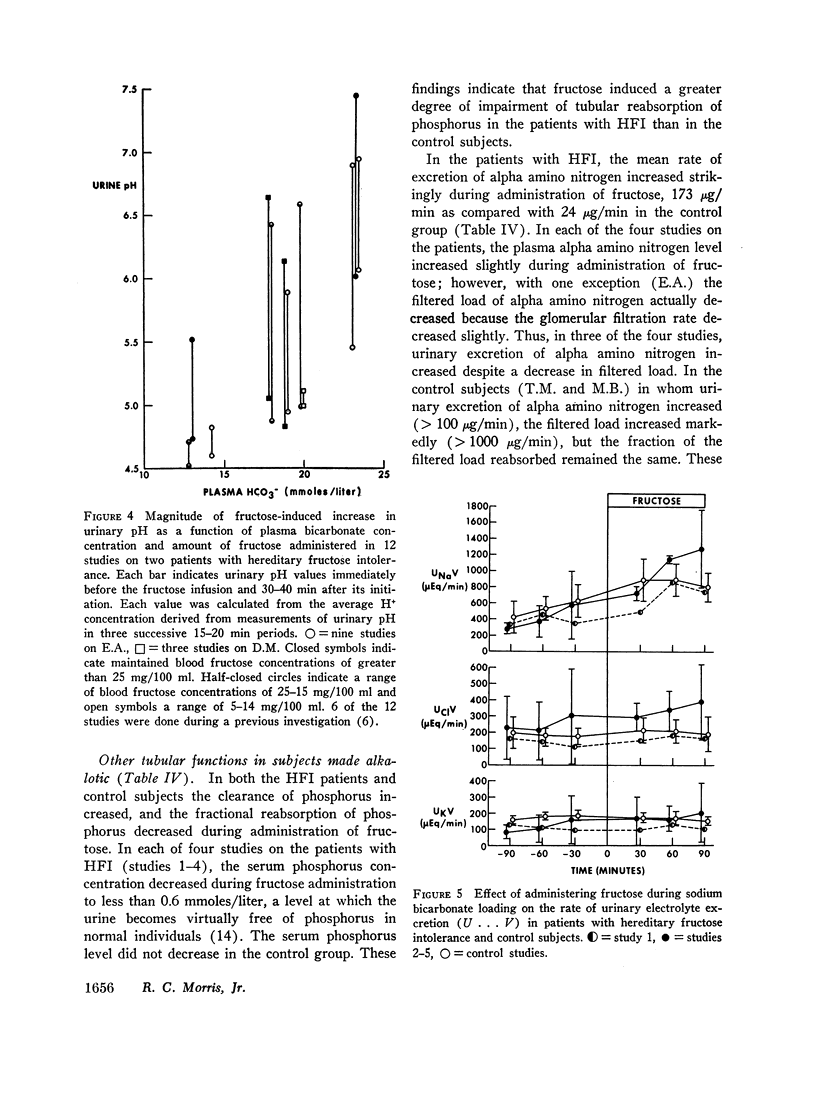
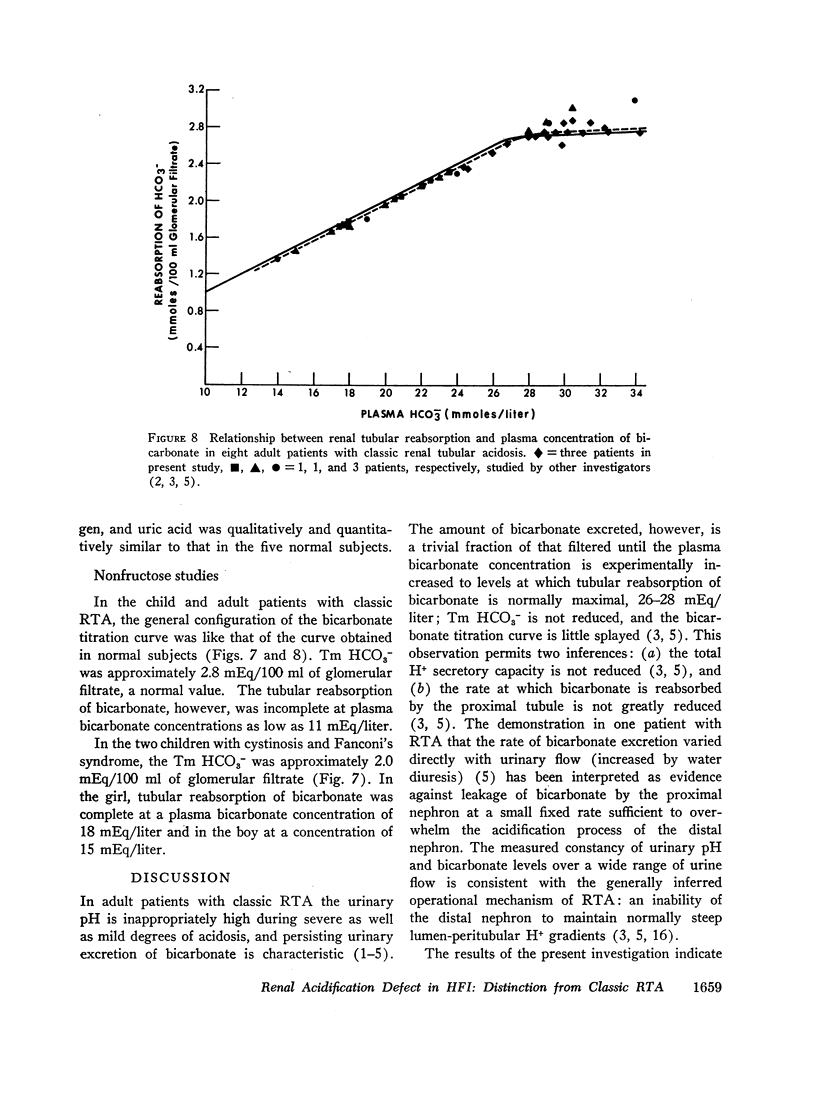
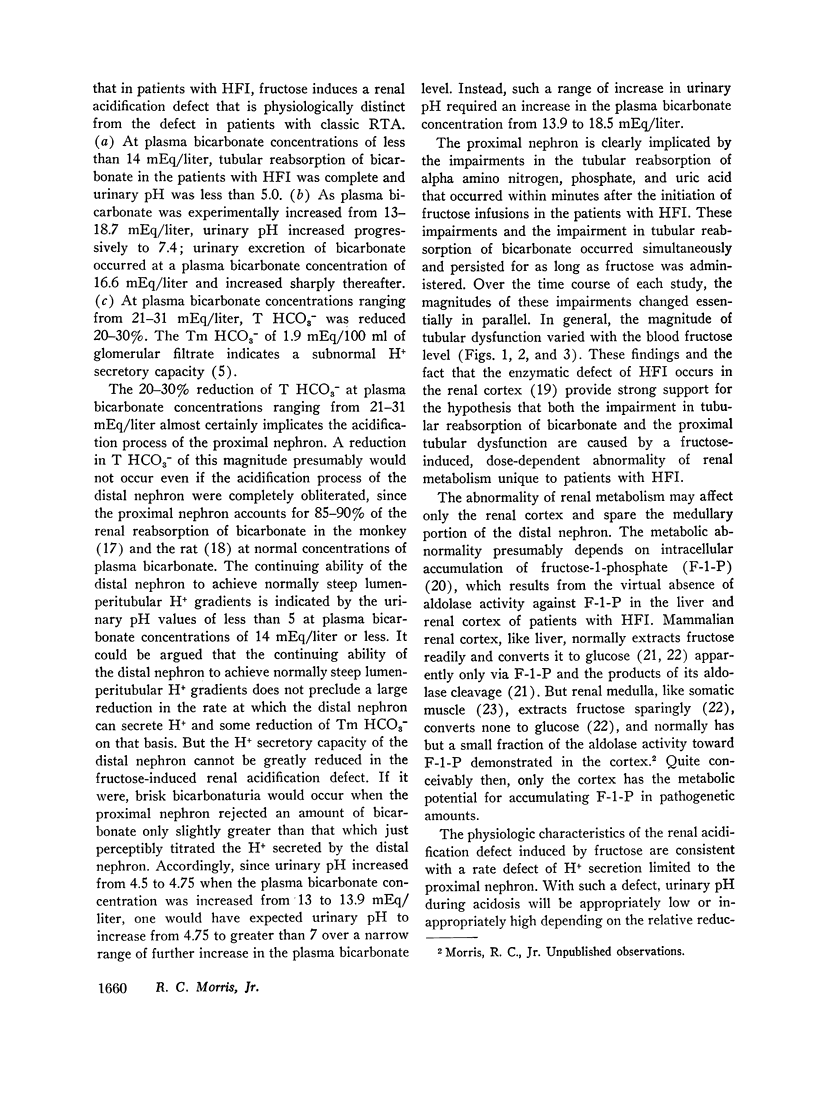
In adult patients with hereditary fructose intolerance (HFI) fructose induces a renal acidification defect characterized by (a) a 20-30% reduction in tubular reabsorption of bicarbonate (T HCO3-) at plasma bicarbonate concentrations ranging from 21-31 mEq/liter, (b) a maximal tubular reabsorption