Abstract
Background and objectives: Matrix metalloproteinases (MMPs) are risk factors for cardiovascular diseases. This study evaluated the association of genotype polymorphisms of MMPs and tissue inhibitors of metalloproteinases (TIMPs) in hemodialysis (HD) patients with arteriovenous fistula (AVF) failure.
Design, setting, participants, & measurements: Genotype polymorphism of MMP-1, MMP-2, MMP-3, and MMP-9 and TIMP-1 and TIMP-2 and clinical and laboratory parameters were compared between Chinese HD patients with (n = 170) and without (n = 426) AVF failure.
Results: Significant associations were found between AVF failure and the following factors (hazard ratio): longer HD duration (1.007 per month), lower pump flow (0.991 per ml/min), higher dynamic venous pressure (1.016 per mmHg), location of AVF on right side (1.630 versus left side) and upper arm (2.385 versus forearm), history of cardiovascular disease (1.656 versus absence of history), 1G/1G genotype of MMP-1 −1607 1G >2G SNP (2.315 versus 1G/2G + 2G/2G genotypes), 6A/6A genotype of MMP-3 −1612 5A >6A SNP (1.712 versus 5A/6A + 5A/5A), and C/C genotype of MMP-9 −1562 C>T SNP (1.650 versus C/T+T/T). The positive predictive rates for AVF failure were 63.0% and 6.7% for patients with the highest-risk (1G1G/6A6A/CC) and lowest-risk (2G2G or 2G1G/5A5A or 6A6A/TT or TC) composite MMP-1/MMP-3/MMP-9 genotype, respectively. The unassisted patency of AVF at 5 years decreased significantly from 93.3% to 38.4% for the composite MMP-1/MMP-3/MMP-9 genotypes (lowest versus highest risk, P < 0.001).
Conclusions: Specific genotypes of MMP-1, MMP-3 and MMP-9 with lower transcriptional activity are associated with higher frequencies of AVF failure, which may result from more accumulation of extracellular matrix, leading to AVF stenosis.
In patients with ESRD, achieving adequate hemodialysis (HD) depends on a well functioning vascular access. Long-term vascular survival is best for the native arteriovenous fistula (AVF), which accounts for a prevalence of approximately 85% of vascular access in Taiwan. However, stenosis and thrombosis substantially contribute to the difficulty in maintaining the patency of AVF. Stenoses account for over 80% of AVF thromboses; thromboses are responsible for 80% to 85% of AVF failures (1). Stenosis of vascular access is histologically characterized by intimal hyperplasia, which results from the initial proliferation of vascular smooth muscle cells (VSMCs) and the subsequent migration of VSMCs from the media to the intima, and exuberant synthesis of extracellular matrix, which leads to further intimal expansion (2).
In addition to the surgical technique of fistula anastomosis and puncture skills, several medical factors may result in the stenosis of AVF, including endothelial dysfunction, stasis, hypercoagulability, medications, and red blood cell mass (3). Among the factors leading to endothelial dysfunction, matrix metalloproteinases (MMPs) are associated with VSMC migration and the degradation of extracellular matrix, which may contribute to the development of AVF stenosis.
The family of MMPs includes at least 25 secreted or surface-bound proteases (4), of which 14 have been identified in vascular cells. According to structural homology and substrate specificity, MMPs can be classified into five subgroups: interstitial collagenases (MMP-1, MMP-8, and MMP-13), gelatinases (MMP-2 and MMP-9), stromelysins/matrilysins (MMP-3, MMP-7, and MMP-10), membrane-type MMPs (MT-MMPs, from MMP-14 to MMP-17), and others (MMP-11 and MMP-12) (5). Some MMPs are expressed as latent or inactive proforms, whereas the MT-MMPs are activated in the endosomal pathway. The activity of MMPs can be regulated at four levels: expression of MMP genes, vesicle secretion and trafficking, activation of inactive proforms, and binding with specific tissue inhibitors of metalloproteinases (TIMPs) (5,6).
The association of genotype polymorphisms of some MMPs with cardiovascular disorders has been widely discussed in previous reports. Rutter et al. (7–9) have shown that the MMP-1 gene −1607 1G/2G polymorphism has an allele-specific effect on driving promoter activity and gene expression that is associated with coronary artery disease (CAD). According to Vasku et al. (10), some specific haplotypes of four MMP-2 promoter polymorphisms (−1575G/A, −1306C/T, −790T/G, and −735C/T) influenced the risk of triple vessel CAD. Interestingly, specific genotype polymorphism(s) of MMP-3 gene −1612 5A/6A was (were) associated with higher frequency of coronary stenosis (11,12), myocardial infarction (13,14), coronary aneurysm (15), restenosis after coronary angioplasty (16,17), carotid intima-media thickness (18), carotid stenosis (19), stroke (20), and arterial stiffness and blood pressure (21). In addition, the MMP-9 −1562 C > T polymorphism has been associated with arterial stiffness (22), intracranial aneurysm (23), abdominal aortic aneurysm (24), and CADs (25,26).
Although the pathogenetic mechanisms of AVF have been well studied in the past few decades, the causes of developing stenoses still remain unknown in a significant proportion of HD patients, which may relate to the differences in genetic background among HD patients. Concerning this issue, AVF patency has been reported to be associated with specific genotype polymorphisms of TGF-β1 (27), methylene tetrahydrofolate reductase (28), and heme oxygenase-1 (29). However, little information is available on the role of MMP genotype polymorphisms in the development of AVF stenosis.
This study is designed to determine whether genotype polymorphisms of MMP/TIMP genes (MMP-1, MMP-2, MMP-3, MMP-9, TIMP-1, and TIMP-2) would be risk markers for stenosis of AVFs in HD patients.
