Abstract
To illustrate the implementation of a bottom-up approach to the study of culture in health disparities, this article describes the development of a cultural cancer screening scale (CCSS) using mixed methodologies. The aim was to identify cultural factors relevant to breast and cervical cancer screening, develop an instrument to assess them and examine its preliminary psychometric properties among Latin American (Latino) and non-Latino White (Anglo) women in Southern California. Seventy-eight Latino and Anglo women participated in semi-structured interviews, which were content coded based on Triandis' methods for the analysis of subjective culture. Based on the emerging cultural elements, items relevant to cancer screening were developed and pilot tested with 161 participants. After the instrument was refined, 314 Latino and Anglo women from various socioeconomic backgrounds completed the CCSS and data were factor analyzed resulting in five cultural factors: cancer screening fatalism, negative beliefs about health professionals, catastrophic disease expectations, symptomatic deterrents and sociocultural deterrents. The instrument demonstrated measurement equivalence, adequate reliability and predictive validity. The research and the CCSS are discussed in terms of implications for the study of culture in relation to health disparities and the development of evidence-based interventions with culturally diverse populations and their health professionals.
Introduction
Research evidence suggests that increasing cancer screening behaviors significantly improves cancer outcomes and lowers mortality rates [1]. Although cancer screening rates in the United States have improved over the past decade, rates for minority populations have improved to a much lesser degree as compared with the Anglo population. For instance, according to data from 1992, rates of mammography (MAM) screening for Anglo and Latino women in the United States were 58 and 55%, respectively. In 2005, the rates were ∼68% for Anglo and 59% for Latino women [2]. These findings represent a 3-fold increase in the screening disparity between the two ethnic groups (from 3 to 9 percentage points) in just over a decade. Although screening rates for cervical cancer are higher than for breast cancer, compared with Anglo American (79%) and African American women (80%), Latino American women (74%) are the least likely to have had a recent Pap test (Pap).
Research has identified a number of factors associated with ethnic disparities in breast and cervical cancer screening. These include income, health insurance status, English proficiency [3], access to transportation [4], education [5], social support [6, 7], acculturation [5, 8] and health care discrimination [9]. These and related findings suggest that health disparities may be in part a function of cultural differences between the health care professionals and the culturally diverse patients they serve [10, 11]. This is particularly important as the US population is becoming increasingly diverse while our health care system, policies and interventions remain predominantly based on traditional Anglo American cultural assumptions [12].
If cultural differences play a role in cancer screening behavior, the cultural elements relevant to screening need to be identified, properly measured and their role in cancer screening should be tested in a culturally diverse population [10–11]. Once psychometrically appropriate instruments have been developed, the cultural variables relevant to cancer screening can be assessed among women from the community targeted for intervention. Then, the obtained cultural data can inform evidence-based targeted or tailored interventions with individuals from that community. Such interventions are likely to be more effective at increasing cancer screening behaviors than interventions based on stereotypical or more general views of ethnic or socioeconomic groups. This is particularly likely to be the case as these groups are increasingly heterogeneous in terms of sources of cultural variation such as country or region of origin, generation status, education, income, acculturation and intercultural contact.
The purpose of this article was to illustrate the implementation of a bottom-up approach to the development of cultural instruments. The corresponding aims of the research were 3-fold: (i) to identify cultural factors relevant to breast and cervical cancer screening among Latino as compared with Anglo women in Southern California, (ii) to develop an instrument relevant to both Latino and Anglo women to assess these cultural factors and (iii) to perform a preliminary test of the psychometric properties of the newly developed cultural instrument. The research was guided by Betancourt's theoretical model for the study of culture in psychology [11, 13, 14], which has been recently applied to the study of health behavior in culturally diverse populations [10].
The study of culture and health behavior
One of the problems observed in the health sciences literature is the lack of clarity concerning the definition of culture. In fact, culture has been defined in many different ways, depending on the focus and conceptual orientation of the author. For instance, Rohner [15] has provided a socially based definition of culture as a learned system of meanings that is shared by a people or an identifiable segment of the population. Others [16, 17] have defined culture as the human-made part of the environment that includes both objective and subjective components. Objective culture refers to elements such as roads, bridges, tools and technology whereas subjective culture refers to norms, roles, beliefs, values and practices. These elements of subjective culture are the basis of how a number of cultural psychologists and health science researchers conceptualize culture as they are more directly related to psychological processes and behavior [see 13,18–20]. In fact, medical anthropologists Hruschka and Hadley [20] argue that when culture is defined in terms of socially learned norms, values and behaviors, it is possible to empirically investigate its influence on health.
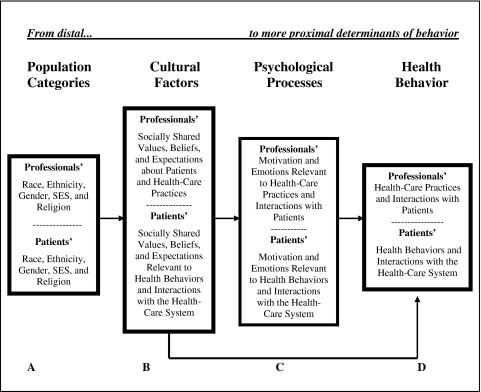
From a health sciences perspective, culture should be conceptualized in terms that are relevant to health phenomena. Consistent with this, culture is defined here in terms of elements such as socially shared values, beliefs, norms, expectations and practices that are relevant to health behavior and outcome [10]. According to this definition, which is consistent with the model guiding this research, aspects of culture are likely to be shared among individuals of an ethnic, racial, socioeconomic status (SES) or gender group. However, such population categories are conceived to be clearly different from culture. For instance, race is generally defined in terms of physical characteristics such as skin color, facial features or hair type [13]. However, these classifications are arbitrary and have been considered problematic and of little relevance to the study of behavior [13, 21–23]. Ethnicity, on the other hand, is usually defined in terms of a common history, nationality, language and culture [13]. Hence, as observed in Fig. 1, ethnicity, race, SES or religion and other population categories are sources of cultural variation, which relate to health behavior through culture and psychological processes.
Fig. 1.
Betancourt's model of culture, psychological processes and behavior adapted for the study of health behavior [10].
Qualitative studies with Latinos have already identified a number of cultural factors relevant to cancer screening. For instance, Chavez et al. [24] have identified fatalistic beliefs. Other researchers [25] have identified the belief that if nothing is wrong, there is no need to screen, and still others [26] have identified beliefs regarding health care professionals as deterrents to cancer screening. These studies represent an important step forward in working with culturally diverse populations. In fact, recent research has developed instruments to assess some of these cultural beliefs relevant to breast cancer screening among Latino women [27]. From a health disparities perspective, research and intervention would greatly benefit from the development of additional cultural instruments designed to assess these aspects of culture relevant to both mainstream (e.g. Anglo) and minority (e.g. Latino) populations. Once instruments are developed for both populations, hypotheses can be tested and evidence-based interventions can be developed to address disparities in breast and cervical cancer screening.
Cultural instruments, such as the one reported here, are expected to be useful for testing the relations among specific cultural factors and other variables included in the model guiding the research. For example, if research with Latino women identifies cancer fatalism as a cultural factor relevant to breast cancer screening, a cultural instrument could then be developed and used to test the influence of cancer fatalism (column B of Fig. 1) on cancer screening (column D), directly and/or indirectly through psychological processes (column C). The cultural instrument could also be used to examine which population categories (e.g. ethnicity or SES in column A) exert a greater influence as a source of variation in cancer fatalism (column B) or whether the influence of cancer fatalism is the same for individuals of different SES or ethnic groups. Such a cultural instrument could be particularly useful in the development of intervention programs ‘targeted’ for a specific culturally diverse community or ‘tailored’ to individuals of that community [28]. Still, when such measures are used to assess cultural factors among individuals of different ethnic or cultural backgrounds, it is crucial that measurement equivalence is established [29]. This is important to ensure that instruments measure the same underlying factors for each cultural group [29, 30].
