Abstract
Background
Excessive pregnancy weight gain appears to increase birth weight and the offspring’s risk for obesity later in life. However, this relationship may be confounded by genetic and other shared influences.
Methods
We used Vital Statistics Natality records to examine all known births in Michigan and New Jersey from 1989 to 2003. Our sample included 513,501 women who had more than one singleton pregnancy and their 1,164,750 offspring. We examined how differences in weight gain that occurred during two or more pregnancies for each woman predicted the birth weight of her offspring, using a within-subject design to minimize confounding.
Findings
We found a remarkably consistent relationship between pregnancy weight gain and birth weight (β 7.35 [95% CI 7.10–7.59], p < 0.0001). Infants of women who gain more than 24 kg during pregnancy were 148.9 g (CI 141.7–156.0) heavier at birth, compared to infants of women who gained 8–10 kg. The odds ratio of giving birth to an infant greater than 4000 g was 2.26 (2.09 – 2.44) for a woman who gained more than 24 kg during pregnancy, compared to a woman who gained 8–10 kg.
Interpretation
Maternal weight gain during pregnancy increases birth weight independent of genetic factors. In view of the apparent relationship between birth weight and adult weight, obesity prevention targeted to woman during pregnancy may be warranted.
INTRODUCTION
The fetal origin of adult disease, or prenatal programming, has been the subject of much study in the last 2 decades. Today, compelling evidence exists in support of the hypothesis, proposed by Barker et al,1–3 that undernutrition during pregnancy and low birth weight increase the risk for diabetes and cardiovascular disease in adulthood. Indeed, the adverse effect of perinatal undernutrition on long-term health may equal or exceed that of many conventional risk factors measured in adulthood.
In view of the rising prevalence of obesity, a variant of the original Barker hypothesis has been formulated, wherein overnutrition during pregnancy and high birth weight may cause obesity and related conditions in adulthood.4–9 According to this concept, excessive maternal body weight or weight gain in pregnancy perturbs the intrauterine environment during fetal development, producing permanent changes in the hypothalamus, pancreatic islet cells, adipose tissue or other biological systems that regulate body weight. Animal research provides an experimental basis for this possibilty.10, 11 Levin and Govek10 studied diet sensitive female rats on standard or high-energy diets prior to and during gestation. Progeny of the mothers in the high energy diet group gained more weight and had higher leptin levels than did progeny of mothers in the standard diet group, even though offspring from both groups were fed the same diet. In humans, high birth weight predicts body mass index (BMI) and adverse health outcomes later in life.12–21
Observational studies have generally found direct associations between maternal body weight or weight gain during pregnancy and birth weight or infant adiposity.22–26 Moreover, maternal adiposity tends to be more strongly related to birth weight27, 28 or childhood BMI29 than paternal adiposity. However, these studies involving comparisons between individuals have fundamental limitations, most notably confounding due to genetic and environmental factors. For example, excessive maternal weight gain may be related to high birth weight simply because a mother and her infant share obesity-related genes. Therefore, the aim of our study is to examine the associations between maternal weight gain, as a measure of overnutrition during pregnancy, and birth weight using state-based birth registry data that provide an opportunity to compare outcomes from several pregnancies in the same mother. This within-subject design serves to reduce or eliminate potential confounding by genetic, sociodemographic and other individual characteristics.
METHODS
Study overview
Data for this study come from individual Vital Statistics Natality records covering all births in Michigan and New Jersey from 1989 to 2003. These records provide information on birth outcomes and maternal characteristics, including weight gain during pregnancy. A summary of the data files, including covariates, is available from the National Center for Health Statistics: http://www.cdc.gov/nchs/births.htm.
The state of Michigan provided a file which identified children born to the same mother. For New Jersey, we performed this match on location in the state’s Department of Health offices based on mother’s name, race, birth date and, in some cases, address. The file was then de-identified. The study was conducted with approval from the Institutional Review Board at Columbia University.
Study population
From an initial sample size of 2,359,843 singleton births, we made the following exclusions: gestational age <37 or ≥ 41 weeks to focus on term pregnancies (n = 358,833 births); maternal diabetes (75,665 births); birth weight < 500 grams or > 7,000 grams, extreme values that could result from data entry error (2,225 births); missing data on pregnancy weight gain (192,819 births); and births to mothers with only 1 child in the database, per study design (1,204,249 births). All observed pregnancies for included mothers were retained in the sample. As a result of these exclusions, the final study sample consists of 1,164,750 singleton births to 513,501 mothers.