of bicarbonate (Tm HCO3-) of approximately 1.9 mEq/100 ml of glomerular filtrate, (c) disappearance of bicarbonaturia at plasma bicarbonate concentrations less than 15 mEq/liter, and (d) during moderately severe degrees of acidosis, a sustained capacity to maintain urinary pH at normal minima and to excrete acid at normal rates. In physiologic distinction from this defect, the renal acidification defect of patients with classic renal tubular acidosis is characterized by (a) just less than complete tubular reabsorption of bicarbonate at plasma bicarbonate concentrations of 26 mEq/liter or less, (b) a normal Tm HCO3- of approximately 2.8 mEq/100 ml of glomerular filtrate, and (c) during acidosis of an even severe degree, a quantitatively trivial bicarbonaturia, as well as (d) a urinary pH of greater than 6.
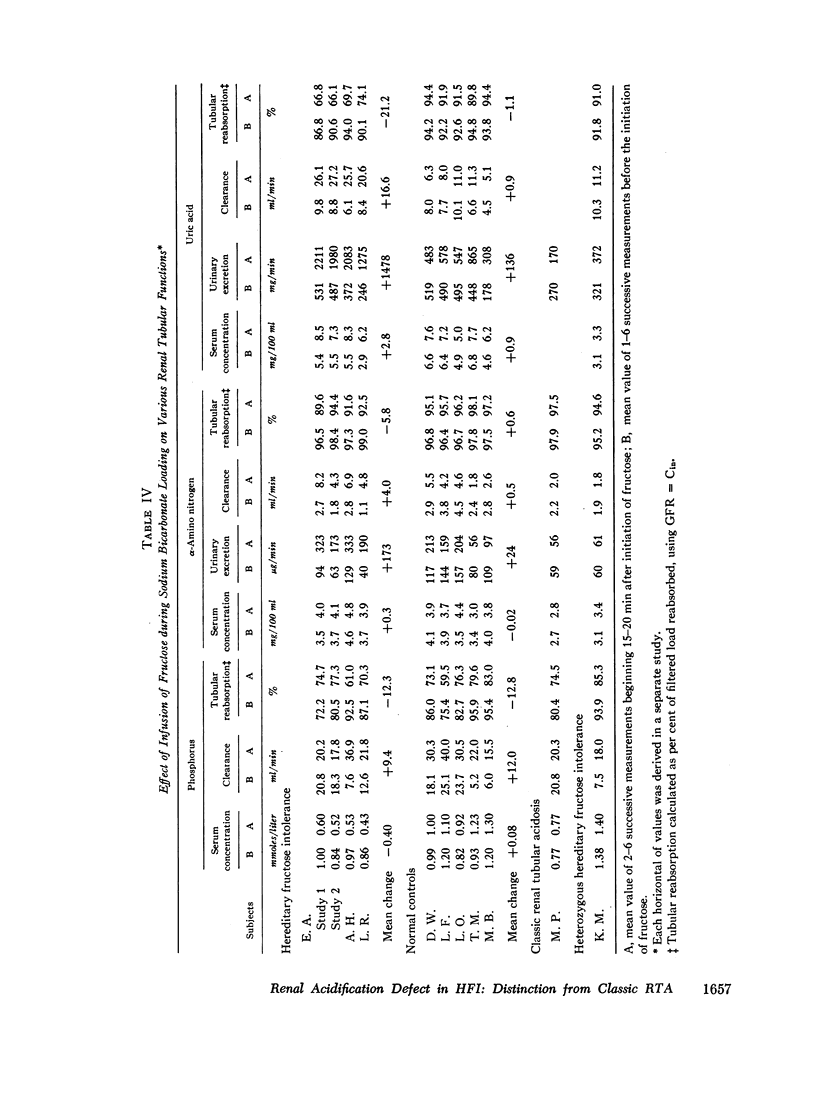
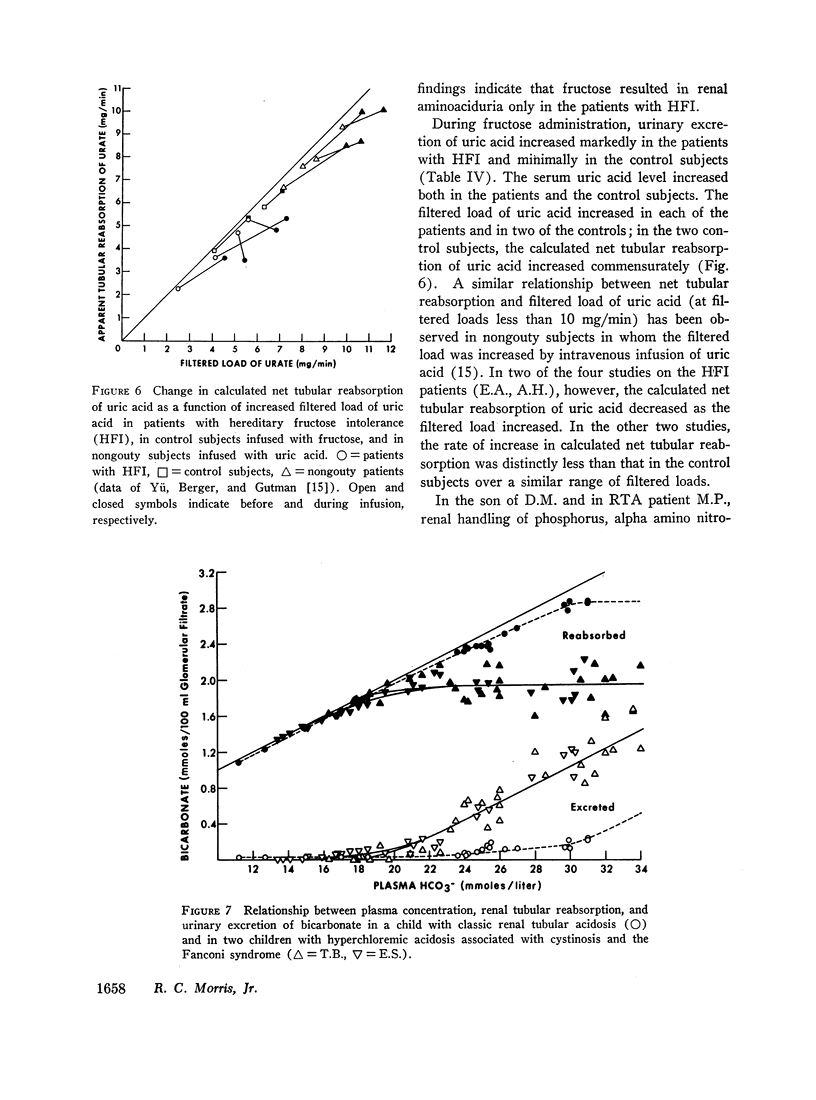
That the fructose-induced renal acidification defect involves a reduced H+ secretory capacity of the proximal nephron is supported by the magnitude of the reduction in T HCO3- (20-30%) and the simultaneous occurrence and the persistence throughout administration of fructose of impaired tubular reabsorption of phosphate, alpha amino nitrogen and uric acid.