Patients and Methods
Study Population
We screened all patients undergoing maintenance HD therapy at Taipei Veterans General Hospital, Shin-Jen HD Center, Hwa-Jong HD Center, and Wen-Lin HD center between January and March 2008 for whom medical records and blood samples for genotyping were available. We included patients in this study if they met the following criteria: (1) creation of a native AVF as the first vascular access for HD irrespective of temporary catheter use between January 1, 1999 and December 31, 2007; (2) creation of AVF by similar surgical skills with end-to-side anastomosis at upper extremity; and (3) receiving HD therapy for 4 hours three times weekly for more than 3 months. Patients were excluded if they fulfilled one of the following criteria: (1) receiving an arteriovenous graft as the first vascular access; or (2) the first episode of fistula failure or interventional procedure resulting from causes such as infectious complication, progressive aneurysmal formation, or steal syndrome. This retrospective study was based on the Helsinki Declaration (edition 6, revised 2000). The Institutional Research Board of Taipei Veterans General Hospital approved the study, and informed consent was obtained from all study patients. For HD patients, we recorded the clinical factors of age, gender, HD therapy duration, side (right or left) and location (elbow or wrist) of the first created native AVF, underlying cause of ESRD (presence or absence of diabetic nephropathy), times of AVF failure, peak dynamic venous pressure, and maximally delivered extracorporeal blood flow during the 30 days before AVF failure or the date of termination of observation. We also recorded the history of vascular diseases, including the presence of hypertension, presence of peripheral artery obstructive disease, presence of cerebrovascular disease, and presence of CAD before AVF failure for those with fistula failure or until March 31, 2008 for those without AVF failure. The primary end point was unassisted patency, which was defined as the time from fistula surgery to the first episode of fistula failure for patients meeting inclusion criteria without presence of any exclusion criteria. We defined fistula failure as the need for any interventional procedure (surgery or angioplasty) to correct a malfunctioning or occlusive fistula, which appeared at least 3 months after fistula surgery. Fistula failure within the first 3 months after fistula construction was regarded as inadequate dilation rather than intimal hyperplasia, so the appropriate timing for cannulation was approximately 3–4 months after placement of AVF, as suggested by Kidney Disease Outcomes Quality Initiative guidelines. These patients were excluded from our analysis. Patients were censored at the time of renal transplantation (n = 2), death with a functioning access (n = 8), shifting to peritoneal dialysis (n = 3), or loss to follow-up (n = 4).
Determination of Single Nucleotide Polymorphisms of MMP and TIMP Genes
Genomic DNA was isolated from anticoagulated venous blood samples using the Puregene DNA purification kit (Gentra, Minneapolis, MN). Single-nucleotide polymorphism (SNP) genotyping was performed using the amplification refractory mutation system PCR methodology. We amplified 50 to 100 ng of DNA in a final volume of 25 μl containing 2.5 mmol MgCl2 (Qiagen), 1× reaction buffer (Qiagen), 200 μmol each deoxynucleoside triphosphate (Roche Applied Science, Mannheim, Germany), 1× Solution Q (Qiagen), 5 μmol of each primer, and 1 U HotStar Taqpolymerase (Qiagen). Primers were designed as shown in Table 1. The protocol for the PCR Express Thermal Cycler was as follows: 15 minutes at 95°C, 30 cycles of 1 minute at 94°C, 30 seconds at 60°C, 1 minute at 72°C, and 7 minutes at 72°C. The amplified products were fractionated electrophoretically on a 2% agarose gel, visualized by ethidium bromide staining (0.5 mg/ml) and ultraviolet light detection, and cut by respective restriction enzymes or analyzed by direct sequencing (allelic discrimination with TaqMan MGB probe by ABI 7700). All typing analysis contained negative and positive controls.
Table 1.
Primer sequences and PCR conditions for amplification of MMP and TIMP SNPs
| SNP | rs Number | Method | Primer | Sequence (5′ to 3′) |
|---|---|---|---|---|
| TIMP-1 372 C/T | rs 4898 | RFLP-PCR | Forward | GCACATCACTACCTGCAGTC |
| Reverse | GAAACAAGCCCACGATTTAG | |||
| TIMP-2 −418 G/C | rs 8179090 | RFLP-PCR | Forward | CGTCTCTTGTTGGCTGGTCA |
| Reverse | CCTTCAGCTCGACTCTGGAG | |||
| TIMP-2 303 C/T | rs 2277698 | RFLP-PCR | Forward | TAGGAACAGCCCCACTTCTG |
| Reverse | CCTCCTCGGCAGTGTGTG | |||
| MMP-1 −1607 1G/2G | rs 11292517 | Fragment analysis | Forward | 6-fam-CCTCTGATGCCTCTGAGAAGA |
| Reverse | TCCTCCCCTTATGGATTCCT | |||
| MMP-2 −735 G/C | rs 2285053 | TaqMan Allelic discrimination | Forward | GGGTAAACCTCCCCACATTG |
| Reverse | ACAGTGGAAGGTCCCAGGTT | |||
| MMP-2 −1306 C/T | rs 243865 | ARMS-PCR | Forward | TGTTGGGAACGCCTGACTTCAG |
| Reverse | CTGACCCCCAGTCCTATCTGCC | |||
| MMP-3 −1612 5A/6A | rs 35068180 | Fragment analysis | Forward | (6-Fam)CCTGCCTCAACCTCTCAAAG |
| Reverse | AATTCACATCACTGCCACCA | |||
| MMP-9 −1562 C/T | rs 34016235 | Direct sequencing | Forward | CATAGCTGGAAAATGGCAGA |
| Reverse | TCGGGCAGGGTCTATATTCA |
ARMS, amplification refractory mutation system; RFLP, restriction fragment length polymorphism.
Statistical Analyses
Data management and statistical analyses were done using the SPSS statistical software (version 11.0). Distributions of continuous variables in groups were expressed as mean ± SD and compared by t test. All data had been tested for normal distribution before using t tests. Categorical variables, such as the distribution of genotype frequencies in patients and controls, were analyzed by χ2 test. Cox regression was performed to adjust for other established risk factors of AVF stenosis. Adjusted odds ratio and 95% confidence interval for every explanatory variable were also calculated. Survival curves of unassisted patency of AVF were calculated by the Kaplan–Meier method and compared by the log-rank test. A statistically significant value was P < 0.05.