Data collection
All data used in this study are mandated by state law to be routinely collected and recorded in birth records. The variables include: pregnancy weight gain, birth weight, an indicator for diabetes during pregnancy, week of gestation, maternal age, maternal education, maternal marital status, maternal race and ethnicity, maternal smoking, adequacy of prenatal care, method of delivery, child gender, child parity, and year of birth.
Physicians were responsible for completing or verifying the birth records. Prior evaluation suggests that birth weight collected in this fashion is highly reliable.30 Physician report of pregnancy weight gain may have somewhat lower reliability. Especially for women with delayed prenatal care, physicians would likely base determination of pregnancy weight gain in part upon mothers’ self report. Consistent with this possibility, the weight gain variable shows evidence of “heaping” in the raw data with rounding to 10-pound increments, accounting for the irregular weight gain frequency distribution in Figure 1 noted especially around the 18 to 20 kg (40 pound) category. However, one validation study that compared birth certificate data to medical records for a random sample of births in North Carolina reported an exact concordance on pregnancy weight gain 82.8% of the time.31 Moreover, pregnancy weight gain obtained from birth records, similar to those we use in our study, has been associated with numerous infant and maternal health outcomes,32 providing evidence of validity. Pre-pregnancy weight and height were not routinely collected on birth certificates. Therefore, pre-pregnancy BMI could not be considered in this study, though absence of this information would not confound study findings for reasons considered below (see Discussion). Because the data files link births to the same mother, it is not possible to determine whether or not siblings had the same father.
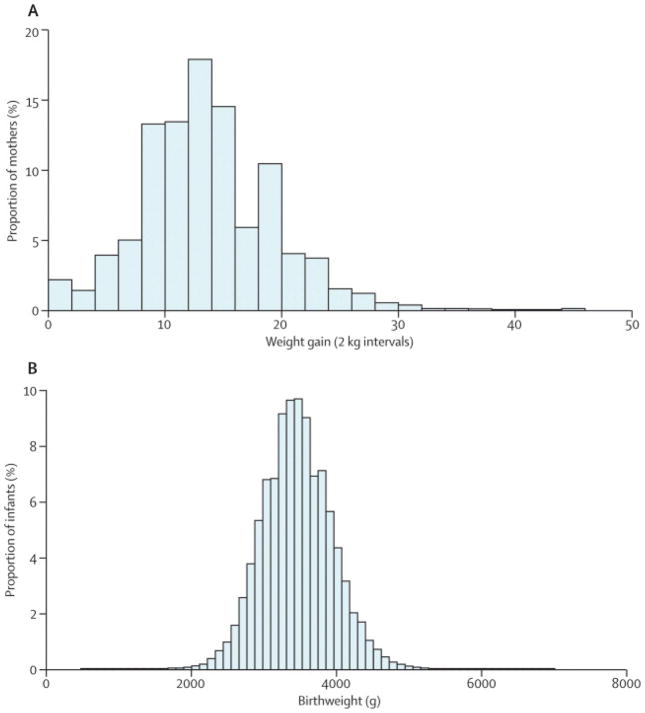
Figure 1.
Distribution of A) Pregnancy Weight Gain and B) Birth Weight.
Statistical analysis
Our primary hypothesis is that maternal weight gain during pregnancy is positively associated with birth weight, independent of confounding factors. The sample selection criteria serve to reduce or eliminate some sources of potential confounding (e.g., maternal diabetes or prematurity), but others remain. Of these remaining potential confounders, some are measured by variables in our data (smoking) whereas others are not (genetic determinants of birth weight). Our analytic strategy was to control for observable confounders through inclusion in the statistical models, and to control for unvarying unobservable confounders by comparing several pregnancies in the same mother. Using this approach, the influence of inter-individual differences in genes and other potentially relevant factors can be minimized.
Our models regress a measure of birth weight (continuous or dichotomous) on indicators for the following categories of maternal weight gain: 0–2, >2–4, >4–6, … >22–24, >24kg. Hence, the effects of weight gain are not constrained to be linear: unless otherwise noted, all of our specifications allow this flexible relationship between the measure of birth weight and the measure of maternal weight gain. The other covariates in all our models include: child gender, maternal education (less than high school, high school, some college, college or more), maternal marital status, an indicator for maternal smoking during pregnancy, child parity (indicators for parity of 1, 2, 3, 4, 5 or more; N.B., the first birth observed in the data is not necessarily the mother’s first born child), indicators for each year of maternal age, and indicators for each year of birth. We included year of birth as a covariate to control for possible secular trends in birth weight unrelated to maternal weight gain during pregnancy. Where categorical data on controls are missing, we also include controls for missing variables.
