Abstract
Background and objectives: Off-pump coronary artery bypass grafting (CABG) has been advocated to cause less inflammation, morbidity, and mortality than the more traditional on-pump technique. This meta-analysis compares these two surgical techniques with respect to causing acute kidney injury (AKI).
Design, setting, participants, & measurements: This study searched for randomized controlled trials in MEDLINE and abstracts from the proceedings of scientific meetings through February 2010. Included were trials comparing off-pump to on-pump CABG that reported the incidence of AKI, as defined by a mixture of criteria including biochemical parameter/urine output/dialysis requirement. Mortality was evaluated among the studies that reported kidney-related outcomes. For primary and subgroup analyses, fixed-effect meta-analyses of odds ratios (OR) were performed.
Results: In 22 identified trials (4819 patients), the weighted incidence of AKI in the on-pump CABG group was 4.0% (95% confidence interval [CI] 1.8%, 8.5%), dialysis requirement 2.4% (95% CI 1.6%, 3.7%), and mortality 2.6% (95% CI 1.6%, 4.0%). By meta-analysis, off-pump CABG was associated with a 40% lower odds of postoperative AKI (OR 0.60; 95% CI 0.43, 0.84; P = 0.003) and a nonsignificant 33% lower odds for dialysis requirement (OR 0.67; 95% CI 0.40, 1.12; P = 0.12). Within the selected trials, off-pump CABG was not associated with a significant decrease in mortality.
Conclusions: Off-pump CABG may be associated with a lower incidence of postoperative AKI but may not affect dialysis requirement, a serious complication of cardiac surgery. However, the different definitions of AKI used in individual trials and methodological concerns preclude definitive conclusions.
First introduced in the 1960s (1–3), coronary artery bypass grafting (CABG) remains the standard of care for symptomatic patients with three-vessel or left main coronary artery disease (4,5). For the past 30 years, CABG has been performed primarily with the use of an extracorporeal cardiopulmonary bypass (CPB) machine (on-pump) requiring cannulation of the heart and aorta, crossclamping of the ascending aorta, and the induction of cardioplegic arrest. However, in the 1990s, interest emerged in performing off-pump CABG (6,7) with the hope of reducing postoperative complications associated with the use of CPB, including the generalized systemic inflammatory response (8) and acute organ dysfunction such as cerebral dysfunction (9), myocardial depression (10), and prolonged mechanical ventilation (11).
Acute kidney injury (AKI) is a serious complication of on-pump CABG, ranging from small postoperative increases in serum creatinine observed in 5% to 20% of patients (12,13) to severe forms requiring dialysis developing in 1% of patients (14,15). Whether defined by various serum creatinine increments or dialysis requirement, AKI has been linked to excessive in-hospital morbidity and mortality (12,14) and increased resource consumption (16,17). With an estimated 176,000 cardiac bypass procedures performed in 2007 (18), preventing AKI postoperatively is an important goal.
Previously published studies comparing the effect of off-pump versus on-pump CABG on kidney end points have yielded conflicting results. Although six meta-analyses have examined this question, results were inconclusive (19,20) or the data synthesis included studies of various designs with a mixture of randomized controlled trials (RCTs) and observational studies (21–24). To shed further light on this question, we conducted a comprehensive meta-analysis restricted to all RCTs published to date, comparing the effect of off-pump versus on-pump CABG on development of AKI including dialysis requirement.
Materials and Methods
Eligibility Criteria
We included all RCTs that examined postoperative primary or secondary kidney end points (as defined below) in adults undergoing off-pump versus on-pump CABG surgery. We excluded duplicate publications. If authors published more than one manuscript on the same study, data from the most inclusive report were used.
Search Strategy
We searched MEDLINE (1966 to February 2010) using the following MeSH database search terms: “Coronary Artery Bypass,” “Coronary Artery Bypass, Off-Pump,” “Cardiopulmonary Bypass,” “Heart Bypass, Left,” or “Extracorporeal Circulation,” and “Heart, Artificial.” The search strategy was limited to human RCTs with no language restrictions. We also searched ClinicalTrials.gov for completed trials using similar search terms; reviewed abstracts from the annual scientific meetings of the American Society of Nephrology (2000 to 2009), American College of Chest Physicians (2003 to 2009), and American Heart Association (2003 to 2009); and performed a manual search of references in narrative reviews and previously published systematic reviews on CABG.
Study Selection
Two independent reviewers (S.A. and V.F.S.) screened the titles and abstracts of all electronic citations. The full-text articles were retrieved for comprehensive review and rescreened. A third reviewer (A.H.P.) screened the abstracts from the annual scientific meetings.
Outcome Measures
The primary outcome was AKI, as defined in individual trials. We focused on AKI in general and dialysis requirement specifically. For the purpose of the meta-analysis, dialysis was defined as the need for hemodialysis or continuous renal replacement therapy (e.g., hemofiltration). The secondary outcome was all-cause mortality and was evaluated only among trials that reported kidney end points.
Data Abstraction
Two reviewers (S.A. and V.F.S.) independently extracted in duplicate the following data from full-text articles: country of origin, year of publication, period of study, study design, population setting (first versus redo CABG), surgery electivity, patient summary characteristics (including sex, mean age, prevalence of hypertension, and diabetes mellitus), mean aortic cross-clamp and CPB time, definition of AKI, and duration of follow-up. Disagreements were resolved through consensus. Eleven authors were contacted by e-mail (up to three attempts per author) for additional information, including confirmation that there were no duplicate data and clarification of the AKI definition used in trials (25–35). Five authors provided additional information (25,29,30,32,33).
Quality Assessment
One reviewer (V.F.S.) assessed the quality of the trials using the Jadad scale, (36), which is based on the adequacy of randomization, blinding, and attrition. This 0 to 5 scale, with a score of 5 corresponding to “best” quality, was used as a surrogate for overall quality assessment (Appendix 1).