Results
Patient Characteristics
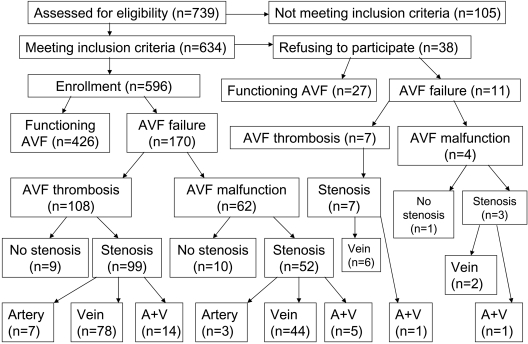
We summarize the lesions associated with AVF failure in Figure 1. One hundred and five patients did not meet the inclusion criteria, including using arteriovenous graft (n = 68) or tunneled catheter (n = 11) as vascular access, and the first episode of fistula failure or interventional procedure developing within 3 months after creation of AVF (n = 20) or resulting from causes such as infectious complication (n = 2), progressive aneurysmal formation (n = 3), or steal syndrome (n = 1). In addition, 38 patients refused to participate in this study, so we finally enrolled 596 HD patients. Among them, 426 did not have but 170 had failure of AVF, including 108 with thrombosis (total occlusion) and 62 with malfunction (not total occlusion but inadequate blood flow to attain HD efficiency) of AVF. The baseline clinical characteristics of these patients are listed in Table 2. Compared with HD patients without AVF failure, those with AVF failure had longer HD duration (89.5 ± 65.9 versus 62.2 ± 53.0 months, P < 0.001), higher prevalence of AVF at right upper extremity (31.8% versus 18.5%, P < 0.001) and upper arm (27.6% versus 9.2%, P < 0.001), higher dynamic venous pressure (147.5 ± 29.4 versus 140.0 ± 29.9 mmHg, P < 0.001), and lower prevalence of hypertension (45.3% versus 55.4%, P = 0.026).
Figure 1.
The flow chart of the enrollment process and the functional as well as anatomical characteristics of AVF in hemodialysis patients. A+V, stenosis of artery and vein.
Table 2.
Clinical characteristics of HD patients by the status of AVF failure
| Characteristic | Overall (n = 596) | No AVF Failure (n = 426) | AVF Failure (n = 170) | P |
|---|---|---|---|---|
| Male (%) | 52.9 | 51.9 | 55.3 | 0.36 |
| Age (years) | 60.0 ± 14.6 | 59.7 ± 14.0 | 60.5 ± 15.8 | 0.56 |
| HD duration (months) | 70.3 ± 58.3 | 62.2 ± 53.0 | 89.5 ± 65.9 | <0.001 |
| Hypertension (%) | 52.5 | 55.4 | 45.3 | 0.026 |
| Diabetes mellitus (%) | 30.4 | 30.8 | 29.6 | 0.78 |
| Cerebral infarction (%) | 8.4 | 7.7 | 10.0 | 0.37 |
| Peripheral arterial obstructive disease (%) | 4.7 | 4.0 | 6.5 | 0.196 |
| CAD (%) | 20.9 | 19.3 | 24.9 | 0.126 |
| CVD (%) | 26.7 | 24.6 | 32.1 | 0.061 |
| Site of AVF (%) | ||||
| right side | 22.3 | 18.5 | 31.8 | <0.001 |
| left side | 77.7 | 81.5 | 68.2 | |
| Location of AVF (%) | ||||
| upper arm | 14.4 | 9.2 | 27.6 | <0.001 |
| forearm | 85.6 | 90.8 | 72.4 | |
| Survival of AVF (months) | 56.6 ± 53.3 | 64.1 ± 52.8 | 38.0 ± 49.7 | <0.001 |
| Time between creation of AVF and initial HD (months) | 1.65 ± 6.22 | 1.77 ± 6.96 | 1.29 ± 3.90 | 0.38 |
| Dynamic venous pressure (mmHg) under pump flow at 250 ml/min | 142.2 ± 29.9 | 140.0 ± 29.9 | 147.5 ± 29.4 | <0.028 |
| Maximal pump flow (ml/min) | 271.9 ± 33.4 | 273.4 ± 34.5 | 268.3 ± 30.13 | 0.093 |
| Serum calcium (mg/dl) | 9.0 ± 0.8 | 8.9 ± 0.8 | 9.1 ± 0.7 | 0.79 |
| Serum phosphate (mg/dl) | 5.1 ± 1.2 | 5.0 ± 1.1 | 5.3 ± 1.3 | 0.52 |
| Calcium phosphate product (mg2/dl2) | 41.2 ± 12.1 | 40.8 ± 11.2 | 42.2 ± 13.8 | 0.58 |
| Parathyroid hormone (pg/ml) | 188.5 ± 69.1 | 194.5 ± 64.2 | 173.4 ± 80.7 | 0.24 |
Association of Genotype Polymorphisms of MMPs with AVF Failure in HD Patients
As shown in Table 3, HD patients with AVF failure (group 1) had higher frequencies of the following genotype polymorphisms of MMPs than those without AVF failure (group 2): 1G/1G genotype of MMP-1 −1607 1G >2G SNP (17% for group 1 versus 9.2% for group 2, P = 0.006), 6A/6A genotype of MMP-3 −1612 5A >6A SNP (84.7% for group 1 versus 76.1% for group 2, P = 0.020), and C/C genotype of MMP-9 −1562 C>T SNP (81.2% for group 1 versus 72.1% for group 2, P = 0.021). However, there was no difference in the frequencies of genotype polymorphisms of MMP-2, TIMP-1, and TIMP-2 between HD patients with and without AVF failure.
Table 3.
