Abstract
Lung cancer rates in Xuanwei County have been among the highest in China for both males and females, and have been causally associated with exposure to indoor smoky (bituminous) coal emissions that contain very high levels of polycyclic aromatic hydrocarbons. There are numerous coal mines across the County. Although lung cancer risk is strongly associated with use of smoky coal as a whole, variation in risk by smoky coal subtype has not been characterized as yet. We conducted a population-based case-control study of 498 lung cancer cases and 498 controls, individually matched to case subjects on age (±2 years) and sex, to examine risk by coal subtype. Odds ratios (ORs) and 95% confidence intervals (CIs) for coal subtype were calculated by conditional logistic regression, adjusting for potential confounders. Overall, smoky coal use was statistically significantly associated with lung cancer risk, as compared to use of smokeless coal or wood (OR=7.7, 95% CI=4.5 to 13.3). Furthermore, there was marked heterogeneity in risk estimates for specific subtypes of smoky coal (test for heterogeneity: p=5.17 × 10−10). Estimates were highest for coal from the Laibin (OR=24.8, 95% CI=12.4 to 49.6) and Longtan (OR=11.6, 95% CI = 5.0 to 27.2) coal types, and lower for coal from other types. These findings strongly suggest that in Xuanwei and elsewhere, the carcinogenic potential of coal combustion products can exhibit substantial local variation by specific coal source.
Keywords: Coal, lung cancer, indoor air pollution, Xuanwei, China
Introduction
Indoor air pollution from household burning of solid fuels, including coal, as practiced by about half of the world’s population in developing countries, is a major public health problem1;2. Exposure to solid fuel smoke is strongly associated with multiple diseases, including chronic obstructive pulmonary disease, acute respiratory infections, and cancer, particularly lung cancer.2–14 Indeed, indoor coal smoke has been causally associated with lung cancer.6;14 Indoor air pollution from solid fuel use has been estimated to be the eighth strongest risk factor for global disease.3 Coal is used extensively in China for heating and cooking 14;15 and is widely and increasingly utilized to generate electricity in many countries, including the United States.16;17
Xuanwei County is located in southwestern Chinese province of Yunnan. It is 102 km from east to west, and 91 km from north to south; its total area is 6,257 km2. Its population was about one million people in the 1980s. Lung cancer rates in Xuanwei have been among the highest in China (27.7 and 25.3 per 100,000 in men and women, respectively, in the 1970s).18 Rates are similar for men and women, even though almost all women are non-smokers.7;18 Xuanwei residents have traditionally used one or more of three different types of fuels for household cooking and heating: “smoky coal” (bituminous), “smokeless coal” (anthracite), and wood. Traditionally, fuel was burned in an unvented fire pit in the floor of the family living area. Such burning generates very high indoor concentrations of airborne particulate matter (sometimes exceeding 20 mg/m3), benzo[a]pyrene (BaP) (which can approach levels experienced by coke oven workers), and other organic compounds.18 Epidemiologic studies in Xuanwei provided early evidence linking smoky coal use and lung cancer in humans.7;9;18–20 Toxicologic studies have shown that combustion products from Xuanwei smoky coal are more tumorigenic and mutagenic than those from smokeless coal and wood products.18;21 Variation in lung cancer risk by coal subtype has not yet been characterized. Documentation of substantial variation in risk with subtype would suggest that exposure to carcinogenic agents, e.g., polycyclic aromatic hydrocarbons (PAHs), could also vary widely in a relatively small area, and such variation could be important from a public health perspective. We conducted a case-control study to evaluate the risk of lung cancer associated with different fuel types and with smoky coal subtypes mined in different Xuanwei districts.
Materials and methods
A population-based case-control study was conducted between 1985 and 1990 in Xuanwei. Study subjects were restricted to farmers, as more than 90% of the total population in Xuanwei are farmers.18 Our case series included all cases of lung cancer newly diagnosed from November 1985 through February 1990 in four hospitals in Xuanwei (Xuanwei County Hospital, Yun Dan Hospital, Laibin Coal Mine Hospital, and Xuanwei Traditional Medicine Hospital), which diagnosed the virtually all lung cancer in Xuanwei. Eligible participants were male and female farmers 18–85 years of age, who resided in Xuanwei County for more than one year prior to diagnosis. A total of 500 eligible lung cancer cases were enrolled. After exclusion of 2 cases with incorrect addresses, 498 cases were included in the analysis. Among these, 195 (39%) were diagnosed based on sputum cytology, or pathological findings from needle biopsy, bronchofiberoscopy, or surgery. The remainder cases were diagnosed based on chest X-ray and clinical history. Among the 51 cases with histological classification, 39% were squamous cell carcinomas, 43% were adenocarcinomas, 10% were undifferentiated carcinomas, and 8% were small cell carcinomas.
Control subjects consisted of a sample of the general population of Xuanwei. In Xuanwei, there are a total of 20 communes. Each commune is divided into 15 to 20 large farming groups, and each large farming group is further divided into 15 to 20 small farming groups. A list of all residents was available at the small farming group level, in the local government center. Therefore, we designed a three-stage, randomized recruitment strategy for control selection. First, a commune was randomly selected, and then a large farming group within the commune was randomly selected, and then a small farming group within the large farming group was randomly selected. Subsequently, a control subject was matched to each case subject by randomly selecting an individual from the subgroup of people in the small farming group that was comparable to the case based on age (±2 years) and sex. The selection of the controls occurred within 4 weeks after the diagnosis and recruitment of corresponding lung cancer cases. Because the variation in population size was considerably larger among communes than among large and small farming groups, we assigned a weighting factor for each commune based on its population size. This served to ensure that potential control subjects had similar probabilities of being selected.
