Abstract
Background
We previously reported that the majority of women seeking bariatric surgery had female sexual dysfunction (FSD) as defined by the validated Female Sexual Function Index (FSFI).
Objective
The current study examined whether FSD resolves after bariatric surgery.
Setting
The Miriam Hospital, Providence RI, USA.
Methods
Fifty-four reportedly sexually active women (43.3±9.5 years) completed the FSFI pre- and 6-months post-operatively after a mean excess weight loss (%EWL) of 42.3% [Laparoscopic adjustable gastric banding (LAGB) n=38; %EWL=34.6±15.7; Roux-en-Y gastric bypass (RYGB) n=16; %EWL=60.0±21.2). The FSFI assesses sexual function across six domains with higher scores indicating better sexual function. Summing of these scores yields a FSFI-total score (range=2–36 with ≤26.55=FSD).
Results
Before surgery, 34 women (63%) had scores indicative of FSD. By 6-months after surgery, FSD had resolved in 23 of these 34 (68%) women, and only 1 woman developed FSD. In the entire sample, there were significant (p<0.05) improvements from pre- to post-surgery on all FSFI domains. FSFI-total scores improved after LAGB (24.2±5.9 to 29.1±4.1, p<0.001) and RYGB (23.7±7.7 to 30.0±4.7, p<0.001). In regression analyses, being married, younger age, and worse preoperative sexual function were related to greater sexual function improvements. Postoperatively, participants’ FSFI-total scores were indistinguishable from published normative controls (29.4±4.3 vs. 30.5±5.3, p=0.18).
Conclusion
FSD resolved in a large percentage of women. Sexual functioning in the entire sample improved to levels consistent with normative controls. This improvement in sexual function did not depend on surgery type or weight loss amount, and appears to be an additional benefit for women undergoing bariatric surgery.
Keywords: Sexual Dysfunction, Women, Bariatric Surgery, Female Sexual Function Index
Introduction
Female sexual dysfunction (FSD) is characterized by impairments in the sexual response cycle and pain during or after intercourse [1]. While initially conceptualized as a purely psychological phenomenon, FSD is now considered to be a multifactorial problem with neurobiological, hormonal, and psychosocial components that combine to undermine women’s health, quality of life and relationships [2, 3]. It is estimated that up to 43% of women are affected by some form of FSD [4, 5], with higher rates linked to increasing age and decreasing estrogen [2]. Increased risk of FSD and lower sexual functioning is also related to a host of medical conditions [6], including obesity [7–11].
Obese women seeking bariatric surgery appear to be at particularly high risk for experiencing FSD. Research by Kolotkin and colleagues [12–14] has demonstrated that women seeking gastric bypass surgery report lower sexual quality of life than obese individuals in non-surgical weight loss programs and equally overweight controls. Two studies [15, 16] have shown disturbances in sexual functioning among female bariatric surgery candidates via use of the Female Sexual Function Index (FSFI) [17]. In the first study [15], surgery patients reported greater sexual impairment overall and on most individual domains of sexual function, compared to healthy controls similar in age, marital status, and education. However, this study did not indicate the number of patients with FSD. In the second study [16], the majority (60%) of bariatric surgery candidates met criteria for FSD and the entire sample exhibited a low level of sexual functioning relative to published normative controls [17].
Only a small group of studies have examined whether obesity-related disturbances in female sexual functioning are alleviated following bariatric surgery. Camps et al. [18] surveyed 28 patients before surgery and at ≥ 1 year after surgery. Patients reported improvements in frequency and enjoyment of sexual intercourse, orgasmic function, and body image. Similarly, in another investigation of 82 patients, the majority (63%) reported finding sexual intercourse more enjoyable at ≥ 1-year postoperatively [19]. Finally, other studies have shown postoperative enhancement of female sexual function within the context of a subjective quality of life assessment [20, 21]. However, none of these studies employed validated measures to systematically assess the extent to which established domains of female sexual function improve and clinical FSD resolves postoperatively.
Therefore, the purpose of the current study was to use the FSFI, a validated measure, to examine whether FSD resolves at 6-months post-surgery. Additionally, we assessed whether participants’ FSFI-total and individual domain scores improved postoperatively to levels similar to those of published normative controls [17].