Comparison of percentage of genotype polymorphisms of MMPs among total and subgroups of HD patients with and without AVF failure
| Genotype Polymorphisms of MMPs | Total HD Patients (n = 596) | HD Patients without AVF Failure (n = 426) | HD Patients with AVF Failure (n = 170) | P |
|---|---|---|---|---|
| MMP-1 −1607 1G/2G | ||||
| (1) 2G2G | 293 (49.2%) | 214 (50.2%) | 79 (46.5%) | 0.006 for (1) + (2) versus (3) |
| (2) 2G1G | 235 (39.4%) | 173 (40.6%) | 62 (36.5%) | |
| (3) 1G1G | 68 (11.4%) | 39 (9.2%) | 29 (17.0%) | |
| MMP-2 −735 C/T | ||||
| (1) CC | 319 (53.5%) | 228 (53.5%) | 91 (53.5%) | 0.989 |
| (2) CT | 230 (38.6%) | 164 (38.5%) | 66 (38.8%) | |
| (3) TT | 47 (7.9%) | 34 (8.0%) | 13 (7.7%) | |
| MMP-2 −790 T/G; −1306 C/T; −1575 G/A | ||||
| (1) TT; CC; GG | 476 (79.8%) | 337 (79.1%) | 139 (81.8%) | 0.465 for (1) versus (2) + (3) |
| (2) TG; CT; GA | 119 (20.0%) | 89 (20.9%) | 30 (17.6%) | |
| (3) GG; TT; AA | 1 (0.2%) | 0 | 1 (0.6%) | |
| MMP-3 −1612 5A/6A | ||||
| (1) 5A5A | 12 (2.0%) | 10 (2.3%) | 2 (1.2%) | 0.020 for (1) + (2) versus (3) |
| (2) 5A6A | 116 (19.5%) | 92 (21.6%) | 24 (14.1%) | |
| (3) 6A6A | 468 (78.5%) | 324 (76.1%) | 144 (84.7%) | |
| MMP-9 −1562 C/T | ||||
| (1) TT | 5 (0.8%) | 4 (0.9%) | 1 (0.6%) | 0.021 for (1) + (2) versus (3) |
| (2) CT | 146 (24.5%) | 115 (27.0%) | 31 (18.2%) | |
| (3) CC | 445 (74.7%) | 307 (72.1%) | 138 (81.2%) | |
| TIMP-1 −393 C/T | ||||
| male | ||||
| (1) C | 150 (47.6%) | 109 (49.1%) | 41 (44.1%) | 0.416 |
| (2) T | 165 (52.4%) | 113 (50.9%) | 52 (55.9%) | |
| female | ||||
| (1) CC | 62 (22.1%) | 46 (22.6%) | 16 (20.8%) | 0.415 |
| (2) CT | 114 (40.6%) | 78 (38.2%) | 36 (46.8%) | |
| (3) TT | 105 (37.3%) | 80 (39.2%) | 25 (32.4%) | |
| TIMP-2 303 G/A | ||||
| (1) GG | 359 (60.2%) | 254 (59.6%) | 105 (61.8%) | 0.434 |
| (2) GA | 207 (34.8%) | 153 (35.9%) | 54 (31.8%) | |
| (3) AA | 30 (5.0%) | 19 (4.5%) | 11 (6.5%) | |
| TIMP-2 −418 G/C | ||||
| (1) GG | 395 (66.3%) | 279 (65.5%) | 116 (68.2%) | 0.772 |
| (2) GC | 180 (30.2%) | 131 (30.8%) | 49 (28.8%) | |
| (3) CC | 21 (3.5%) | 16 (3.8%) | 5 (2.9%) |
Cox Regression Model of Multivariate Analysis for AVF Failure
Table 4 shows the Cox regression model for the association of AVF failure with the selected parameters carrying obvious or borderline statistical significances from Tables 2 and 3. Significant associations were found between AVF failure and the following factors (hazard ratio): longer HD duration (1.007 per month), lower pump flow (0.991 per ml/min), higher dynamic venous pressure (1.016 per mmHg), location of AVF on right side (1.630 versus left side), upper arm (2.385 versus forearm), presence of cardiovascular disease (CVD; 1.656 versus absence), 1G/1G genotype of MMP-1 −1607 1G >2G SNP (2.315 versus 1G/2G + 2G/2G genotypes), 6A/6A genotype of MMP-3 −1612 5A >6A SNP (1.712 versus 5A/6A + 5A/5A genotypes), and C/C genotype of MMP-9 −1562 C>T SNP (1.650 versus C/T+T/T genotypes).
Table 4.
Cox regression model of factors associated with AVF failure in HD patients
| Significance | Hazard Ratio | 95% CI Lower | 95% CI Upper | |
|---|---|---|---|---|
| HD duration (months) | <0.001 | 1.007 | 1.004 | 1.010 |
| Pump flow (ml/min) | 0.013 | 0.991 | 0.984 | 0.998 |
| Maximal venous pressure (mmHg) | <0.001 | 1.016 | 1.008 | 1.023 |
| Right versus left side | 0.039 | 1.630 | 1.026 | 2.590 |
| Upper arm versus forearm | 0.001 | 2.385 | 1.400 | 4.064 |
| Cardiovascular disease | 0.039 | 1.656 | 1.025 | 2.675 |
| Hypertension | 0.202 | 0.760 | 0.499 | 1.158 |
| MMP-1 −1607 genotypes (1G/1G versus 1G/2G + 1G/2G) | 0.007 | 2.315 | 1.258 | 4.260 |
| MMP-3 −1612 genotypes (6A/6A versus 5A/6A + 5A/5A) | 0.049 | 1.712 | 1.003 | 2.924 |
| MMP-9 −1562 genotypes (C/C versus C/T + T/T) | 0.048 | 1.650 | 1.005 | 2.710 |
CI, confidence interval.
Association of Composite MMP Genotypes with AVF Failure in HD Patients
According to the data in Tables 3 and 4, the abovementioned genotypes could be divided into two genotypes each for MMP-1, MMP-3, and MMP-9, respectively (i.e., high-risk or low-risk genotype). Thus, eight composite genotypes could be derived from the random combination of either genotype of MMP-1, MMP-3, and MMP-9 (Table 5). The highest-risk composite genotype of MMP-1/MMP-3/MMP-9 was 1G1G/6A6A/CC, with a positive predictive rate of 63% for AVF failure; on the contrary, that for the lowest-risk genotype (2G2G or 2G1G/5A5A or 6A6A/TT or TC) was only 6.7%. As compared with the most common genotype 2G1G or 2G2G/6A6A/CC (which accounts for 54.9% of the study subjects), the association with higher or lower frequency of AVF failure was still significant for the highest- or lowest-risk genotype, respectively, in univariate and multivariate regression models after adjustment for location and side of AVF, duration of HD, extracorporeal pump flow rate, maximal dialytic venous pressure, hypertension, and CVD.
Table 5.