A reduced H+ secretory capacity of the proximal nephron also appears operative in two unrelated children with hyperchloremic acidosis, Fanconi's syndrome, and cystinosis. In both, T HCO3- was reduced 20-30% at plasma bicarbonate concentrations ranging from 20-30 mEq/liter. The bicarbonaturia disappeared at plasma bicarbonate concentrations ranging from 15-18 mEq/liter, and during moderate degrees of acidosis, urinary pH decreased to less than 6, and the excretion rate of acid was normal.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BABER M. D. A case of congenital cirrhosis of the liver with renal tubular defects akin to those in the Fanconi syndrome. Arch Dis Child. 1956 Oct;31(159):335–339. doi: 10.1136/adc.31.159.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett C. M., Brenner B. M., Berliner R. W. Micropuncture study of nephron function in the rhesus monkey. J Clin Invest. 1968 Jan;47(1):203–216. doi: 10.1172/JCI105710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett W. M., Hempel K. H., Berland J. E., Porter G. A. Renal tubular acidosis. Arch Intern Med. 1968 Jan;121(1):81–86. [PubMed] [Google Scholar]
- CARRE I. J., WOOD B. S., SMALLWOOD W. C. Idiopathic renal acidosis in infancy. Arch Dis Child. 1954 Aug;29(146):326–333. doi: 10.1136/adc.29.146.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DENT C. E. Rickets and osteomalacia from renal tubule defects. J Bone Joint Surg Br. 1952 May;34-B(2):266–274. doi: 10.1302/0301-620X.34B2.266. [DOI] [PubMed] [Google Scholar]
- Edelmann C. M., Soriano J. R., Boichis H., Gruskin A. B., Acosta M. I. Renal bicarbonate reabsorption and hydrogen ion excretion in normal infants. J Clin Invest. 1967 Aug;46(8):1309–1317. doi: 10.1172/JCI105623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HENNEMAN P. H., DEMPSEY E. F., CARROLL E. L., HENNEMAN D. H. Acquired vitamin D-resistant osteomalacia: a new variety characterized by hypercalcemia, low serum bicarbonate and hyperglycinuria. Metabolism. 1962 Jan;11:103–116. [PubMed] [Google Scholar]
- KHACHADURIAN A., KNOX W. E., CULLEN A. M. Colorimetric ninhydrin method for total alpha amino acids of urine. J Lab Clin Med. 1960 Aug;56:321–332. [PubMed] [Google Scholar]
- LEE J. B., VANCE V. K., CAHILL G. F., Jr Metabolism of C14-labeled substrates by rabbit kidney cortex and medulla. Am J Physiol. 1962 Jul;203:27–36. doi: 10.1152/ajplegacy.1962.203.1.27. [DOI] [PubMed] [Google Scholar]
- LIGHTWOOD R., PAYNE W. W., BLACK J. A. Infantile renal acidosis. Pediatrics. 1953 Dec;12(6):628–644. [PubMed] [Google Scholar]
- LITIN R. B., RANDALL R. V., GOLDSTEIN N. P., POWER M. H., DIESSNER G. R. Hypercalciuria in hepatolenticular degeneration (Wilson's disease). Am J Med Sci. 1959 Nov;238:614–620. [PubMed] [Google Scholar]
