Abstract
Mammary hamartomas are typically a benign condition and rarely develop into malignant lesions. Only 14 cases of carcinomas associated with a hamartoma have been documented in the literature. In this case report, we describe a case of invasive ductal carcinoma within a hamartoma in a 72-year-old woman. Mammography, ultrasonography, and magnetic resonance imaging showed the features of a typical hamartoma with a suspicious mass arising in it. This case illustrates the importance of identification of unusual findings in a typical mammary hamartoma on radiologic examinations.
Keywords: Mammary hamartoma, Invasive ductal carcinoma
Mammary hamartomas are localized overgrowths of fibrous, epithelial, and fatty elements which occur primarily in adults during the reproductive years (1). Mammary hamartomas are widely known to have no special propensity to undergo malignant transformation, and are not a marker for increased relative risk for breast cancer development (1); however, some investigators have suggested that malignant transformation of mammary hamartomas is possible, given the presence of glandular tissue in this type of lesion (2-4). In fact, 14 cases of carcinomas associated with mammary hamartomas have been previously documented in the literature (2-12). In this report, we review the literature and describe a new case of invasive ductal carcinoma (IDC) arising in a mammary hamartoma that was detected while the patient was being followed for a known hamartoma.
CASE REPORT
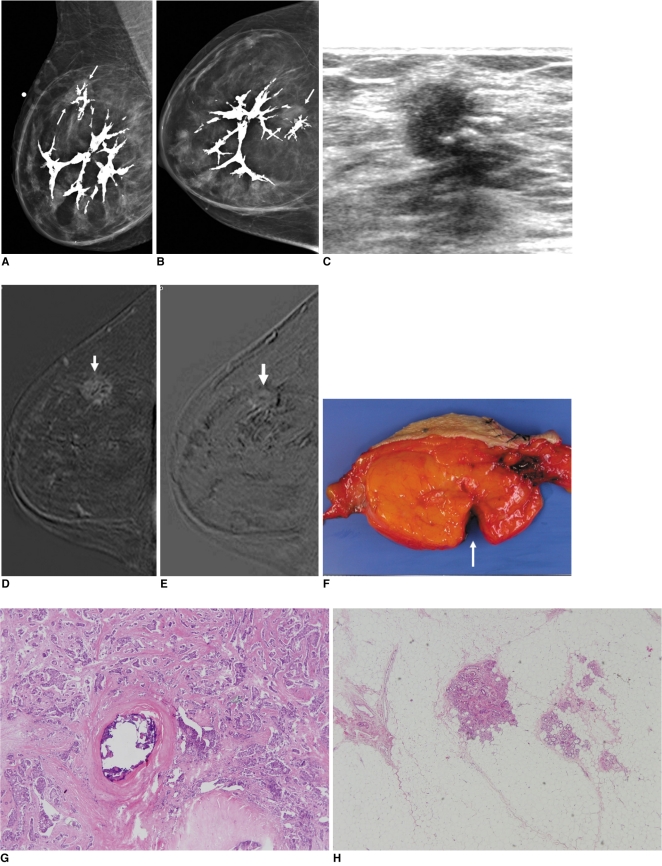
A 72-year-old woman presented for further examination of a right breast lump. According to the patient, the lump had been present for at least 10 years. She complained of discomfort of recent onset in the right breast. On physical examination, a soft, mobile, 10 cm mass, which occupied nearly the entire right breast, was palpated. On mammography, a large circumscribed mass surrounded by a water-density capsule was shown in the right breast (Fig. 1A, B). The mass was a mixture of isodense and fat densities and had dystrophic calcifications in a branching pattern. The mammograms were initially interpreted as a benign hamartomatous lesion (Fig. 1A, B). On ultrasonography (US), the mass was very heterogeneous and completely encompassed in a thin echogenic pseuduocapsule of compressed breast tissue, which was compatible with hamartoma. However, a careful US examination revealed an irregular hypoechoic mass of 1.4 cm with a non-parallel orientation within the hamartoma (Fig. 1C). A retrospective review of the mammograms revealed focal asymmetry, which correlated with the suspicious mass on US (Fig. 1A, B). The lesion was early enhanced and a washout on enhanced MRI scans (Fig. 1D, E), thus it was thought to be a malignancy. Surgical excision for entire mass was done and the diagnosis from the frozen specimen of the suspicious area was IDC.
Fig. 1.
Invasive ductal carcinoma and mammary hamartoma in 72-year-old woman.
A, B. Mediolateral oblique and craniocaudal views of right breast show fat-containing mass including dystrophic calcifications, suggesting hamartoma. There is focal asymmetry (arrows) at 12 o'clock within hamartoma.
C. US of right breast at 12 o'clock shows spiculated, nonparallel, hypoechoic mass, which corresponds with focal asymmetry on mammogram (A, B).
D, E. Standard subtraction image (D) and reverse subtraction image (E) of dynamic MRI show suspicious mass (arrows) within hamartoma, which was early enhanced (D) and washout (E).
