Abstract
Background and objectives: Cardiac failure is directly affected by left ventricular (LV) dysfunction, and particularly LV systolic dysfunction is strongly associated with survival in ESRD patients. The aim of this study was to determine the prognostic value of reduced LV ejection fraction (LVEF) measured at the time of initiation of hemodialysis (HD) in incident HD patients.
Design, setting, participants, & measurements: 1254 consecutive ESRD patients who electively started HD therapy were screened by echocardiography within 1 month after its inception. They were divided into five groups according to LVEF levels with a decrease of 0.1 each and were followed up for up to 7 years. Survival was examined with the Kaplan-Meier method and compared using the log-rank test.
Results: Among the 1254 patients, LVEF levels ≥0.6, 0.5 to 0.6, 0.4 to 0.5, 0.3 to 0.4, and <0.3 were seen in 842 (67.1%), 247 (19.7%), 107 (8.5%), 41 (3.3%), and 17 (1.4%) patients, respectively. On Kaplan-Meier analysis, 7-year event-free rates from cardiovascular death were 84.2, 83.7, 73.6, 59.4, and 30.9% in order of groups with decreasing LVEF of 0.1 each, respectively. Seven-year event-free rates from all-cause death were 69.2, 61.7, 57.1, 45.9, and 23.1% in the respective groups. Even after adjustment for other risk factors, decreasing LVEF was a strong independent predictor for cardiovascular death.
Conclusions: Reduced LVEF on starting HD therapy could stratify risk of cardiovascular and all-cause mortality in ESRD patients. Screening by echocardiography at start of HD therapy might be recommended to predict prognosis in patients with ESRD.
Cardiovascular disease is a major complication in patients on maintenance hemodialysis (HD) and accounts for one half of the causes of their deaths (1–5). Moreover, in this population, cardiac dysfunction is common (6) and is related to a higher incidence of mortality and hospitalization (7). Left ventricular (LV) dysfunction directly affects cardiac failure, particularly, and is strongly associated with a poor survival in patients with ESRD with constant body-fluid overload status (8).
Routine assessment of LV ejection fraction (EF) has been recommended in patients with heart failure (9). Curtis and co-workers showed that lower LVEF was associated with a linear increase in mortality in nearly 8000 non-HD patients with stable heart failure (10). Analysis of patients on maintenance HD by ultrasonic-echocardiography (UCG) has been recommended for risk stratification (11). Zoccali et al. revealed an association between reduced LVEF and increased adverse events in 254 asymptomatic HD patients in their cohort study (12). However, the association between LV systolic dysfunction at the beginning of HD therapy and the prognosis remains unclear in such patients. We hypothesized that LVEF might predict their prognosis after initiating HD therapy. Thus, we assessed the potential prognostic value of reduced LVEF detected by UCG at the beginning of HD therapy in ESRD patients in this study.
Materials and Methods
Study Population
This study consisted of 1254 consecutive ESRD patients who began HD therapy between November 2000 and August 2007. UCG was prospectively performed on a nondialysis day within 1 month after beginning HD therapy. The patients were followed up for up to 7 years.
Blood data were analyzed from fasting blood samples obtained between 7:00 and 8:00 a.m. on the next day of HD when UCG was performed. The primary endpoint was cardiovascular death caused by heart failure, myocardial infarction, arrhythmia, sudden death, and other cardiac deaths. The secondary endpoint was all-cause death. Data for endpoints were obtained from hospital charts and through telephone interviews with patients conducted by trained reviewers blinded to the UCG analysis. In this study, cases of unwitnessed death were counted as sudden deaths. Diabetes was defined as a history or presence of diabetes and/or a fasting plasma glucose concentration >126 mg/dl and/or having a fasting plasma glucose concentration >126 mg/dl or a glycosylated hemoglobin (HbA1c) concentration >6.5%. Hypertension was defined as having systolic BP >160 mmHg and/or diastolic BP >90 mmHg or undergoing antihypertensive treatment. Dyslipidemia was defined as having total cholesterol levels >220 mg/dl or taking lipid-lowering therapy. Smoking habit was defined as currently smoking or having discontinued cigarette use within 6 months before starting HD.
The study protocol conformed to the guidelines of the ethics committee of our institution and was conducted in accordance with the Declaration of Helsinki. The physicians obtained written informed consent from each patient.