Methods
Participants and procedures
Participants were severely obese (BMI ≥ 35 kg/m2) adult (21–75 years of age) women who were reportedly involved in a stable, sexually active partner relationship and preparing to undergo either Roux-en-Y gastric bypass (RYGB) or laparoscopic adjustable gastric banding (LAGB). Recruitment, screening, and preoperative measurement procedures have been reported in detail previously [16]. Participants had their height and weight measured and completed questionnaires assessing demographics, health history, medication usage, and sexual function, in one of three clinics on average 104 ± 75 days before surgery. Sexual function, medication usage, and weight were measured again at 6-months (194 ± 40 days) after surgery. Participants did not receive payment for completing the study. The study procedures were approved by The Miriam Hospital Institutional Review Board, Providence, RI, USA.
Seventy-seven women completed measures preoperatively and reached 6-month follow-up, meeting initial criteria for study inclusion. Of these 77, 63 (82%) completed measures post-operatively. Compared with non-completers, completers did not differ on preoperative FSFI-total scores, demographics or BMI. Among the completers, 9 reported that they were sexually inactive during the previous 4 weeks either preoperatively (n=2), postoperatively (n=5), or at both time points (n=2). These participants were excluded from analyses as the FSFI is designed for use in participants who have engaged in some level of sexual activity during the measurement period(s) [17]. As a result, the final sample consisted of 54 participants.
Measures
Demographic characteristics, health history, and medication usage
Before surgery, participants completed a demographics questionnaire and a health history checklist. Participants were asked to list the names of medications they were currently taking before and after surgery.
Sexual function and dysfunction
The Female Sexual Function Index (FSFI) [17] was used to measure sexual function and to differentiate participants with and without FSD. The FSFI is a 19-item questionnaire that assesses level of sexual functioning during the past month across 6 domains: 1) sexual desire (assessed as frequency and desire level), 2) sexual arousal (assessed as frequency, level, confidence and satisfaction), 3) lubrication (assessed as frequency, difficulty, frequency of maintaining and difficulty in maintaining), 4) orgasm (frequency, difficulty, and satisfaction), 5) sexual satisfaction (assessed as the amount of closeness with partner, sexual relationship and overall sex life), and 6) sexual pain (assessed as pain frequency during vaginal penetration and pain frequency following vaginal penetration). The FSFI provides scores for each domain as well as a total score, with higher scores indicating better sexual function (sexual desire: 1.2–6; sexual satisfaction: 0.8–6; sexual arousal, lubrication, orgasm, and sexual pain: 0–6; total: 2–36). The FSFI is shown to have psychometric and clinical validity as well as high test-retest reliability for each of the individual domains [17]. We used the validated FSFI-total cut-off score of 26.55 to classify women with and without FSD [22].
Statistical analyses
Statistical analyses were conducted using the Statistical Package for Social Sciences, version 14.0 (SPSS for Windows, SPSS, Chicago, IL). McNemar’s chi square test was used to examine differences in the proportion of participants with FSD across the pre- and post-operative time points. Paired samples t-tests were used to assess pre-to post-operative changes in FSFI-total and individual domain scores. Analysis of covariance (ANCOVA) was used to examine changes in FSFI-total scores by surgery type (LAGB vs RYGB), adjusting for age, marital status, and preoperative FSFI scores. Similar ANCOVA procedures were performed to assess changes in FSFI-total scores as a function of pre- and post-operative antidepressant medication use, given that FSD is a common side effect of such medications [23]. Regression analyses were conducted to examine multivariate predictors of pre- to post-operative changes in FSFI-total scores. For these analyses, a hierarchical two-step procedure was employed in which demographic (age and marital status) and preoperative variables (BMI, FSFI-total scores) were entered in the first step, and postoperative weight loss and type of surgical procedure were entered in the second step. Finally, we compared participants’ FSFI scores at the pre- and postoperative time points with published normative controls [17] using t-tests. All tests were two-tailed and statistical significance was set at p < 0.05.
Results
Participants
Preoperative characteristics of participants are presented in Table 1. On average, participants were aged 43 years (range = 25 to 61 years) and predominantly Caucasian (89%) and married (81%). Half (50%) of participants had at least a 4-year college/university degree. The most commonly reported diagnosed health conditions preoperatively were depression (48%), and hypertension (44%). Slightly less than one third (30%) of participants had experienced menopause. Medications most commonly taken preoperatively were those to treat depression (44%) and gastroesophageal reflux disease (32%). The average BMI among participants was 45 kg/m2 (range = 35 to 67).
Table 1.