Interviews were conducted in the subject’s home (19% for cases and 96% for controls), or in the hospital (81% for cases and 4% for controls). The questionnaire elicited information on lifetime history of fuel use, residential history, cooking history, time spent indoors and outdoors, smoking history, environmental tobacco smoke exposure history, medical history, family history of cancer, dietary factors, and socioeconomic status. The participation rates were 100% for cases and 97% for controls. This study was approved by the Chinese Academy of Preventive Medicine, and was conducted according to the recommendations of the World Medical Association Declaration of Helsinki for human study subject protection. Oral informed consent was obtained from all study subjects.
Coal type exposure assessment
In the 1980s when this study was carried out, more than 90% of Xuanwei residents were farmers, and the population was very stable.7 Typically, male residents live in the same village (often the same house) over their lifetime, whereas female residents generally move into their husbands’ homes after marriage. Even so, women usually did not leave their commune of birth. Coal users usually purchased coal from the mine nearest to their home. Subjects were queried about which coal mine they purchased coal from, and the total tonnage of coal that they purchased annually. They were also asked about any changes in the type of coal that was used and the rate of coal consumption over time, i.e., tons of coal used per year. Cumulative coal use was determined by multiplying the annual tonnage of coal use by the number of years of coal use. Annual tonnage of coal consumption was generally fixed for a given house holdover the lifetime of study subjects. Based on a local geologic analysis of coal type locations in Xuanwei County,22 we classified the coal sources into 12 different types. Among them, 10 were smoky coal and two were smokeless coal subtypes, which are named for the district in Xuanwei where most of the coal from a given type was mined. In addition, subjects (cases or controls) who resided in the same commune likely used the same fuel type, although the amount of fuel used might have been different.
Indoor Air Sampling
In 1986, household indoor concentrations of the carcinogen benzo[a]pyrene (BaP) were measured in 27 representative houses in 11 Xuanwei communes (11 types of coal).19 Sampling details have been reported previously. Briefly, households were selected based on fuel type used, number of years lived in Xuanwei (at least 15 years), house type (traditional structure), and stove type (unvented fire pit). In each household, filter samples were collected over 3 consecutive days during four different time periods. BaP concentrations were determined using fluorescence spectrophotometry. The time-weighted BaP concentration was calculated for each of the 11 coal types.19 Seven of these 11 area-specific average indoor BaP concentrations could be paired with coal-type specific odds ratios (ORs) in the present study.
Statistical Methods
Conditional logistic regression was employed to estimate ORs and 95% confidence intervals (95% CIs) (SAS software, version 9.0.3; SAS Institute, Cary, NC, USA). All statistical tests were two-sided. Based on previous studies, we expected lung cancer risk to be low in users of smokeless coal and wood.7;18;19 Therefore, we combined smokeless coal and wood users as the reference group.
Potential confounders were included in multivariable models if their inclusion caused β parameter estimates to change by more than 10%, or if previous studies showed an effect on lung cancer risk. Final multivariable logistic models for coal subtype and lung cancer included literacy, lung cancer in first-degree relatives, cumulative lifetime hours spent at home, coal mine work history, tobacco use (coded as never users; sole users of other types of tobacco or cigarettes smoked with a water pipe, ≤20 pack-years of cigarettes smoked without a water pipe; >20 pack-years of cigarettes smoked without a water pipe, and passive smoke exposure history (yes/no). Adjustment for other covariates including ethnicity, cumulative tons of coal used, and cooking history, did not affect modeled risks appreciably, so these were not included in the final models.
Separate analyses of the association between lung cancer risk and the coal subtype used when the subject was born, and the subtype used for the longest time, were conducted. Since women in this population tend to spend a greater amount of time at home, cooking and doing house work than men, risks were estimated not only for both sexes combined, but also for each sex separately. Heterogeneity among ORs for different coal subtypes was determined using a Wald chi-square statistic for homogeneity.23 In addition, interactions were assessed by including cross-product terms as well as main effect terms in a logistic regression model. The statistical significance of interactions between sex and tobacco use, and each coal subtype, were evaluated by comparing models with and without the cross-product terms using the likelihood ratio test. These interactions were not significant, and were therefore not included in final models.