Echocardiography
According to the recommendations of the American Society of Echocardiography, UCG was performed on a nondialysis day. UCG recordings were evaluated by two expert physicians blinded to other clinical information. LVEF was measured using modified Sympson method (13). The measurements from two technicians were averaged. Patients were divided into five groups according to their LVEF levels: patients with LVEF ≥0.6, 0.5 to 0.6, 0.4 to 0.5, 0.3 to 0.4, and <0.3, respectively. LVEF <0.5 was considered as LV systolic dysfunction (14,15).
The intraobserver variabilities of LVEF in UCG were well correlated (r = 0.939, P < 0.001). The mean difference was 0.002 ± 0.04.
Statistical Analyses
SPSS was used for statistical analyses. All values are expressed as mean ± SD or incidences (%). Differences among the groups were evaluated by unpaired t test for continuous variables and by χ2 test for categorical variables. Differences in event-free survival among the groups were examined with Kaplan-Meier method and compared using a log-rank test.
Hazard ratios (HR) and 95% confidence intervals (CIs) were calculated for each factor by a Cox univariate analysis. Covariates including established risk factors (age, gender, body mass index [BMI], diabetes, hypertension, dyslipidemia, smoking status, serum albumin levels, serum C-reactive protein [CRP] levels, and LV mass index) and LVEF were assessed by Cox multivariable regression analysis to determine significant predictors for the endpoint. In addition, estimates of the Harrell C index of the Cox models and its 95% CIs were calculated in a baseline model with established risk factors and a second enriched model containing the baseline established risk factors plus LVEF (16,17). In addition, likelihood-ratio tests were performed to evaluate whether the model with established risk factors improved after the addition of LVEF, as Harrell described (18). A value of P < 0.05 was considered statistically significant.
Results
The median duration of follow-up was 4.2 years (SD 2.4). Among 1254 enrolled patients, 828 (66.0%) were males. The mean age was 62 ± 14 years. Diabetes was seen in 564 patients (45.0%). The mean BMI was 21.0 ± 3.2 kg/m2. LV systolic dysfunction with LVEF <0.5 was observed in 165 (13.2%) ESRD patients at the beginning of HD therapy.
Table 1 shows baseline characteristics stratified by LVEF values: group 1 consisted of subjects with LVEF ≥0.6 (n = 842); group 2, LVEF ≥0.5 and <0.6 (n = 247); group 3, LVEF ≥0.4 and <0.5 (n = 107); group 4, LVEF ≥0.3 and <0.4 (n = 41); group 5, LVEF <0.3 (n = 17). Gender (P = 0.016), age (P = 0.013), incidence of diabetes (P = 0.010), hypertension (P = 0.0008), and LV mass index (P < 0.0001) were significantly different among the groups.
Table 1.
Baseline characteristics among groups according to LVEF levels
| Entire Cohort | ≥0.6 (n = 842) | 0.6 to 0.5 (n = 247) | 0.5 to 0.4 (n = 107) | 0.4 to 0.3 (n = 41) | <0.3 (n = 17) | P | |
