Abstract
Background
The direct anterior approach in THA is an intermuscular approach that requires no muscle detachment. However, it is difficult to elevate the proximal femur for access to the femoral canal.
Questions/purposes
We asked (1) which part of the capsule should be released to allow effective elevation of the proximal femur; (2) whether the release of the internal obturator tendon allows elevation; and (3) whether hip hyperextension reduces the ability to elevate the femur.
Methods
We conducted a cadaver study and a clinical study. In the first study, the elevation of the proximal femur was measured in 6 hips in 3 cadavers after excision of the anterior capsule, after the release of the superior capsule or the posterior capsule, after the release of the superior and posterior capsule, and after the release of the internal obturator tendon under traction of 70 N. Each hip was positioned at 0°, 15°, and 25° hyperextension. In the second study of 39 patients, the posterior capsule was released after the superior capsule in the first 13 hips, and the superior capsule was released after the posterior capsule in the next 26 hips. The elevation achieved for each hip was measured as in the cadaver study.
Results
In our cadaver study, hip elevation increased after superior capsule release but not after release of the internal obturator tendon. After superior capsule release, the ability to elevate the femur was not diminished by hip hyperextension. In our clinical study, elevation increased after superior capsule release.
Conclusions
Superior capsule release was most effective of all releases for elevating the proximal femur in the direct anterior approach.
Introduction
In so-called minimally invasive hip arthroplasty, the direct anterior approach is an intermuscular approach that requires no muscle detachment. In one cadaver study, the damage to the abductor muscles and the external rotators in THA using the direct anterior approach were reportedly limited compared with that in THA using the posterior approach [7]. Clinically, the dislocation rate is reportedly as low as that for a conventional direct lateral approach [4, 5, 8, 12]. Early postoperative recovery is also apparently improved compared with that after THA using the miniposterior approach [9] and a conventional anterolateral approach [6]. Functional outcome assessed by using the Medical Outcomes Study 36-Item Short-Form Health Survey has also reportedly been superior in comparison with that for THA using the mini-anterolateral approach [1].
Beginning in 1947, Judet and Judet used the Hueter anterior approach for hip exposure for neck arthroplasty and THA [2]. The initial technique involved removing the anterior tensor fasciae latae from the anterolateral iliac crest, sectioning the reflected head of the rectus, and releasing the piriformis. This approach had been modified to allow exposure of the acetabulum and femur through a single incision that does not require release of any muscles or tendons from the pelvis or femur [5, 12]; we call this approach the “direct anterior approach.” When using the direct anterior approach in THA, view of and access to the acetabulum seem equal to those for any other surgical approaches [10], whereas a more demanding task is preparation of the femur [10]. To expose the proximal femur and elevate it almost to the skin level to allow for more or less straight access to the femoral canal, some surgeons have used special surgical tables [5, 12]. Others use a standard surgical table [10, 11] but position the limb in hyperextension, external rotation, and adduction as a first step to expose the proximal femoral canal for preparation. Elevation of the proximal femur is then aided by a bone hook or retractors, and then the capsule and external rotators are released. Capsular releases have been variably described, and the strategy for releasing external rotators is not systematic [3, 5, 10–12]. Some authors specify the superior portion of the capsule as the first part to be released; others specify instead the superior portion, the lateral portion, or the posterior portion. Additionally, some authors have recommended further release of the internal obturator tendon, piriformis tendon, external obturator tendon, or gemelli tendon.
We therefore asked (1) which part of the capsule should be released to allow effective elevation of the proximal femur; (2) whether the release of the internal obturator tendon allows elevation; and (3) whether hip hyperextension reduces the ability to elevate the femur.