Statistical Analyses
We performed meta-analyses of the odds ratio (OR) for AKI, dialysis requirement, and death in patients undergoing off-pump CABG relative to those undergoing on-pump CABG. Because of the low number of events in most studies (often zero in one study group), we used the Peto fixed-effect model for our primary analysis (37,38). As a sensitivity analysis, we also performed a random-effects model meta-analysis (39). For both methods, the studies with no events in both groups were excluded from the meta-analyses. For graphical purposes, we calculated the OR for studies with no events in either group by adding 0.5 to the numbers of events and nonevents and displayed the resulting OR in the forest plots. We calculated the I2 and the χ2 P value to assess for heterogeneity among studies. To evaluate the heterogeneity, we performed subgroup analyses using the Peto fixed-effect model on the basis of a priori selected characteristics including mean age (<65 versus ≥65 years), percentage with diabetes mellitus (<25 versus ≥25%), sample size (less than versus median or greater), AKI incidence rate and mortality rate in the on-pump CABG group (less than versus median or greater), surgery setting (elective versus urgent/elective), AKI definition (biochemical parameter/urine output versus dialysis requirement), percentage with hypertension (less than versus median or greater), and study quality (defined by the Jadad score). The t test was used to compare subgroups. The summary control rates (event rates in the on-pump CABG groups) were determined with random-effects model meta-analysis, including studies with no events. The meta-analyses were performed using MetaAnalyst beta version 3.1 (Tufts University, Boston, MA) (40) and the metan command (version 9) in Stata version 11 (41).
Results
Study Characteristics
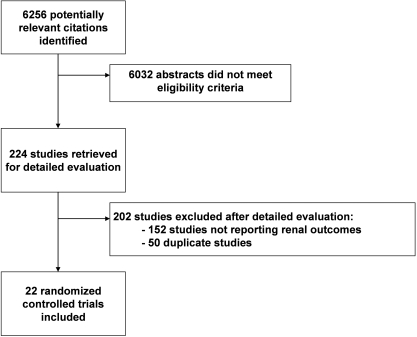
A total of 6256 potentially relevant citations were identified and screened, of which 5232 originated from MEDLINE; 224 articles were retrieved for detailed evaluation, of which 22 fulfilled eligibility criteria (Figure 1) (25–30,32–35,42–53).
Figure 1.
Study selection flow diagram.
Characteristics of the individual trials are displayed in Table 1. The trials spanned more than 10 years and varied in sample size from 20 to 2203 patients. All trials had more men, ranging from 52% to 99%, with a range of mean ages of 48 to 76 years. When reported, mean preoperative serum creatinine ranged from 1.0 to 1.5 mg/dl. By design, one trial restricted enrollment to patients with pre-existing chronic kidney disease (52) and another study was restricted to patients undergoing urgent CABG (32). All 22 studies reported on the incidence of AKI, with seven studies defining AKI exclusively as the need for dialysis (25,26,33,47,49–51). Six studies did not describe the criteria used to define AKI (27,34,35,42,46,48). The remaining nine studies defined AKI using variable absolute or relative increases in serum creatinine, decreases in GFR, decreases in urine output, or need for dialysis (Table 2) (28–30,32,43–45,52,53).
Table 1.
Characteristics of the RCTs included in the meta-analysis
| Author | Year | Country | Study Period | Population Setting | Number of Patientsa | Surgery Status | Men (%) | Age (years) | Hypertension (%) | Diabetes Mellitus | Preoperative Serum Creatinine (mg/dl) |
On-Pump Cross-Clamp Time (minutes) | On-Pump CPB Time (minutes) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Off-pump CABG | On-pump CABG | |||||||||||||
| Vural | 1995 | Turkey | NR | CABG | 50 | NR | 88 | 48 | NR | NR | NR | NR | NR | NR |
| Ascione | 1999 | United Kingdom | NR | First CABG | 200 | Elective | 81 | 62 | NR | 16 | NR | NR | 42 | 67 |
| van Dijk | 2001 | The Netherlands | 1998 to 2000 | First CABG | 281 | Elective | 68 | 61 | 42 | 13 | 1.0 | 1.0 | 44 | 66 |
| Tang | 2002 | United Kingdom | NR | CABG | 45 | Elective | 80 | 63 | NR | 0 | 1.1 | 1.1 | NR | NR |
| Carrier | 2003 | Canada | 2001 to 2002 | First and redo CABGb | 65 | NR | 77 | 70 | 81 | 48 | NR | NR | NR | NR |
| Puskas | 2003 | USA | 2000 to 2001 | Primary CABG | 200 | Elective | 77 | 62 | 63 | 31 | NR | NR | NR | NR |
| Vedin | 2003 | Sweden | 1999 to 2001 | First CABG | 59 | Elective | 76 | 64 | 56 | 16 | 1.0 | 1.0 | 37 | 69 |
| Velissaris | 2003 | United Kingdom | NR | Primary CABG | 54 | Elective | 80 | 62 | 44 | 0 | NR | NR | 32 | 62 |
| Straka | 2004 | Czech Republic | 2000 to 2002 | First and redo CABG | 400 | Elective and urgent | 81 | 66 | 57 | 28 | NR | NR | 28 | 51 |
| Wehlin | 2004 | Sweden | 2000 to 2001 | First CABG | 38 | Elective | 81 | 65 | NR | 16 | 1.0 | 1.1 | 32 | 58 |
| Wan | 2004 | Hong Kong | NR | CABG | 37 | Elective | 70 | 65 | 76 | 35 | <2.3 | <2.3 | NR | NR |
| Ascione | 2005 | United Kingdom | NR | First CABG | 20 | Elective | 85 | 62 | 75 | 0 | NR | NR | NR | NR |
| Celik | 2005 | Turkey | NR | First CABG | 60 | Elective | 52 | 67 | NR | 35 | 1.4 | 1.3 | NR | 127 |
| Kobayashi | 2005 | Japan | 2002 to 2004 | First CABG | 167 | Elective | 87 | 59 | 68 | 53 | <2.0 | <2.0 | 60 | 87 |
| Vedin | 2005 | Sweden | NR | First CABG | 31 | Elective | 77 | 66 | NR | 16 | 1.0 | 1.1 | 31 | 60 |
| Al-Ruzzeh | 2006 | United Kingdom | NR | Primary CABG | 168 | Elective | 84 | 63 | 59 | 23 | <2.0 | <2.0 | NR | NR |
| Niranjan | 2006 | United Kingdom | NR | First CABG | 80 | Elective | 83 | 67 | 70 | 14 | <2.3 | <2.3 | 58 | 94 |
| Tatoulis | 2006 | Australia | NR | CABG | 100 | Elective | 78 | 65 | 79 | 32 | NR | NR | NR | NR |
| Sajja | 2007 | India | 2004 to 2005 | Primary CABG + CKD | 120 | Elective | 89 | 60 | 72 | 56 | 1.4 | 1.5 | NR | NR |
| Fattouch | 2009 | Italy | 2002 to 2007 | Myocardial infarction with ST elevation | 128 | Urgent | 69 | 62 | 64 | 39 | NR | NR | NR | NR |
| Shroyer | 2009 | USA | 2002 to 2008 | First and redo CABG | 2203 | Elective and urgent | 99 | 62 | 86 | 44 | NR | NR | NR | NR |
| Møller | 2010 | Denmark | 2002 to 2008 | First and redo CABGb | 341 | Elective and urgent | 64 | 76 | 50 | 18 | NR | NR | 38 | 65 |
Summary data on age, serum creatinine, and aortic cross-clamp and CPB time are displayed as means unless indicated otherwise. Criteria obtained directly by e-mail from author. NR, not reported; CPB, cardiopulmonary bypass; CABG, coronary artery bypass grafting.