Preoperative participant characteristics
| Age (M ± SD years) | 43.3 ± 9.5 |
|---|---|
| Race (%) | |
| Caucasian | 88.9 |
| Hispanic | 7.4 |
| African American | 3.7 |
| Marital Status (%) | |
| Married | 81.5 |
| Divorced | 11.2 |
| Single | 7.3 |
| Education (%) | |
| < 4 years college | 50.0 |
| ≥ 4 years college | 50.0 |
| Gynecological health events/conditions (%) | |
| Menopause | 29.6 |
| Gynecological surgery | 29.6 |
| Urinary tract symptoms | 20.4 |
| Polycystic ovary syndrome | 11.1 |
| Frequently reported health conditions (%) | |
| Depression | 48.1 |
| Hypertension | 44.4 |
| Anxiety disorder | 35.2 |
| Diabetes | 18.5 |
| Abnormal thyroid | 14.8 |
| Frequently reported medications (%) | |
| Antidepressants | 44.4 |
| Antireflux | 31.5 |
| Cholesterol-lowering agents | 20.4 |
| β-blockers | 16.7 |
| Oral diabetes medications | 14.8 |
| BMI (M ± SD kg/m2) | 45.1 ± 6.8 |
Pre- and post-operative female sexual function
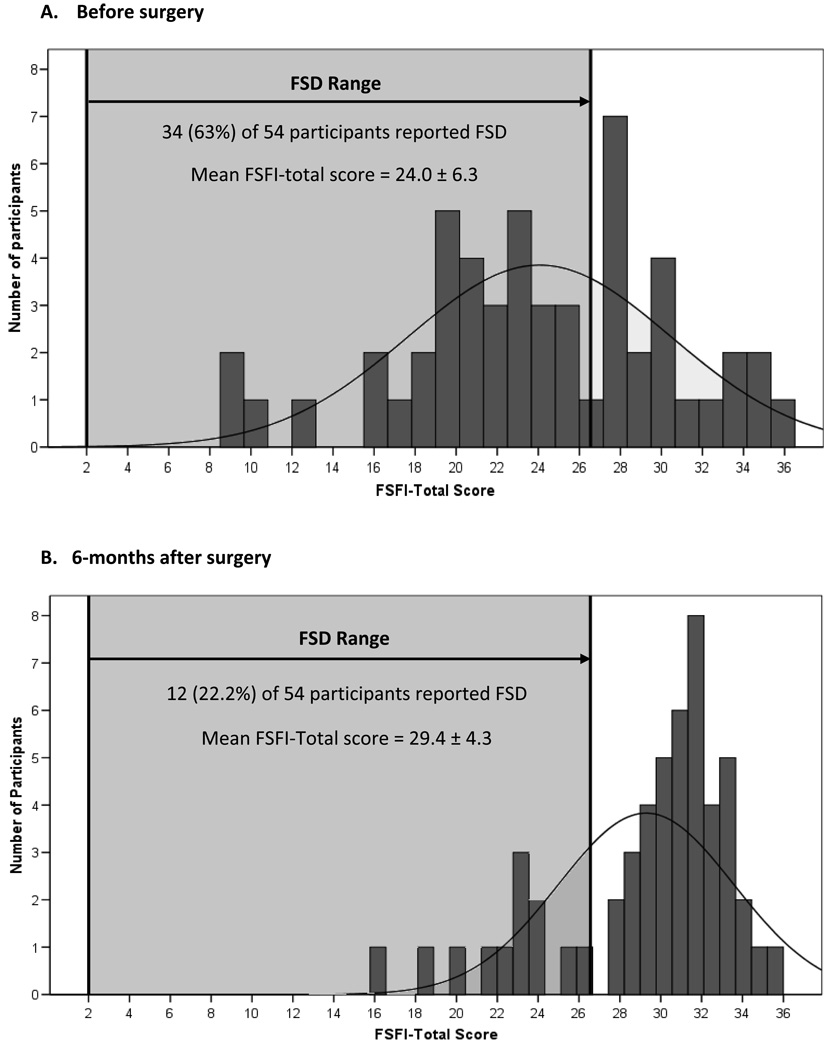
Figure 1 shows the distributions of FSFI-total scores for the sample before surgery and at 6-months after surgery. Before surgery, the average FSFI-total score was 24.0 ± 6.3 out of a maximum score of 36. Using the validated cut-off score of 26.55, 34 of 54 (63.0%) participants were classified as having FSD. At 6-months after surgery, the average FSFI-total score increased to 29.4 ± 4.3 and the rate of FSD in the entire sample decreased to 22.2%. FSD resolved in 23 of 34 (68%) patients postoperatively. One participant who did not have FSD before surgery developed FSD after surgery.