For models using birth weight as a continuous variable, we conducted two analyses. First, we estimated models that include maternal fixed effects using the XTREG command in STATA (Release 11, STATA Corp., College Station TX). Any maternal covariate that does not change over time will be controlled by this procedure.33 Thus, the effect of the mother’s weight prior to first observed pregnancy is controlled, as is the effect of maternal height (even though neither are observed in our data). Although fixed effects estimates may be less precise than ordinary least squares models, this issue is of little concern in a large sample size.34 We accounted for the presence of multiple values for each mother by using the CLUSTER command in STATA to correlate and adjust the errors. This procedure did not materially change our mean estimates or confidence intervals, and therefore data are presented without clustering.
As an alternative, conceptually simpler analytic method to control for covariates that change between but not within individuals, we calculated the differences in weight gain and in birth weight between adjacent pregnancies for each mother. We then regressed changes in birth weight on categories of changes in maternal weight gain (<−12, >=−12 to −10, … >10 to <=12, >12 kg), including those of the other covariates described above which can vary between births for the same mother. The sample in these models was restricted to sibling pairs in which the difference in gestational age is less than 3 weeks. In these “first difference” models, changes in the year of birth and in maternal age are the same. Also, most changes in parity are equal to one. Therefore, we included indicators for each year of maternal age at the time of the first observed birth, and indicators for parity of the first birth observed in the data set. The distribution of changes in weight gain suggests that on average women gain slightly less weight for higher order pregnancies: the 10th, 50th and 90th percentiles of the distribution of the difference in pregnancy weight gain between an older sibling and the next younger sibling are 6.24, −.45, and −8.62 kg respectively. In other words, the majority of women gain rather similar amounts of weight over subsequent pregnancies.
We also estimated models using a dichotomous “high birth weight” (>4000 g) measure as the dependent variable. The independent variables were categories of maternal weight gain (0–2, >2–4, >4–6, … >24 kg). We estimated a fixed effect logit (or conditional logit) using the CLOGIT procedure in STATA.35 These models control for the same variables as the fixed effects models discussed above. Finally, we conducted subgroup analyses to examine for effect modification. Based on our primary results, we constrained the main effect of pregnancy weight gain to be linear; that is, the weight gain categories included in the previous models were excluded, and only a single continuous weight gain variable (and its interaction) were included.
We chose 8 to 10 kg as the reference pregnancy weight gain category for Figures 2a and 3 because this category is within the 7.0 – 11.5 kg range recommended for overweight women by the Institute of Medicine36 and because the mean BMI among adult women in the US is within the overweight range. All data are presented as means and standard deviations (SD, for maternal cohort characteristics) or 95% confidence intervals (CI, for outcome data).
Figure 2.
Associations Between Pregnancy Weight Gain and Birth Weight. Data from a) fully adjusted fixed effect model, using a reference group of 8–10kg; and b) first difference model, subtracting values of variables from the first observed pregnancy from those of the second observed pregnancy for each woman. Grey bands indicated 95% confidence intervals.
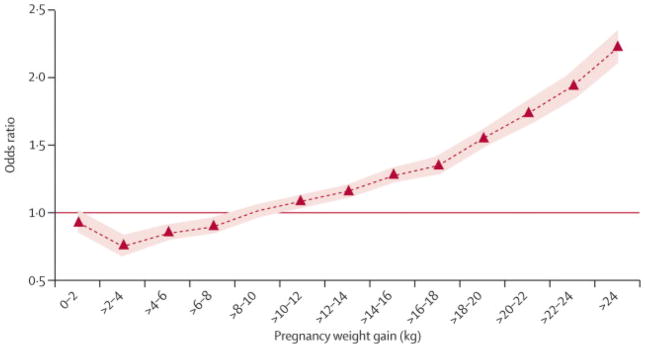
Figure 3.
Odds Ratio for High Birth Weight (> 4000 g). Grey bands indicate 95% confidence intervals.
Role of the funding sources
Funding sources had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. David Ludwig had full access to all data analyses and Janet Currie had full access to all primary data in the study; both had final responsibility to submit for publication.
RESULTS
Table 1 presents descriptive characteristic of the 513,501 women and 1,164,750 offspring included in the study. These characteristics were similar to the 77,125 women and 192,819 offspring excluded from the study because of missing data on pregnancy weight gain. Mean maternal weight gain was 13.7 kg and the mean birth weight was 3453 g. Approximately 12% (n = 138,304) of the offspring had birth weight greater than 4000 g. On average, each mother had 2.41 offspring in the data set, and the mean birth order was 2.17. African Americans comprised 19.0% (n = 220,904) of the offspring and Hispanics comprised 10.0% (n = 116,490). The average mother had 13.2 years of education and 13.2% (n = 154,221) of the offspring had mothers who smoked during pregnancy.