Total number of patients randomized.
Defined by the authors as “high-risk” patients.
Table 2.
Definitions of AKI in the RCTs included in the meta-analysis
| Author | Year | Definition of AKI |
|---|---|---|
| Vural | 1995 | Not defined (no renal complications in either group) |
| Ascione | 1999 | Need for hemofiltration |
| van Dijk | 2001 | Need for dialysis |
| Tang | 2002 | Persistent oliguria or anuria with a postoperative 2-fold increase in serum creatininea |
| Carrier | 2003 | Postoperative increase in serum creatinine by >100 μmol/L (1.1 mg/dl), or need for dialysis |
| Puskas | 2003 | Postoperative 1.5-fold increase in serum creatinine, or postoperative creatinine >2.0 mg/dl |
| Vedin | 2003 | Not defined (no acute renal failure during the hospital stay) |
| Velissaris | 2003 | Not defined (no end-organ failure) |
| Straka | 2004 | Need for hemodialysis |
| Wehlin | 2004 | Not defined (no acute renal failure observed during the hospital stay) |
| Wan | 2004 | Not defined (no postoperative acute renal failure) |
| Ascione | 2005 | Need for hemofiltrationa |
| Celik | 2005 | Need for hemodialysis |
| Kobayashi | 2005 | Need for hemodialysis |
| Vedin | 2005 | Not defined (no acute renal failure during the hospital stay) |
| Al-Ruzzeh | 2006 | Abnormal laboratory test results (not specified) or need for hemofiltration |
| Niranjan | 2006 | Postoperative serum creatinine >200 μmol/L (2.3 mg/dl) with or without need for hemofiltrationa |
| Tatoulis | 2006 | Postoperative 2-fold increase in serum creatinine, postoperative serum creatinine >2.0 mg/dl, or need for dialysis |
| Sajja | 2007 | Postoperative ≥1.2-fold increase in serum creatinine |
| Fattouch | 2009 | Oliguria (urine output <0.5 ml/kg) or anuria and postoperative increase in serum creatinine by more than 0.5 mg/dla |
| Shroyer | 2009 | Need for dialysis |
| Møller | 2010 | Postoperative 2-fold increase in serum creatinine, postoperative serum creatinine ≥200 μmol/L (2.3 mg/dl), or need for hemodialysis |
Criteria obtained by directly contacting the corresponding author.
Death was ascertained in-hospital in nine trials (25,27–29,32,34,46,48,51), at 30 days in nine trials (25,26,30,33,35,44,45,47,53), and at 60 days in one trial (42). The duration of follow-up was not documented in the three remaining studies (43,50,52).
Study Quality
The criteria used to assess study quality are listed in Appendix 1 with overall poor (arbitrarily defined as 0 to 1 on the Jadad scale) to fair (2,3) Jadad quality scores. Because no RCT was double-blinded because of the nature of the intervention, no study could be rated as good (4,5) by the Jadad quality score. In brief, randomization was adequate in 12 (26,28,30,32–35,45,47,51–53) of the 14 trials that documented the procedure (26,28–30,32–35,44,45,47,51–53), but there were attrition and crossover rates as high as 13% and 11%, respectively. Only three studies reported on allocation concealment (29,30,35). Among the 15 trials that provided optimal documentation of their analysis (25,26,28,33,34,43–49,51–53), 11 used an intent-to-treat analysis (25,26,28,33,34,43,45,47,49,51,53).
Data Synthesis and Analysis
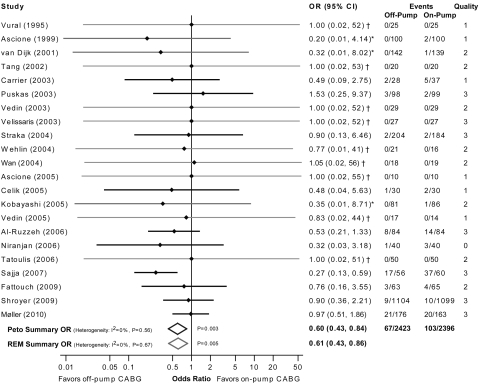
Effect of Off-Pump CABG on AKI
All 22 RCTs, with a total of 4819 analyzable patients (Figure 2), reported AKI rates. The overall weighted incidence of AKI in the on-pump CABG group was 4.0% (95% confidence interval [CI] 1.8%, 8.5%; range 0%, 62%). By meta-analysis, off-pump CABG was associated with a 40% lower odds of postoperative AKI (OR 0.60; 95% CI 0.43, 0.84; P = 0.003). However, nine studies had no patients with AKI in either group and thus did not contribute to the meta-analysis. Although the trials differed considerably in their size and quality score, the test for heterogeneity of effects was not significant (I2 = 0%; P = 0.56).
Figure 2.
Forest plot of off-pump versus on-pump CABG on the incidence of AKI. Peto fixed-effect model and DerSimonian & Laird random-effects model (REM) estimate of OR. Dark gray lines correspond to studies with zero events in one arm whereas light gray lines correspond to studies with zero events in both arms. The quality score is based on the Jadad scale, ranging from 0 to 5. *No events in one group: The displayed estimate and CI were calculated by adjusting the numbers of events and nonevents. †Study omitted from meta-analyses because there were no events in both groups: The displayed estimate and CI were calculated by adjusting the numbers of events and nonevents.