Univariate and multivariate regression models for composite MMP genotypes in association with AVF failure in HD patients
| Composite Genotypes for MMP-1/-3/-9 | Rate of AVF Failure (%) | Univariate Regression Hazard Ratio (95% CI), P | Multivariate Regressionc Hazard Ratio (95% CI), P |
|---|---|---|---|
| 2GnG/6A6A/CCa | 30.3 (99/327) | 1.0 (–), – | 1.0 (–), – |
| 2GnG/5ANA/TXb | 6.7 (2/30) | 0.165 (0.038 to 0.704), 0.01 | 0.200 (0.045 to 0.889), 0.034 |
| 2GnG/5ANA/CC | 22.1 (15/68) | 0.652 (0.351 to 1.211), 0.176 | 0.740 (0.378 to 1.448), 0.379 |
| 2GnG/6A6A/TX | 24.3 (25/103) | 0.738 (0.444 to 1.227), 0.242 | 0.747 (0.421 to 1.325), 0.319 |
| 1G1G/5ANA/TX | 28.6 (2/7) | 0.921 (0.176 to 4.829), 0.923 | 1.593 (0.269 to 9.442), 0.608 |
| 1G1G/5ANA/CC | 30.4 (7/23) | 1.008 (0.402 to 2.526), 0.987 | 1.080 (0.385 to 3.027), 0.884 |
| 1G1G/6A6A/TX | 27.3 (3/11) | 0.864 (0.224 to 3.324), 0.831 | 0.669 (0.144 to 3.111), 0.609 |
| 1G1G/6A6A/CCb | 63 (17/27) | 3.915 (1.731 to 8.853), 0.001 | 3.579 (1.420 to 9.016), 0.007 |
Referent genotype for calculation of odds ratio in regression model, 2GnG represents 2G2G or 2G1G (n = 1 or 2).
Statistically significant, 5ANA represents 5A5A or 5A6A (n = 5 or 6), TX represents TT or TC (X = T or C).
Multivariate regression model with adjustment for location (upper arm or forearm) and side (right or left) of AVF, duration of HD, extracorporeal pump flow rate, maximal dialytic venous pressure, hypertension, and CVD.
Unassisted Patency and Relative Incidences of Failure of AVF According to MMP Genotype Polymorphisms
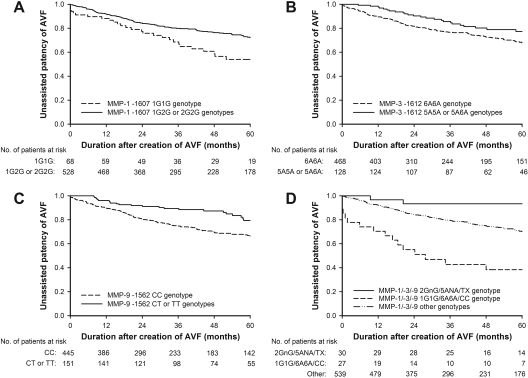
The effect of different genotypes of MMPs on AVF patency was compared in this study. As shown in Figure 2A, AVF patency differed significantly when patients were classified according to their MMP-1 −1607 genotypes. The unassisted patency of AVF at 5 years decreased significantly, from 72.2% in patients with 2G/2G or 2G/1G genotypes to 55.2% in patients with 1G/1G genotypes (P = 0.0038 by log-rank test; Figure 2A).
Figure 2.
Comparison between the survival curves of 5-year unassisted patency of AVF in HD patients with different genotypes of (A) MMP-1 −1607 1G/2G (P = 0.0038), (B) MMP-3 −1612 5A/6A (P = 0.0094), (C) MMP-9 −1562 C/T (P = 0.0205), and (D) the composite MMP-1/MMP-3/MMP-9 (P < 0.0001); n = 1 or 2, n = 5 or 6, X = C or T.
In regard to the MMP-3 −1612 genotypes, the 5-year patency of AVF decreased significantly from 77.3% in patients with 5A/5A or 5A/6A genotypes to 67.9% in patients with 6A/6A genotypes (P = 0.0094 by log-rank test; Figure 2B). As to the MMP-9 −1562 genotypes, the patency of AVF decreased significantly from 79.0% in patients with C/T or T/T genotypes to 67.1% in those with C/C genotypes (P = 0.0205 by log-rank test; Figure 2C). In terms of the composite MMP-1/MMP-3/MMP-9 genotypes, the AVF patency decreased significantly from 93.3% in patients with 2G-/5A-/T-allele-containing genotypes to 38.4% in those with 1G1G/6A6A/CC genotypes, whereas it was 70.1% for all of the other genotypes in between (P < 0.001 by log-rank test; Figure 2D). In addition, the relative incidences of AVF failure according to the genotype polymorphisms of MMPs are listed in Table 6.
Table 6.
Relative incidences of AVF failure according to MMP genotypes in HD patients
| Genotype | Total Observations (patient-months) | Episodes (times) | Episode/Patient-Months | P |
|---|---|---|---|---|
| Total | 29,727.83 | 268 | 1/110.9 | |
| MMP-1 −1607 1G/2G | ||||
| (1) 2G2G | 15,353.67 | 123 | 1/124.8 | P = 0.017 |
| (2) 2G1G | 11,340.07 | 94 | 1/120.6 | |
| (3) 1G1G | 3034.10 | 51 | 1/59.5 | |
| MMP-3 −1612 5A/6A | ||||
| (1) 5A5A | 574.93 | 3 | 1/191.6 | P = 0.226 |
| (2) 5A6A | 6194.13 | 43 | 1/144.05 | |
| (3) 6A6A | 22,958.77 | 222 | 1/103.4 | |
| MMP-9 −1562 C/T | ||||
| (1) CC | 21,862.9 | 219 | 1/99.8 | P = 0.031 |
| (2) CT | 7483.17 | 48 | 1/155.9 | |
| (3) TT | 381.77 | 1 | 1/381.8 | |
| MMP-1,-3,-9 | ||||
| (1) 1G1G/6A6A/CC | 960.2 | 34 | 1/28.2 | P < 0.001 |
| (2) 2GnG/5ANA/TXa | 1707.9 | 3 | 1/569.3 | |
| (3) other genotypes | 27,059.73 | 231 | 1/117.1 |
2GnG represents 2G2G or 2G1G (n = 1 or 2), 5ANA represents 5A5A or 5A6A (n = 5 or 6), TX represents TT or TC (X = T or C).
Discussion
In this investigation of 596 Chinese HD patients, we showed that there was a significant association between AVF failure and genotype polymorphisms of MMP-1, MMP-3, and MMP-9 as well as factors including longer HD duration, lower pump flow, higher dynamic venous pressure, presence of CVD, and location of AVF on right side and upper arm. The positive and negative predictive rates of the development of AVF failure could be increased to 63% and 93.3% in HD patients with the highest-risk and lowest-risk composite genotypes of MMP-1/MMP-3/MMP-9, respectively.