The development of the cultural cancer screening scale
Triandis' methods for the study of subjective culture [31] and Betancourt's model and bottom-up approach for the study of culture [10, 11, 14] guided all phases of the mixed methods research. The bottom-up approach begins with specific observations relevant to an area of research (e.g. cancer screening), which are derived from the population(s) of interest (e.g. ethnic or SES group) [10]. This approach evolves from observations to the development of instruments, to testing hypotheses employing the newly developed cultural instrument. To this end, mixed methodologies are used to implement the bottom-up approach.
An advantage of the bottom-up approach is that aspects of culture specifically relevant to cancer screening can be identified directly from the individuals, rather than based on stereotypical views that may ignore within-group differences [10]. An additional advantage of this approach is that the resulting instrument developed for use with minority (e.g. Latino) and mainstream (e.g. Anglo) populations are more likely to demonstrate measurement equivalence. Often times, instruments intended for Anglo American populations are simply translated for other ethnic groups without establishing measurement equivalence. Such research fails to ensure that instruments measure the same underlying factors for each cultural group prior to testing hypotheses concerning cultural differences [29, 30].
In Phase I, open-ended, semi-structured interviews were conducted with Latino and Anglo women to identify cultural factors associated with breast and cervical cancer screening. In Phase II, close-ended items were developed based on the emerging cultural elements identified in Phase I. Then, an instrument was compiled with these items, which was pilot tested with a sample of Latino and Anglo women and further refined. In Phase III, the instrument underwent preliminary psychometric testing with a larger sample to examine the structure, reliability, predictive validity and measurement equivalence of the cultural cancer screening scale (CCSS).
Phase I: identification of cultural elements
Sampling procedures
Standard procedures for the study of culture as defined by Triandis et al. [31] involves the inclusion of a comparison group in order to identify elements of culture that are unique to a particular group (Latino), those that are unique to the mainstream (Anglo) group or those that are common to all participants. In accordance with these procedures, monolingual English and English–Spanish bilingual experimenters interviewed 78 self-identified Latino and Anglo American women.
According to the model for the study of culture, psychological processes and health behavior (see Fig. 1), population categories such as ethnicity, education and income transmit culture and are sources of cultural variation. From this perspective, sampling procedures associated with the bottom-up approach must recognize the critical importance of recruiting individuals from various demographic backgrounds. Since the interview responses are expected to provide the basis for the cultural elements represented in the cultural instrument, failing to interview individuals from various demographic backgrounds will result in a limited perspective concerning the most relevant cultural elements associated with cancer screening.
In accordance with this perspective, multi-stage, stratified sampling was conducted in order to obtain nearly equal proportions of Latino and Anglo women of varying demographic characteristics. To ensure demographic diversity, participants were recruited from various settings including markets, churches, universities, free-/low-cost health clinics, mobile home parks and community settings. Using US Census tract data from the Federal Financial Institutions Examination Council, projections regarding ethnicity, SES and age were anticipated for each recruitment setting prior to data collection. Once data were collected from a number of sites, the distribution of participants across demographic criteria was examined. Based on these analyses, efforts were made to recruit participants that would provide nearly equal proportions of individuals within the different strata.
Development of interview schedule
A semi-structured interview schedule was developed based on Triandis' methods for the study of subjective culture, in a manner similar to applications to health behavior [32]. In accordance with the definition of culture outlined in the model (see Fig. 1), open-ended questions were developed to obtain information concerning cultural aspects such as socially shared beliefs, norms and expectations concerning breast and cervical cancer screening behaviors, including their antecedents and consequences. An example of a question designed to identify socially shared beliefs regarding the causes for cancer screening included, ‘Why do you think some women choose to have a mammogram?’ A sample question designed to identify socially shared expectations included, ‘What do you think happens to women who do not have regular Pap tests?’
Identification of cultural elements
One of the key components of the bottom-up approach is that observations are made directly from the population of interest. This approach provides valuable contextual and linguistic information that can be used for the development of items relevant to the emerging cultural elements and is more likely to produce psychometrically sound instruments that ensure measurement equivalence [33]. To this end, all interviews were transcribed and coded in their original language by a group of monolingual English and bilingual Spanish–English-speaking judges using standard content analysis procedures.
Frequency distributions were calculated for Latino and Anglo women separately based on the identified cultural elements. Results revealed distinct cultural elements relevant to breast and cervical cancer screening. These included socially shared beliefs about cancer in general, symptoms, systematic barriers to screening, fatalistic avoidance and beliefs relevant to health care professionals who perform screening examinations. Some of the cultural aspects were reported as relevant by Latino women but were not reported by Anglo women (e.g. Latino-specific cultural belief). At the same time, some elements were identified as culturally specific to Anglo women (e.g. Anglo-specific cultural belief), whereas others were shared by both ethnic groups (e.g. ethnic-general cultural belief).
Phase II: item development and pilot test of cultural elements emerging from Phase I
Item development and translation
Based on the most frequently reported ethnic-specific and ethnic-general cultural themes that emerged from the content analysis of the Phase I interviews, dichotomous and 7-point Likert Scale items were developed to assess these cultural aspects in relation to clinical breast examinations (CBE), MAM and Pap. To ensure scale equivalence, the items were constructed in the language of the interview from which it emerged in Phase I. In fact, many of the items were developed using the exact terminology and language that women used during their interviews.
Since most of the cultural elements identified in Phase I were relevant to both breast and cervical cancer screening, 60 similarly worded items were developed for the breast and cervical cancer sections of the instrument, respectively. Items were then translated into the other language by a group of bilingual Spanish–English-speaking experts through the double back-translation procedure to eliminate parochial wording [33, 34]. The translation process occurred side by side to compare the English and Spanish versions for appropriateness and equivalence. Although efforts were made to preserve participants' language, a decentering process was also employed, which views both languages as equally important and equally open to modification [35]. A final blind back-translation process was also employed in which a translator not familiar with the original version of the instrument translated it back into the original language [36].
Instrument administration and refinement
A total of 161 Latino and Anglo women were administered the pilot version of the CCSS in a group setting by monolingual English and bilingual English–Spanish-speaking research assistants. When participants were finished, they met one-on-one with a research assistant to provide feedback concerning the instrument. Based on participants' feedback and preliminary statistical analyses, 22 items were eliminated. The remaining items were factor analyzed revealing a number of similar factors relevant to both breast and cervical cancer screening. Internal consistency was adequate and several factors were correlated with breast and cervical cancer screening behaviors.
Prior to testing the CCSS with a larger sample in Phase III, some items were further refined for proper language and dichotomous items were transformed into 7-point Likert scale items to be consistent with the response format for the overall instrument. As a result, each section of the instrument was reduced to 38 items representing the cultural elements identified through the bottom-up approach.
Phase III: preliminary psychometric validation
Methods
Two propositions were tested in Phase III using the CCSS: (i) Latino and Anglo women were expected to score differently on the emerging cultural factors. (ii) The CCSS was expected to demonstrate predictive validity with breast and cervical cancer screening behaviors and related psychological processes such as screening emotions.
Participants
As in Phases I and II, multi-stage, stratified sampling was conducted to obtain nearly equal proportions of participants from varying demographic characteristics (e.g. ethnicity, SES, age). Based on the recommendation that the number of participants for factor analysis should be five times the number of variables [37, 38], the sample of 314 participants (167 Latino, 147 Anglo) is considered sufficient. All women were 21 years of age and older who had never been diagnosed with breast or cervical cancer. Of these participants, 158 (84 Latino, 74 Anglo) were administered the breast cancer version of the instrument while 156 (83 Latino, 73 Anglo) responded to the cervical cancer version (see Table I).