|---|---|---|---|---|---|---|---|
| Male | 66.0 | 63.3 | 74.1 | 60.7 | 73.2 | 70.6 | 0.016 |
| Age (years) | 62 ± 14 | 59.0 ± 14.1 | 59.4 ± 13.4 | 59.5 ± 14.2 | 63.2 ± 11.2 | 68.1 ± 12.3 | 0.033 |
| Diabetes | 45.0 | 41.3 | 49.4 | 52.8 | 60.0 | 52.9 | 0.010 |
| Hypertension | 71.9 | 73.2 | 71.6 | 80.6 | 55.3 | 37.5 | 0.0008 |
| Dyslipidemia | 16.5 | 16.0 | 16.1 | 20.4 | 20.5 | 12.5 | 0.76 |
| Smoking | 24.7 | 22.9 | 33.8 | 13.6 | 27.3 | 40.0 | 0.061 |
| BMI (kg/m2) | 21.0 ± 3.2 | 21.1 ± 3.3 | 20.8 ± 3.1 | 21.0 ± 2.9 | 20.6 ± 2.9 | 19.9 ± 2.2 | 0.42 |
| Hematocrit | 29.2 ± 4.4 | 29.3 ± 4.5 | 29.6 ± 4.5 | 29.0 ± 4.5 | 28.5 ± 3.3 | 29.2 ± 3.7 | 0.69 |
| Albumin (g/dl) | 3.5 ± 0.4 | 3.5 ± 0.4 | 3.5 ± 0.5 | 3.4 ± 0.4 | 3.4 ± 0.4 | 3.6 ± 0.4 | 0.14 |
| Calcium (mg/dl) | 8.1 ± 0.9 | 8.1 ± 0.9 | 8.1 ± 0.8 | 8.0 ± 0.9 | 8.1 ± 1.0 | 7.8 ± 0.6 | 0.62 |
| Phosphate (mg/dl) | 5.1 ± 1.4 | 5.0 ± 1.3 | 5.2 ± 1.6 | 5.3 ± 1.8 | 4.9 ± 1.2 | 4.7 ± 1.0 | 0.18 |
| CRP (mg/l) | 10.5 ± 23.8 | 9.1 ± 22.5 | 11.7 ± 23.4 | 11.2 ± 23.7 | 7.3 ± 10.6 | 15.7 ± 17.5 | 0.39 |
| LVMI (g/m2) | 259 ± 89 | 246 ± 83 | 280 ± 89 | 286 ± 103 | 317 ± 108 | 287 ± 76 | <0.0001 |
LVMI, left ventricular mass index. Values are given as mean ± SD or percentage.
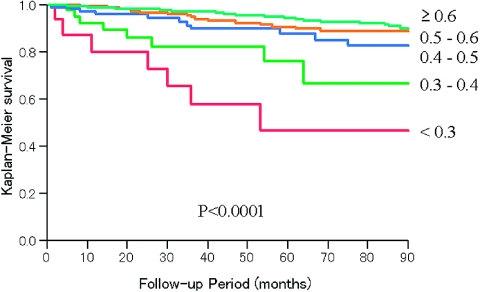
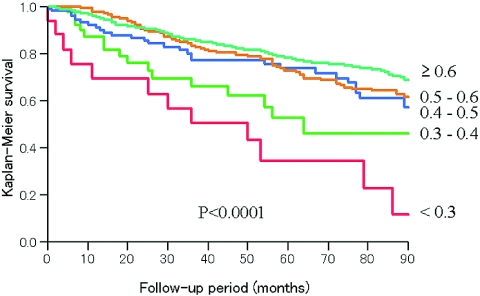
A total of 317 patients (25.3%) died during the follow-up period (Table 2). Among them, 99 (7.9% of total patients) of these deaths were cardiovascular deaths. Figure 1 shows Kaplan-Meier curves for the primary endpoint. The cardiovascular deaths significantly increased when the LVEF levels decreased. The 7-year event-free rates from cardiovascular deaths were 84.2, 83.7, 73.6, 59.4, and 30.9% in groups 1, 2, 3, 4, and 5, respectively. According to the secondary endpoint, survival rates significantly decreased as the LVEF levels decreased. The 7-year event-free rates from all-cause death were 69.2, 61.7, 57.1, 45.9, and 23.1% in groups 1, 2, 3, 4, and 5, respectively (Figure 2).
Table 2.
Proportion of mortality among the groups according to LVEF levels
| ≥0.6 (n = 842) | 0.6 to 0.5 (n = 247) | 0.5 to 0.4 (n = 107) | 0.4 to 0.3 (n = 41) | <0.3 (n = 17) | |
|---|---|---|---|---|---|
| Overall death, N (%) | 186 (22.1) | 70 (28.3) | 33 (30.8) | 16 (39.0) | 12 (70.6) |
| Cardiovascular death, N (%) | 48 (5.7) | 21 (8.5) | 13 (12.1) | 9 (21.9) | 8 (47.1) |
| Noncardiovascular death, N (%) | 138 (16.4) | 49 (19.8) | 20 (18.7) | 7 (17.1) | 4 (23.5) |
| Proportion of cause of death | |||||
| Cardiovascular (%) | 25.8 | 30.0 | 39.3 | 56.2 | 66.7 |
| heart failure (%) | 9.7 | 14.3 | 24.2 | 18.8 | 41.7 |
| myocardial infarction (%) | 7.5 | 4.3 | 3.0 | 12.5 | 8.3 |
| sudden death (%) | 4.8 | 2.9 | 6.1 | 6.3 | 8.3 |
| arrhythmia (%) | 1.1 | 7.1 | 3.0 | 12.5 | 8.3 |
| other cardiovascular (%) | 2.7 | 1.4 | 3.0 | 6.3 | 0.0 |
| Noncardiovascular (%) | 74.2 | 70.0 | 60.7 | 43.8 | 33.3 |
Figure 1.