Table 1.
Descriptive characteristics of the mothers and offspring included in the study. (Mean ± Standard Deviation)
| Mother Characteristics | Mean for analysis sample* | Mean including those with missing weight gain** |
|---|---|---|
| Maternal weight gain (lb) | 13.7 ± 5.7 | |
| Maternal age (years) | 27.7 ± 5.8 | 27.7 ± 5.8 |
| Race/ethnicity (%) | ||
| African American | 19.0 | 20.1 |
| Hispanic | 10.0 | 9.9 |
| White/Other | 71.0 | 70.0 |
| Mother’s education (years) | 13.2 ± 2.5 | 13.1 ± 2.5 |
| Mother smoker (%) | 13.2 | 12.8 |
| Adequacy of prenatal care (%) | 55.4 ± 49.7 | 55.8 ± 49.7 |
| Infant Characteristics | ||
| Parity | 2.17 ± 1.24 | 2.17 ± 1.25 |
| Birth weight (g) | 3453 ± 473 | 3446 ± 477 |
| Birth Weight > 4000 grams (%) | 11.9 | 11.7 |
| Offspring gender (% male) | 51.0 | 51.0 |
| Number of offspring observed | 2.41 ± 0.73 | 2.46 ± 0.79 |
| Gestation length (weeks) | 39.3 ± 1.1 | 39.3 ± 1.1 |
Sample size = 513,501 mothers and 1,164,750 offspring
Sample size = 590,626 mothers and 1,357,569 offspring. Includes siblings of offspring for whom pregnancy weight gain was missing.
Figure 1a shows that many women exceeded recommended limits for weight gain during a singleton pregnancy, currently established as 11.5–16 kg for those with normal prepregnancy weight, 7–11.5 kg for those with overweight, and 5–9 kg for those with obesity.36 Weight gain of over 20 kg occurred in 11.9% (n = 139,040) of pregnancies. As expected, pregnancy weight gain was positively associated with length of pregnancy (p < 0.0001) and inversely associated with smoking (p < 0.0001). Figure 1b shows that the birth weight distribution was approximately normal, with very few greater than 5000 g.
Figure 2a, using a fixed effects model, demonstrates a remarkably consistent relationship between maternal weight gain and birth weight (β 7.35 [CI 7.10–7.59], p < 0.0001). Relative to the reference category of 8–10 kg, infants of mothers who gained 20–22 kg weighed 103.8 g (CI 97.0–110.6) more on average, while infants of mothers who gained over 24 kg weighed 148.9 g (CI 141.7–156.0) more.
Figure 2b plots coefficient estimates from the “first difference” model (see Methods). As expected, women who gained the same amount of weight in both pregnancies had infants of similar mean birth weight. Women who gained over 12 kg more in the second pregnancy had second infants who weighed 107.6 g (CI 98.2–117.0) more than first infants, and those who gained over 12 kg less in the second pregnancy had second infants who weighed 85.8 g (CI 93.5–78.1) less.
Figure 3 shows the odds ratio for birth weight above 4000 g according to pregnancy weight gain from the conditional logit models. Relative to the reference category of 8–10 kg, the odds ratio of having a baby with high birth weight was 1.72 (CI 1.59–1.86) for those who gained between 20 and 22 kg, and 2.26 (CI 2.09–2.44) for woman who gained more than 24 kg.
To test for residual confounding, we excluded women who had ever smoked, those who delivered by caesarean section, and those who had any pregnancy with gestational length < 39 wk or > 40 weeks. The results of these analyses were not materially different from those of our other models (data not shown). To examine the reliability of the independent variable, we performed an analysis limited to the 208,067 women and their 469,472 infants with adequate prenatal care indicated on the birth certificate. (The excluded women would have relatively less data in the medical record upon which an accurate assessment of pregnancy weight gain could be based, causing the physician to rely more on maternal self report.) These results were very similar to those of the full group (data not shown).
We also looked for evidence of effect modification in additional subgroup analyses that included a “main effect” of weight gain (β), and an interaction describing the differential weight gain between the main group and the subgroup (γ). Based on our primary results, we constrained the main effect of pregnancy weight gain to be linear. The slope for the relationship between pregnancy weight gain and birth weight was modestly smaller for African Americans (β = 7.63, 7.34–7.91; γ = −1.05, −1.60 – −.50), and larger for male infants (β = 7.01, 6.69 – 7.33; γ = 0.66, 0.26 – 1.05). There was no effect of older maternal age (age >= 28, β = 7.39, 7.23 – 7.71; γ = −0.11, −0.54 – 0.34) or state (Michigan: β = 7.62, 7.23 – 8.00; γ = −.46, −0.95 – 0.04).