Figure 1.
Distribution of Female Sexual Function Index (FSFI-total) scores before surgery (A) and at 6-months after surgery (B)
Table 2 shows pre- to post-operative changes in FSFI-total scores by type of surgical procedure. While LAGB and RYGB participants differed significantly in the amount of weight loss they attained, they were similar in preoperative sexual function and degree of postoperative sexual function improvement.
Table 2.
Preoperative body mass index (BMI), percentage excess weight loss, and Female Sexual Function Index (FSFI-total) scores by type of surgical procedure
| Type of Surgical Procedure | P value | ||
|---|---|---|---|
| LAGB (n=38) |
RYGB (n=16) |
||
| Preoperative BMI | 44.6 ± 6.4 | 46.1 ± 7.7 | 0.47 |
| % Excess weight loss (M ± SD) | 34.6 ± 15.7 | 60.0 ± 21.2 | <0.001 |
| FSFI-total scores | |||
| Preoperative | 24.2 ± 5.9 | 23.7 ± 7.4 | 0.82 |
| Postoperative change | 4.9 ± 5.3 | 6.0 ± 4.9 | 0.41* |
Adjusted for age, marital status, and preoperative FSFI scores
Changes in FSFI-total scores were also assessed as a function of antidepressant medication use at pre- and post-surgery. Change scores were not significantly different among participants who were taking these medications at neither time point (n=29), at both time points (n=17), or only before surgery (n=7), with and without adjustment for covariates (i.e. age, marital status, preoperative FSFI scores and percentage of excess weight loss). Only one participant who was not on these medications before surgery began taking them after surgery.
We next examined multivariate correlates of pre- to post-operative changes in sexual function including demographics, preoperative variables, and percentage of excess weight loss and surgery type. The results of the final regression model are shown in Table 3. Younger age, being married, and lower preoperative FSFI-total scores were independently related to greater postoperative improvements in FSFI-total scores.
Table 3.
Predictors of pre- to post-operative changes in female sexual function.
| Variable | Standardized β | t | p value |
|---|---|---|---|
| Age | −0.275 | −2.624 | 0.012 |
| Marital status (married) | 0.231 | 2.165 | 0.036 |
| Preoperative BMI | 0.050 | 0.526 | 0.601 |
| Preoperative FSFI-total scores | −0.780 | −7.862 | <0.001 |
| Surgery type (RYGB) | −0.151 | −1.391 | 0.171 |
| % Excess Weight loss | −0.177 | −1.568 | 0.124 |
Model: R2 = 0.64, F (6, 51) = 13.5, p < 0.001
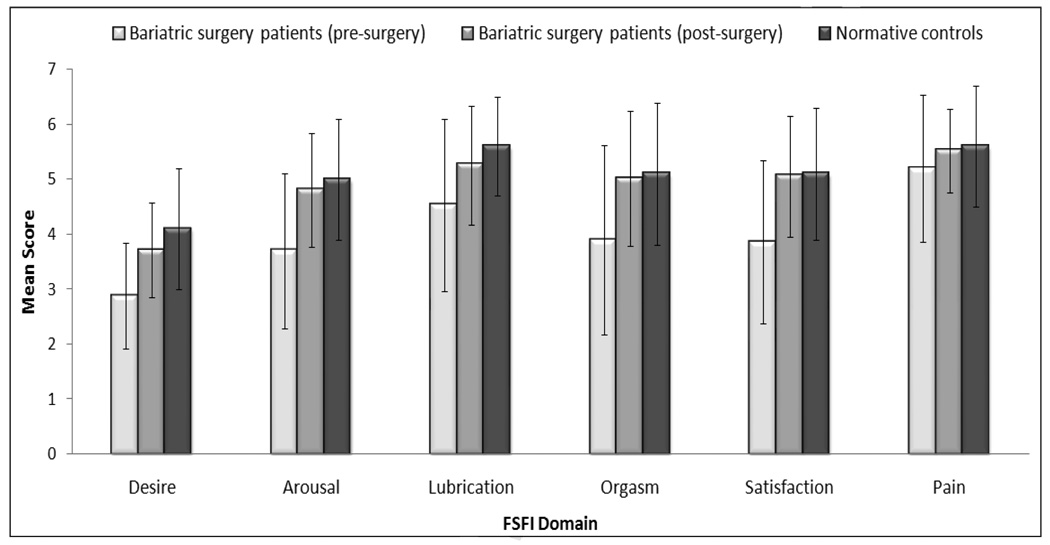
Finally, to provide context to the findings, participants’ pre- and post-operative FSFI scores were compared to published normative controls [17]. Preoperatively, participants’ FSFI-total scores were significantly lower compared to controls (24.0 ± 6.3 vs. 30.5 ± 5.3, p < 0.0001). Postoperatively, participants’ FSFI-total scores (29.4 ± 4.3) were indistinguishable from the control group (p = 0.18). Figure 2 shows a similar pattern of findings across each of the individual FSFI domains. Before surgery, participants scored significantly (p < 0.05) lower than the controls on all of the individual FSFI domains. However, after surgery, participants scored similarly (p > 0.20) to controls on all of the domains, except for desire (p = 0.02) and lubrication (p = 0.01), where participants had slightly worse scores.