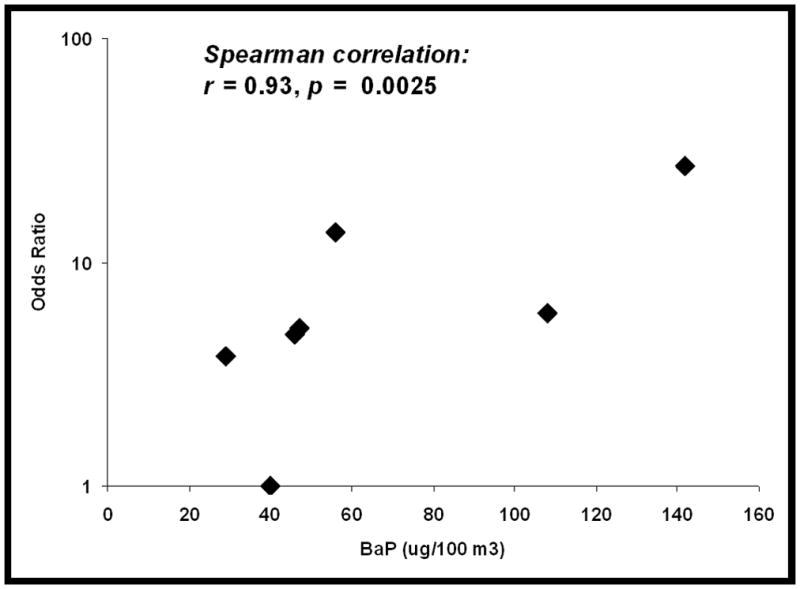
For the seven coal subtypes mentioned above, the non-parametric Spearman correlation test was used to evaluate the relationship between indoor BaP concentration for different types of coal with the OR of lung cancer for the same type of coal used in the home where subjects were born.
Results
Table 1 summarizes subject characteristics. About 98% of the cases and 95% of the controls were Han Chinese. More cases (34%) than controls (27%) were illiterate. Compared with controls, cases were more likely to have been coal miners, and to have a family history of lung cancer and a personal history of non-malignant lung disease. Cases spent more time at home than controls did. About 88% of the males were tobacco smokers, whereas only one female smoked. Therefore, the effect of tobacco smoking was evaluated only in males. Among men, cigarette smoking was associated with increased risk of lung cancer risk. In multiple logistic regression models, ORs and 95% CIs for ≤20 pack-years and >20 pack-years of cigarette smoking vs. never smokers were 1.7 (0.6 to 4.5) and 3.8 (1.2 to 12.4), respectively. Other modes of smoking tobacco (primarily with a water pipe) were weakly and nonsignificantly associated with lung cancer risk (OR = 1.5, 95% CI: 0.6 to 3.9).
Table 1.
Characteristics of lung caner patients and population controls in Xuanwei, China.
| All | Male | Female | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Cases N (%) | Controls N (%) | P | Cases N (%) | Controls N (%) | P | Cases N (%) | Controls N (%) | P | |
| Categorical variables | |||||||||
| Ethnicity | |||||||||
| Han | 490 (98) | 474 (95) | 257 (99) | 245 (94) | 233 (98) | 229 (96) | |||
| Others | 8 (2) | 24 (5) | 0.0040 | 3 (1) | 15 (6) | 0.0040 | 5 (2) | 9 (4) | 0.28 |
| Literacy | |||||||||
| No | 330 (66) | 363 (73) | 123 (47) | 149 (57) | 207 (87) | 214 (90) | |||
| Yes | 167 (34) | 135 (27) | 0.026 | 136 (52) | 111 (43) | 0.025 | 31 (13) | 24 (10) | 0.32 |
| Coal mine work history | |||||||||
| No | 450 (90) | 474 (95) | 212 (82) | 236 (91) | 238 (100) | 238 (100) | |||
| Yes | 48 (10) | 24 (5) | 0.0033 | 48 (18) | 24 (9) | 0.0023 | 0 (0) | 0 (0) | |
| Number of family members | |||||||||
| <=5 | 300 (60) | 245 (49) | 164 (63) | 139 (53) | 136 (57) | 106 (45) | |||
| >5 | 189 (38) | 239 (48) | 0.0007 | 88 (34) | 108 (42) | 0.044 | 101 (42) | 131 (55) | 0.0058 |
| Lung cancer in first-degree relatives | |||||||||
| No | 460 (92) | 495 (99) | 238 (92) | 259 (100) | <0.0001* | 215 (90) | 234 (98) | ||
| Yes | 38 (8) | 3 (1) | <0.0001* | 22 (8) | 1 (0) | 23 (10) | 4 (2) | 0.0002* | |
| Non-malignant lung disease history | |||||||||
| No | 393 (79) | 461 (93) | 197 (76) | 249 (96) | 196 (82) | 212 (89) | |||
| Yes | 105 (21) | 37 (7) | <0.0001 | 63 (24) | 11 (4) | <0.0001 | 42 (18) | 26 (11) | 0.036 |
| Ever cook | |||||||||
| No | 167 (34) | 170 (34) | 164 (63) | 170 (65) | 3 (1) | 0 (0) | |||
| Yes | 330 (66) | 326 (65) | 0.82 | 95 (37) | 88 (34) | 0.54 | 235 (99) | 238 (100) | 0.25* |
| Location of starting fire | |||||||||
| Indoors | 474 (96) | 465 (94) | 246 (96) | 245 (95) | 228 (96) | 220 (93) | |||
| Outdoors | 20 (4) | 29 (6) | 0.19 | 11 (4) | 13 (5) | 0.68 | 9 (4) | 16 (7) | 0.15 |
| Respondent status | |||||||||
| Personal | 415 (83) | 496 (100) | 224 (86) | 259 (100) | <0.0001* | 191 (80) | 237 (100) | ||
| Next-of-kin | 83 (17) | 2 (0) | <0.0001* | 36 (14) | 1 (0) | 47 (20) | 1 (0) | <0.0001* | |
| Passive smoke exposure& | |||||||||
| No | 29 (5) | 45 (9) | 22 (8) | 34 (13) | 7 (3) | 11 (5) | |||
| Yes | 469 (94) | 453 (91) | 0.053 | 238 (92) | 226 (87) | 0.090 | 231 (97) | 227 (95) | 0.34 |
| Ever smoke cigarettes (Males) | |||||||||
| None | 26 (16) | 34 (24) | |||||||
| Yes | 132 (84) | 110 (76) | 0.12 | ||||||
| Tobacco use (Males) | |||||||||
| Never smoker | 26 (10) | 34 (13) | |||||||
| Other tobacco | 112 (43) | 123 (47) | |||||||
| ≤ 20 pack-year cigarettes | 64 (25) | 81 (31) | |||||||