F. Gross specimen shows 9-cm smooth circumscribed fatty mass. Suspicious mass was excised from fatty mass (arrow).
G, H. Photomicrograph of histopathologic specimen of excised suspicious mass reveals invasive ductal carcinoma and dystrophic calcifications (in H) located within carcinoma.
The patient therefore underwent a modified radical mastectomy. The microscopic examination showed an IDC arising in a hamartoma (Fig. 1F-H). There was no IDC which was outside the hamartoma. There was no intraductal component and there was no axillary lymph node metastasis. The remaining palpable mass was hamartoma with dystrophic calcifications. The patient subsequently underwent adjuvant chemotherapy. At 24 months post surgery, there was no evidence of local recurrence of the IDC or any distant metastasis.
DISCUSSION
Mammary hamartomas, a term applied to breast tumors in 1971 by Arrigoni et al. (13), have also been referred to as lipofibroadenomas, adenolipofibromas, and fibroadenolipomas (1). Hamartomas may present as tender or non-tender palpable lumps, but are often discovered incidentally during a screening mammography (1, 14). The typical mammographic feature of hamartomas is a circumscribed fibrofatty mass (15). On US, most mammary hamartomas have circumscribed margins, an oval shape, and heterogeneous internal echogenicity (16, 17).
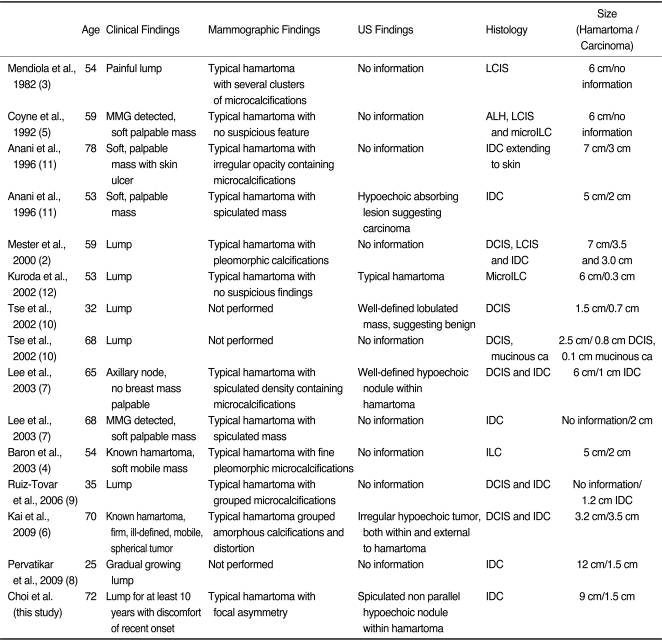
Malignancies associated with hamartomas are rare. The clinical, radiologic, and histologic findings of the previously described 14 cases of malignant hamartomas and the current case are summarized in Table 1. The mean patient age was 56.3 years (range, 25-78 years). The lesions are frequently recognized as palpable masses. The size of the hamartomas range from 1.5-12.0 cm in diameter and the size of the associated carcinomas range from 0.3-3.5 cm in diameter.
Table 1.
Summarized Clinicopathologic Features of Reported Hamartoma-Associated Malignancy
Note.-ALH = atypical lobular hyperplasia, DCIS = ductal carcinoma in situ, IDC = invasive ductal carcinoma, ILC = invasive lobular carcinoma, LCIS = lobular carcinoma in situ, MMG = mammography
Of the described 15 cases, mammography was obtained in 12 cases, of which 10 showed the typical appearance of hamartomas with suspicious features, such as clusters of microcalcifications, pleomorphic micocalcifications, and spiculated masses. The remaining two cases had the typical appearance of a hamartoma with no suspicious features, thus co-existing malignancies were unexpected findings at the time of tumorectomy. US findings were available in only six cases, of which four had suspicious masses with irregular margins, hypoechogenicity, or a non parallel orientation within the hamartomas; and two cases were diagnosed pre-operatively as carcinomas by US-guided fine needle aspiration or core needle biopsies and underwent one-step curative surgery (6, 7). As stated above, the majority of cases had suspicious findings within the hamartoma on mammography or US. Radiologists therefore need to pay careful attention in order to detect subtle suspicious findings, even though mammography or US may show typical hamartomas.
Among the 15 cases described here, 12 had carcinomas that were confined to the hamartomas and the remaining three cases had carcinomas that involved both the hamartomas and adjacent normal breast tissue. If carcinomas involve both the hamartoma and normal breast tissue, it is difficult to determine whether the carcinoma arises within the hamartoma or an isolated carcinoma which initiates growth nearby later extends into the hamartoma. However, in the majority of cases described here, including the current case, the carcinomas were located within the hamartomas, (2-5, 7, 8, 10-12) thus we believe that the malignancies arose within the hamartomas.