Kaplan-Meier estimates: Event-free survival from cardiovascular death.
Figure 2.
Kaplan-Meier estimates: Event-free survival from all-cause death.
Table 2 shows the proportion of cause of death among the groups according to LVEF levels. The lower the LVEF, the more frequent the cardiovascular deaths. Especially, in group 5, cardiovascular death accounted for 70% of total deaths.
Table 3 and Table 4 show the results of Cox hazard analysis to determine the predictive value for cardiovascular mortality and all-cause mortality. As LVEF decreased, the risks of cardiovascular death and all-cause death increased, even after multivariate analysis. These data suggested that LV systolic dysfunction was a strong and independent predictor of cardiovascular death and all-cause death. For cardiovascular mortality, the age, diabetes, and serum CRP levels were also independent predictors (age: HR 1.03, 95% CI 1.01 to 1.05, P = 0.0041; diabetes: HR 2.36, 95% CI 1.45 to 3.87, P = 0.0006; serum CRP levels: HR 1.01, 95% CI 1.01 to 1.02, P = 0.0002). As to all-cause mortality, other independent predictors were age, male gender, diabetes, BMI, serum albumin levels, and serum CRP levels (age: HR 1.05, 95% CI 1.03 to 1.06, P < 0.0001; male: HR 1.60, 95% CI 1.08 to 2.38, P = 0.019; diabetes: HR 1.85, 95% CI 1.30 to 2.64, P = 0.0007; BMI: HR 0.86, 95% CI 0.80 to 0.92, P < 0.0001; serum albumin levels: HR 0.62, 95% CI 0.43 to 0.90, P = 0.012; serum CRP levels: HR 1.01, 95% CI 1.01 to 1.02, P < 0.0001).
Table 3.
Predictive value of LVEF for cardiovascular mortality
| Nonadjusted |
Adjusted |
|||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| LVEF (versus ≥0.6) | <0.0001 | <0.0001 | ||
| 0.5 to 0.6 | 1.45 (0.87 to 2.44) | 1.20 (0.65 to 2.21) | ||
| 0.4 to 0.5 | 2.41 (1.27 to 4.56) | 2.58 (1.19 to 5.06) | ||
| 0.3 to 0.4 | 5.32 (2.50 to 11.3) | 4.99 (1.91 to 13.0) | ||
| <0.3 | 11.53 (5.18 to 25.7) | 9.42 (3.82 to 23.3) | ||
| Age | 1.03 (1.01 to 1.05) | 0.0041 | ||
| Diabetes | 2.36 (1.45 to 3.87) | 0.0006 | ||
| CRP | 1.01 (1.01 to 1.02) | 0.0002 | ||
Table 4.
Predictive value of LVEF for all-cause mortality
| Nonadjusted |
Adjusted |
|||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| LVEF (versus ≥0.6) | <0.0001 | <0.0001 | ||
| 0.5 to 0.6 | 1.21 (0.92 to 1.59) | 1.02 (0.80 to 1.42) | ||
| 0.4 to 0.5 | 1.45 (0.99 to 2.13) | 1.26 (1.01 to 1.85) | ||
| 0.3 to 0.4 | 2.55 (1.53 to 4.25) | 4.00 (2.02 to 7.92) | ||
| <0.3 | 4.74 (2.64 to 8.51) | 7.28 (3.06 to 7.34) | ||
| Age | 1.60 (1.08 to 2.38) | 0.019 | ||
| Male | 1.05 (1.03 to 1.06) | <0.0001 | ||
| Diabetes | 1.85 (1.30 to 2.64) | 0.0007 | ||
| Body mass index | 0.86 (0.80 to 0.92) | <0.0001 | ||
| Serum albumin | 0.62 (0.43 to 0.90) | 0.012 | ||
| CRP | 1.01 (1.01 to 1.02) | <0.0001 | ||
Table 5 shows the results of the Harrell C index calculations for Cox regression analysis predicting cardiovascular mortality and all-cause mortality in a baseline model with established risk factors and a model with established risk factors plus LVEF. The Harrell C index increased significantly when LVEF was added to a model with established risk factors in prediction of both cardiovascular mortality and all-cause mortality (0.789 versus 0.750, P = 0.0049; 0.768 versus 0.751, P = 0.001, respectively).