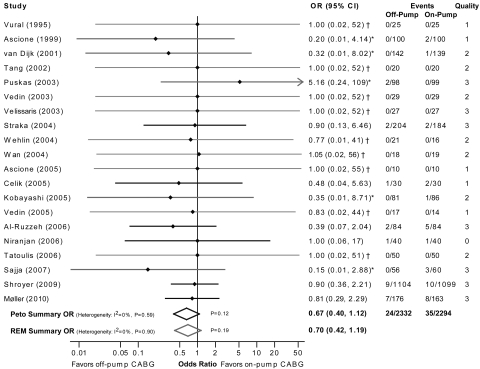
Effect of Off-Pump CABG on Dialysis Requirement
The analysis included 20 RCTs, with a total of 4626 analyzable patients (Figure 3). However, nine studies had no patients who required dialysis in either group and thus did not contribute to the meta-analysis. The overall weighted incidence of dialysis requirement in the on-pump CABG group was 2.4% (95% CI 1.6%, 3.7%; range 0%, 7%). By meta-analysis, off-pump CABG was associated with a nonstatistically significant 33% lower odds of dialysis requirement (OR 0.67; 95% CI 0.40, 1.12; P = 0.12).
Figure 3.
Forest plot displaying the effect of off-pump versus on-pump CABG on dialysis requirement. Peto fixed-effect model and DerSimonian & Laird random-effects model (REM) estimate of OR. Dark gray lines correspond to studies with zero events in one arm whereas light gray lines correspond to studies with zero events in both arms. The quality score is based on the Jadad scale, ranging from 0 to 5. *No events in one group: The displayed estimate and CI were calculated by adjusting the numbers of events and nonevents. †Study omitted from meta-analyses because there were no events in both groups: The displayed estimate and CI were calculated by adjusting the numbers of events and nonevents.
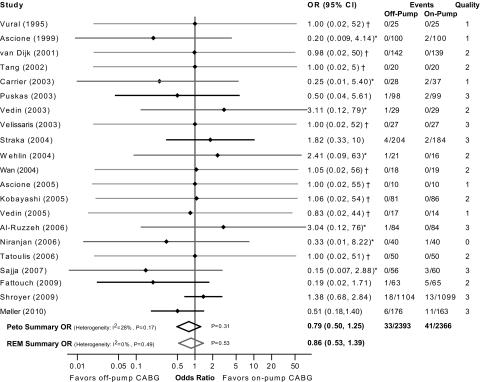
Effect of Off-Pump CABG on Mortality
This analysis was restricted to the 21 RCTs that reported both AKI and mortality results. They included a total of 4759 analyzable patients (Figure 4). However, nine studies had no deaths in either group and thus did not contribute to the meta-analysis. The overall weighted mortality rate in the on-pump CABG group was 2.6% (95% CI, 1.6%, 4.0%; range 0%, 8%). By meta-analysis, off-pump CABG was not associated with a significant reduction in mortality compared with on-pump CABG (OR 0.79; 95% CI 0.50, 1.25; P = 0.31).
Figure 4.
Forest plot displaying the effect of off-pump versus on-pump CABG on mortality. Peto fixed-effect model and DerSimonian & Laird random-effects model (REM) estimate of OR. Dark gray lines correspond to studies with zero events in one arm whereas light gray lines correspond to studies with zero events in both arms. The quality score is based on the Jadad scale, ranging from 0 to 5. *No events in one group: The displayed estimate and CI were calculated by adjusting the numbers of events and nonevents. †Study omitted from meta-analyses because there were no events in both groups: The displayed estimate and CI were calculated by adjusting the numbers of events and nonevents.
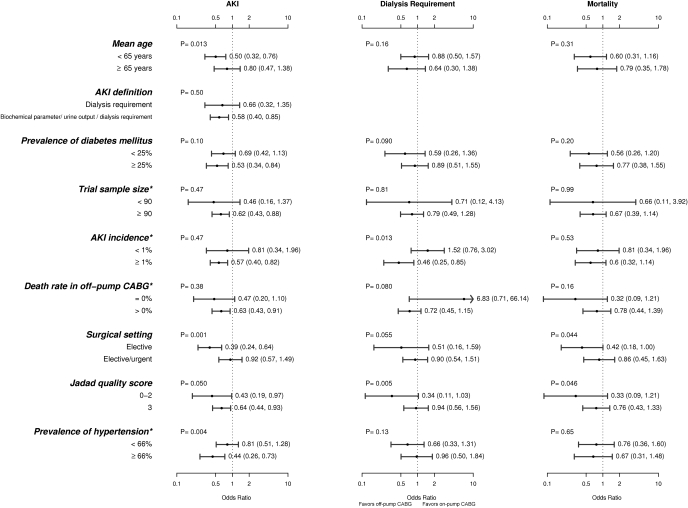
Subgroup and Sensitivity Analyses
Despite the absence of significant heterogeneity among the trials, to explore the robustness of our findings in the Peto fixed-effects model, we repeated the meta-analyses using random-effects models and performed several subgroup analyses. As shown in Figures 2 through 4, the random-effects models displayed similar effect estimates. The subgroup analyses are displayed in Figure 5. In brief, pooled point estimates for AKI in the off-pump CABG group had larger effects among studies that had a lower mean age (<65 versus ≥65 years), were restricted to elective CABG surgery, had a lower Jadad quality score (0 to 1 versus 2 to 3), and had a higher prevalence of hypertension (≥66% versus <66%). Subgroup analyses among studies that used a more liberal definition of AKI (entailing a mixture of biochemical parameter/urine output/dialysis requirement) did not greatly influence the pooled point estimates as compared with studies where the definition of AKI was restricted to dialysis requirement. For the outcome of dialysis requirement, studies with a higher incidence of AKI and studies with lower Jadad quality scores were associated with larger effects. For the outcome of death, studies restricted to elective setting and those with lower Jadad quality scores were associated with a larger effect favoring off-pump CABG. All but three studies that reported preoperative serum creatinine had no outcome events, precluding a meaningful subgroup analysis based on this variable.
Figure 5.
Subgroup analyses displaying the effect of off-pump versus on-pump CABG on the incidence of AKI, dialysis requirement, and mortality. Peto fixed-effect model estimate of OR. The P value refers to the difference among subgroups using the t test. *Where indicated, the subgroups represent trials with variables of interest that are above or below the median value.