The longer HD duration could mean that the longer the patients receive HD, the higher the risk of AVF failure they may be exposed to. As to the preferable location of vascular access, usually the first native AVF will be created at the forearm of the nondominant hand. The finding that HD patients with their first fistula placed on the dominant side or upper arm could mean that they had poor vascular condition at the time of fistula creation.
The effect of MMPs on extracellular matrix degradation may be regulated at several levels, including modulation of transcription, activation of latent MMPs, and suppression of MMP activity by TIMPs.
According to the results of our study, MMP-9 SNP (−1562 C>T) T allele and T-allele-containing genotypes are associated with a lower frequency of AVF stenosis. Functional studies indicate that the −1562 C > T polymorphism has an allele-specific effect on MMP-9 transcription. In vitro experiments using reporter assay techniques indicate that the T-1562 allele has higher promoter activity in driving gene expression than the C-1562 allele (25). Similarly, Medley et al. (22) showed that MMP-9 mRNA levels, protein levels, and activity in aortic tissues were higher in T-1562 allele carriers than in noncarriers. Furthermore, Blankenberg et al. (30) showed that plasma MMP-9 levels were also higher in T-1562 allele carriers than in noncarriers. These findings suggest that the −1562 C > T polymorphism not only has an effect on MMP-9 promoter activity in in vitro experiments but also has an influence on MMP-9 transcription in vivo, and that this effect is translated into differences in MMP-9 protein level and activity between individuals of different MMP-9 genotypes.
Because many studies have demonstrated that the −1562 T-allele of MMP-9 gene is associated with a higher level of mRNA and protein expression and enzyme activity of MMP-9, our results that MMP-9 −1562 T allele and T-allele-containing genotypes are associated with a lower frequency of AVF stenosis can be explained by the following pathogenetic mechanism. In particular, the higher activity of MMP-9 may contribute to a stronger capability of degrading elastin in the internal elastic lamina, which leads to vascular dilation and an increased luminal diameter of AVFs. Thus, the progression of the above events in relation to the −1562 T-allele of the MMP-9 gene may increase access blood flow, which is associated with not only a lower frequency of vascular stenosis but also a higher patency of AVFs. The dilation of AVF is quite similar to the formation of aneurismal dilation of abdominal aorta, which has also been demonstrated to be associated with the MMP-9 SNP (−1562 C>T) T allele and T-allele-containing genotypes by Jones et al. (24). They studied the MMP-9 −1562 C > T polymorphism in patients with abdominal aortic aneurysm and healthy controls and found that the frequency of the T-1562 allele-bearing genotypes was significantly higher in the case group than in the control group (24). The development and rupture of aneurysms involve degradation of vascular structural proteins including collagens and elastin. Elastinolysis is particularly pertinent to vessel dilation, whereas collagenolysis plays a more important role in aneurysmal rupture (31). MMP-9 expression is increased in abdominal aortic aneurysmal tissues compared with normal blood vessels, and the development of experimental abdominal aortic aneurysms is suppressed in MMP-9 knockout animals (31).
The most studied polymorphism of the MMP-3 gene is the −1612 5A >6A variant. In experiments testing promoter activity by reporter gene assay, the promoter with the 5A allele was associated with greater gene expression than that with the 6A allele (32). This finding has been noted in several cell types, including smooth muscle cells, macrophages, and fibroblasts. According to Lichtinghagen et al. (33), the levels of MMP-3 mRNA and protein in vascular tissues were lowest in 6A/6A homozygotes, intermediate in 5A/6A heterozygotes, and highest in 5A/5A homozygotes. This difference comes from the more effective binding of NFκB p50/p50 dimer to the 6A allele than to the 5A allele. The NFκB p50 homodimer has been shown to function as a transcriptional repressor for several genes (34). Thus, this indicates that the higher promoter activity of the 5A allele is a result of reduced binding of the transcriptional repressor p50/p50 to the 5A allele compared with the 6A allele.
In terms of the polymorphisms of the MMP-1 gene, Rutter et al. have shown that the −1607 1G >2G polymorphism has an effect on the binding of an Ets transcription factor (7). The promoter containing 2G had a higher activity in driving gene expression than that with 1G. This MMP-1 gene polymorphism has been reported to be associated with CAD. Patients with the 2G/2G genotype had a 50% lower risk of coronary heart disease compared with those homozygous for the less transcriptionally active 1G allele (9).
Interestingly, we found that a higher frequency of AVF failure is associated with lower transcription activity-related genotype polymorphisms of MMPs including the 1G/1G genotype of the MMP-1 −1607 1G >2G variant, 6A/6A genotype of the MMP-3 −1612 5A >6A variant, and the C/C genotype of the MMP-9 −1562 C>T SNP. The pathogenetic mechanisms of this association may be explained as follows. The HD patients with these specific genotype polymorphisms that possess lower transcriptional activity of MMP-1, MMP-3, and MMP-9 promoters may be more susceptible to the intravascular accumulation of extracellular matrix, the deposition of which may lead to the narrowing of the luminal diameter (stenosis) of AVF, which consequently decreases the access blood flow of AVF, thus causing a higher frequency of AVF failure.
Some limitations should be considered in our study. First, the study population was mainly composed of Chinese, thus the results may or may not apply to other ethnic groups. Second, the association may not be present for other types of vascular access, such as arteriovenous graft, because our result comes from patients with AVF. Third, a selection bias might exist because this study is based on a retrospective observational cohort study. Only those who survived at the time of study enrollment had the opportunity to be selected and of receiving venous sampling; all those who had dropped out from maintenance HD treatment would be excluded from this study. The selection bias may be avoided by conducting a randomized prospective cohort study. However, there were still 27 of the 62 patients with AVF malfunction receiving interventional procedure on account of access flow lower than 500 ml/min, which is a good indicator of stenosis of AVF. Future study should be conducted to explore whether preemptive intervention of hemodynamically significant stenosis according to access flow measurement will improve the patency of AVF in HD patients, especially in those carrying specific genotype polymorphisms of MMPs that predict higher risk of AVF failure. Nevertheless, several strengths could be found in this study. First, we determined genotype polymorphisms of multiple MMP and TIMP genes related by similar biologic pathways. Thus, the respective roles of specific genes and gene-gene interactions on AVF patency could be clarified. Second, this study helps us identify some composite genotype polymorphisms of MMPs as specific markers for early identification of patients with different risks of AVF failure, thus enabling a large-scale screening of high-risk patients. Third, in terms of the stability of laboratory examination for MMPs, the constancy of genotype is superior to the fluctuation of serum concentration determined by ELISA kits, which may be influenced by many factors (e.g., diet, inflammation, oxidative stress, hemodynamic instability, and different settings of dialysis therapy).