Figure 2.
Comparison of bariatric surgery patients’ pre- and post-surgery FSFI domain scores with normative controls
Note. Bariatric surgery patients (pre-surgery) and controls are significantly (p < 0.05) different on all domains. Bariatric surgery patients (post-surgery) and controls are similar (p > 0.20) on all domains, except for desire and lubrication (p < 0.05). Means and standard deviations for controls are derived from Rosen et al. [17].
Discussion
Female sexual dysfunction (FSD) is a prevalent and complex condition that can result in considerable personal distress and adversely affect women’s health and quality of life [2]. Previously, we reported that the majority (60%) of women seeking bariatric surgery had FSD as defined by the Female Sexual Function Index (FSFI) [16]. In the present study, we examined whether FSD resolves postoperatively and if sexual functioning improves to levels consistent with published normative controls.
Results showed a dramatic reversal of FSD after bariatric surgery. By 6 months after surgery, FSD had resolved in 68% of patients who reported FSD at baseline. Across the whole sample, there were significant postoperative improvements on all of the sexual function domains. Greater sexual function improvements were associated with younger age, being married and worse preoperative sexual function.
The impact of bariatric surgery on sexual function, particularly in women, is an understudied area. While prior research has shown improvements in female sexual function after bariatric surgery [18–21], interpretation and comparison of findings is difficult given inconsistency in selection and definition of outcomes and use of non-standardized or quality-of-life measures to assess these outcomes. The current study advances this line of research by demonstrating for the first time significant resolution of FSD and improvements in established domains of female sexual function after bariatric surgery using a validated measure. Further research using the FSFI and other standardized measures is needed to replicate our findings in larger samples and determine whether female sexual function improvements are maintained across longer postoperative intervals.
Interestingly, our findings suggest that sexual function improvements in women undergoing bariatric surgery may not be dependent on amount of weight loss. Consequently, further research is needed to assess to what extent postoperative changes in related variables including body image and health-related quality of life [18, 20, 21, 24, 25], reproductive hormones [26], and endocrine and metabolic parameters [6, 10, 27] may account for these improvements, and whether there is a minimum weight loss requirement for improvement in sexual functioning. Additionally, depression and drugs used in its treatment are frequently associated with FSD [23, 28]. Although it appears from our study that antidepressants may not affect postoperative changes in women’s sexual function, further investigation of the effects of improvements in depression symptoms and discontinued use of antidepressants after surgery in larger samples is needed.
Finally, to provide some context to our findings, we compared participants’ pre- and post-operative sexual function with published normative controls [17]. Preoperatively, our sample of patients reported significantly worse overall sexual function than the normative control group. Postoperatively, however, these groups were indistinguishable from each other, suggesting a “normalization” of female sexual function after bariatric surgery.
The major strengths of this study include its prospective design and use of the validated FSFI measure to assess postoperative changes in key dimensions of women’s sexual function. One of the limitations of this study is that the majority of women were Caucasian. Women of different racial groups may display different patterns of FSD [2]. Although women who were lost to follow-up were similar to study completers in baseline characteristics, these non-completers may have experienced different changes in sexual function over time.