In conclusion, breast hamartomas have generally been classified as rare, benign tumors, and carcinomas occur only rarely. However, hamartomas may be diagnosed with greater frequency due to widespread screening mammography. Radiologists should recognize that malignancy may co-exist or develop in hamartomas and be alert to the presence of suspicious features within a hamartoma.
References
- 1.Stavros AT. Breast ultrasound. Philadelphia: LWW; 2004. pp. 560–569. [Google Scholar]
- 2.Mester J, Simmons RM, Vazquez MF, Rosenblatt R. In situ and infiltrating ductal carcinoma arising in a breast hamartoma. AJR Am J Roentgenol. 2000;175:64–66. doi: 10.2214/ajr.175.1.1750064. [DOI] [PubMed] [Google Scholar]
- 3.Mendiola H, Henrik-Nielsen R, Dyreborg U, Blichert-Toft M, Al-Hariri JA. Lobular carcinoma in situ occurring in adenolipoma of the breast. Report of a case. Acta Radiol Diagn (Stockh) 1982;23:503–505. doi: 10.1177/028418518202300511. [DOI] [PubMed] [Google Scholar]
- 4.Baron M, Ladonne JM, Gravier A, Picquenot JM, Berry M. Invasive lobular carcinoma in a breast hamartoma. Breast J. 2003;9:246–248. doi: 10.1046/j.1524-4741.2003.09313.x. [DOI] [PubMed] [Google Scholar]
- 5.Coyne J, Hobbs FM, Boggis C, Harland R. Lobular carcinoma in a mammary hamartoma. J Clin Pathol. 1992;45:936–937. doi: 10.1136/jcp.45.10.936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kai M, Tada K, Tamura M, Gomi N, Horii R, Akiyama F, et al. Breast cancer associated with mammary hamartoma. Breast Cancer. 2009 doi: 10.1007/s12282-009-0147-3. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Lee EH, Wylie EJ, Bourke AG, Bastiaan De Boer W. Invasive ductal carcinoma arising in a breast hamartoma: two case reports and a review of the literature. Clin Radiol. 2003;58:80–83. doi: 10.1053/crad.2003.1133. [DOI] [PubMed] [Google Scholar]
- 8.Pervatikar SK, Rao R, Dinesh US, Parameswaraiah S. Large mammary hamartoma with focal invasive ductal carcinoma. Indian J Pathol Microbiol. 2009;52:249–251. doi: 10.4103/0377-4929.48935. [DOI] [PubMed] [Google Scholar]
- 9.Ruiz-Tovar J, Reguero-Callejas ME, Aláez AB, Ramiro C, Rojo R, Collado MV, et al. Infiltrating ductal carcinoma and ductal carcinoma in situ associated with mammary hamartoma. Breast J. 2006;12:368–370. doi: 10.1111/j.1075-122X.2006.00279.x. [DOI] [PubMed] [Google Scholar]
- 10.Tse GM, Law BK, Pang LM, Cheung HS. Ductal carcinoma in situ arising in mammary hamartoma. J Clin Pathol. 2002;55:541–542. doi: 10.1136/jcp.55.7.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anani PA, Hessler C. Breast hamartoma with invasive ductal carcinoma. Report of two cases and review of the literature. Pathol Res Pract. 1996;192:1187–1194. doi: 10.1016/S0344-0338(96)80149-X. [DOI] [PubMed] [Google Scholar]
- 12.Kuroda N, Sugimoto T, Numoto S, Enzan H. Microinvasive lobular carcinoma associated with intraductal spread arising in a mammary hamartoma. J Clin Pathol. 2002;55:76–77. doi: 10.1136/jcp.55.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arrigoni MG, Dockerty MB, Judd ES. The identification and treatment of mammary hamartoma. Surg Gynecol Obstet. 1971;133:577–582. [PubMed] [Google Scholar]
- 14.Daya D, Trus T, D'Souza TJ, Minuk T, Yemen B. Hamartoma of the breast, an underrecognized breast lesion. A clinicopathologic and radiographic study of 25 cases. Am J Clin Pathol. 1995;103:685–689. doi: 10.1093/ajcp/103.6.685. [DOI] [PubMed] [Google Scholar]
- 15.Helvie MA, Adler DD, Rebner M, Oberman HA. Breast hamartomas: variable mammographic appearance. Radiology. 1989;170:417–421. doi: 10.1148/radiology.170.2.2911664. [DOI] [PubMed] [Google Scholar]
- 16.Chao TC, Chao HH, Chen MF. Sonographic features of breast hamartomas. J Ultrasound Med. 2007;26:447–452. doi: 10.7863/jum.2007.26.4.447. [DOI] [PubMed] [Google Scholar]
- 17.Park SY, Oh KK, Kim EK, Son EJ, Chung WH. Sonographic findings of breast hamartoma: emphasis on compressibility. Yonsei Med J. 2003;44:847–854. doi: 10.3349/ymj.2003.44.5.847. [DOI] [PubMed] [Google Scholar]