| >20 pack-year cigarettes | 55 (21) | 21 (8) | <0.0001 | ||||||
| Continuous variables | |||||||||
| Age | |||||||||
| 53±11 | 53±11 | 0.46 | 53±12 | 53±13 | 0.62 | 53±10 | 53±10 | 0.56 | |
| Coal used during lifetime (Tons) | |||||||||
| 190±119 | 179±117 | 0.16 | 183±133 | 172±115 | 0.32 | 197±102 | 188±118 | 0.32 | |
| Years cooking food (Mean ± SD) | |||||||||
| 32±17 | 33±16 | 0.29 | 16±16 | 18±17 | 0.58 | 39±11 | 39±11 | 0.69 | |
| Hours spent at home lifetime (*1000) | |||||||||
| 321±76 | 302±711 | <0.0001 | 312±79 | 292±74 | 0.0038 | 331±71 | 312±67 | 0.0026 | |
Fisher’s exact test.
Lung disease history includes chronic bronchitis, emphysema, asthma, or tuberculosis.
Smoking by any family member who lived with the subject.
The analysis of the domestic coal subtypes used when the subjects were born is presented in Table 2. Compared to smokeless coal or wood, smoky coal use was associated with a 7.7-fold (95% CI, 4.5 to 13.3) increased risk of lung cancer. Risks were similar among women (OR = 6.7; 95% CI, 3.2 to 14.2) and men (OR = 9.0; 95% CI, 4.1 to 19.8). There was marked variation in risk estimates for lung cancer by coal subtype (Table 2). Tests for heterogeneity among coal subtypes for all subjects, males, and females, were statistically significant (p = 5.17 × 10−10, 0.00017, and 0.00056, respectively). A much higher proportion of lung cancer cases (55% men and 56% women) than controls (14% men and 12% women) used Laibin coal, which was associated with the highest risk of lung cancer (Table 2). Risk estimates for different types of coal tended to be similar in women and men. The subtypes that were most strongly associated with lung cancer risk in women were also most strongly associated with risk in men (Spearman correlation of men’s with women’s modeled ORs: r = 0.89, p = 0.0005). Further analyses stratified by tobacco smoking (ever/never) showed that risk estimates were similar among smokers and nonsmokers (data not shown). These estimates were similar to those obtained after stratifying by sex, as shown in Table 2.
Table 2.
Adjusted odds ratios (ORs)* and 95% confidence intervals (CIs) for lung cancer in relation to coal subtype used when the subject was born.
| All | Male | Female | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coal type | Cases (%) | Controls (%) | OR* (95% CI) | Cases (%) | Controls (%) | OR# (95% CI) | Cases (%) | Controls (%) | OR& (95% CI) |
| Smokeless coal or wood | 23 (5) | 146 (30) | 1 | 14 (5) | 77 (30) | 1 | 9 (4) | 69 (29) | 1 |
| Smoky coal | 475 (95) | 351 (70) | 7.7 (4.5–13.3) | 246 (95) | 182 (70) | 9.0 (4.1–19.8) | 229 (96) | 169 (71) | 6.7 (3.2–14.2) |
| Smoky coal subtypes | |||||||||
| Laibin | 276 (55) | 64 (13) | 24.8 (12.4–49.6) | 143 (55) | 36 (14) | 25.2 (9.4–67.3) | 133 (56) | 28 (12) | 26.4 (9.6–72.6) |
| Longtan | 44 (9) | 24 (5) | 11.6 (5.0–27.2) | 24 (9) | 13 (5) | 14.8 (4.2–51.5) | 20 (8) | 11 (5) | 9.4 (2.8–31.1) |
| Baoshan | 12 (2) | 17 (3) | 6.0 (2.2–16.7) | 6 (2) | 12 (5) | 5.8 (1.4–23.9) | 6 (3) | 5 (2) | 6.6 (1.4–30.5) |
| Longchang | 42 (8) | 51 (10) | 4.1 (2.0–8.6) | 16 (6) | 16 (6) | 7.4 (2.2–24.5) | 26 (11) | 35 (15) | 2.9 (1.1–7.6) |
| Yangchang | 47 (9) | 56 (11) | 3.8 (1.8–8.3) | 28 (11) | 31 (12) | 4.9 (1.6–15.4) | 19 (8) | 25 (11) | 3.1 (1.0–9.4) |
| Wenxing | 14 (3) | 27 (5) | 3.8 (1.4–10.5) | 6 (2) | 12 (5) | 4.6 (1.0–22.0) | 8 (3) | 15 (6) | 3.4 (0.9–13.3) |
| Tangtang | 18 (4) | 30 (6) | 2.8 (1.2–6.6) | 6 (2) | 14 (5) | 3.6 (0.9–14.2) | 12 (5) | 16 (7) | 2.2 (0.6–7.5) |
| Shuanghe | 4 (1) | 21 (4) | 1.1 (0.2–4.7) | 2 (1) | 14 (5) | 1.2 (0.2–8.6) | 2 (1) | 7 (3) | 0.9 (0.1–10.9) |
| Tianba | 9 (2) | 41 (8) | 0.6 (0.2–1.9) | 8 (3) | 23 (9) | 1.0 (0.2–4.4) | 1 (0) | 18 (8) | 0.2 (0.02–2.1) |
| Yangliu | 3 (1) | 14 (3) | 0.7 (0.2–3.1) | 1 (0) | 6 (2) | 0.5 (0.1–5.2) | 2 (1) | 8 (3) | 0.9 (0.1–6.0) |
Adjusted for age, sex, literacy, lung cancer in first-degree relatives, hours spent at home per day, coal mine work history, tobacco use, and passive smoke exposure history.