Table I.
Demographics for Phase III sample
| Latinos, n = 165 | Anglos, n = 149 | Total, n = 314 | |
| Age (mean)* | 41.19 | 47.98 | 44.39 |
| Education (mean)* | 12.75 | 14.82 | 13.73 |
| Income (%)* | |||
| 0–14 999 | 21.70 | 17.60 | 19.70 |
| 15 000–24 999 | 14.50 | 10.80 | 12.70 |
| 25 000–39 999 | 17.50 | 16.90 | 17.20 |
| 40 000–59 999 | 13.90 | 14.90 | 14.30 |
| >60 000 | 22.90 | 39.20 | 30.60 |
| Missing | 9.60 | 0.70 | 5.40 |
| Marital status (%) | |||
| Single | 19.30 | 15.50 | 17.50 |
| Married | 55.40 | 54.70 | 55.10 |
| Cohabitating | 4.20 | 2.00 | 3.20 |
| Divorced/separated | 16.30 | 17.60 | 16.90 |
| Widowed | 4.20 | 10.10 | 7.0 |
| Missing | 0.60 | 0.30 | |
| Foreign born (%)* | 41.6 | 4.1 | |
| Mexico | 85 | ||
| Puerto Rico | 2.9 | ||
| Central America | 7.3 | ||
| Cuba | 0.7 | ||
| South America | 2.2 | ||
| Other: Latin America | 1.5 | ||
| Europe | 2.70 | ||
| Canada | 1.40 | ||
| Insurance status (%)* | |||
| Yes | 72.30 | 89.90 | 80.60 |
| Missing | 6.0 | 2.70 | 4.50 |
| Survey language (%)* | |||
| English | 73.50 | 100.00 | 86.0 |
| Spanish | 26.50 | 14.0 |
*P < 0.05.
Measures
A questionnaire was compiled including a refined version of the CCSS in addition to measures designed to test the scale's predictive validity. To this end, a cancer screening measure was included to assess past breast and cervical cancer screening behaviors and intention to screen in the future. Consistent with the conceptual model guiding the research (see Fig. 1), measures of psychological variables such as emotions associated with cancer screening were also included to further test the predictive validity of the CCSS.
Demographics.
Items relevant to participants' age, education, ethnicity, income, marital status, immigration status and insurance status were assessed.
Cultural cancer screening scale.
Since similar factors emerged as relevant to both breast and cervical cancer screening in Phase II, the instrument for this phase included a total of 38 similarly worded items in each section of the CCSS. The main differences between the sections of the instrument were the wording of items and/or instructions specific to the type of screening behavior (e.g. MAM, CBE, Pap). For instance, an item from the factor ‘catastrophic disease expectations’ was worded ‘Breast cancer (cervical cancer) is the worst thing that can happen to a woman’. Since several items from the two sections are worded similarly, participants completed either the breast cancer screening or the cervical cancer screening version of the CCSS to avoid response bias and fatigue.
Cancer screening behaviors.
Participants were provided an illustration of a woman having a MAM, CBE or Pap followed by a brief description of the corresponding test. Participants were then asked the question ‘Have you ever had a MAM (CBE or Pap, respectively)?’ followed by ‘If yes, how many have you had in the last five years?’. A compliance proportion score was computed based on age recommendations for each screening exam as outlined by the American Cancer Society [39]. Using methods similar to those employed by Kundadjie-Gyamfi and Magai [40], the screening compliance score for each type of screening exam was calculated for participants based on the total number of MAM/CBE/Paps reported divided by the maximum number of tests a woman of her age should have if they were fully compliant with screening guidelines (maximum compliance = 1.0). To assess intention to screen, participants were asked ‘In the next year, how likely are you to have a MAM (CBE/Pap)?’. Response options were based on a 7-point Likert scale from ‘not at all’ to ‘very likely’.
Screening emotions.
During the qualitative phase of this research, participants were also asked if they experienced any emotions when they thought about breast or cervical cancer screening. The content analysis revealed that fear and anxiety were the predominant emotions experienced by both Latino and Anglo women. Therefore, six items were developed to assess the extent to which participants experienced fear and anxiety in anticipation of having a MAM, CBE and Pap, respectively. A sample item includes ‘Thinking about having a mammogram (CBE, Pap) makes me extremely anxious’. Items were based on a 7-point Likert scale from ‘strongly disagree’ to ‘strongly agree’. The following represent the scale reliabilities, CBE emotions: Latino α = 0.94, Anglo α = 0.89 and total α = 0.92; MAM emotions: Latino α = 0.89, Anglo α = 0.89 and total α = 0.90; and Pap emotions: Latino α = 0.84, Anglo α = 0.71 and total α = 0.80.
Procedure
The study was conducted at a university in Southern California and Institutional Review Board approval was granted prior to data collection. Advertisements were placed at recruitment settings indicating a specific time and place where interested women could go to fill out the questionnaire. At the time of participation, participants were met by a bilingual research assistant who explained the study. Participants who met the study inclusion criteria and were willing to participate were provided with a written consent form to sign. Participants were then given an English or Spanish version of the questionnaire, which took ∼30 min to complete. All participants were given $20 in cash as compensation for their participation.
Results
Preliminary analyses were conducted to determine if it was appropriate to collapse the two sections (e.g. breast and cervical cancer) of the CCSS for psychometric analyses. An examination of the demographic background of the samples revealed that there were no significant demographic differences, other than age, which was expected as a result of efforts to recruit a larger number of women >40 years to complete the breast cancer section. Also, there were no significant differences in the mean scores of items from the breast cancer section as compared with the cervical cancer section. These results suggest that items from each section of the instrument functioned similarly. Furthermore, principal axis exploratory factor analysis with Oblimin rotation and Kaiser normalization revealed similar factors for the breast and cervical cancer sections. Last, t-tests revealed that the mean score for each factor from the breast cancer section was not significantly different from the mean score on the corresponding factor for the cervical cancer section.
Based on results from the analyses reported above, data from the two sections of the instrument were collapsed. Hence, all analyses were conducted using the total sample of 314 women who responded to one or the other screening section of the instrument. As a result of multi-staged stratified sampling, this sample was well-balanced between Latino (n = 165) and Anglo (n = 149) participants. Furthermore, Latino and Anglo women were represented across all levels of income, education and age, respectively. Still, within the corresponding strata Latino women were overall younger, of lower income and education and more likely to be uninsured than their Anglo counterparts (see Table I).
Based on the sample of 314 women, principal axis factor analysis with Oblimin rotation and Kaiser normalization was conducted for each ethnic group separately, as well as for the total sample. Conceptual meaning in addition to the examination of scree plots were used to determine the number of factors for the CCSS. A cutoff of 0.30–0.40 and conceptual consistency of the item with the factor were used as guidelines for item inclusion.
Results revealed five distinct cultural factors, which are reported in Table II. Factor loadings from the pattern matrix are reported for Latino women, Anglo women and the total sample. The solution resulted in a matrix with simple structure, and the structure was consistent across the two groups. Total variance recaptured by the solution was 65.11% for the Latino sample, 62.84% for the Anglo sample and 62.55% for the total sample. The rotated eigen values (5.63, 2.49, 1.90, 1.61 & 1.40 for Latino; 4.94, 2.66, 1.23, 2.15 & 1.59 for Anglo and 5.21, 2.55, 1.89, 1.46 & 1.40 for the total sample) suggested a good balance of factor influence, consistent with the number of items in each factor.
Table II.