DISCUSSION
Weight gain during pregnancy has been associated with birth weight and measures of adiposity early in life. This study, using a state-based registry with more than one million singleton births, provides evidence for a causal relationship independent of shared genes. We observed that every additional kg of pregnancy weight gain increases birth weight by about 7.35 g and that variation in pregnancy weight gain through the observed range can affect birth weight by approximately 200 g. Because high birth weight predicts BMI later in life,12, 14, 17–19, 21 these findings suggest that excessive pregnancy weight gain may increase the long-term risk for obesity-related disease in the offspring. High birth weight may also increase risk for other diseases later in life, including asthma, atopy and cancer.13, 15, 16, 20
With regard to potential mechanisms, the physiologic pathways that may link fetal overnutrition to higher birth weight have been described. During pregnancy, insulin resistance develops in the mother in order to shunt vital nutrients to the growing fetus.37 Excessive weight or weight gain during pregnancy exaggerates this normal process by further increasing insulin resistance and possibly also by altering other maternal hormones that regulate placental nutrient transporters.38 The resulting excessive rate of nutrient transfer stimulates fetal insulin secretion, overgrowth and increased adiposity. Indeed, maternal postprandial glycemia, even within the normal range, is strongly associated with birth weight in the third trimester.39 The mechanisms whereby in utero overnutrition and related physiological derangements affect body weight later in life remain speculative,9, 11, 38 though the critical role of maternal hyperglycemia is highlighted by recent research.40
The primary limitations of this study involve the possibility of measurement error and confounding. The pregnancy weight gain variable, more so than birth weight, is subject to recall and reporting bias that may vary by BMI, education and level of prenatal care, among other factors. However, the within subject design would tend to minimize systematic bias arising from such factors. Thus, some individuals may tend to underestimate, and others overestimate weight gain, though each would likely do so in a similar fashion across multiple pregnancies. Any random measurement error would tend to diminish apparent effect size,41 causing our estimates to be conservative. In addition, results of a secondary analysis excluding individuals with inadequate prenatal care – a group especially subject to error in the measurement of pregnancy weight gain – were very similar to the primary analysis. Other evidence of reliability derives from associations in the expected direction here (with length of pregnancy and smoking) and elsewhere (with preeclampsia, cephalopelvic disproportion, failed induction and cesarean delivery)32 involving the pregnancy weight gain variable obtained from birth certificates. Furthermore, a validation study showed an exact concordance between pregnancy weight gain obtained from birth certificates and from medical records 82.8% of the time.31
Our within-subject design should effectively eliminate confounding by genetic and other unvarying factors. An important study limitation is the lack of information on maternal prepregnancy BMI. We address this limitation to some degree through the use of fixed effects models and adjustment for age and parity, controlling in part for BMI prior to the first pregnancy and weight change between pregnancies. In any event, we contend that absence of prepregnancy BMI could not account for the primary findings for a fundamental statistical reason. In order for a confounder to explain a positive association between an independent variable and a dependent variable, it must be associated with both in the same fashion, either positive or inverse. But prepregnancy BMI is inversely associated with pregnancy weight gain,42–44 and positively associated with birth weight.22–26 In addition, we used a secondary analytic approach to examine for residual confounding, comparing differences in subsequent pregnancies for each woman (Figure 2b). We found that weight gain had a similar effect on birth weight regardless of which pregnancy had greater weight gain. This would not have occurred if prepregnancy BMI differed between pregnancies in a systematic way that confounded findings. We recognize that pregnancy weight gain might affect birth weight differently among women with high compared to low prepregnancy BMI (i.e, effect modification). However, the similarity in findings from analyses involving subgroups expected to differ in prepregnancy BMI, such as older and younger women or blacks and white, provides evidence against this possibility (and against confounding). Moreover, unrecognized effect modification by prepregnancy BMI, diet quality, physical activity level or other factors wouldn’t threaten the validity of the study’s primary findings.