Adjusted for the same variables as in *, with exception of sex.
Adjusted for the same variables as in *, with exception of sex, coal mine work history, and smoking.
Since some subjects’ fuel types changed over time, we examined temporal changes in fuel use by study subjects. About 81% of cases and 76% of controls used only one type of coal over their lifetimes. When we restricted the analysis to subjects in this subgroup, the results were essentially unchanged from those reported above (data not shown). Also, analysis of fuel type used for the longest time for the entire study population yielded results very similar to those for analysis of fuels used at birth (Table 3).
Table 3.
Adjusted odds ratios (ORs)* and 95% confidence interval (CIs) for lung cancer in relation to coal subtype used for the longest time.
| All | Male | Female | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coal type | Cases (%) | Controls (%) | OR* (95% CI) | Cases (%) | Controls (%) | OR# (95% CI) | Cases (%) | Controls (%) | OR& (95% CI) |
| Smokeless coal or wood | 19 (4) | 114 (23) | 1 | 12 (5) | 62 (24) | 1 | 7 (3) | 52 (22) | 1 |
| Smoky coal | 479 (96) | 384 (77) | 7.4 (4.1–13.1) | 248 (95) | 198 (76) | 8.4 (3.6–19.6) | 231 (97) | 186 (78) | 6.4 (2.9–14.5) |
| Smoky coal subtypes | |||||||||
| Laibin | 291 (58) | 79 (16) | 22.2 (10.8–46.0) | 148 (57) | 43 (17) | 21.3 (7.6–60.0) | 143 (60) | 36 (15) | 30.0 (9.8–92.0) |
| Longtan | 38 (8) | 34 (7) | 7.9 (3.3–19.0) | 22 (8) | 15 (6) | 14.4 (3.8–54.7) | 16 (7) | 19 (8) | 4.4 (1.3–15.3) |
| Baoshan | 13 (3) | 19 (4) | 6.0 (2.2–16.7) | 6 (2) | 13 (5) | 5.2 (1.2–21.9) | 7 (3) | 6 (3) | 10.8 (2.2–52.9) |
| Longchang | 37 (7) | 48 (10) | 4.4 (2.0–10.0) | 13 (5) | 15 (6) | 6.5 (1.8–23.3) | 24 (10) | 33 (14) | 3.4 (1.1–10.8) |
| Yangchang | 53 (11) | 55 (11) | 4.4 (2.0–9.6) | 31 (12) | 31 (12) | 5.6 (1.8–17.2) | 22 (9) | 24 (10) | 4.4 (1.4–14.3) |
| Wenxing | 11 (2) | 30 (6) | 2.3 (0.8–6.4) | 5 (2) | 12 (5) | 3.5 (0.7–16.7) | 6 (3) | 18 (8) | 1.8 (0.5–7.3) |
| Tangtang | 16 (3) | 27 (5) | 2.3 (0.9–5.9) | 6 (2) | 13 (5) | 3.2 (0.7–14.1) | 10 (4) | 14 (6) | 2.2 (0.5–8.7) |
| Shuanghe | 4 (1) | 22 (4) | 1.1 (0.3–4.4) | 2 (1) | 14 (5) | 1.3 (0.2–8.9) | 2 (1) | 8 (3) | 1.0 (0.1–7.4) |
| Tianba | 6 (1) | 42 (8) | 0.5 (0.1–1.8) | 6 (2) | 25 (10) | 0.8 (0.2–4.3) | 0 (0) | 17 (7) | -- |
| Yangliu | 2 (0) | 19 (4) | 0.4 (0.1–1.9) | 1 (0) | 10 (4) | 0.4 (0.0–3.7) | 1 (0) | 9 (4) | 0.3 (0.03–4.3) |
Adjusted for age, sex, literacy, lung cancer in first-degree relatives, hours spent at home per day, coal mine work history, tobacco use, and passive smoke exposure history.
Adjusted for the same variables as in *, with exception of sex.
Adjusted for the same variables as in *, with exception of sex, coal mine work history, and smoking.