Factor loadings for Latinos/Anglos/total
| 1 | 2 | 3 | 4 | 5 | |
| Sociocultural deterrents | |||||
| Having problems making an appointment is a reason for not screening regularly. | 0.84/0.70/0.77 | −0.004/0.01/0.01 | −0.002/0.07/0.02 | −0.07/0.02/−0.04 | 0.09/−0.004/0.03 |
| Not knowing where I can be screened for breast/cervical cancer is a reason for not screening regularly. | 0.76/0.58/0.70 | 0.01/0.23/0.12 | 0.03/−0.05/0.03 | −0.05/−0.04/−0.05 | −0.08/0.01/−0.03 |
| Not being able to get time off work is a reason for not screening regularly. | 0.68/0.79/0.74 | 0.01/−0.10/−0.05 | −0.02/0.15/0.01 | −0.05/0.03/0.02 | 0.01/0.02/−0.02 |
| Not having transportation to get to my appointment is a reason for not screening regularly. | 0.65/0.49/0.60 | 0.04/0.02/0.04 | −0.06/−0.11/−0.06 | −0.06/−0.13/−0.01 | −0.18/0.11/−0.05 |
| Not receiving a reminder postcard is a reason for not screening for breast/cervical cancer regularly. | 0.62/0.54/0.59 | −0.02/−0.07/−0.02 | −0.09/−0.07/−0.11 | −0.08/−0.18/−0.10 | 0.00/−0.19/0.05 |
| Having to take care of my child(ren) or family is a reason for not screening regularly. | 0.60/0.54/0.55 | 0.09/0.02/0.04 | −0.04/0.22/−0.05 | 0.12/−0.07/0.04 | 0.01/−0.12/−0.08 |
| Not having health insurance or the money to pay for the exam is a reason for not screening regularly. | 0.51/0.47/0.51 | −0.16/−0.08/−0.12 | −0.10/−0.10/−0.02 | 0.12/0.01/0.13 | −0.02/0.21/0.03 |
| Cancer screening fatalism | |||||
| It is not important to screen regularly because everyone will eventually die of something anyway. | −0.05/−0.07/−0.03 | 0.82/0.70/0.79 | −0.14/−0.01/−0.10 | −0.05/−0.09/−0.04 | −0.15/0.004/−0.09 |
| It is not necessary to screen for breast/cervical cancer regularly because it is in God's hands anyway. | −0.10/0.02/−0.05 | 0.67/0.87/0.71 | −0.18/−0.02/−0.10 | 0.00/0.03/0.05 | 0.12/0.08/0.08 |
| If nothing is physically wrong, then you do not need to screen. | 0.12/0.05/0.08 | 0.60/0.84/0.66 | 0.09/0.08/0.03 | 0.09/−0.05/0.04 | −0.01/−0.06/−0.06 |
| Symptomatic deterrents | |||||
| Feeling healthy is a reason for not screening for breast/cervical cancer regularly. | 0.09/0.02/0.02 | 0.10/0.20/0.13 | −0.88/−0.04/−0.91 | 0.10/−0.89/0.09 | 0.02/−0.09/0.05 |
| Having several normal screening test results is a reason for not screening regularly. | 0.20/0.09/0.10 | 0.02/−0.02/−0.01 | −0.82/0.07/−0.81 | 0.06/−0.75/0.03 | 0.60/−0.02/0.01 |
| Not feeling anything abnormal is a reason for not screening regularly. | 0.06/0.003/0.04 | 0.08/−0.03/0.03 | −0.68/0.07/−0.72 | −0.12/−0.81/−0.06 | −0.18/0.01/−0.10 |
| Catastrophic disease expectations | |||||
| Breast/cervical cancer is the worst thing that can happen to a woman. | 0.06/−0.06/0.00 | 0.06/0.06/0.08 | 0.08/0.10/0.07 | 0.83/0.01/0.77 | 0.02/0.59/−0.01 |
| Breast/cervical cancer is a deadly disease. | −0.14/0.12/−0.02 | −0.03/−0.06/−0.05 | −0.12/0.05/−0.10 | 0.81/−0.08/0.75 | −0.04/0.75/−0.004 |
| Negative beliefs about health professionals | |||||
| Health professionals are not compassionate for what their patients are going through. | 0.11/−0.03/0.03 | 0.01/−0.03/−0.05 | 0.04/0.78/0.02 | −0.04/0.01/−0.02 | −0.80/0.08/−0.83 |
| Health professionals are always in a hurry and do not have time for their patients. | −0.06/0.04/−0.03 | −0.21/−0.18/−0.24 | −0.09/0.57/−0.12 | 0.04/−0.12/0.02 | −0.63/−0.01/−0.60 |
| I do not feel comfortable with health professionals doing the screening examination. | 0.001/−0.01/−0.01 | 0.27/0.04/0.16 | −0.03/0.51/−0.07 | −0.04/−0.13/−0.04 | −0.58/−0.01/−0.56 |
| Some health professionals inappropriately touch their patients during the screening examination. | 0.16/0.16/0.13 | 0.11/0.18/0.12 | −0.03/0.57/0.05 | 0.05/0.13/0.05 | −0.50/0.05/−0.53 |
| Health professionals performing screening examinations are not trustworthy. | 0.11/−0.07/0.02 | 0.28/0.08/0.21 | 0.15/0.61/0.10 | 0.12/0.004/0.12 | −0.30/0.09/−0.43 |
Factor names were applied on the basis of item content. The ‘cancer screening fatalism’ factor represents the belief that life events are inevitable thereby rendering cancer screening unnecessary. ‘The negative cultural beliefs about health professionals’ factor reflects socially shared unfavorable beliefs about health professionals, including lack of concern, compassion and trustworthiness. The factor catastrophic disease expectations points to the highly negative socially shared expectations associated with a cancer diagnosis. Finally, the ‘symptomatic deterrents’ factor reflects socially shared beliefs that screening is not necessary when feeling healthy or having negative test results, while the ‘sociocultural deterrents’ factor represents socially shared beliefs concerning social and structural barriers to cancer screening.
Correlations among the cultural factors and the total CCSS are reported for both groups in Table III. As with the factor loadings, the pattern of factor correlations was similar across the two groups. All but one correlation were small to medium in magnitude, indicating conceptual discreteness among the factors. The one correlation that approached a large magnitude for both ethnic groups was between symptomatic deterrents and sociocultural deterrents (Latinos: r = 0.54, P < 0.01; Anglo: r = 0.47, P < 0.01).
Table III.
Correlations between cultural factors for Latino and Anglo sample
| 1 | 2 | 3 | 4 | 5 | 6 | |
| Sociocultural deterrents | 1.00 | 0.03 | 0.47** | 0.20* | 0.21* | 0.75** |
| Cancer screening fatalism | 0.10 | 1.00 | 0.24** | 0.11 | 0.15 | 0.39** |
| Symptomatic deterrents | 0.54** | 0.29** | 1.00 | 0.12 | 0.26** | 0.75** |
| Catastrophic disease expectations | −0.01 | 0.11 | 0.02 | 1.00 | 0.20* | 0.39** |
| Negative beliefs about health care professionals | 0.39** | 0.28** | 0.24** | 0.18* | 1.00 | 0.59** |
| CCSS | 0.79** | 0.50** | 0.76** | 0.27** | 0.74** | 1.00 |
Bottom left represents Latino correlations and top right represents Anglo correlations. *P < 0.05, **P < 0.01.
Means, standard deviations and scale reliabilities as estimated using Cronbach's alphas for Latinos, Anglos and the combined sample are reported in Table IV. Alphas for the overall CCSS were excellent (Latino 0.84, Anglo 0.83, total, 0.84) and the alphas for the cultural factors ranged from 0.66 to 0.90. The lowest alphas were obtained for the catastrophic disease expectations factor, which contains only two items.
Table IV.