While improvements in sexual function were similar after RYGB and LAGB, the smaller number of RYGB patients may have limited statistical power to detect differences between these surgery groups. As noted above, a more comprehensive study of predictors of sexual function enhancement in this population is needed, as is information about whether participants perceived FSD to be a significant source of distress [29]. Finally, it is remarkable that despite remaining obese, participants reported a level of postoperative sexual functioning that was similar on average to that of normative reference controls. It is possible that participant responses were influenced by social desirability or the rapid weight loss and marked improvements in other aspects of health-related quality of life that occur during the early postoperative period. Consequently, it will be important for future studies to examine whether these improvements persist after weight has stabilized and/or regain has occurred.
In summary, this study showed marked resolution of women’s reported sexual dysfunction within 6 months of having bariatric surgery. Sexual function across the entire sample improved to levels that mirrored normative controls. Findings suggest that women undergoing bariatric surgery can experience this benefit regardless of type of operation or amount of weight loss. Future research directions may include examination of whether physiological, medical, and psychosocial factors play a mediating role, and if these improvements are sustained over time.
Acknowledgements
Dr. Bond is supported by a grant from the National Institutes of Diabetes and Digestive and Kidney Diseases (DK083438). Appreciation is expressed to Jennifer Trautvetter, B.A. for her assistance with data collection.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Basson R, Berman J, Burnett A, et al. Report of the international consensus development conference on female sexual dysfunction: definitions and classifications. J Urol. 2000;163:888–893. [PubMed] [Google Scholar]
- 2.Salonia A, Munarriz RM, Nasprop R, et al. Women’s sexual dysfunction: a pathophysiological review. BJU Int. 2004;93:1156–1164. doi: 10.1111/j.1464-410X.2004.04796.x. [DOI] [PubMed] [Google Scholar]
- 3.Clayton AH. Epidemiology and neurobiology of female sexual dysfunction. J Sex Med. 2007;4 Suppl 4:260–268. doi: 10.1111/j.1743-6109.2007.00609.x. [DOI] [PubMed] [Google Scholar]
- 4.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281:537–544. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 5.Laumann EO, Nicolosi A, Glasser DB, et al. Sexual problems among women and men aged 40–80 y: prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. Int J Impot Res. 2005;17:39–57. doi: 10.1038/sj.ijir.3901250. [DOI] [PubMed] [Google Scholar]
- 6.Palacios S, Castano R, Grazziotin A. Epidemiology of female sexual dysfunction. Maturitas. 2009;63:119–123. doi: 10.1016/j.maturitas.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 7.Esposito K, Ciotola M, Giugliano F, et al. Association of body weight with sexual function in women. Int J Impot Res. 2007;19:353–357. doi: 10.1038/sj.ijir.3901548. [DOI] [PubMed] [Google Scholar]
- 8.Melin I, Falconer C, Rossner S, Altman D. Sexual function in obese women: impact of lower urinary tract dysfunction. Int J Obes (Lond) 2008;32:1312–1318. doi: 10.1038/ijo.2008.67. [DOI] [PubMed] [Google Scholar]
- 9.Abu Ali RM, Al Hajeri RM, Khader YS, Ajlouini KM. Factors associated with sexual dysfunction in Jordanian women and their sexual attitudes. Ann Saudi Med. 2009;29:270–274. doi: 10.4103/0256-4947.55312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pace G, Silvestri V, Guala L, Vicentini C. Body mass index, urinary incontinence, and female sexual dysfunction: how they affect female postmenopausal health. Menopause. 2009;16:1188–1192. doi: 10.1097/gme.0b013e3181a6b491. [DOI] [PubMed] [Google Scholar]
- 11.Veronelli A, Mauri C, Zecchini B, et al. Sexual dysfunction is frequent in premenopausal women with diabetes, obesity, and hypothyroidism, and correlates with markers of increased cardiovascular risk. A preliminary report. J Sex Med. 2009;6:1561–1568. doi: 10.1111/j.1743-6109.2009.01242.x. [DOI] [PubMed] [Google Scholar]