We carried out a sensitivity analysis to explore the question of whether or not risk estimates for coal may have been biased due to potential under-detection of cases in districts that were relatively distant from the diagnosing hospitals, because people in Laibin lived relatively close to one or more of the study hospitals. We excluded 129 cases and 279 controls who lived more than one district away from these hospitals. Using unconditional logistic regression and adjusting for the original matching variables, we found that results for the reduced data set were similar to those for the full data set (e.g., ORs (95% CIs) for Laibin coal were 22.1 (6.6–74.4) and 22.2 (10.8–46.0), respectively, see Table 3).
In figure 1, indoor BaP concentration is plotted against modeled OR for lung cancer for seven smoky coal subtypes. The BaP concentration for each smoky coal type was correlated with the OR of lung cancer (Spearman r =0.93, p=0.0025) for the same type of coal used in the home where subjects were born. After deleting the value with the highest BaP concentration and OR, the Spearman correlation diminished to 0.88, but remained statistically significant (p = 0.019).
Figure 1.
Discussion
In this population-based case-control study of lung cancer in Xuanwei, China, we found that lung cancer risk was much higher among smoky coal users than smokeless coal and wood users. This was true especially for users of Laibin coal. There was substantial heterogeneity in risk estimates for the different subtypes of smoky coal that were used. To the best of our knowledge, this is the first time that lung cancer risk has been reported by specific coal subtypes in an epidemiologic study.
An increased risk of lung cancer has been observed for subjects exposed to combustion products from indoor coal burning in several previous case-control studies, with risks varying from 1.03 to 18.75.15;24–27 The reason for this variation in risk across studies has not been systematically addressed as yet, but it could plausibly be explained, at least in part, by exposure to different types or levels of carcinogens present in coals from different locations.
Incomplete coal combustion can produce respirable particles, as well as many volatile and nonvolatile organic compounds, such as BaP, benzene, and formaldehyde.28 The health threat posed by a given coal subtype depends largely on its composition.21 This in turn is a consequence of its plant precursors, the environment in which it was produced, and the chemical/physical processes that the precursor organic matter went through over time. The fact that we found a wide variation in lung cancer risk associated with the different coal subtypes strongly suggests that coal subtypes’ composition and combustion products may be different. Further, indoor BaP concentrations positively and significantly correlated with ORs of lung cancer for the different coal subtypes. This suggests that in Xuanwei at least, there is wide variation in exposure to BaP by coal type. Even though the measurements were limited, they suggested a plausible and coherent link between exposure to BaP, and quite possibly other carcinogens, and lung cancer. To fully evaluate risk in this population requires collection of detailed exposure data on coal type, usage, and personal habits in the home including cooking practices and other activities that could influence exposure intensity and duration. A new case-control study of lung cancer among non-smoking women in this population is currently in progress. This includes detailed exposure assessment, and will provide an opportunity to replicate and extend the findings reported here.
This study has several strengths. It is a population-based case-control study with very high participation rates, conducted in a rural, stable population with very little exposure to automotive or industrial air pollution. Most study subjects lived in only one or two residences over their lifetimes, and most households used only one type of fuel for cooking and heating. Thus, it is very unlikely that our results were affected appreciably by exposure misclassification. This contrasts with studies carried out in urban populations, which are far more mobile than the Xuanwei population, which often use multiple types of fuels, and which are exposed to complex, changing mixtures of ambient air pollution.
Our study also has several limitations. As this is a case-control study, recall bias is a potential concern. However, as mentioned above, this is unlikely to have occurred as most subjects only lived in 1–2 residences over their lifetime, and differential recall of coal source seems improbable. There were surrogate respondents for 17% of the cases and only 0.4% of the controls, and reporting bias could conceivably have affected the results. However, results from analyses of lung cancer risk by coal type, after excluding proxy interviews, were essentially identical to results reported for the entire study population. Further, the great majority of surrogates, 87%, were the subject’s spouse, parent, or child, who well knew where he or she purchased coal.
It is possible that lung cancer cases in districts that were distant from diagnosing hospitals were less likely to receive a lung cancer diagnosis. To explore the influence of this potential bias, we conducted a sensitivity analysis, restricting the data set to study subjects who lived relatively close to diagnosing hospitals, and found that risk estimates in the reduced data set were similar to risk estimates in the full data set.
In addition, among the 498 patients diagnosed with lung cancer, only 39% of the diagnoses had cytological or histological confirmation, and disease misclassification could have occurred. However, other diseases that might have been responsible for the clinical symptoms and abnormal chest x-rays of potential study subjects were carefully considered by diagnosing physicians. Also, the clinical course was very similar in diagnosed lung cancer patients with and without cytologic/histologic confirmation.20;25 Further, any misclassification is unlikely to be associated with type of coal, so it should – be nondifferential in nature. Restricting the analysis to cases diagnosed by cytology or histology yielded very similar results. Finally, most cases were interviewed in the hospital and almost all controls were interviewed at their homes, raising the possibility of recall bias. Again, however, this would have been unlikely, because Xuanwei residents consistently purchased coal from the mine closest to home.