Alphas, means (M) and standard deviations (SDs)
| Latino/Anglo/total | Latinos (n = 157) | Anglos (n = 147) | Total (n = 304) | |
| Factors | Alphas | M (SD) | M (SD) | M (SD) |
| Sociocultural deterrents | 0.86/0.79/0.83 | 2.40 (1.47) | 2.44 (1.30) | 2.42 (1.39) |
| Cancer screening fatalism | 0.72/0.80/0.75 | 1.89 (1.44) | 1.48 (0.95) | 1.69 (1.24) |
| Symptomatic deterrents | 0.90/0.87/0.89 | 2.84 (2.06) | 2.87 (1.91) | 2.85 (1.99) |
| Catastrophic disease expectations | 0.70/0.66/0.69 | 5.37 (1.65) | 4.75 (1.53) | 5.08 (1.62) |
| Negative beliefs about health professionals | 0.77/0.75/0.77 | 2.56 (1.46) | 2.18 (1.15) | 2.38 (1.33) |
| CCSS | 0.84/0.83/0.84 | 2.78 (1.1) | 2.50 (0.85) | 2.65 (1.00) |
Based on the suggestions of van de Vijver and Leung [29] for establishing psychometric adequacy with different cultural populations, a test for the equality of reliability coefficients was conducted. Results revealed no significant differences based on ethnicity. Construct equivalence was tested through target rotations and the computation of an index of factorial agreement (Tucker's phi [41]) across the ethnic samples. The test for measurement equivalence revealed a Tucker's phi of 0.98, indicating strong factorial congruence for the two ethnic groups. The establishment of measurement equivalence suggests that findings relevant to ethnic group differences are most likely due to true cross-cultural differences rather than the result of measurement artifacts [30].
As predicted, there were some apparent differences between the two groups in the mean scores obtained for some cultural factors. Independent t-tests of group differences between Latino and Anglo women for all factor scores are reported in Table V. The overall CCSS and three of the five cultural factors (catastrophic disease expectations, cancer screening fatalism, and negative beliefs about health professionals) showed significantly higher scores for Latino women.
Table V.
Differences in cultural factors based on ethnicity
| Factors | t | df | P | d | Confidence interval |
| Sociocultural deterrents | 0.25 | 293 | 0.80 | 0.03 | (−2.78, 0.36) |
| Cancer screening fatalism | −2.94 | 271.54 | 0.004 | 0.34 | (−0.68, −0.14) |
| Symptomatic deterrents | 1.6 | 294 | 0.87 | 0.03 | (−0.42, 0.49) |
| Catastrophic disease expectations | −3.44 | 308.61 | 0.001 | 0.39 | (−0.98, −0.27) |
| Negative beliefs about health professionals | −2.52 | 298.14 | 0.01 | 0.29 | (−0.67, −0.08) |
| CCSS | −2.49 | 310 | 0.01 | 0.28 | (−0.50, −0.06) |
The correlations between the CCSS and breast and cervical cancer screening behaviors, intentions and screening emotions are represented in Tables VI and VII. The overall CCSS was correlated with several cancer screening behaviors and screening emotions. For self-reported screening behaviors and intentions, symptomatic deterrents produced the most statistically significant results, though all factors produced at least one correlation coefficient of medium magnitude. The cultural factors correlated more highly with screening emotions than with screening behaviors or intentions. Screening emotions, in turn, were highly correlated with screening behaviors and intentions, particularly for the Latino sample. Also, some of the cultural factors were stronger predictors of one or the other type of cancer screening behaviors or intentions.
Table VI.
Correlations among cultural factors, breast cancer screening and screening procedure emotions
| MAM compliance ratio |
MAM intention |
CBE compliance ratio |
CBE intention |
MAM emotions |
CBE emotions |
|||||||||||||
| Latinoa | Anglob | Totalc | Latinod | Angloe | Totalf | Latinog | Angloh | Totali | Latinoj | Anglok | Totall | Latinom | Anglon | Totalo | Latinop | Angloq | Totalr | |
| Sociocultural deterrents | −0.21 | 0.03 | −0.08 | −0.01 | −0.37* | −0.16 | −0.13 | −0.08 | −0.10 | −0.21 | −0.29* | −0.25** | 0.29* | 0.07 | 0.18 | 0.37** | 0.34** | 0.35** |
| Cancer screening fatalism | −0.20 | −0.41** | −0.31** | −0.27 | −0.21 | −0.26** | −0.35** | −0.27 | −0.34** | −0.09 | −0.03 | −0.06 | 0.03 | 0.12 | 0.09 | 0.07 | 0.15 | 0.13 |
| Symptomatic deterrents | −0.36* | −0.32* | −0.33** | −0.21 | −0.25 | −0.23* | −0.17 | −0.15 | −0.17* | −0.11 | −0.20 | −0.14 | 0.42** | 0.27* | 0.38** | 0.49† | 0.26† | 0.42** |
| Catastrophic disease expectations | −0.36* | −0.20 | −0.27** | −0.13 | −0.09 | −0.14 | −0.04 | −0.11 | −0.10 | −0.05 | −0.19 | −0.10 | 0.33* | 0.12 | 0.26** | 0.30** | 0.14 | 0.26** |
| Negative beliefs about health professionals | −0.10 | −0.20 | −0.15 | −0.15 | −0.14 | −0.16 | −0.33** | 0.12 | −0.16 | 0.06 | −0.13 | −0.01 | 0.01 | 0.28* | 0.16 | 0.36 | 0.52** | 0.42** |
| CCSS | −0.44** | −0.33* | −0.38** | −0.21 | −0.37** | −0.29** | −0.33** | −0.14 | −0.28** | −0.12 | −0.25* | −0.16 | 0.40** | 0.28* | 0.37** | 0.58** | 0.46** | 0.56** |
| MAM emotions | −0.53** | −0.24 | −0.38** | −0.09 | −0.27* | −0.19* | −0.50** | −0.09 | −0.30** | −0.11 | −0.26* | −0.17 | ||||||
| CBE emotions | −0.37** | −0.20 | −0.30** | −0.06 | −0.14 | −0.10 | −0.40** | 0.01 | −0.25** | 0.05 | −0.20 | −0.05 | ||||||
The italic, bold pairs represent significant differences in the correlation magnitudes between Latino and Anglo women at P < 0.05 and bold pairs (no italics) are significant at P < 0.10. †P < 0.10, *P < 0.05, **P < 0.01.
n ranges from 49 to 52,
n = 57–60,
n = 106–112,
n = 66–74,
n = 68–70,
n = 134–144,
n = 63–71,
n = 68–71,
n = 131–142,
n = 66–74,
n = 68–70,
n = 134–144,
n = 50–53,
n = 58–61,
n = 108–114,
n = 70–78,
n = 72–75,
n = 142–153.
Table VII.
Correlations among cultural factors, cervical cancer screening and screening procedure emotions
| Pap compliance ratio |
Pap intention |
Pap emotions |
|||||||
| Latinoa | Anglob | Totalc | Latinod | Angloe | Totalf | Latinog | Angloh | Totali | |
| Sociocultural deterrents | −0.15 | 0.13 | 0.01 | 0.02 | 0.11 | 0.06 | 0.09 | 0.03 | 0.06 |
| Cancer screening fatalism | −0.15 | −0.14 | −0.11 | −0.21 | −0.39** | −0.24** | −0.04 | 0.03 | −0.004 |
| Symptomatic deterrents | −0.09 | −0.03 | −0.08 | −0.22 | −0.11 | −0.17* | 0.06 | 0.20 | 0.11 |
| Catastrophic disease expectations | 0.19 | 0.02 | 0.10 | 0.01 | 0.05 | 0.05 | −0.03 | 0.20 | 0.07 |
| Negative beliefs about health professionals | 0.13 | −0.38** | −0.14 | −0.13 | −0.05 | −0.06 | 0.09 | 0.08 | 0.10 |
| CCSS | −0.10 | −0.08 | −0.08 | −0.21† | −0.09 | −0.14† | 0.05 | 0.18 | 0.10 |
| Pap emotions | 0.10 | −0.33** | −0.13 | −0.16 | −0.04 | −0.08 | 0.09 | 0.07 | 0.09 |
n ranges from 59 to 63,
n = 57–59,
n = 117–122,
n = 72–76,
n = 71–73,
n = 142–147,
n = 74–79,
n = 72–74,
n = 146–151.