Materials and Methods
We conducted two studies: a cadaver study to answer questions 1, 2, and 3 and a clinical study to answer questions 1 and 3. In our cadaver study, we obtained three fresh-frozen female cadavers (six hips) that had not undergone any hip or pelvic surgery. Each cadaver was placed in the supine position. An incision of 10 cm was started from the point 2 cm lateral and 1 cm distal from the anterosuperior iliac spine and was oriented along the longitudinal axis of the tensor fasciae latae. The interval between the tensor fasciae latae and the sartorius muscles was developed by splitting. The rectus femoris was mobilized medially, and the anterior capsule was exposed by placing the retractors superior and inferior to the femoral neck. The anterior capsule was excised, and the retractors were repositioned intracapsularly to expose the femoral neck. The femoral neck was osteotomized in situ with an oscillating saw, and the femoral head was removed. In this step, two Kirschner wires were fixed to the ilium as a reference. A bone hook was then attached to a tensiometer. Placing a bone hook at the inner surface of the medial cortex near the osteotomized site, we elevated the proximal femur vertically under traction at 70 N. We placed a square on the wires, and then measured the change in distance between the square on the reference level and a bar on the bone hook when traction was increased from 0 N to 70 N. The measurement was performed with each hip in 0° extension, 90° external rotation, and 0° adduction. We defined the part of the capsule that was attached between the ilium and the trochanteric fossa as the superior capsule and the part that was attached between the posterior rim of the acetabulum and posterior surface of the femoral neck as the posterior capsule (Fig. 1). We released the superior capsule on one side and the posterior capsule on the other side. The distance of change in elevation of the proximal femur was then measured with hips in 0°, 15°, and 25° hyperextension. After releasing the superior and posterior on both sides, we measured the distance of change in elevation with hips in 0°, 15°, and 25° hyperextension. Finally, the internal obturator tendon was released, and the distance of change in elevation was measured at hip positions of 0°, 15°, and 25° hyperextension.
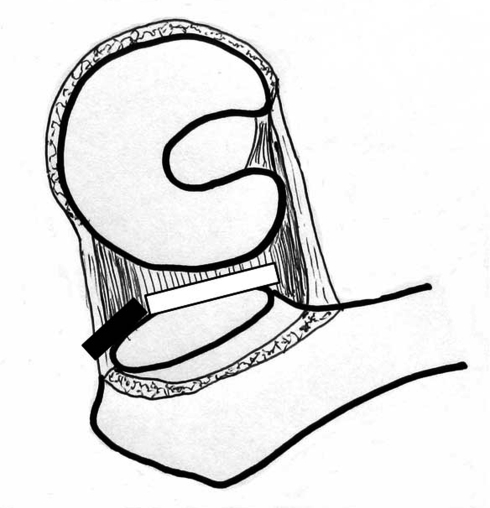
Fig. 1.
The schematic illustration demonstrates the release of the superior capsule (black bar), which was attached between the ilium and the trochanteric fossa, and the release of the posterior capsule (white bar), which was attached between the posterior rim of the acetabulum and posterior surface of the femoral neck. (This illustration was presented as Fig. 1 in Poster No. 2039 at the 55th Annual Meeting of the Orthopaedic Research Society, February 22–25, 2009 in Las Vegas, Nevada.)
In our clinical study, we performed THAs using a direct anterior approach in 39 sequential patients. After excising the anterior capsule and removing the femoral head, we released the posterior capsule after releasing the superior capsule in the first 13 hips (12 females and one male). The average age of patients at surgery was 73.0 years (range, 66–84 years). The average body mass index (BMI) of patients was 22.5 kg/m2 (range, 18.7–27.5 kg/m2). The diagnosis that made THA necessary was secondary coxarthrosis resulting from a dysplastic hip in 11 and osteonecrosis in two. In the next 26 hips (all in women), the superior capsule was released after the posterior capsule release. The average age of patients at surgery was 71.5 years (range, 58–85 years). The average BMI was 23.6 kg/m2 (range, 16.2–32.5 kg/m2). The diagnosis was secondary coxarthrosis resulting from a dysplastic hip in 24, rheumatoid arthritis in one, and femoral neck fracture in one.
The side bar of the operation table was used as a reference level (Fig. 2A). For the cadaver study we attached a bone hook to a tensiometer (Fig. 2B). Placing a bone hook at the inner surface of the medial cortex near the osteotomized site, we elevated the proximal femur vertically under traction of 70 N. Putting a square on the bar of the operation table, we measured the change in the distance between the reference level and a bar on the bone hook when the traction level changed from 0 N to a level of 70 N in three steps: after removal of the femoral head, after release of the posterior capsule or the superior capsule, and after release of both posterior and superior capsules (Fig. 2A–B). The distance of the change in elevation of the proximal femur was measured with the hip in 0° extension. After the release of either the posterior or the superior capsule, the distance was measured again, with the hip in 15° and 25° hyperextension. After these capsule releases, the exposure of the proximal femur was adequate for preparing the femoral canal in all hips; thus, the additional release of the internal obturator tendon was not performed.
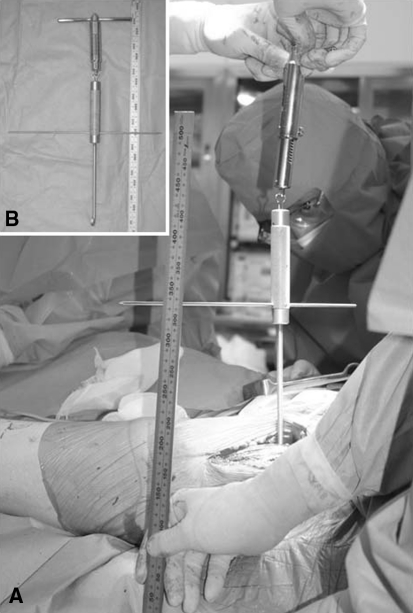
Fig. 2A–B.