Table 5.
Harrell C index for Cox regression models predicting cardiovascular mortality and all-cause mortality
| C Index | 95% CI | P | |
|---|---|---|---|
| Cardiovascular mortality | |||
| established risk factors | 0.750 | 0.682 to 0.818 | Reference |
| established risk factors plus LVEF | 0.789 | 0.715 to 0.863 | 0.0049 |
| All-cause mortality | |||
| established risk factors | 0.751 | 0.712 to 0.790 | Reference |
| established risk factors plus LVEF | 0.768 | 0.729 to 0.809 | 0.0010 |
Established risk factors included age, gender, BMI, diabetes, hypertension, dyslipidemia, smoking status, serum albumin levels, serum C-reactive protein levels, and LV mass index.
When we divided patients into quartiles according to LVEF, the first quartile (Q1), second quartile (Q2), third quartile (Q3), and fourth quartile (Q4) included patients with LVEF <0.559, 0.559 to 0.614, 0.614 to 0.653, and ≥0.653, respectively. The 7-year event-free rates from cardiovascular death were 81.7% in Q1, 92.0% in Q2, 93.8% in Q3, and 87.6% in Q4 by Kaplan-Meier survival rate (P = 0.0004). As to all-cause death, the 7-year event-free rates were 57.0% in Q1, 71.8% in Q2, 75.8% in Q3, and 67.7% in Q4 (P = 0.0015).
We performed logistic regression analysis to assess the association of clinical characteristics and other UCG variables with LVEF <0.5. Diabetes, asynergic wall motion, and mitral regurgitation were independently associated with LVEF <0.5 (diabetes: OR 1.48, 95% CI 1.02 to 2.13, P = 0.038; asynergic wall motion: OR 3.68, 95% CI 2.61 to 5.20, P < 0.0001; mitral regurgitation: OR 2.07, 95% CI 1.70 to 2.51, P < 0.0001).
Discussion
The main finding of this study is that the reduced LVEF at the start of HD strongly predicts poor survival for both cardiovascular and all-cause mortality. Severe LV systolic dysfunction (LVEF <0.3) had a ninefold higher risk for cardiovascular death and a fourfold higher risk for all-cause death even after adjustment for other risk factors. Besides, even mild LV systolic dysfunction significantly worsened a survival rate in HD patients. Furthermore, more than one tenth of patients had LVEF levels <0.5 when starting HD therapy. One strength of this study is that the sample size is relatively large; enrolled HD patients numbered 1254. In addition, we calculated the Harrell C index to determine model discrimination and showed that a combination of established risk factors and LVEF significantly increased the C index to predict both cardiovascular and all-cause mortality, compared with a combination of established risk factors only.
So far, many studies have attempted to investigate whether there is a causal relationship between the reduced LVEF and mortality (10,12,19–23); however, the results have been inconsistent. Of those studies, Curtis and co-workers showed that lower LVEF is associated with a linear increment in mortality in outpatients with stable heart failure. Furthermore, even after adjustment for other risk factors, LVEF <35% is an independent predictor in a large cohort study recruiting nearly 8000 patients with stable heart failure (10). However, the study consisted of a limited number of patients with chronic kidney disease. On the other hand, Zoccali and co-workers enrolled 250 asymptomatic HD patients with mean duration of HD for 40 months and assessed the prognostic value of LV systolic function prospectively (12). They showed that if the LVEF decreases by 1%, the risk of fatal and nonfatal cardiovascular events independently increase by 1.04-fold on multivariate analysis in patients on hemodialysis. They suggested repeating UCG after 1.5 years might be useful for risk stratification. However, few reports have examined the potential association between the value of LVEF at the beginning of HD therapy and the prognosis in patients with ESRD. Only one report has shown that such populations are associated with lower cardiac functions upon starting therapy for ESRD, resulting in a poor prognosis (24). We consider the point when starting HD therapy to be very important because predictors for future cardiovascular events are clinically relevant. The present findings may, thus, be of great significance from the viewpoint of risk stratification in ESRD patients at the beginning of HD.