Summary OR estimates were not affected when the largest trial (33) was excluded from the analysis for AKI (OR 0.60; 95% CI 0.43, 0.84 versus OR 0.56; 95% CI 0.39, 0.81) and dialysis requirement (OR 0.67; 95% CI 0.40, 1.12 versus OR 0.58; 95% CI 0.31, 1.08). Notably, however, when a relatively small trial with the highest reported incidence of AKI was excluded from the analysis for the outcome of AKI (52) the statistical significance was lost (OR 0.73; 95% CI 0.50, 1.07), although the point estimate remained similar to the overall analysis. This relatively small study had a 62% incidence of AKI in the on-pump CABG group. Although this study's large effects size might seem improbable as compared with the ones observed in larger studies such as the Randomized On/Off Bypass (ROOBY) trial, this might be due in part to a very sensitive definition of AKI used by the authors and to the inclusion criteria that were restricted to patients with pre-existing renal dysfunction. This trial also had the third highest rate of dialysis requirement in the on-pump CABG group (5%) among all studies.
Funnel plots were slightly asymmetric on visual inspection for all three measured outcomes, possibly suggesting unpublished studies favoring on-pump CABG (data not shown).
Discussion
The present meta-analysis suggests that off-pump CABG performed in a relatively heterogeneous patient population with coronary artery disease is associated with a reduction in the incidence of AKI but has no effect on dialysis requirement or all-cause mortality. Meta-analyses of the published literature are commonly used to assess treatment effect by allowing similar trials to be combined quantitatively, thereby increasing the precision of treatment effect estimates. In the past decade, six meta-analyses were published, five comparing the effect of off-pump versus on-pump CABG on major adverse outcomes including development of AKI (19–21,23,24), and one was specifically designed to evaluate kidney end points (22). A summary of these six meta-analyses is provided in Table 3. In brief, these authors used a small number of RCTs and included observational studies in their meta-analysis.
Table 3.
Comparison of the results of the present meta-analysis with previously published reports
| Author | Year | Number of Studies with Kidney End Points | Studies Included |
Conclusion |
||
|---|---|---|---|---|---|---|
| RCTs | Cohort Studies | AKI | Dialysis Requirement | |||
| Reston | 2003 | 17 | 1 | 16 | Beneficial effect | NR |
| Cheng | 2005 | 10 | 10 | 0 | No statistically significant difference | NR |
| Wijeysundera | 2005 | 13 | 5 | 8 | No statistically significant difference (RCTs), beneficial effect (cohort studies) | NR |
| Sedrakyan | 2006 | 10 | 10 | 0 | No statistically significant difference | NR |
| Nigwekar | 2009 | 22 | 6 | 16 | Beneficial effect | No statistically significant difference |
| Kuss | 2010 | 17 | 0 | 17 | Beneficial effect | NR |
| Seabra | 2010 | 22 | 22 | 0 | Beneficial effect | No statistically significant difference |
NR, not reported.
The recently published large multicenter ROOBY trial assigned 2203 patients scheduled for urgent or elective CABG to on-pump or off-pump procedures (33). This study alone had more patients than any of the five previously published meta-analyses when considering only RCTs. The ROOBY trial showed no statistically significant benefit of off-pump CABG on kidney end points; moreover, at 1 year of follow-up, the off-pump group had worse composite outcomes of all-cause mortality, repeat revascularization, or nonfatal myocardial infarction than did the on-pump group (33).
Our updated meta-analysis of RCTs showed a statistically significant benefit of off-pump versus on-pump CABG with respect to AKI when a liberal definition was used (consisting of a mixture of biochemical parameters/urine output/dialysis requirement criteria), but no significant benefit with respect to dialysis requirement or mortality.
Our data synthesis has several strengths. The robust nature of our global findings is supported by a nonsignificant statistical heterogeneity test and by the fact that the lower OR for AKI in the off-pump CABG group persisted in almost every subgroup analysis. Moreover, our results are in agreement with those observed in the largest trial published to date (33).
However, there are several important limitations to consider. We were unable to identify unpublished reports, which might have biased our results toward the off-pump benefit. In fact, funnel plots showed visual asymmetry, which might denote publication bias but might also be secondary to other causes (54). Another shortcoming is the use of different definitions of AKI with most trials defining AKI as the need for dialysis or a mixture of a biochemical/urine output parameter or dialysis requirement. We can only speculate as to whether the inclusion of less severe forms of AKI, or defining AKI purely on the basis of serum creatinine or urine output fluctuations, would have yielded different results. Also, the small sample size of most of the studies resulting in low to zero event rates is a major limitation of the evidence. We were also unable to perform a subgroup analysis by baseline kidney function because the studies included in this meta-analysis provided insufficient data on pre-existing kidney disease to perform such analysis.
Finally, the lower odds of AKI observed in our analysis did not translate into lower odds of death. Ascertaining only death in trials that provided kidney outcomes (the primary objective of our meta-analysis) might have influenced the assessment of this secondary end point, although there is no obvious reason why relative mortality rates would differ in studies that reported AKI outcomes and those that did not.
Four ongoing large multicenter RCTs comparing the effect of off-pump versus on-pump CABG on clinical outcomes are expected to enroll a total of 7800 patients and to conclude within the next 5 years (55–58). However, only two of the four trials list AKI as a primary outcome as a single or composite end point (57,58).
In conclusion, in the present meta-analysis, off-pump CABG appears to reduce the risk of AKI compared with on-pump surgery. These findings are hampered by the variable AKI definitions used in individual trials, precluding definitive conclusions. A subgroup analysis restricted to dialysis requirement, a well accepted and very serious complication of cardiac surgery, was not influenced by the surgical technique. The selection of surgical candidates deemed at low risk for developing postoperative AKI might explain in part why the off-pump CABG technique had no added protection in some studies. Therefore, a large multicenter RCT recruiting surgical candidates with preoperative high-risk of renal dysfunction (i.e., those with chronic kidney disease or resolving contrast-induced nephropathy) is warranted to validate the potential advantage of off-pump over on-pump CABG in this population. Such a trial should be primarily powered to ascertain AKI as a primary end point using a composite of major kidney end points such as the doubling of serum creatinine or dialysis requirement.
Disclosures
None.
Supplementary Material
Acknowledgments
This work was made possible in part by an International Society of Nephrology Commission for the Global Advancement of Nephrology (COMGAN) Fellowship awarded to Dr. Seabra. Dr. Jaber is funded in part by a grant from the National Institutes of Health (DK077751). Part of this material was presented at the annual meeting of the American Society of Nephrology; October 27 through November 1, 2009; San Diego, CA.
Appendix
Appendix 1.