Several other methodological issues merit consideration. Concern for reverse causation can be largely dismissed, because increased fetal weight would make a small contribution (< 10%) to the associated increase in maternal weight. Even so, we cannot rule out the possibility that hormonal or metabolic signals from the fetus might have an additional influence on maternal weight. Some women with unrecognized diabetes may exist in our sample and contribute to the observed effect size, especially if they developed the disease in some but not all of their pregnancies. Furthermore, diagnostic criteria and screening practices may have change during the study period. We aimed to minimize these influences by excluding individuals who reported diabetes during any pregnancy, a group that would be at highest risk during every pregnancy. In addition, there was no significant difference in a subgroup analysis involving older women, who are at substantially increased risk for this complication.45 Finally, we recognize the lack of information about paternity as a study limitation. However, the similar effect of maternal weight gain on birth weight in first and second pregnancies, regardless of which had greater weight gain (Figure 2b), argues against any systematic bias.
In conclusion, our findings suggest that excessive maternal weight gain during pregnancy increases birth weight. In view of the apparent association between high birth weight and adult adiposity, an advantageous time to initiate obesity prevention efforts may be during pregnancy.
Acknowledgments
The collection of data used in this project was supported under NIH R21 HD055613-01. DSL was supported in part by a career grant from the NIDDK (K24 DK082730) and a grant from the New Balance Foundation. Cecilia Machado provided assistance with research. We thank Drs. Cara Ebbeling, Matthew Gillman, Steven Gortmaker, Joseph Majzoub and Eric Rimm for critical review of the manuscript.
Footnotes
Contributors: Both authors contributed to the design of the study and drafting of the manuscript. DSL formulated the study hypotheses and JC supervised data collection and analysis.
Conflict of interest statement: The authors have no conflicts of interest with respect to this work. The authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Barker DJ, Gluckman PD, Godfrey KM, Harding JE, Owens JA, Robinson JS. Fetal nutrition and cardiovascular disease in adult life. Lancet. 1993;341:938–941. doi: 10.1016/0140-6736(93)91224-a. [DOI] [PubMed] [Google Scholar]
- 2.Barker DJ, Osmond C, Forsen TJ, Kajantie E, Eriksson JG. Trajectories of growth among children who have coronary events as adults. N Engl J Med. 2005;353:1802–1809. doi: 10.1056/NEJMoa044160. [DOI] [PubMed] [Google Scholar]
- 3.Hales CN, Barker DJ. Type 2 (non-insulin-dependent) diabetes mellitus: the thrifty phenotype hypothesis. Diabetologia. 1992;35:595–601. doi: 10.1007/BF00400248. [DOI] [PubMed] [Google Scholar]
- 4.Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360:473–482. doi: 10.1016/S0140-6736(02)09678-2. [DOI] [PubMed] [Google Scholar]
- 5.Barker DJ. Obesity and early life. Obes Rev. 2007;8:45–49. doi: 10.1111/j.1467-789X.2007.00317.x. [DOI] [PubMed] [Google Scholar]
- 6.Eriksson J, Forsen T, Tuomilehto J, Osmond C, Barker D. Size at birth, childhood growth and obesity in adult life. Int J Obes Relat Metab Disord. 2001;25:735–740. doi: 10.1038/sj.ijo.0801602. [DOI] [PubMed] [Google Scholar]
- 7.Oken E, Gillman MW. Fetal origins of obesity. Obes Res. 2003;11:496–506. doi: 10.1038/oby.2003.69. [DOI] [PubMed] [Google Scholar]
- 8.Pettitt DJ, Jovanovic L. Birth weight as a predictor of type 2 diabetes mellitus: the U-shaped curve. Curr Diab Rep. 2001;1:78–81. doi: 10.1007/s11892-001-0014-x. [DOI] [PubMed] [Google Scholar]
- 9.Whitaker RC, Dietz WH. Role of the prenatal environment in the development of obesity. J Pediatr. 1998;132:768–776. doi: 10.1016/s0022-3476(98)70302-6. [DOI] [PubMed] [Google Scholar]