(A) Putting a square on a bar of the surgery table, we measured the change in the distance between the bar on the table and a bar on the bone hook when traction was changed from 0 N to 70 N. (B) The traction force was indicated by a tensiometer.
We were unaware of any studies on the targeted distance of change in elevation of the proximal femur in THA through a direct anterior approach, so we did not know whether the required elevation distance depends on volume, tension, and length of the muscles; thickness of subcutaneous fatty tissue; or other factors in each patient. We used the Scheffé test of one-way factorial analysis of variance to compare the distance of change in elevation among three steps and three hip positions. Power analyses for effect size and required total sample size were 0.94 and 30, respectively, in the comparison among the steps of capsule release (total sample size = 103) and 0.91 and 36, respectively in the comparison among hip hyperextension positions (total sample size = 86).
Results
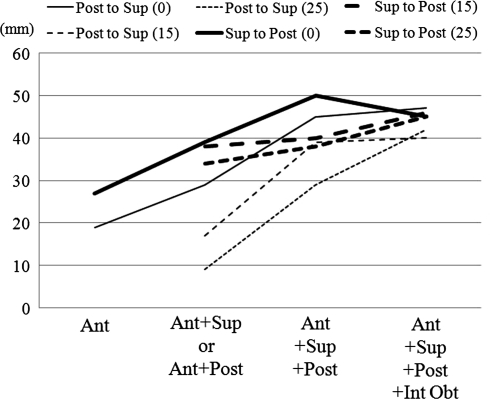
In our cadaver study, superior capsule release allowed elevation of the proximal femur because the distance of the change in elevation after that release was larger than that after posterior capsule release with the hip in 15° and 25° extension (Fig. 3). No effects of further release of the internal obturator tendon were observed. With the hips in 15° and 25° hyperextension, the distance did not change after superior capsule release, whereas the distance decreased after posterior capsule release. This diminution of elevation with hip hyperextension was solved by adding superior capsule release.
Fig. 3.
Distance of change in elevation of the proximal femur in each step in the cadaver study is shown. Superior capsule release was most effective for elevation of the proximal femur. No major effects of further release of the internal obturator tendon were observed. Post to Sup = the posterior capsule was released after the superior capsule release; Sup to Post = the superior capsule was released after the posterior capsule release. Ant = anterior capsule release; Sup = superior capsule release; Post = posterior capsule release; Int Obt = internal obturator muscle release. Parenthetic numerals indicate the angle of hip hyperextension.
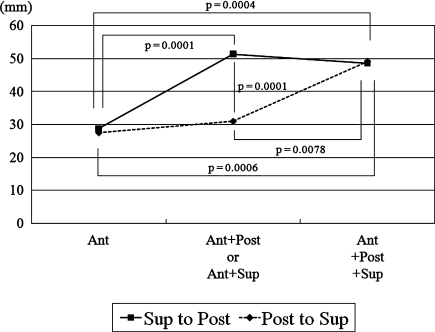
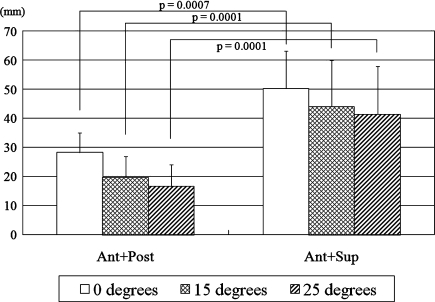
In our clinical study, the effect of superior capsule release on elevation of the proximal femur was greater (p < 0.001) than in posterior capsule release (Fig 4). After superior capsule release or posterior capsule release, the distance gradually decreased as the hip was positioned at 15° and 25° hyperextension (Fig. 5).
Fig. 4.
Distance of change in elevation of the proximal femur in each step in our clinical study is shown. With hips at 0° extension, the effect of superior capsule release on femur elevation was greater than for posterior capsule release. Post to Sup = the posterior capsule was released after the superior capsule; Sup to Post = the superior capsule was released after the posterior capsule; Ant = anterior capsule release; Sup = superior capsule release; Post = posterior capsule release. (This illustration was presented as Fig. 4 in Poster No. 2039 at the 55th Annual Meeting of the Orthopaedic Research Society, February 22–25, 2009 in Las Vegas, Nevada.)