Another important finding in this study is that even mild LV systolic dysfunction significantly worsened the prognosis in ESRD patients. Pre-existing systemic arteriosclerosis and constant fluid overload in patients with ESRD might play an important additional role in poor survival. It is well known that microvascular disease and macrovascular disease, cardiac fibrosis, and sympathetic hyperactivity are associated with cardiovascular death including sudden death in patients on HD (25,26). These factors may also be related to structural cardiac abnormalities such as asynergic wall motion and mitral regurgitation. These multifactorial pathologic conditions might result in lower LVEF and a worse prognosis especially in patients with LV systolic dysfunction.
In agreement with previous studies, diabetes and serum CRP levels were associated with adverse clinical outcomes in this study. Diabetes has been well known as a risk factor for ischemic heart disease, reduced cardiac functions, and cardiac events (27,28). Serum CRP levels also reflect vascular wall inflammation and predict adverse cardiac events (29–31). In addition, BMI and serum albumin levels were inversely related to all-cause mortality (32,33). These factors might be related to MIA syndrome, which indicates malnutrition, inflammation, and atherosclerosis. These risk factors should also be considered in managing patients on HD.
Limitations
This study has several limitations. First, this study had a single-center design. Larger multicenter studies are warranted to corroborate our findings. Second, we did not evaluate LV diastolic function. Third, all enrolled patients in the study were Japanese. A report showed that 5-year survival rates in overall patients on HD were 54% in Japan, 48% in Europe, and 40% in the United States, respectively (34). These differences should be considered to interrupt the results. Fourth, we have no data on other variables related to dialysis therapy such as access or urea clearance × time normalized by total body water. Finally, precise medical treatment and therapeutic intervention were not evaluated in this study. These data may be very clinically important. We did not have data on the efficacies of medications to prevent adverse events. Further investigations are warranted in this regard.
Conclusions
LVEF at inception of dialysis appears to be a strong prognostic marker for CV and all-cause death. Knowledge of LVEF improved discrimination of a prognostic model incorporating known cardiovascular risk factors and may be a useful adjunct in assessing the mortality risk in incident dialysis patients.
Disclosures
None.
Acknowledgments
The authors thank Dr. Shonen Yoshida (Division of Clinical Research, Nagoya Kyoritsu Hospital) for valuable suggestions on this manuscript. We also thank Mr. Koichi Ibuki and Mr. Ryuhei Kanda (Division of Clinical Laboratory, Nagoya Kyoritsu Hospital) for their technical support.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Lindner A, Charra B, Sherrard DJ, Scribner BH: Accelerated atherosclerosis in prolonged maintenance hemodialysis. N Engl J Med 290: 697–701, 1974 [DOI] [PubMed] [Google Scholar]
- 2.Goldsmith DJA, Covic A: Coronary artery disease in uremia: Etiology, diagnosis, and therapy. Kidney Int 60: 2059–2078, 2001 [DOI] [PubMed] [Google Scholar]
- 3.Herzog CA, Ma JZ, Collins AJ: Poor long-term survival after acute myocardial infarction among patients on long-term dialysis. N Engl J Med 339: 799–805, 1998 [DOI] [PubMed] [Google Scholar]
- 4.Parfrey PS, Foley RN: The clinical epidemiology of cardiac disease in chronic renal failure. J Am Soc Nephrol 10: 1606–1615, 1999 [DOI] [PubMed] [Google Scholar]