Quality assessment of the randomized controlled trials included in the meta-analysis
| Author | Year | Randomization | Double blinding | Attrition (%) | Allocation concealment | Cross-over (%) | Intent-to-treat analysis | Jadad score |
|---|---|---|---|---|---|---|---|---|
| Vural | 1995 | NR | No | NR | NR | NR | NR | 1 |
| Ascione | 1999 | NR | No | NR | NR | 1.0 | Yes | 1 |
| van Dijk | 2001 | Adequate | No | NR | NR | 5.3 | Yes | 2 |
| Tang | 2002 | NR | No | 12.5 | NR | 0 | Yes | 2 |
| Carrier | 2003 | Unclear | No | NR | NR | 9.2 | No | 1 |
| Puskas | 2003 | Adequate | No | 1.5 | NR | 2.0 | Yes | 3 |
| Vedin | 2003 | NR | No | 0 | NR | 0 | No | 2 |
| Velissaris | 2003 | Adequate | No | 0 | NR | 0 | Yes | 3 |
| Straka | 2004 | Adequate | No | 3.0 | NR | 10.8 | Yes | 3 |
| Wehlin | 2004 | NR | No | 2.6 | NR | 0 | No | 2 |
| Wan | 2004 | Adequate | No | NR | Yes | NR | NR | 2 |
| Ascione | 2005 | NR | No | NR | NR | 0 | Yes | 1 |
| Celik | 2005 | NR | No | NR | NR | NR | NR | 1 |
| Kobayashi | 2005 | Adequate | No | NR | NR | 0.6 | Yes | 2 |
| Vedin | 2005 | NR | No | NR | NR | NR | NR | 1 |
| Al-Ruzzeh | 2006 | Adequate | No | 0 | NR | 0 | Yes | 3 |
| Niranjan | 2006 | Sub-optimal | No | NR | Yes | NR | NR | 0 |
| Tatoulis | 2006 | Adequate | No | NR | Yes | NR | NR | 2 |
| Sajja | 2007 | Adequate | No | 3.3 | NR | 0 | No | 3 |
| Fattouch | 2009 | Adequate | No | NR | NR | 0.8 | NR | 2 |
| Shroyer | 2009 | Adequate | No | 0 | NR | 8.0 | Yes | 3 |
| Møller | 2010 | Adequate | No | 0.6 | NR | 4.1 | Yes | 3 |
NR, not reported.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Goetz RH, Rohman M, Haller JD, Dee R, Rosenak SS: Internal mammary-coronary artery anastomosis. A nonsuture method employing tantalum rings. J Thorac Cardiovasc Surg 41: 378–386, 1961 [PubMed] [Google Scholar]
- 2.Kolessov VI: Mammary artery-coronary artery anastomosis as method of treatment for angina pectoris. J Thorac Cardiovasc Surg 54: 535–544, 1967 [PubMed] [Google Scholar]
- 3.Favaloro RG: Saphenous vein autograft replacement of severe segmental coronary artery occlusion: Operative technique. Ann Thorac Surg 5: 334–339, 1968 [DOI] [PubMed] [Google Scholar]
- 4.Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Stahle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW: Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 360: 961–972, 2009 [DOI] [PubMed] [Google Scholar]
- 5.Hlatky MA, Boothroyd DB, Bravata DM, Boersma E, Booth J, Brooks MM, Carrie D, Clayton TC, Danchin N, Flather M, Hamm CW, Hueb WA, Kahler J, Kelsey SF, King SB, Kosinski AS, Lopes N, McDonald KM, Rodriguez A, Serruys P, Sigwart U, Stables RH, Owens DK, Pocock SJ: Coronary artery bypass surgery compared with percutaneous coronary interventions for multivessel disease: A collaborative analysis of individual patient data from ten randomised trials. Lancet 373: 1190–1197, 2009 [DOI] [PubMed] [Google Scholar]
- 6.Benetti FJ, Naselli G, Wood M, Geffner L: Direct myocardial revascularization without extracorporeal circulation. Experience in 700 patients. Chest 100: 312–316, 1991 [DOI] [PubMed] [Google Scholar]
- 7.Cleveland JC, Jr, Shroyer AL, Chen AY, Peterson E, Grover FL: Off-pump coronary artery bypass grafting decreases risk-adjusted mortality and morbidity. Ann Thorac Surg 72: 1282–1288, 2001, discussion 1288–1289 [DOI] [PubMed] [Google Scholar]
- 8.Edmunds LH, Jr: Inflammatory response to cardiopulmonary bypass. Ann Thorac Surg 66: S12–S16, 1998, discussion S18–S25 [DOI] [PubMed] [Google Scholar]
- 9.Taylor KM: Brain damage during cardiopulmonary bypass. Ann Thorac Surg 65: S20–S26, 1998, discussion S27–28 [DOI] [PubMed] [Google Scholar]
- 10.Royster RL: Myocardial dysfunction following cardiopulmonary bypass: recovery patterns, predictors of inotropic need, theoretical concepts of inotropic administration. J Cardiothorac Vasc Anesth 7: 19–25, 1993 [DOI] [PubMed] [Google Scholar]
- 11.Cislaghi F, Condemi AM, Corona A: Predictors of prolonged mechanical ventilation in a cohort of 5123 cardiac surgical patients. Eur J Anaesthesiol 26: 396–403, 2009 [DOI] [PubMed] [Google Scholar]
- 12.Lassnigg A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, Hiesmayr M: Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: A prospective cohort study. J Am Soc Nephrol 15: 1597–1605, 2004 [DOI] [PubMed] [Google Scholar]
- 13.Liangos O, Tighiouart H, Perianayagam MC, Kolyada A, Han WK, Wald R, Bonventre JV, Jaber BL: Comparative analysis of urinary biomarkers for early detection of acute kidney injury following cardiopulmonary bypass. Biomarkers 14: 423–431, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chertow GM, Levy EM, Hammermeister KE, Grover F, Daley J: Independent association between acute renal failure and mortality following cardiac surgery. Am J Med 104: 343–348, 1998 [DOI] [PubMed] [Google Scholar]
- 15.Hannan EL, Wu C, Smith CR, Higgins RS, Carlson RE, Culliford AT, Gold JP, Jones RH: Off-pump versus on-pump coronary artery bypass graft surgery: Differences in short-term outcomes and in long-term mortality and need for subsequent revascularization. Circulation 116: 1145–1152, 2007 [DOI] [PubMed] [Google Scholar]
- 16.Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW: Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol 16: 3365–3370, 2005 [DOI] [PubMed] [Google Scholar]