We found a modest effect of smoking with lung cancer risk in this study. Our results are consistent with previous findings in this population, including relatively weak observed effects found among smokers in the highest risk coal subtypes (data not shown).9;10;20 We hypothesize that combined exposure to tobacco smoke and very high indoor air pollution levels tends to attenuate the observed effect of smoking. Analyses are underway to test this hypothesis formally. Most importantly, we note that the pattern of variation of risk by coal subtype was similar in men, almost all of whom smoke, and women, essentially none of whom smoke. In addition, the smoking frequencies among male controls for different coal types were very similar (ranging from 81–100% in the 10 smoky coal subgroups), even though lung cancer risks for these subtypes varied substantially. Finally, risk estimates for coal subtypes were essentially unchanged among men after adjustment for tobacco use. These observations indicate that the observed relationship between exposure to coal and lung cancer risk could not be due to smoking.
The sampling procedure for control selection could be a potential source of bias. Although population weighting factors were applied for communes, they were not applied for large or small farming groups. Thus, our strategy of randomly selecting farming groups implied that individuals living in larger farming groups would be underrepresented among controls. However, populations of large and small farming groups were quite similar throughout Xuanwei. The population of a large farming groups varied from about 2000 to 3000, and for small farming groups varied from several hundred to about 1000. Therefore, we seriously doubt whether our sampling strategy introduced appreciable bias into the results.
An International Agency for Research on Cancer (IARC) monograph working group has recently concluded that indoor emissions from household combustion of coal are carcinogenic to humans (Group 1) and are associated primarily with an increased risk of lung cancer.6 Our study of coal types on lung cancer risks provides further evidence on the link between coal use and lung cancer risk and suggests that the association varies dramatically between different types of coal.
The quality of coal that is used in households around the world varies dramatically across countries and regions due to differences in local coal deposits. Little attention has been paid to the types of coal that are used by households and commercial users in developing countries, with regard to health hazards to people who are in closest proximity to the coal. Our study suggests that household coal fuels should be evaluated for their carcinogenic potential and that steps should be taken to minimize exposure to hazardous coals.
We found some evidence that BaP levels in air were associated with increased risk of lung cancer. However, the analysis was based on a small number of data points. Further, coal combustion products are a complex mixture, and can contain other carcinogenic or co-carcinogenic compounds, so it is possible that more than one type of exposure has contributed to the striking lung cancer excess in this region. Additional studies are underway to identify and characterize the full range of potential carcinogens (e.g., polycyclic aromatic hydrocarbons, particulates, and heavy metals) present in coal combustion products, and to study their dose-response relationships with lung cancer in a new, larger study of lung cancer among nonsmoking women in this region of China. In addition, this study will be able to evaluate genetic modification of these relationships, which should provide new insights into the underlying mechanism of the association, as well as increase our understanding of lung cancer risk for distinct subgroups of the population.
In summary, our results show substantial variation in risk of lung cancer by different types of coals used in Xuanwei. These findings strongly suggest that the carcinogenic potential of smoky coal varies by coal type, and strongly caution against overgeneralizing results obtained in one location to other locations. Thus, these findings provide an important justification for additional research into, and comparison of, indoor air pollution health effects in multiple locations.
Acknowledgments
Supported by the Chinese Academy of Preventive Medicine, Beijing, China, by the Yunnan Province Antiepidemic Station, Kunming, China, by the U.S. Environmental Protection Agency, and by the Intramural Research Program of the National Institutes of Health. This study would not have been possible without the cooperation of the subjects, and of many Chinese administrative and public health officials, physicians, and survey workers. We are especially grateful to Chaofu Huang of the Xuanwei County Antiepidemic Station.
Reference List
- 1.Rehfuess E, Mehta S, Pruss-Ustun A. Assessing household solid fuel use: multiple implications for the Millennium Development Goals. Environ Health Perspect. 2006;114:373–378. doi: 10.1289/ehp.8603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith KR. Indoor air pollution in developing countries: recommendations for research. Indoor Air. 2002;12:198–207. doi: 10.1034/j.1600-0668.2002.01137.x. [DOI] [PubMed] [Google Scholar]