In conclusion, for the first time, we demonstrated in this study that specific genotypes of MMP-1, MMP-3, and MMP-9 with lower transcriptional activity are associated with higher frequency of AVF failure. The lower activity of MMPs may result in more extensive accumulation of intravascular extracellular matrix, leading to the progressive narrowing of the vascular lumen and a higher risk of AVF stenosis. Recently, there has been increasing evidence that genetic background may explain at least part of the excessive risk for AVF failure observed in HD patients. AVF failure still remains a major clinical problem, although the programs for regular monitoring and surveillance of AVF are encouraged. Thus, more prospective studies are needed to confirm our results and investigate whether pharmacologic or physical-therapeutic regulation of MMP activity will improve AVF patency for HD patients with specific genetic backgrounds.
Disclosures
None.
Acknowledgments
This work was supported by grants from the Ministry of Education, the Aim for the Top University Plan (National Yang-Ming University 97A-C-T193, 98A-C-T193), an intramural grant (V96B2-009), and grants for the Integrated Genome Project (V96ER2-004, V97ER2-006) from Taipei Veterans General Hospital and the National Science Council (NSC97-2314-B-010 to 010-MY3) in Taiwan. This abstract will be presented at the XLVII ERA-EDTA congress in Munich, Germany on June 25 through 28, 2010.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Windus DW: Permanent vascular access: A nephrologist's view. Am J Kidney Dis 21: 457–471, 1993 [DOI] [PubMed] [Google Scholar]
- 2.Weiss MF, Scivittaro V, Anderson JM: Oxidative stress and increased expression of growth factors in lesions of failed hemodialysis access. Am J Kidney Dis 37: 970–980, 2001 [DOI] [PubMed] [Google Scholar]
- 3.Abularrage CJ, Sidawy AN, Weiswasser JM, White PW, Arora S: Medical factors affecting patency of arteriovenous access. Semin Vasc Surg 17: 25–31, 2004 [DOI] [PubMed] [Google Scholar]
- 4.Visse R, Nagase H: Matrix metalloproteinases and tissue inhibitors of metalloproteinases: Structure, function, and biochemistry. Circ Res 92: 827–839, 2003 [DOI] [PubMed] [Google Scholar]
- 5.Sternlicht MD, Werb Z: How matrix metalloproteinases regulate cell behavior. Annu Rev Cell Dev Biol 17: 463–516, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Newby AC: Dual role of matrix metalloproteinases (matrixins) in intimal thickening and atherosclerotic plaque rupture. Physiol Rev 85: 1–31, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Rutter JL, Mitchell TI, Buttice G, Meyers J, Gusella JF, Ozelius LJ, Brinckerhoff CE: A single nucleotide polymorphism in the matrix metalloproteinase-1 promoter creates an Ets binding site and augments transcription. Cancer Res 58: 5321–5325, 1998 [PubMed] [Google Scholar]
- 8.Ranganathan AC, Nelson KK, Rodriguez AM, Kim KH, Tower GB, Rutter JL, Brinckerhoff CE, Huang TT, Epstein CJ, Jeffrey JJ, Melendez JA: Manganese superoxide dismutase signals matrix metalloproteinase expression via H2O2-dependent ERK1/2 activation. J Biol Chem 276: 14264–14270, 2001 [DOI] [PubMed] [Google Scholar]
- 9.Ye S, Gale CR, Martyn CN: Variation in the matrix metalloproteinase-1 gene and risk of coronary heart disease. Eur Heart J 24: 1668–1671, 2003 [DOI] [PubMed] [Google Scholar]
- 10.Vasku A, Goldbergova M, Izakovicova Holla L, Siskova L, Groch L, Beranek M, Tschoplova S, Znojil V, Vacha J: A haplotype constituted of four MMP-2 promoter polymorphisms (−1575G/A, −1306C/T, −790T/G and −735C/T) is associated with coronary triple-vessel disease. Matrix Biol 22: 585–591, 2004 [DOI] [PubMed] [Google Scholar]
- 11.Schwarz A, Haberbosch W, Tillmanns H, Gardemann A: The stromelysin-1 5A/6A promoter polymorphism is a disease marker for the extent of coronary heart disease. Dis Markers 18: 121–128, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hirashiki A, Yamada Y, Murase Y, Suzuki Y, Kataoka H, Morimoto Y, Tajika T, Murohara T, Yokota M: Association of gene polymorphisms with coronary artery disease in low- or high-risk subjects defined by conventional risk factors. J Am Coll Cardiol 42: 1429–1437, 2003 [DOI] [PubMed] [Google Scholar]
- 13.Terashima M, Akita H, Kanazawa K, Inoue N, Yamada S, Ito K, Matsuda Y, Takai E, Iwai C, Kurogane H, Yoshida Y, Yokoyama M: Stromelysin promoter 5A/6A polymorphism is associated with acute myocardial infarction. Circulation 99: 2717–2719, 1999 [DOI] [PubMed] [Google Scholar]
- 14.Zhou X, Huang J, Chen J, Su S, Chen R, Gu D: Haplotype analysis of the matrix metalloproteinase 3 gene and myocardial infarction in a Chinese Han population. The Beijing atherosclerosis study. Thromb Haemost 92: 867–873, 2004 [DOI] [PubMed] [Google Scholar]
- 15.Lamblin N, Bauters C, Hermant X, Lablanche JM, Helbecque N, Amouyel P: Polymorphisms in the promoter regions of MMP-2, MMP-3, MMP-9, and MMP-12 genes as determinants of aneurysmal coronary artery disease. J Am Coll Cardiol 40: 43–48, 2002 [DOI] [PubMed] [Google Scholar]