- Morris R. C., Jr An experimental renal acidification defect in patients with hereditary fructose intolerance. I. Its resemblance to renal tubular acidosis. J Clin Invest. 1968 Jun;47(6):1389–1398. doi: 10.1172/JCI105830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris R. C., Jr, Fudenberg H. H. Impaired renal acidification in patients with hypergammaglobulinemia. Medicine (Baltimore) 1967 Jan;46(1):57–69. doi: 10.1097/00005792-196701000-00003. [DOI] [PubMed] [Google Scholar]
- Morris R. C., Jun, Ueki I., Loh D., Eanes R. Z., McLin P. Absence of renal fructose-1-phosphate aldolase activity in hereditary fructose intolerance. Nature. 1967 May 27;214(5091):920–921. doi: 10.1038/214920b0. [DOI] [PubMed] [Google Scholar]
- Morris R. C., Piel C. F., Audioun E. Renal tubular acidosis. Effects of sodium phosphate and sulfate on renal acidification in two patients with renal tubular acidosis. Pediatrics. 1965 Dec;36(6):899–904. [PubMed] [Google Scholar]
- PEONIDES A., LEVIN B., YOUNG W. F. THE RENAL EXCRETION OF HYDROGEN IONS IN INFANTS AND CHILDREN. Arch Dis Child. 1965 Feb;40:33–39. doi: 10.1136/adc.40.209.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitts R. F., Ayer J. L., Schiess W. A., Miner P. THE RENAL REGULATION OF ACID-BASE BALANCE IN MAN. III. THE REABSORPTION AND EXCRETION OF BICARBONATE. J Clin Invest. 1949 Jan;28(1):35–44. doi: 10.1172/JCI102050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RELMAN A. S. RENAL ACIDOSIS AND RENAL EXCRETION OF ACID IN HEALTH AND DISEASE. Adv Intern Med. 1964;12:295–347. [PubMed] [Google Scholar]
- RENOLD A. E., THORN G. W. Clinical usefulness of fructose. Am J Med. 1955 Aug;19(2):163–168. doi: 10.1016/0002-9343(55)90370-3. [DOI] [PubMed] [Google Scholar]
- REYNOLDS T. B. Observations on the pathogenesis of renal tubular acidosis. Am J Med. 1958 Oct;25(4):503–515. doi: 10.1016/0002-9343(58)90040-8. [DOI] [PubMed] [Google Scholar]
- SALOMON L. L., LANZA F. L., SMITH D. E. Renal conversion of fructose to glucose. Am J Physiol. 1961 Apr;200:871–877. doi: 10.1152/ajplegacy.1961.200.4.871. [DOI] [PubMed] [Google Scholar]
- SMITH L. H., Jr, SCHREINER G. E. Studies on renal hyperchloremic acidosis. J Lab Clin Med. 1954 Mar;43(3):347–358. [PubMed] [Google Scholar]
- STANBURY S. W. Some aspects of disordered renal tubular function. Adv Intern Med. 1958;9:231–282. [PubMed] [Google Scholar]
- WORTHEN H. G., GOOD R. A. The de Toni-Fanconi syndrome with cystinosis; clinical and metabolic study of two cases in a family and a critical review on the nature of the syndrome. AMA J Dis Child. 1958 Jun;95(6):653–688. [PubMed] [Google Scholar]
- WRONG O., DAVIES H. E. The excretion of acid in renal disease. Q J Med. 1959 Apr;28(110):259–313. [PubMed] [Google Scholar]
- YU T. S., BERGER L., GUTMAN A. B. Renal function in gout. II. Effect of uric acid loading on renal excretion of uric acid. Am J Med. 1962 Dec;33:829–844. doi: 10.1016/0002-9343(62)90215-2. [DOI] [PubMed] [Google Scholar]
- York S. E., Yendt E. R. Osteomalacia associated with renal bicarbonate loss. Can Med Assoc J. 1966 Jun 25;94(26):1329–1342. [PMC free article] [PubMed] [Google Scholar]