- 3.Ezzati M, Lopez AD, Rodgers A, Vander HS, Murray CJ. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–1360. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 4.Smith KR. Indoor air pollution and acute respiratory infections. Indian Pediatr. 2003;40:815–819. [PubMed] [Google Scholar]
- 5.Smith KR, Mehta S. The burden of disease from indoor air pollution in developing countries: comparison of estimates. Int J Hyg Environ Health. 2003;206:279–289. doi: 10.1078/1438-4639-00224. [DOI] [PubMed] [Google Scholar]
- 6.Straif K, Baan R, Grosse Y, Secretan B, El Ghissassi F, Cogliano V. Carcinogenicity of household solid fuel combustion and of high-temperature frying. Lancet Oncol. 2006;7:977–978. doi: 10.1016/s1470-2045(06)70969-x. [DOI] [PubMed] [Google Scholar]
- 7.Chapman RS, Mumford JL, Harris DB, He ZZ, Jiang WZ, Yang RD. The epidemiology of lung cancer in Xuan Wei, China: current progress, issues, and research strategies. Arch Environ Health. 1988;43:180–185. doi: 10.1080/00039896.1988.9935850. [DOI] [PubMed] [Google Scholar]
- 8.Chapman RS, He X, Blair AE, Lan Q. Improvement in household stoves and risk of chronic obstructive pulmonary disease in Xuanwei, China: retrospective cohort study. BMJ. 2005;331:1050. doi: 10.1136/bmj.38628.676088.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lan Q, Chapman RS, Schreinemachers DM, Tian L, He X. Household stove improvement and risk of lung cancer in Xuanwei, China. J Natl Cancer Inst. 2002;94:826–835. doi: 10.1093/jnci/94.11.826. [DOI] [PubMed] [Google Scholar]
- 10.Liu ZY, He XZ, Chapman RS. Smoking and other risk factors for lung cancer in Xuanwei, China. Int J Epidemiol. 1991;20:26–31. doi: 10.1093/ije/20.1.26. [DOI] [PubMed] [Google Scholar]
- 11.Lubin JH, Li JY, Xuan XZ, Cai SK, Luo QS, Yang LF, Wang JZ, Yang L, Blot WJ. Risk of lung cancer among cigarette and pipe smokers in southern China. Int J Cancer. 1992;51:390–395. doi: 10.1002/ijc.2910510310. [DOI] [PubMed] [Google Scholar]
- 12.Peto R, Darby S, Deo H, Silcocks P, Whitley E, Doll R. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ. 2000;321:323–329. doi: 10.1136/bmj.321.7257.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Samet JM. The epidemiology of lung cancer. Chest. 1993;103:20S–29S. doi: 10.1378/chest.103.1_supplement.20s. [DOI] [PubMed] [Google Scholar]
- 14.Zhang JJ, Smith KR. Household air pollution from coal and biomass fuels in china: measurements, health impacts, and interventions. Environ Health Perspect. 2007;115:848–855. doi: 10.1289/ehp.9479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao Y, Wang S, Aunan K, Seip HM, Hao J. Air pollution and lung cancer risks in China--a meta-analysis. Sci Total Environ. 2006;366:500–513. doi: 10.1016/j.scitotenv.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 16.Cheng H, Zhang Y, Meng A, Li Q. Municipal solid waste fueled power generation in China: a case study of waste-to-energy in Changchun City. Environ Sci Technol. 2007;41:7509–7515. doi: 10.1021/es071416g. [DOI] [PubMed] [Google Scholar]
- 17.Evans DA, Hobbs BF, Oren C, Palmer KL. Modeling the effects of changes in new source review on national SO2 and NOx emissions from electricity-generating units. Environ Sci Technol. 2008;42:347–353. doi: 10.1021/es070003c. [DOI] [PubMed] [Google Scholar]
- 18.Mumford JL, He XZ, Chapman RS, Cao SR, Harris DB, Li XM, Xian YL, Jiang WZ, Xu CW, Chuang JC. Lung cancer and indoor air pollution in Xuan Wei, China. Science. 1987;235:217–220. doi: 10.1126/science.3798109. [DOI] [PubMed] [Google Scholar]
- 19.He XZ, Chen W, Liu ZY, Chapman RS. An epidemiological study of lung cancer in Xuan Wei County, China: current progress. Case-control study on lung cancer and cooking fuel. Environ Health Perspect. 1991;94:9–13. doi: 10.1289/ehp.94-1567943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lan Q, He X, Costa DJ, Tian L, Rothman N, Hu G, Mumford JL. Indoor coal combustion emissions, GSTM1 and GSTT1 genotypes, and lung cancer risk: a case-control study in Xuan Wei, China. Cancer Epidemiol Biomarkers Prev. 2000;9:605–608. [PubMed] [Google Scholar]
- 21.Liang CK, Quan NY, Cao SR, He XZ, Ma F. Natural inhalation exposure to coal smoke and wood smoke induces lung cancer in mice and rats. Biomed Environ Sci. 1988;1:42–50. [PubMed] [Google Scholar]
- 22.Tian L. Coal combustion emissions and lung cancer in Xuan Wei, China [ Thesis. University of California; Berkeley: 2005. [Google Scholar]
- 23.Rothman KJ. Modern Epidemiology. 1998. [Google Scholar]
- 24.Dai XD, Lin CY, Sun XW, Shi YB, Lin YJ. The etiology of lung cancer in nonsmoking females in Harbin, China. Lung Cancer. 1996;14 (Suppl 1):S85–S91. doi: 10.1016/s0169-5002(96)90213-5. [DOI] [PubMed] [Google Scholar]
- 25.Le CH, Ko YC, Cheng LS, Lin YC, Lin HJ, Huang MS, Huang JJ, Kao EL, Wang HZ. The heterogeneity in risk factors of lung cancer and the difference of histologic distribution between genders in Taiwan. Cancer Causes Control. 2001;12:289–300. doi: 10.1023/a:1011270521900. [DOI] [PubMed] [Google Scholar]
- 26.Wu AH, Henderson BE, Pike MC, Yu MC. Smoking and other risk factors for lung cancer in women. J Natl Cancer Inst. 1985;74:747–751. [PubMed] [Google Scholar]
- 27.Xu ZY, Blot WJ, Li G, Fraumeni JF, Jr, Zhao DZ, Stone BJ, Yin Q, Wu A, Henderson BE, Guan BP. Environmental determinants of lung cancer in Shenyang, China. IARC Sci Publ. 1991:460–465. [PubMed] [Google Scholar]
- 28.Zhang J, Smith KR. Indoor air pollution: a global health concern. Br Med Bull. 2003;68:209–225. doi: 10.1093/bmb/ldg029. [DOI] [PubMed] [Google Scholar]