Fig. 5.
Distance of change in elevation of the proximal femur after posterior capsule release or superior capsule release is shown. The distance gradually decreased as the hip was positioned in 15° and 25° hyperextension after posterior release or superior release. Ant = anterior capsule release; Sup = superior capsule release; Post = posterior capsule release.
Discussion
The surgical technique of direct anterior approach for THA has been described by a number of authors [3, 5, 10–12]. The exposure of the acetabulum that is obtained with this approach is reportedly equal to that obtained with any other surgical approach [10], whereas effort is required to expose the proximal femur and elevate it almost to the skin level to allow for more or less straight access to the femoral canal [10]. All of these authors have recommended that the hip be positioned in hyperextension, external rotation, and adduction. Some authors use a special traction table [5, 12] and bone hook [3, 5]. All authors who have described the steps for capsule release and release of external rotators have done so from their own experience, and thus, there are many variations (Table 1). To clarify the part of the capsule most effective for elevation of the proximal femur, we first defined the superior capsule and the posterior capsule. We then investigated which part of the capsule is most effective for femoral elevation. Because the internal obturator tendon is composed of long, thick bundles and attaches the most anteriorly to the greater trochanter, we theorized that it might stabilize the proximal femur during elevation. Thus, we next investigated whether the release of the internal obturator tendon allows elevation. To expose the proximal femoral canal for preparation, the surgeon must position the limb in hyperextension, external rotation, and abduction as a first step. Finally, we investigated whether hip hyperextension reduces the ability to elevate the femur. In our cadaver and clinical studies, releasing the superior capsule was most effective for elevating the proximal femur, so we did not continue on to observe the effects of the release of the internal obturator tendon. After the superior capsule release, the ability to elevate the femur was not diminished by hip hyperextension.
Table 1.
Reported strategy for obtaining straight access to the femoral canal in THA using a direct anterior approach
| Authors | Surgical table | Hip position | Elevator | First release | Second release | Preservation | Option |
|---|---|---|---|---|---|---|---|
| Kennon et al. (2003) [3] | Standard surgical table | Hyperextension Adduction Maximal external rotation |
Bone hook Retractors |
Tensor fasciae latae Medial capsule Posterior capsule Short external rotator tendons |
Abductor mechanism | Secondary incision | |
| Siguier et al. (2004) [12] | Judet surgical table (Tasserit, Sens, France) | 90º external rotation Hyperextension |
Pressure Retractors |
Superior capsule | Gluteus medius External rotators |
||
| Matta et al. (2005) [5] | Judet surgical table PROfx surgical table (Mizuho OSI, Union City, CA) |
90º external rotation Hyperextension Adduction |
Femoral hook Retractors |
Lateral capsule | Further capsule Obturator internus Piriformis tendon Obturator externus |
Posterior capsule External rotators Abductor tendon |
Offset broach handle |
| Nogler et al. (2006) [10] | Standard surgical table | 30º–40º hyperextension External rotation Adduction |
Retractors | Posterolateral capsule | Piriformis Superior and inferior gemelli External obturator |
Posterior capsule | Double-offset broach handle |
| Oinuma et al. (2007) [11] | Standard surgical table | Hyperextension Slight adduction 90º external rotation |
Retractors | Posterior capsule | Internal obturator Gemelli |
Piriform muscle Gluteal muscles |
Our two studies had a number of limitations. First, the cadaver study was limited by sample size due to the difficulty in obtaining cadavers in Japan as it is not culturally acceptable in our nation to donate one’s body to science, and thus it was insufficiently powered to show statistical differences among release steps. Second, cadaveric tissue may not possess the same physical and mechanical properties as in vivo tissue and may not adequately reflect the tension of muscle, tendon, and capsule. However, we used fresh cadavers, which might have compensated somewhat for any differences in mechanical properties and tension. Third, in our clinical study, the diagnosis in the majority of the hips was secondary coxarthrosis resulting from hip dysplasia. Also, our patients were slim compared with American and European patients (average height, 152.0 cm; average body weight, 53.7 kg; average BMI, 23.2 kg/m2). These structural differences might affect the soft tissue tension and thus further release of external rotators might not be required. Fourth, although many authors recommend releasing several external rotator tendons [3, 5, 10–12], we investigated only the effects of the release of the internal obturator tendon on femoral elevation. Its release had no effect on elevation in our cadaver study, and we did not need to release any external rotators in our clinical study. Further study is needed to investigate which, if any, external rotators should be released to gain additional elevation of the proximal femur in particular circumstances.