- 16.Humphries SE, Martin S, Cooper J, Miller G: Interaction between smoking and the stromelysin-1 (MMP3) gene 5A/6A promoter polymorphism and risk of coronary heart disease in healthy men. Ann Hum Genet 66: 343–352, 2002 [DOI] [PubMed] [Google Scholar]
- 17.de Maat MP, Jukema JW, Ye S, Zwinderman AH, Moghaddam PH, Beekman M, Kastelein JJ, van Boven AJ, Bruschke AV, Humphries SE, Kluft C, Henney AM: Effect of the stromelysin-1 promoter on efficacy of pravastatin in coronary atherosclerosis and restenosis. Am J Cardiol 83: 852–856, 1999 [DOI] [PubMed] [Google Scholar]
- 18.Gnasso A, Motti C, Irace C, Carallo C, Liberatoscioli L, Bernardini S, Massoud R, Mattioli PL, Federici G, Cortese C: Genetic variation in human stromelysin gene promoter and common carotid geometry in healthy male subjects. Arterioscler Thromb Vasc Biol 20: 1600–1605, 2000 [DOI] [PubMed] [Google Scholar]
- 19.Ghilardi G, Biondi ML, DeMonti M, Turri O, Guagnellini E, Scorza R: Matrix metalloproteinase-1 and matrix metalloproteinase-3 gene promoter polymorphisms are associated with carotid artery stenosis. Stroke 33: 2408–2412, 2002 [DOI] [PubMed] [Google Scholar]
- 20.Flex A, Gaetani E, Papaleo P, Straface G, Proia AS, Pecorini G, Tondi P, Pola P, Pola R: Proinflammatory genetic profiles in subjects with history of ischemic stroke. Stroke 35: 2270–2275, 2004 [DOI] [PubMed] [Google Scholar]
- 21.Beilby JP, Chapman CM, Palmer LJ, McQuillan BM, Thompson PL, Hung J: Stromelysin-1 (MMP-3) gene 5A/6A promoter polymorphism is associated with blood pressure in a community population. J Hypertens 23: 537–542, 2005 [DOI] [PubMed] [Google Scholar]
- 22.Medley TL, Cole TJ, Dart AM, Gatzka CD, Kingwell BA: Matrix metalloproteinase-9 genotype influences large artery stiffness through effects on aortic gene and protein expression. Arterioscler Thromb Vasc Biol 24: 1479–1484, 2004 [DOI] [PubMed] [Google Scholar]
- 23.Peters DG, Kassam A, St Jean PL, Yonas H, Ferrell RE: Functional polymorphism in the matrix metalloproteinase-9 promoter as a potential risk factor for intracranial aneurysm. Stroke 30: 2612–2616, 1999 [DOI] [PubMed] [Google Scholar]
- 24.Jones GT, Phillips VL, Harris EL, Rossaak JI, van Rij AM: Functional matrix metalloproteinase-9 polymorphism (C-1562T) associated with abdominal aortic aneurysm. J Vasc Surg 38: 1363–1367, 2003 [DOI] [PubMed] [Google Scholar]
- 25.Zhang B, Ye S, Herrmann SM, Eriksson P, de Maat M, Evans A, Arveiler D, Luc G, Cambien F, Hamsten A, Watkins H, Henney AM: Functional polymorphism in the regulatory region of gelatinase B gene in relation to severity of coronary atherosclerosis. Circulation 99: 1788–1794, 1999 [DOI] [PubMed] [Google Scholar]
- 26.Morgan AR, Zhang B, Tapper W, Collins A, Ye S: Haplotypic analysis of the MMP-9 gene in relation to coronary artery disease. J Mol Med 81: 321–326, 2003 [DOI] [PubMed] [Google Scholar]
- 27.Heine GH, Ulrich C, Sester U, Sester M, Kohler H, Girndt M: Transforming growth factor beta1 genotype polymorphisms determine AV fistula patency in hemodialysis patients. Kidney Int 64: 1101–1107, 2003 [DOI] [PubMed] [Google Scholar]
- 28.Fukasawa M, Matsushita K, Kamiyama M, Mikami Y, Araki I, Yamagata Z, Takeda M: The methylentetrahydrofolate reductase C677T point mutation is a risk factor for vascular access thrombosis in hemodialysis patients. Am J Kidney Dis 41: 637–642, 2003 [DOI] [PubMed] [Google Scholar]
- 29.Lin CC, Yang WC, Lin SJ, Chen TW, Lee WS, Chang CF, Lee PC, Lee SD, Su TS, Fann CS, Chung MY: Length polymorphism in heme oxygenase-1 is associated with arteriovenous fistula patency in hemodialysis patients. Kidney Int 69: 165–172, 2006 [DOI] [PubMed] [Google Scholar]
- 30.Blankenberg S, Rupprecht HJ, Poirier O, Bickel C, Smieja M, Hafner G, Meyer J, Cambien F, Tiret L: Plasma concentrations and genetic variation of matrix metalloproteinase 9 and prognosis of patients with cardiovascular disease. Circulation 107: 1579–1585, 2003 [DOI] [PubMed] [Google Scholar]
- 31.Pyo R, Lee JK, Shipley JM, Curci JA, Mao D, Ziporin SJ, Ennis TL, Shapiro SD, Senior RM, Thompson RW: Targeted gene disruption of matrix metalloproteinase-9 (gelatinase B) suppresses development of experimental abdominal aortic aneurysms. J Clin Invest 105: 1641–1649, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ye S, Eriksson P, Hamsten A, Kurkinen M, Humphries SE, Henney AM: Progression of coronary atherosclerosis is associated with a common genetic variant of the human stromelysin-1 promoter which results in reduced gene expression. J Biol Chem 271: 13055–13060, 1996 [DOI] [PubMed] [Google Scholar]
- 33.Lichtinghagen R, Bahr MJ, Wehmeier M, Michels D, Haberkorn CI, Arndt B, Flemming P, Manns MP, Boeker KH: Expression and coordinated regulation of matrix metalloproteinases in chronic hepatitis C and hepatitis C virus-induced liver cirrhosis. Clin Sci (Lond) 105: 373–382, 2003 [DOI] [PubMed] [Google Scholar]
- 34.Udalova IA, Richardson A, Denys A, Smith C, Ackerman H, Foxwell B, Kwiatkowski D: Functional consequences of a polymorphism affecting NF-κB p50–p50 binding to the TNF promoter region. Mol Cell Biol 20: 9113–9119, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]