- 12.Kolotkin RL, Crosby RD, Williams GR. Health-related quality of life varies among obese subgroups. Obes Res. 2002;10:748–756. doi: 10.1038/oby.2002.102. [DOI] [PubMed] [Google Scholar]
- 13.Kolotkin RL, Pendelton R, Strong M, Gress RE, Adams T. Health-related quality of life in patients seeking gastric bypass surgery vs non-treatment-seeking controls. Obes Surg. 2003;13:371–377. doi: 10.1381/096089203765887688. [DOI] [PubMed] [Google Scholar]
- 14.Kolotkin RL, Binks M, Crosby RD, Ostbye T, Gress RE, Adams T. Obesity and sexual quality of life. Obesity (Silver Spring) 2006;14:472–479. doi: 10.1038/oby.2006.62. [DOI] [PubMed] [Google Scholar]
- 15.Assimakopoulos K, Panayiotopolous S, Iconomou G, et al. Assessing sexual function in obese women preparing for bariatric surgery. Obes Surg. 2006;16:1087–1091. doi: 10.1381/096089206778026442. [DOI] [PubMed] [Google Scholar]
- 16.Bond DS, Vithiananthan S, Leahey TM, et al. Prevalence and degree of sexual dysfunction in a sample of women seeking bariatric surgery. Surg Obes Relat Dis. 2009;5:698–704. doi: 10.1016/j.soard.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosen R, Brown C, Heiman J, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 18.Camps MA, Zervos E, Goode S, Rosemurgy AS. Impact of bariatric surgery on body image perception and sexuality in morbidly obese patients and their partners. Obes Surg. 1996;6:356–360. doi: 10.1381/096089296765556700. [DOI] [PubMed] [Google Scholar]
- 19.Kinzl JF, Trefalt E, Fiala M, Hotter A, Biebl W, Aigner F. Partnership, sexuality, and sexual disorders in morbidly obese women: consequences of weight loss after gastric banding. Obes Surg. 2001;11:455–458. doi: 10.1381/096089201321209323. [DOI] [PubMed] [Google Scholar]
- 20.Dziurowicz-Kozlowska A, Lisik W, Wierzbicki Z, Kosieradzki M. Health-related quality of life after the surgical treatment of obesity. J Physiol Pharmacol. 2005;56 Suppl 6:127–134. [PubMed] [Google Scholar]
- 21.Kolotkin RL, Crosby RD, Gress RE, Hunt SC, Adams TD. Two-year changes in health-related quality of life in gastric bypass patients compared with severely obese controls. Surg Obes Relat Dis. 2009;5:250–256. doi: 10.1016/j.soard.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): cross-validation and development of clinical cut-off scores. J Sex Marital Ther. 2005;31:1–20. doi: 10.1080/00926230590475206. [DOI] [PubMed] [Google Scholar]
- 23.Serretti A, Chiesa A. Treatment-emergent sexual dysfunction related to antidepressants: a meta-analysis. J Clin Psychopharmacol. 2009;29:259–266. doi: 10.1097/JCP.0b013e3181a5233f. [DOI] [PubMed] [Google Scholar]
- 24.Hrabosky JI, Masheb RM, White MA, Rothschild BS, Burke-Martindale CH, Grilo CM. A prospective study of body dissatisfaction and concerns in extremely obese gastric bypass patients: 6- and 12-month outcomes. Obes Surg. 2006;16:1615–1621. doi: 10.1381/096089206779319527. [DOI] [PubMed] [Google Scholar]
- 25.Sarwer DB, Fabricatore AN. Psychiatric considerations of the massive weight loss patient. Clin Plast Surg. 2008;35:1–10. doi: 10.1016/j.cps.2007.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Merhi ZO. Impact of bariatric surgery on female reproduction. Fertil Steril. 2009;92:1501–1508. doi: 10.1016/j.fertnstert.2009.06.046. [DOI] [PubMed] [Google Scholar]
- 27.Rubino F, Schauer PR, Kaplan LM, Cummings DE. Metabolic surgery to treat type 2 diabetes: clinical outcomes and mechanisms of action. Annu Rev Med. 2010;61:393–411. doi: 10.1146/annurev.med.051308.105148. [DOI] [PubMed] [Google Scholar]
- 28.Kennedy SH, Rizvi S. Sexual dysfunction, depression, and the impact of antidepressants. J Clin Psychopharmacol. 2009;29:157–164. doi: 10.1097/JCP.0b013e31819c76e9. [DOI] [PubMed] [Google Scholar]
- 29.Hayes RD, Dennerstein L, Bennett CM, Fairley CK. What is the “true” prevalence of female sexual dysfunctions and does the way we assess these conditions have an impact? J Sex Med. 2008;5:777–787. doi: 10.1111/j.1743-6109.2007.00768.x. [DOI] [PubMed] [Google Scholar]