- 10.Levin BE, Govek E. Gestational obesity accentuates obesity in obesity-prone progeny. Am J Physiol. 1998;275:R1374–1379. doi: 10.1152/ajpregu.1998.275.4.R1374. [DOI] [PubMed] [Google Scholar]
- 11.Wu Q, Suzuki M. Parental obesity and overweight affect the body-fat accumulation in the offspring: the possible effect of a high-fat diet through epigenetic inheritance. Obes Rev. 2006;7:201–208. doi: 10.1111/j.1467-789X.2006.00232.x. [DOI] [PubMed] [Google Scholar]
- 12.Araujo CL, Hallal PC, Nader GA, et al. Effect of birth size and proportionality on BMI and skinfold thickness in early adolescence: prospective birth cohort study. Eur J Clin Nutr. 2009;63:634–639. doi: 10.1038/ejcn.2008.20. [DOI] [PubMed] [Google Scholar]
- 13.Eriksson M, Wedel H, Wallander MA, et al. The impact of birth weight on prostate cancer incidence and mortality in a population-based study of men born in 1913 and followed up from 50 to 85 years of age. Prostate. 2007;67:1247–1254. doi: 10.1002/pros.20428. [DOI] [PubMed] [Google Scholar]
- 14.Gillman MW, Rifas-Shiman S, Berkey CS, Field AE, Colditz GA. Maternal gestational diabetes, birth weight, and adolescent obesity. Pediatrics. 2003;111:e221–226. doi: 10.1542/peds.111.3.e221. [DOI] [PubMed] [Google Scholar]
- 15.Harder T, Plagemann A, Harder A. Birth weight and subsequent risk of childhood primary brain tumors: a meta-analysis. Am J Epidemiol. 2008;168:366–373. doi: 10.1093/aje/kwn144. [DOI] [PubMed] [Google Scholar]
- 16.Hjalgrim LL, Westergaard T, Rostgaard K, et al. Birth weight as a risk factor for childhood leukemia: a meta-analysis of 18 epidemiologic studies. Am J Epidemiol. 2003;158:724–735. doi: 10.1093/aje/kwg210. [DOI] [PubMed] [Google Scholar]
- 17.Leong NM, Mignone LI, Newcomb PA, et al. Early life risk factors in cancer: the relation of birth weight to adult obesity. Int J Cancer. 2003;103:789–791. doi: 10.1002/ijc.10886. [DOI] [PubMed] [Google Scholar]
- 18.Parsons TJ, Power C, Logan S, Summerbell CD. Childhood predictors of adult obesity: a systematic review. Int J Obes Relat Metab Disord. 1999;23:S1–107. [PubMed] [Google Scholar]
- 19.Pietilainen KH, Kaprio J, Rasanen M, Winter T, Rissanen A, Rose RJ. Tracking of body size from birth to late adolescence: contributions of birth length, birth weight, duration of gestation, parents’ body size, and twinship. Am J Epidemiol. 2001;154:21–29. doi: 10.1093/aje/154.1.21. [DOI] [PubMed] [Google Scholar]
- 20.Remes ST, Patel SP, Hartikainen AL, Jarvelin MR, Pekkanen J. High birth weight, asthma and atopy at the age of 16 yr. Pediatr Allergy Immunol. 2008;19:541–543. doi: 10.1111/j.1399-3038.2007.00707.x. [DOI] [PubMed] [Google Scholar]
- 21.Wei JN, Li HY, Sung FC, et al. Birth weight correlates differently with cardiovascular risk factors in youth. Obesity (Silver Spring) 2007;15:1609–1616. doi: 10.1038/oby.2007.190. [DOI] [PubMed] [Google Scholar]
- 22.Eastman NJ, Jackson E. Weight relationships in pregnancy. I. The bearing of maternal weight gain and pre-pregnancy weight on birth weight in full term pregnancies. Obstet Gynecol Surv. 1968;23:1003–1025. [PubMed] [Google Scholar]
- 23.Fleten C, Stigum H, Magnus P, Nystad W. Exercise during pregnancy, maternal prepregnancy body mass index, and birth weight. Obstet Gynecol. 2010;115:331–337. doi: 10.1097/AOG.0b013e3181ca4414. [DOI] [PubMed] [Google Scholar]
- 24.Getahun D, Ananth CV, Peltier MR, Salihu HM, Scorza WE. Changes in prepregnancy body mass index between the first and second pregnancies and risk of large-for-gestational-age birth. Am J Obstet Gynecol. 2007;196:e531–538. doi: 10.1016/j.ajog.2006.12.036. [DOI] [PubMed] [Google Scholar]
- 25.Simpson JW, Lawless RW, Mitchell AC. Responsibility of the obstetrician to the fetus. II. Influence of prepregnancy weight and pregnancy weight gain on birthweight. Obstet Gynecol. 1975;45:481–487. [PubMed] [Google Scholar]
- 26.Verhaeghe J, van Bree R, Van Herck E. Maternal body size and birth weight: can insulin or adipokines do better? Metabolism. 2006;55:339–344. doi: 10.1016/j.metabol.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 27.Guillaume M, Lapidus L, Beckers F, Lambert A, Bjorntorp P. Familial trends of obesity through three generations: the Belgian-Luxembourg child study. Int J Obes Relat Metab Disord. 1995;3:S5–9. [PubMed] [Google Scholar]