Of the minimally invasive approaches for THA, the direct anterior approach uses the intermuscular and internervous plane between the tensor fasciae latae and sartorius without intentional detachment of any muscle except for some external rotators. In our cadaver and clinical studies, release of the superior capsule was the most effective for elevation of the proximal femur with hips in 15° and 25° hyperextension. Release of the posterior capsule did not increase elevation; thus, the additional posterior capsule release is unnecessary.
In THA using the direct anterior approach, no muscle must be detached; thus, the direct anterior approach is considered truly muscle-sparing. Minimal muscle damage allows for more rapid recovery of hip function [6, 9] and reduces the risk of hip dislocation [12]. Our data show excision of the anterior capsule and release of the superior capsule enable exposure of the acetabulum and elevation of the proximal femur for straight access to the femoral canal. The additional posterior capsule release is unnecessary. Our strategy for obtaining straight access to the femoral canal is to release the superior capsule and to hyperextend the hip somewhere between 15° and 25°, because elevation was compromised by hip hyperextension after release of the superior capsule. The release of the internal rotator tendon had minor effects on the elevation. Further study is needed to investigate which, if any, external rotators should be released to obtain additional elevation of the proximal femur when the elevation is otherwise inadequate.
Acknowledgments
We thank Katharine O’Moore-Klopf, ELS, for providing editorial services.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution either has waived or does not require approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Bender B, Nogler M, Hozack WJ. Direct anterior approach for total hip arthroplasty. Orthop Clin North Am. 2009;40:321–328. doi: 10.1016/j.ocl.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Judet J, Judet R. The use of an artificial femoral head for arthroplasty of the hip joint. J Bone Joint Surg Br. 1950;32:166–173. doi: 10.1302/0301-620X.32B2.166. [DOI] [PubMed] [Google Scholar]
- 3.Kennon RE, Keggi JM, Wetmore RS, Zatorski LE, Huo MH, Keggi KJ. Total hip arthroplasty through a minimally invasive anterior surgical approach. J Bone Joint Surg Am. 2003;85(Suppl 4):39–48. doi: 10.2106/00004623-200300004-00005. [DOI] [PubMed] [Google Scholar]
- 4.Masonis JL, Bourne RB. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Relat Res. 2002;405:46–53. doi: 10.1097/00003086-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005;441:115–124. doi: 10.1097/01.blo.0000194309.70518.cb. [DOI] [PubMed] [Google Scholar]
- 6.Mayr E, Nogler M, Benedetti MG, Kessler O, Reinthaler A, Krismer M, Leardini A. A prospective randomized assessment of earlier function recovery in THA patients treated by minimally invasive direct anterior approach: a gait analysis study. Clin Biomech Bristol, Avon. 2009;24:812–818. doi: 10.1016/j.clinbiomech.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 7.Meneghini RM, Pagnano MW, Trousdale RT, Hozack WJ. Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Relat Res. 2006;453:293–298. doi: 10.1097/01.blo.0000238859.46615.34. [DOI] [PubMed] [Google Scholar]
- 8.Moskal JT, Mann JW., III A modified direct lateral approach for primary and revision total hip arthroplasty. A prospective analysis of 453 cases. J Arthroplasty. 1996;11:255–266. doi: 10.1016/S0883-5403(96)80075-1. [DOI] [PubMed] [Google Scholar]
- 9.Nakata K, Nishikawa M, Yamamoto K, Hirota S, Yoshikawa H. A clinical comparative study of the direct anterior with mini-posterior approach: two consecutive series. J Arthroplasty. 2009;24:698–704. doi: 10.1016/j.arth.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 10.Nogler M, Krismer M, Hozack WJ, Merritt P, Rachbauer F, Mayr E. A double offset broach handle for preparation of the femoral cavity in minimally invasive direct anterior total hip arthroplasty. J Arthroplasty. 2006;21:1206–1208. doi: 10.1016/j.arth.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Oinuma K, Eingartner C, Saito Y, Shiratsuchi H. Total hip arthroplasty by a minimally invasive, direct anterior approach. Oper Orthop Traumatol. 2007;19:310–326. doi: 10.1007/s00064-007-1209-3. [DOI] [PubMed] [Google Scholar]
- 12.Siguier T, Siguier M, Brumpt B. Mini-incision anterior approach does not increase dislocation rate: a study of 1037 total hip replacements. Clin Orthop Relat Res. 2004;426:164–173. doi: 10.1097/01.blo.0000136651.21191.9f. [DOI] [PubMed] [Google Scholar]