- 5.Cheung AK, Sarnak MJ, Yan G, Dwyer JT, Heyka RJ, Rocco MV, Teehan BP, Levey AS: The Hemodialysis (HEMO) Study. Atherosclerotic cardiovascular disease risks in chronic hemodialysis patients. Kidney Int 58: 353–362, 2000 [DOI] [PubMed] [Google Scholar]
- 6.Stack AG, Bloembergen WE: A cross-sectional study of the prevalence and clinical correlates of congestive heart failure among incident US dialysis patients. Am J Kidney Dis 38: 992–1000, 2001 [DOI] [PubMed] [Google Scholar]
- 7.Trespalacios FC, Taylor AJ, Agodoa LY, Bakris GL, Abbott KC: Heart failure as a cause for hospitalization in chronic dialysis patients. Am J Kidney Dis 41: 1267–1277, 2003 [DOI] [PubMed] [Google Scholar]
- 8.Parfrey PS, Foley RN, Harnett JD, Kent GM, Murray DC, Barre PE: Outcome and risk factors for left ventricular disorders in chronic uraemia. Nephrol Dial Transplant 11: 1277–1285, 1996 [PubMed] [Google Scholar]
- 9.Hunt SA, Baker DW, Chin MH, Cinquegrani MP, Feldman AM, Francis GS, Ganiats TG, Goldstein S, Gregoratos G, Jessup ML, Noble RJ, Packer M, Silver MA, Stevenson LW, Gibbons RJ, Antman EM, Alpert JS, Faxon DP, Fuster V, Jacobs AK, Hiratzka LF, Russell RO, Smith SC, Jr.: American College of Cardiology/American Heart Association ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: Executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1995 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol 38: 2101–2113, 2001 [DOI] [PubMed] [Google Scholar]
- 10.Curtis JP, Sokol SI, Wang Y, Rathore SS, Ko DT, Jadbabaie F, Portnay EL, Marshalko SJ, Radford MJ, Krumholz HM: The association of left ventricular ejection fraction, mortality, and cause of death in stable outpatients with heart failure. J Am Coll Cardiol 42: 736–742, 2003 [DOI] [PubMed] [Google Scholar]
- 11.K/DOQI Workgroup K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis 45[Suppl 3]: S1–S154, 2005 [PubMed] [Google Scholar]
- 12.Zoccali C, Benedetto FA, Mallamaci F, Tripepi G, Giacone G, Cataliotti A, Seminara G, Stancanelli B, Malatino LS: Prognostic value of echocardiographic indicators of left ventricular systolic function in asymptomatic dialysis patients. J Am Soc Nephrol 15: 1029–1037, 2004 [DOI] [PubMed] [Google Scholar]
- 13.Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I, Silverman NH, Tajik AJ: Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 2: 358–367, 1989 [DOI] [PubMed] [Google Scholar]
- 14.Laaban JP, Pascal-Sebaoun S, Bloch E, Orvoën-Frija E, Oppert JM, Huchon G: Left ventricular systolic dysfunction in patients with obstructive sleep apnea syndrome. Chest 122: 1133–1138, 2002 [DOI] [PubMed] [Google Scholar]
- 15.Kjøller-Hansen L, Steffensen R, Grande P: Beneficial effects of ramipril on left ventricular end-diastolic and end-systolic volume indexes after uncomplicated invasive revascularization are associated with a reduction in cardiac events in patients with moderately impaired left ventricular function and no clinical heart failure. J Am Coll Cardiol 37: 1214–1220, 2001 [DOI] [PubMed] [Google Scholar]
- 16.Harrell FE, Jr, Lee KL, Mark DB: Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15: 361–387, 1996 [DOI] [PubMed] [Google Scholar]
- 17.Pencina MJ, D'Agostino RB: Overall C as a measure of discrimination in survival analysis: Model specific population value and confidence interval estimation. Stat Med 23: 2109–2123, 2004 [DOI] [PubMed] [Google Scholar]
- 18.Harrell FE, Jr.: Quantifying predictive ability. In: Regression Modeling Strategies with Applications to Linear Models, Logistic Regression, and Survival Analysis, 1st ed., New York, Springer, 2001, pp 492–493 [Google Scholar]
- 19.Pozzoli M, Capomolla S, Pinna G, Cobelli F, Tavazzi L: Doppler echocardiography reliably predicts pulmonary artery wedge pressure in patients with chronic heart failure with and without mitral regurgitation. J Am Coll Cardiol 27: 883–893, 1996 [DOI] [PubMed] [Google Scholar]