*P < 0.05, **P < 0.01, †P < 0.10.
There were also some apparent differences in correlation magnitude between the two ethnic groups based on Fischer's r-to-z transformations and z-tests of difference. Four of these differences were statistically significant and one approached significance (correlation differences noted in Table VI). Except for one of these differences, screening was more highly correlated with culture and/or screening emotions for the Latino group.
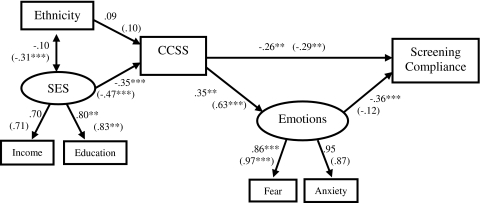
The predictive validity of the CCSS was examined using Bentler's structural equations program [42] (EQS, 2005) for the analysis of causal models. To this end, a model was tested including the hypothesized relations among scores on the CCSS as predictors of cancer screening and screening emotions. In a manner consistent with the model for the study of culture, demographic factors conceived as sources of cultural variation were included in the model as antecedents of the cultural factors assessed by the CCSS (see Fig. 2). A mean composite score for the CCSS was calculated which was expected to directly and/or indirectly predict breast and cervical cancer screening through screening emotions.
Fig. 2.
Model testing the predictive validity of CCSS (paths in parentheses represent the paths for CBE; paths not in parentheses represent paths for MAM).
Adequacy of model fit was assessed using χ2 goodness-of-fit statistic, the ratio of χ2 to the degrees of freedom (χ2/df), the comparative fit index (CFI) and the root mean square error of approximation (RMSEA). The nonsignificant (P > 0.05) χ2 was used to determine the degree to which the estimated covariance model matches the data covariance matrix. For χ2/df, a ratio of <2.0 is indicative of a good model fit [43]. A CFI value >0.90 is considered indicative of an adequate fitting model whereas a value of 0.95 is indicative of a good-fitting model [44]. For the average error of parameter estimates, or the RMSEA, a value <0.05 indicates close approximate fit [45] and values ranging from 0.08 to 0.10 indicate mediocre fit [49]. Due to limitations with relying on cutoff points, several goodness-of-fit measures should be used to determine global model fit [46].
The model testing the predictive validity of the CCSS with MAM and MAM emotions provided a good fit of the data [CFI = 0.96, χ2(11, n = 103) = 18.15, P = 0.08, χ2/df = 1.65, RMSEA = 0.08] and accounted for 26% of the variance (see Fig. 2). Women who scored higher on the CCSS were less likely to be compliant with MAM screening (β = −0.26, P < 0.01) and more likely to have negative MAM emotions (β = 0.35, P < 0.01). In fact, the CCSS was found to exert both a direct as well as an indirect effect on MAM compliance through negative MAM emotions (βindirect = −0.126, P < 0.01). The model testing the predictive validity of the CCSS with CBE compliance and negative CBE emotions provided an adequate fit [CFI = 0.95, χ2(11, n = 127) = 27.85, P = 0.00, χ2/df = 2.53, RMSEA = 0.11] and accounted for 14% of the variance (see Fig. 2; paths noted in parentheses). Higher scores on the CCSS predicted less CBE compliance (β = −0.29, P < 0.01) and greater negative CBE emotions (β = 0.63, P < 0.001). The CCSS however only exerted a direct and no indirect effect on CBE compliance through CBE emotions (βindirect = −0.029, P > 0.05). A third model predicting Pap compliance was tested and also provided an adequate fit [CFI = 0.95, χ2(11, n = 113) = 16.13, P = 0.10, χ2/df = 1.46, RMSEA = 0.07]. In this case, the path between CCSS and Pap compliance was not very strong (β = −0.09, P > 0.05). However, when intention to have a Pap was used as an outcome, the path was stronger (β = −0.17, P < 0.05) [CFI = 0.94, χ2(11, n = 140) = 19.54, P = 0.03, χ2/df = 1.78, RMSEA = 0.08].
Discussion
Overall, this research serves to illustrate the implementation of the bottom-up approach to the study of culture and psychological processes in health behavior with culturally diverse populations employing mixed methodologies. The research resulted in the development of an instrument designed to assess cultural factors related to cancer screening that can inform evidence-based interventions with Latino and Anglo women. A number of distinct features that characterize the research involved in the development of the CCSS are noteworthy. First, the work was guided by a theoretical model (see Fig. 1) that clearly specifies the manner in which the identified cultural factors were expected to relate to screening behavior and psychological processes, as well as to population categories conceived as sources of cultural variation (e.g. ethnicity and SES). This is important as theory-based results may contribute not only to intervention but also to advance theory and future research. Second, the identification of cultural factors was based on a well-defined concept of culture that focuses on phenomena particularly relevant to psychological functioning and health behavior, such as socially shared beliefs, norms and expectations. Third, the bottom-up approach allowed for the generation of items based on cultural aspects that emerged directly from the minority and majority populations, respectively. Last, statistical procedures consistent with recommendations for cross-cultural research were implemented to establish measurement equivalence [29] resulting in an instrument that could be used with both minority and majority populations to examine ethnic-based health disparities.
The resulting CCSS includes five factors that emerged from the analysis of cultural elements identified as important to one or the other ethnic group, but relevant to individuals from both groups. Interestingly the contents of some of the factors that emerged from this research are similar to those identified as deterrents of cancer screening in previous qualitative studies [24–26]. The CCSS was found to be reliable and demonstrated predictive validity. Moreover, the CCSS demonstrated measurement equivalence across ethnic groups suggesting that it could be useful for health disparities research and intervention efforts with both Latino and Anglo women of various SES backgrounds.
Concerning the relations between cultural factors and screening (see Tables VI and VII), the finding that some factors were relevant to all forms of cancer screening while others were relevant to one or another is consistent with the unique nature of some screening methods. Specifically, the procedures and type of health professionals involved when having a CBE, MAM or Pap are quite different. Also, intention to screen and screening compliance represent different behavioral responses and may reflect different concerns for patients. Hence, although the CCSS can be used to assess cultural aspects relevant to a variety of cancer screening behaviors, it is important to consider that some cultural factors may relate to or influence each form of screening in a different way. Ignoring this, as well as assuming that a particular cultural factor is equally important to all individuals of an ethnic group can negatively impact intervention efforts and may explain some of the inconsistencies observed in research findings and interventions dealing with the role of culture and cultural sensitivity in health behavior.
Despite the differential influence of the individual cultural factors on screening behaviors, the CCSS demonstrated predictive validity. Consistent with the model for the study of culture, structural equation modeling demonstrated a good level of predictive validity for the CCSS, particularly in the case of MAM and CBE compliance in addition to MAM and CBE emotions. Still, even though the predictive validity of intention to have a Pap was also good, the lower predictive validity for Pap compliance needs to be further examined in future research. The observed differences in predictive validity may be a consequence of collapsing the individual cultural factors into one composite score. For instance, correlations suggest that in the case of cervical cancer screening, cancer screening fatalism and negative beliefs about health care professionals are the two cultural factors that relate to Pap screening the most. Although it was beyond the scope of this paper to test the predictive validity of the individual cultural factors, this should be more closely examined in future research along with other aspects of the conceptual model that guided this study.