- 28.Okun N, Verma A, Mitchell BF, Flowerdew G. Relative importance of maternal constitutional factors and glucose intolerance of pregnancy in the development of newborn macrosomia. J Matern Fetal Med. 1997;6:285–290. doi: 10.1002/(SICI)1520-6661(199709/10)6:5<285::AID-MFM9>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 29.Lawlor DA, Smith GD, O’Callaghan M, et al. Epidemiologic evidence for the fetal overnutrition hypothesis: findings from the mater-university study of pregnancy and its outcomes. Am J Epidemiol. 2007;165:418–424. doi: 10.1093/aje/kwk030. [DOI] [PubMed] [Google Scholar]
- 30.Northam S, Knapp TR. The reliability and validity of birth certificates. J Obstet Gynecol Neonatal Nurs. 2006;35:3–12. doi: 10.1111/j.1552-6909.2006.00016.x. [DOI] [PubMed] [Google Scholar]
- 31.Buescher PA, Taylor KP, Davis MH, Bowling JM. The quality of the new birth certificate data: a validation study in North Carolina. Am J Public Health. 1993;83:1163–1165. doi: 10.2105/ajph.83.8.1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.DeVader SR, Neeley HL, Myles TD, Leet TL. Evaluation of gestational weight gain guidelines for women with normal prepregnancy body mass index. Obstet Gynecol. 2007;110:745–751. doi: 10.1097/01.AOG.0000284451.37882.85. [DOI] [PubMed] [Google Scholar]
- 33.Allison PD. Fixed effects regression models. Vol. 160. Los Angeles: Sage Publications; 2009. [Google Scholar]
- 34.Kaufman JS. Commentary: Why are we biased against bias? Int J Epidemiol. 2008;37:624–626. doi: 10.1093/ije/dyn035. [DOI] [PubMed] [Google Scholar]
- 35.Chamberlain G. Analysis of Covariance with Qualitative Data. Rev Economic Studies. 1980;47:225–238. [Google Scholar]
- 36.Kuehn BM. Guideline for pregnancy weight gain offers targets for obese women. JAMA. 2009;302:241–242. doi: 10.1001/jama.2009.964. [DOI] [PubMed] [Google Scholar]
- 37.Ryan EA. Hormones and insulin resistance during pregnancy. Lancet. 2003;362:1777–1778. doi: 10.1016/S0140-6736(03)14942-2. [DOI] [PubMed] [Google Scholar]
- 38.Jansson N, Nilsfelt A, Gellerstedt M, et al. Maternal hormones linking maternal body mass index and dietary intake to birth weight. Am J Clin Nutr. 2008;87:1743–1749. doi: 10.1093/ajcn/87.6.1743. [DOI] [PubMed] [Google Scholar]
- 39.Parretti E, Mecacci F, Papini M, et al. Third-trimester maternal glucose levels from diurnal profiles in nondiabetic pregnancies: correlation with sonographic parameters of fetal growth. Diabetes Care. 2001;24:1319–1323. doi: 10.2337/diacare.24.8.1319. [DOI] [PubMed] [Google Scholar]
- 40.Hillier TA, Pedula KL, Schmidt MM, Mullen JA, Charles MA, Pettitt DJ. Childhood obesity and metabolic imprinting: the ongoing effects of maternal hyperglycemia. Diabetes Care. 2007;30:2287–2292. doi: 10.2337/dc06-2361. [DOI] [PubMed] [Google Scholar]
- 41.Alwin DF. Margins of error: a study of reliability in survey measurement. Wiley-Interscience; 2007. [Google Scholar]
- 42.Dietz PM, Callaghan WM, Sharma AJ. High pregnancy weight gain and risk of excessive fetal growth. Am J Obstet Gynecol. 2009;201:e51–56. doi: 10.1016/j.ajog.2009.04.051. [DOI] [PubMed] [Google Scholar]
- 43.Nohr EA, Vaeth M, Baker JL, Sorensen TI, Olsen J, Rasmussen KM. Pregnancy outcomes related to gestational weight gain in women defined by their body mass index, parity, height, and smoking status. Am J Clin Nutr. 2009;90:1288–1294. doi: 10.3945/ajcn.2009.27919. [DOI] [PubMed] [Google Scholar]
- 44.Wise LA, Palmer JR, Heffner LJ, Rosenberg L. Prepregnancy body size, gestational weight gain, and risk of preterm birth in African-American women. Epidemiology. 2010;21:243–252. doi: 10.1097/EDE.0b013e3181cb61a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.King H. Epidemiology of glucose intolerance and gestational diabetes in women of childbearing age. Diabetes Care. 1998;21:B9–13. [PubMed] [Google Scholar]