- 17.Liangos O, Wald R, O'Bell JW, Price L, Pereira BJ, Jaber BL: Epidemiology and outcomes of acute renal failure in hospitalized patients: A national survey. Clin J Am Soc Nephrol 1: 43–51, 2006 [DOI] [PubMed] [Google Scholar]
- 18.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M, Meigs J, Mozaffarian D, Nichol G, O'Donnell C, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Steinberger J, Thom T, Wasserthiel-Smoller S, Wong N, Wylie-Rosett J, Hong Y: Heart disease and stroke statistics—2009 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 119: e21–e181, 2009 [DOI] [PubMed] [Google Scholar]
- 19.Cheng DC, Bainbridge D, Martin JE, Novick RJ: Does off-pump coronary artery bypass reduce mortality, morbidity, and resource utilization when compared with conventional coronary artery bypass? A meta-analysis of randomized trials. Anesthesiology 102: 188–203, 2005 [DOI] [PubMed] [Google Scholar]
- 20.Sedrakyan A, Wu AW, Parashar A, Bass EB, Treasure T: Off-pump surgery is associated with reduced occurrence of stroke and other morbidity as compared with traditional coronary artery bypass grafting: A meta-analysis of systematically reviewed trials. Stroke 37: 2759–2769, 2006 [DOI] [PubMed] [Google Scholar]
- 21.Reston JT, Tregear SJ, Turkelson CM: Meta-analysis of short-term and mid-term outcomes following off-pump coronary artery bypass grafting. Ann Thorac Surg 76: 1510–1515, 2003 [DOI] [PubMed] [Google Scholar]
- 22.Nigwekar SU, Kandula P, Hix JK, Thakar CV: Off-pump coronary artery bypass surgery and acute kidney injury: A meta-analysis of randomized and observational studies. Am J Kidney Dis 54: 413–423, 2009 [DOI] [PubMed] [Google Scholar]
- 23.Wijeysundera DN, Beattie WS, Djaiani G, Rao V, Borger MA, Karkouti K, Cusimano RJ: Off-pump coronary artery surgery for reducing mortality and morbidity: Meta-analysis of randomized and observational studies. J Am Coll Cardiol 46: 872–882, 2005 [DOI] [PubMed] [Google Scholar]
- 24.Kuss O, von Salviati B, Borgermann J: Off-pump versus on-pump coronary artery bypass grafting: A systematic review and meta-analysis of propensity score analyses. J Thorac Cardiovasc Surg, 2010, in press [DOI] [PubMed] [Google Scholar]
- 25.Ascione R, Lloyd CT, Underwood MJ, Lotto AA, Pitsis AA, Angelini GD: Economic outcome of off-pump coronary artery bypass surgery: A prospective randomized study. Ann Thorac Surg 68: 2237–2242, 1999 [DOI] [PubMed] [Google Scholar]
- 26.van Dijk D, Nierich AP, Jansen EW, Nathoe HM, Suyker WJ, Diephuis JC, van Boven WJ, Borst C, Buskens E, Grobbee DE, Robles De Medina EO, de Jaegere PP.Octopus Study G: Early outcome after off-pump versus on-pump coronary bypass surgery: Results from a randomized study. Circulation 104: 1761–1766, 2001 [DOI] [PubMed] [Google Scholar]
- 27.Vedin J, Antovic A, Ericsson A, Vaage J: Hemostasis in off-pump compared to on-pump coronary artery bypass grafting: A prospective, randomized study. Ann Thorac Surg 80: 586–593, 2005 [DOI] [PubMed] [Google Scholar]
- 28.Al-Ruzzeh S, George S, Bustami M, Wray J, Ilsley C, Athanasiou T, Amrani M: Effect of off-pump coronary artery bypass surgery on clinical, angiographic, neurocognitive, and quality of life outcomes: Randomised controlled trial. BMJ 332: 1365, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Niranjan G, Asimakopoulos G, Karagounis A, Cockerill G, Thompson M, Chandrasekaran V: Effects of cell saver autologous blood transfusion on blood loss and homologous blood transfusion requirements in patients undergoing cardiac surgery on- versus off-cardiopulmonary bypass: A randomised trial. Eur J Cardiothorac Surg 30: 271–277, 2006 [DOI] [PubMed] [Google Scholar]
- 30.Tatoulis J, Rice S, Davis P, Goldblatt JC, Marasco S: Patterns of postoperative systemic vascular resistance in a randomized trial of conventional on-pump versus off-pump coronary artery bypass graft surgery. Ann Thorac Surg 82: 1436–1444, 2006 [DOI] [PubMed] [Google Scholar]
- 31.Puskas JD, Kilgo PD, Kutner M, Pusca SV, Lattouf O, Guyton RA: Off-pump techniques disproportionately benefit women and narrow the gender disparity in outcomes after coronary artery bypass surgery. Circulation 116: I192–I199, 2007 [DOI] [PubMed] [Google Scholar]
- 32.Fattouch K, Guccione F, Dioguardi P, Sampognaro R, Corrado E, Caruso M, Ruvolo G: Off-pump versus on-pump myocardial revascularization in patients with ST-segment elevation myocardial infarction: A randomized trial. J Thorac Cardiovasc Surg 137: 650–656, 2009, discussion 656–657 [DOI] [PubMed] [Google Scholar]
- 33.Shroyer AL, Grover FL, Hattler B, Collins JF, McDonald GO, Kozora E, Lucke JC, Baltz JH, Novitzky D: On-Pump versus off-pump coronary-artery bypass surgery. N Engl J Med 361: 1827–1837, 2009 [DOI] [PubMed] [Google Scholar]
- 34.Velissaris T, Tang A, Murray M, El-Minshawy A, Hett D, Ohri S: A prospective randomized study to evaluate splanchnic hypoxia during beating-heart and conventional coronary revascularization. Eur J Cardiothorac Surg 23: 917–924, 2003, discussion 924 [DOI] [PubMed] [Google Scholar]
- 35.Wan IY, Arifi AA, Wan S, Yip JH, Sihoe AD, Thung KH, Wong EM, Yim AP: Beating heart revascularization with or without cardiopulmonary bypass: Evaluation of inflammatory response in a prospective randomized study. J Thorac Cardiovasc Surg 127: 1624–1631, 2004 [DOI] [PubMed] [Google Scholar]
- 36.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ: Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials 17: 1–12, 1996 [DOI] [PubMed] [Google Scholar]