Of theoretical and practical significance is the finding that in the case of MAM compliance, the influence of the CCSS was both direct and indirect through screening emotions. Correlations among the individual cultural factors from the CCSS suggest a similar trend. For instance, some cultural factors were not related to screening but were related to psychological processes such as emotions that in turn were related to screening behavior. Therefore, when research only examines the direct influence of cultural factors on health behavior and ignores the role of potential indirect psychological aspects, these important cultural factors may not appear to be related to health behavior. As a result, such aspects of culture may be left out of instruments or interventions dealing with diverse populations. Future research should examine the extent to which the individual cultural factors included in the CCSS may relate to psychological processes such as emotions, which in turn are likely to influence cancer screening behaviors.
These findings also point to the necessity for employing statistical procedures such as Fischer's r-to-z test of difference or multi-group structural equation modeling. Such statistical analyses specifically take into consideration the divergence in findings based on ethnicity and their impact on psychological processes and health behavior. For example, consider the differential relation between negative beliefs about health professionals and CBE compliance for Latino and Anglo women (r = −0.33, P <0.01 and r = 0.12, P >0.05, respectively). If these data were not analyzed separately for the two ethnic groups, but rather collapsed across ethnicity, one might conclude that this cultural factor does not relate to CBE compliance (r = −0.16, p > 0.05). As a result, intervention efforts may erroneously ignore cultural beliefs about health professionals that are particularly important for Latino women.
An additional conceptual and methodological issue to be further examined is the influence of ethnicity and SES as sources of variation in the CCSS. Results from t-tests revealed that on the average Latino women reported higher scores on the CCSS as compared with Anglo women. However, structural equation modeling indicated that when SES is taken into consideration, the impact of ethnicity as a source of cultural variation is weaker. Moreover, these analyses did not reveal a direct effect of SES or ethnicity on screening behaviors, highlighting that cultural factors measured through the CCSS were more proximal predictors of cancer screening. Murguia and Zea [47] reported similar findings in that Latino cultural health beliefs were found to be better predictors of health care utilization as compared with SES and acculturation.
While these findings are consistent with the view of the model for the study of culture, which conceives SES as a source of cultural variation, the complexity of relations between ethnicity, SES and other demographic factors needs to be further examined, as suggested by Borrayo and Jenkins [48]. Still, it is important to recognize that ethnicity influenced the strength of relations among the cultural factors and cancer screening. These findings suggest that even though the same cultural aspects apply to both ethnic and SES groups, ethnicity moderates these relations.
Despite the demonstrated utility of the CCSS, the interpretation of results is limited in some ways. For instance, while measurement equivalence was established for the Latino and Anglo samples, it was not possible to establish equivalence based on the Spanish and English version of the CCSS since only 43 Latino women completed the Spanish survey. An examination of the reliabilities for the English and Spanish versions suggests that the Spanish CCSS is likely to be reliable (e.g. alphas for three of the five subscales and the total CCSS was higher for the Spanish version). However, future research should demonstrate the factor structure, predictive validity and measurement equivalence of the Spanish CCSS. Furthermore, the convergent and discriminant validity of the CCSS needs to be established.
Another potentially limiting factor is that the region in which the research was conducted is predominantly comprised of Latinos of Mexican cultural background. Therefore, it is unclear how the factors included in the instrument may work with Latinos from other national origins or regions of the United States. Furthermore, while this research demonstrated between-ethnic group differences in the relations among some of the cultural factors and cancer screening, within-ethnic group differences are also possible. Hence, future research should examine whether or not variations in the relevance of the cultural factors exist among individuals from Latino subpopulations such as SES, national origin, region in which they reside and generation status.
An important aspect of this research and the development of the CCSS is that it provides the tools necessary for generating empirical findings that can inform the development of evidence-based cultural interventions. The procedures outlined in this research and the resulting CCSS allow for the development of both targeted and tailored programs based on the assessment of cultural information. Utilizing the CCSS, health professionals can obtain a profile of the screening-relevant cultural factors for a particular population or community. Although the development of the CCSS is expected to be particularly important for working with culturally diverse populations, health professionals must be cautious when attributing to a community or subpopulation cultural factors based on mean scores for a much larger and more heterogeneous ethnic population.
Health professionals should also take into consideration the importance of within-group differences such as those based on immigration status, education and income in their clinical work at the individual level. To this end, the CCSS can be administered to an individual from a particular community to determine their personal cancer-relevant cultural profile. To enhance the effectiveness of tailored interventions, health professionals can consider an individual's cultural profile to identify specific cancer-relevant cultural elements that may be particularly important to that individual.
Funding
National Cancer Institute and the Office of Research on Women's Health at the National Institutes of Health, Grant 1R21CA101867, H. Betancourt, PI.
Conflict of interest statement
None declared.
Acknowledgments
We would like to thank Claudia Argueta, Crystal Coker, Monica Hodges, Natalie Kaiser, Brenda Navarrete and Jennifer Tucker for their help collecting data and their assistance with preliminary data analyses. We would also like to thank all of the women that graciously agreed to participate in this study and the community organizations that facilitated this process.
References
- 1.Kerlikoske K, Grady D, Rubin SM, et al. Efficacy of screening mammography: a meta-analysis. J Am Med Assoc. 1995;273:149–54. [PubMed] [Google Scholar]
- 2.Ries LA, Melbert D, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2005. Bethesda, MD: National Cancer Institute; 2008. [Google Scholar]
- 3.Ramirez AG, Talavera GA, Villarreal R, et al. Breast cancer screening in regional Hispanic populations. Health Educ Res. 2000;15:559–68. doi: 10.1093/her/15.5.559. [DOI] [PubMed] [Google Scholar]
- 4.Maxwell A, Bastani R, Warda U. Mammography utilization and related attitudes among Korean-American women. Women Health. 1998;27:89–107. doi: 10.1300/J013v27n03_07. [DOI] [PubMed] [Google Scholar]
- 5.Gorin SS, Heck JE. Cancer screening among Latino subgroups in the United States. Prev Med. 2005;40:515–26. doi: 10.1016/j.ypmed.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 6.Katapodi MC, Facione NC, Miaskowski C, et al. The influence of social support on breast cancer screening in a multicultural community sample. Oncol Nurs Forum. 2002;29:845–52. doi: 10.1188/02.ONF.845-852. [DOI] [PubMed] [Google Scholar]