- 20.Giannuzzi P, Temporelli PL, Bosimini E, Silva P, Imparato A, Corrà U, Galli M, Giordano A: Independent and incremental prognostic value of Doppler-derived mitral deceleration time of early filling in both symptomatic and asymptomatic patients with left ventricular dysfunction. J Am Coll Cardiol 28: 383–390, 1996 [DOI] [PubMed] [Google Scholar]
- 21.Juillière Y, Barbier G, Feldmann L, Grentzinger A, Danchin N, Cherrier F: Additional predictive value of both left and right ventricular ejection fractions on long-term survival in idiopathic dilated cardiomyopathy. Eur Heart J 18: 276–280, 1997 [DOI] [PubMed] [Google Scholar]
- 22.Vasan RS, Larson MG, Benjamin EJ, Evans JC, Reiss CK, Levy D: Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population-based cohort. J Am Coll Cardiol 33: 1948–1955, 1999 [DOI] [PubMed] [Google Scholar]
- 23.Gottdiener JS, McClelland RL, Marshall R, Shemanski L, Furberg CD, Kitzman DW, Cushman M, Polak J, Gardin JM, Gersh BJ, Aurigemma GP, Manolio TA: Outcome of congestive heart failure in elderly persons: Influence of left ventricular systolic function. The Cardiovascular Health Study. Ann Intern Med 137: 631–639, 2002 [DOI] [PubMed] [Google Scholar]
- 24.Foley RN, Parfrey PS, Harnett JD, Kent GM, Martin CJ, Murray DC, Barre PE: Clinical and echocardiographic disease in patients starting end-stage renal disease therapy. Kidney Int 47: 186–192, 1995 [DOI] [PubMed] [Google Scholar]
- 25.Ritz E, Wanner C: The challenge of sudden death in dialysis patients. Clin J Am Soc Nephrol 3: 920–929, 2008 [DOI] [PubMed] [Google Scholar]
- 26.de Bie MK, van Dam B, Gaasbeek A, van Buren M, van Erven L, Bax JJ, Schalij MJ, Rabelink TJ, Jukema JW: The current status of interventions aiming at reducing sudden cardiac death in dialysis patients. Eur Heart J 30: 1559–1564, 2009 [DOI] [PubMed] [Google Scholar]
- 27.Wanner C, Krane V, März W, Olschewski M, Mann JF, Ruf G, Ritz E: German Diabetes and Dialysis Study Investigators. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med 353: 238–248, 2005 [DOI] [PubMed] [Google Scholar]
- 28.Drechsler C, Krane V, Ritz E, März W, Wanner C: Glycemic control and cardiovascular events in diabetic hemodialysis patients. Circulation 120: 2421–2428, 2009 [DOI] [PubMed] [Google Scholar]
- 29.Ridker PM, Rifai N, Rose L, Buring JE, Cook NR: Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med 347: 1557–1565, 2002 [DOI] [PubMed] [Google Scholar]
- 30.Ridker PM: Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation 107: 363–369, 2003 [DOI] [PubMed] [Google Scholar]
- 31.Ishii H, Toriyama T, Aoyama T, Takahashi H, Amano T, Hayashi M, Tanaka M, Kawamura Y, Yasuda Y, Yuzawa Y, Maruyama S, Matsuo S, Matsubara T, Murohara T: Prognostic values of C-reactive protein levels on clinical outcome after implantation of sirolimus-eluting stents in patients on hemodialysis. Circ Cardiovasc Intervent 2: 513–518, 2009 [DOI] [PubMed] [Google Scholar]
- 32.Stenvinkel P, Heimbürger O, Paultre F, Diczfalusy U, Wang T, Berglund L, Jogestrand T: Strong association between malnutrition, inflammation, and atherosclerosis in chronic renal failure. Kidney Int 55: 1899–1911, 1999 [DOI] [PubMed] [Google Scholar]
- 33.Pecoits-Filho R, Lindholm B, Stenvinkel P: The malnutrition, inflammation, and atherosclerosis (MIA) syndrome – the heart of the matter. Nephrol Dial Transplant 17[Suppl 11]: 28–31, 2002 [DOI] [PubMed] [Google Scholar]
- 34.Held PJ, Brunner F, Odaka M, Garcia JR, Port FK, Gaylin DS: Five-year survival for end-stage renal disease patients in the United States, Europe, and Japan, 1982 to 1987. Am J Kidney Dis 15: 451–457, 1990 [DOI] [PubMed] [Google Scholar]