- 37.Yusuf S, Peto R, Lewis J, Collins R, Sleight P: Beta blockade during and after myocardial infarction: An overview of the randomized trials. Prog Cardiovasc Dis 27: 335–371, 1985 [DOI] [PubMed] [Google Scholar]
- 38.Rucker G, Schwarzer G, Carpenter J, Olkin I: Why add anything to nothing? The arcsine difference as a measure of treatment effect in meta-analysis with zero cells. Stat Med 28: 721–738, 2009 [DOI] [PubMed] [Google Scholar]
- 39.DerSimonian R, Laird N: Meta-analysis in clinical trials. Control Clin Trials 7: 177–188, 1986 [DOI] [PubMed] [Google Scholar]
- 40.Wallace BC, Schmid CH, Lau J, Trikalinos TA: Meta-Analyst: Software for meta-analysis of binary, continuous and diagnostic data. BMC Med Res Methodol 9: 80, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ross JH, Michael JB, Jonathan JD, Roger MH, Douglas GA, Jonathan ACS: Metan: Fixed- and random-effects meta-analysis. Stata Journal 8: 28, 2008 [Google Scholar]
- 42.Vural KM, Tasdemir O, Karagoz H, Emir M, Tarcan O, Bayazit K: Comparison of the early results of coronary artery bypass grafting with and without extracorporeal circulation. Thorac Cardiovasc Surg 43: 320–325, 1995 [DOI] [PubMed] [Google Scholar]
- 43.Tang AT, Knott J, Nanson J, Hsu J, Haw MP, Ohri SK: A prospective randomized study to evaluate the renoprotective action of beating heart coronary surgery in low risk patients. Eur J Cardiothorac Surg 22: 118–123, 2002 [DOI] [PubMed] [Google Scholar]
- 44.Carrier M, Perrault LP, Jeanmart H, Martineau R, Cartier R, Page P: Randomized trial comparing off-pump to on-pump coronary artery bypass grafting in high-risk patients. Heart Surg Forum 6: E89–E92, 2003 [PubMed] [Google Scholar]
- 45.Puskas JD, Williams WH, Duke PG, Staples JR, Glas KE, Marshall JJ, Leimbach M, Huber P, Garas S, Sammons BH, McCall SA, Petersen RJ, Bailey DE, Chu H, Mahoney EM, Weintraub WS, Guyton RA: Off-pump coronary artery bypass grafting provides complete revascularization with reduced myocardial injury, transfusion requirements, and length of stay: A prospective randomized comparison of two hundred unselected patients undergoing off-pump versus conventional coronary artery bypass grafting. J Thorac Cardiovasc Surg 125: 797–808, 2003 [DOI] [PubMed] [Google Scholar]
- 46.Vedin J, Jensen U, Ericsson A, Bitkover C, Samuelsson S, Bredin F, Vaage J: Cardiovascular function during the first 24 hours after off pump coronary artery bypass grafting—A prospective, randomized study. Interact Cardiovasc Thorac Surg 2: 489–494, 2003 [DOI] [PubMed] [Google Scholar]
- 47.Straka Z, Widimsky P, Jirasek K, Stros P, Votava J, Vanek T, Brucek P, Kolesar M, Spacek R: Off-pump versus on-pump coronary surgery: Final results from a prospective randomized study PRAGUE-4. Ann Thorac Surg 77: 789–793, 2004 [DOI] [PubMed] [Google Scholar]
- 48.Wehlin L, Vedin J, Vaage J, Lundahl J: Activation of complement and leukocyte receptors during on- and off pump coronary artery bypass surgery. Eur J Cardiothorac Surg 25: 35–42, 2004 [DOI] [PubMed] [Google Scholar]
- 49.Ascione R, Ghosh A, Reeves BC, Arnold J, Potts M, Shah A, Angelini GD: Retinal and cerebral microembolization during coronary artery bypass surgery: A randomized, controlled trial. Circulation 112: 3833–3838, 2005 [DOI] [PubMed] [Google Scholar]
- 50.Celik JB, Gormus N, Topal A, Okesli S, Solak H: Effect of off-pump and on-pump coronary artery bypass grafting on renal function. Ren Fail 27: 183–188, 2005 [PubMed] [Google Scholar]
- 51.Kobayashi J, Tashiro T, Ochi M, Yaku H, Watanabe G, Satoh T, Tagusari O, Nakajima H, Kitamura S; Japanese Off-Pump Coronary Revascularization Investigation Study Group: Early outcome of a randomized comparison of off-pump and on-pump multiple arterial coronary revascularization. Circulation 112: I338–I343, 2005 [DOI] [PubMed] [Google Scholar]
- 52.Sajja LR, Mannam G, Chakravarthi RM, Sompalli S, Naidu SK, Somaraju B, Penumatsa RR: Coronary artery bypass grafting with or without cardiopulmonary bypass in patients with preoperative non-dialysis dependent renal insufficiency: A randomized study. J Thorac Cardiovasc Surg 133: 378–388, 2007 [DOI] [PubMed] [Google Scholar]
- 53.Moller CH, Perko MJ, Lund JT, Andersen LW, Kelbaek H, Madsen JK, Winkel P, Gluud C, Steinbruchel DA: No major differences in 30-day outcomes in high-risk patients randomized to off-pump versus on-pump coronary bypass surgery: The best bypass surgery trial. Circulation 121: 498–504, 2010 [DOI] [PubMed] [Google Scholar]
- 54.Lau J, Ioannidis JP, Terrin N, Schmid CH, Olkin I: The case of the misleading funnel plot. BMJ 333: 597–600, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Puskas JD. SMART trial longitudinal follow-up: Off-pump versus on-pump coronary artery bypass surgery. Available at: http://www.clinicaltrials.gov/ct2/show/NCT00209053 Accessed June 10, 2010
- 56.Houlind KC, Mortensen PE: The Danish on-pump, off-pump randomization study (DOORS). Available at: http://www.clinicaltrials.gov/ct2/show/NCT00123981 Accessed June 10, 2010
- 57.Andre L, Yusuf S, Taggart D: Coronary artery bypass surgery (CABG) Off or On Pump Revascularization Study (CORONARY). Available at: http://www.clinicaltrials.gov/ct2/show/NCT00463294 Accessed June 10, 2010
- 58.Diegeler A, Hilker M: German Off Pump Coronary Artery Bypass in Elderly Study (GOPCABE). Available at: http://www.clinicaltrials.gov/ct2/show/NCT00719667 Accessed June 10, 2010
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.