- 7.Suarez L, Ramirez AG, Villareal L, et al. Social networks and cancer screening in four U.S. Hispanic groups. Am J Prev Med. 2000;19:47–52. doi: 10.1016/s0749-3797(00)00155-0. [DOI] [PubMed] [Google Scholar]
- 8.Shah M, Zhu K, Wu H, et al. Hispanic acculturation and utilization of cervical cancer screening in the United States. Prev Med. 2005;42:146–9. doi: 10.1016/j.ypmed.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 9.Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 10.Betancourt H, Flynn P. The psychology of health: physical health and the role of culture in behavior. In: Villarruel FA, Carlo G, Contreras Grau JM, et al., editors. Handbook of US Latino Psychology. Thousand Oaks, CA: Sage Publications; 2009. pp. 347–61. [Google Scholar]
- 11.Betancourt H, Fuentes JL. Culture and Latino issues in health psychology. In: Kazarian S, Evans D, editors. Handbook of Cultural Health Psychology. San Diego, CA: Academic Press; 2001. pp. 305–21. [Google Scholar]
- 12.Roosa MW, Dumka LE, Gonzales NA, et al. Cultural/ethnic issues and the prevention scientist in the 21st century. Prev Treat. 2002 Available at: http://journals.apa.org/prevention/volume5/pre0050005a.html. Accessed: 20 August 2009. [Google Scholar]
- 13.Betancourt H, Lopez SR. The study of culture, ethnicity, and race in American psychology. Am Psychol. 1993;48:629–37. [Google Scholar]
- 14.Betancourt H, Hardin C, Manzi J. Beliefs, value orientation, and culture in attribution processes and helping behavior. J Cross Cult Psychol. 1992;23:179–95. [Google Scholar]
- 15.Rohner RP. Toward a conceptualization of culture for cross-cultural psychology. J CrossCult Psychol. 1989;15:111–38. [Google Scholar]
- 16.Herskovits M. Man and His Works. New York: Knopf; 1948. [Google Scholar]
- 17.Triandis H, Lambert W, Berry J, et al. Handbook of Cross-Cultural Psychology. Boston, MA: Allyn & Bacon; 1980. [Google Scholar]
- 18.Poortinga Y, Malpass R. Making inferences from cross-cultural data. In: Looner WJ, Berry JW, editors. Field Methods in Cross-Cultural Research. Beverly Hills, CA: Sage Publications, Inc.; 1984. pp. 17–46. [Google Scholar]
- 19.Fiske AP, Kitayama S, Markus H, et al. The cultural matrix of social psychology. In: Gilbert DT, Fiske ST, editors. Handbook of Social Psychology. 4th edn. New York: McGrawHill; 1998. pp. 915–81. [Google Scholar]
- 20.Hruschka DJ, Hadley C. A glossary of culture in epidemiology. Journal of Epidemiol Commun H. 2008;62:947–51. doi: 10.1136/jech.2008.076729. [DOI] [PubMed] [Google Scholar]
- 21.Zuckerman M. Some dubious premises in research and theory on racial differences: scientific, social and ethnical issues. Am Psychol. 1990;45:1297–303. doi: 10.1037//0003-066x.45.12.1297. [DOI] [PubMed] [Google Scholar]
- 22.Jones JM. Psychological models of race: what have they been and what should they be? In: Goodchild JD, editor. Psychological Perspectives on Human Diversity in America. Washington, DC: American Psychological Association; 1991. pp. 5–46. [Google Scholar]
- 23.Smedly A, Smedly BD. Race as biology is fiction, racism as a social problem is real: anthropological and historical perspectives on the social construction of race. Am Psychol. 2005;60:16–26. doi: 10.1037/0003-066X.60.1.16. [DOI] [PubMed] [Google Scholar]
- 24.Chavez LR, Hubbell FA, Mishra SI, et al. The influence of fatalism on self-reported use of Papanicolaou smears. Am J Prev Med. 1997;13:418–24. [PubMed] [Google Scholar]
- 25.Borrayo EA, Jenkins SR. Feeling healthy: so why should Mexican-descent women screen for breast cancer? Qual Health Res. 2001;11:812–23. doi: 10.1177/104973201129119550. [DOI] [PubMed] [Google Scholar]
- 26.Moy B, Park ER, Feibelmann S, et al. Barriers to repeat mammography: cultural perspectives of African-American, Asian, and Hispanic women. Psychooncology. 2006;15:523–634. doi: 10.1002/pon.994. [DOI] [PubMed] [Google Scholar]
- 27.Borrayo EA, Gonzalez P, Swaim R, et al. The Latina breast cancer screening scale: beliefs about breast cancer and breast cancer screening. J Health Psychol. 2009;14:944–55. doi: 10.1177/1359105309341203. [DOI] [PubMed] [Google Scholar]
- 28.Kreuter MW, Lukwago SN, Bucholtz DC, et al. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003;30:133–46. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- 29.van de Vijver FJ, Leung K. Methods and Data Analysis for Cross-Cultural Research. Thousand Oaks, CA: Sage Publications, Inc.; 1997. [Google Scholar]
- 30.Chen FF. What happens if we compare chopsticks with forks? The impact of making inappropriate comparisons in cross-cultural research. J Pers Soc Psychol. 2008;95:1005–18. doi: 10.1037/a0013193. [DOI] [PubMed] [Google Scholar]
- 31.Triandis HC, Kilty KM, Shanmugam AV, et al. Cognitive structures and the analysis of values. In: Triandis HC, editor. The Analysis of Subjective Culture. New York: John Wiley; 1972. [Google Scholar]
- 32.Marin BV, Perez-Stable EJ, Marin G, et al. Attitudes and behaviors of Hispanic smokers: implications for cessation interventions. Health Educ Quart. 1990;17:287–97. doi: 10.1177/109019819001700305. [DOI] [PubMed] [Google Scholar]
- 33.Knight GP, Roosa MW, Umana-Taylor AJ. Studying Ethnic Minority and Economically Disadvantaged Populations. Washington, DC: American Psychological Association; 2009. [Google Scholar]
- 34.Brislin RW. Translation and content analysis of oral and written materials. In: Triandis HC, Berry JW, editors. Handbook of Cross-Cultural Psychology. Boston, MA: Allyn & Bacon; 1980. pp. 389–444. [Google Scholar]
- 35.Prieto AJ. A method for translation of instruments to other languages. Adult Educ Quart. 1992;43:1–14. [Google Scholar]
- 36.Wang WL, Lee HL, Fetzer SJ. Challenges and strategies of instrument translation. Western J Nurs Res. 2006;28:310–21. doi: 10.1177/0193945905284712. [DOI] [PubMed] [Google Scholar]
- 37.Bryant FB, Yarnold PR. Principal-components analysis and exploratory and confirmatory factor analysis. In: Grimm LG, Yarnold PR, Grimm LG, et al., editors. Reading and Understanding Multivariate Statistics. Washington, DC: American Psychological Association; 1995. [Google Scholar]
- 38.Gorsuch R. Factor Analysis. 2nd edn. Hillsdale, NJ: Erlbaum; 1983. [Google Scholar]
- 39.Smith RA, Cokkinides V, Eyre HJ. American Cancer Society guidelines for the early detection of cancer, 2006. CA Cancer J Clin. 2006;56:11–25. doi: 10.3322/canjclin.56.1.11. [DOI] [PubMed] [Google Scholar]
- 40.Kudadjie-Gyamfi E, Magai C. The influence of coping styles on mammography screening. Cultur Divers Ethnic Minor Psychol. 2008;14:183–92. doi: 10.1037/1099-9809.14.3.183. [DOI] [PubMed] [Google Scholar]
- 41.Tucker LR. A Method for Synthesis of Factor Analysis Studies (Personnel Research Section Report No. 984) Washington, DC: Department of the Army; 1951. [Google Scholar]
- 42.Bentler PM. EQS 6 Structural Equations Program Manual. Encino, CA: Multivariate Software; 2005. [Google Scholar]
- 43.Tabachnick BG, Fidell LS. Using Multivariate Statistics. New York: Harper Collins; 2001. [Google Scholar]
- 44.Browne M, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Thousand Oaks, CA: Sage Publications, Inc.; 1993. [Google Scholar]
- 45.MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychol Methods. 1996;1:130–49. [Google Scholar]
- 46.Bentler PM. On tests and indices for evaluating structural models. Pers Individ Dif. 2007;42:825–9. [Google Scholar]
- 47.Murguia A, Zea MC. The development of the Cultural Health Attributions Questionnaire (CHAQ) Cultur Divers Ethnic Minor Psychol. 2000;6:268–83. doi: 10.1037/1099-9809.6.3.268. [DOI] [PubMed] [Google Scholar]
- 48.Borrayo EA, Jenkins SR. Feeling frugal: socioeconomic status, acculturation, and cultural health beliefs among women of Mexican descent. Cultur Divers Ethnic Minor Psychol. 2003;9:197–206. doi: 10.1037/1099-9809.9.2.197. [DOI] [PubMed] [Google Scholar]