Abstract
Background
Anteversion of an acetabular component often is difficult to ascertain in patients with THA in whom excessively anteverted or retroverted femurs may result in limited ROM or risk of dislocation. Restriction of motion, however, is determined by the combination of version of both components.
Questions/purposes
We therefore determined the combined anteversion values that provide adequate ROM. We varied acetabular version by differing implantations and varied femoral version with modular necks.
Methods
ROM was tested by changing cup anteversion after setting the femoral version to 20° or 60° anteversion or 20° retroversion. The angle of the modular neck was adjusted in 11 increments of 5° each. Range of internal rotation (IR) at 90° flexion, external rotation (ER) at 0° extension, and flexion (Flex) were measured when any impingement occurred before dislocation. We defined a required ROM as having 40° IR, 30° ER, and 110° Flex.
Results
At 60° anteversion, ER was less than 10° even when the acetabular component was set at 10° retroversion because of posterior impingement. When a modular neck with 25° retroversion was used, ER improved to greater than 30°. At 20° retroversion, IR was 31° even when the acetabular component was opened to 35° anteversion. IR improved to 34° and 40° with 20° and 25° anteverted modular necks, respectively.
Conclusions and Clinical Relevance
In cases with excessive femoral anteversion or retroversion, the required ROM could not be achieved by simply changing the version of acetabular components. The adjustment of femoral versions using the modular necks allowed additional improvement of ROM.
Introduction
Dislocation is one of the most frequent complications after THA with an incidence of 0.6% to 11% in the early postoperative period [10, 30, 32]. Factors affecting dislocation include patient characteristics, variations in surgical techniques such as placement of the implant and soft tissue repair [24], and the implant design, including the head/neck ratio [1, 18, 22]. Of these factors, between 13% and 30% of dislocations reportedly are caused by implant malpositioning [6, 11].
One study suggests optimal placement of the acetabular component is 45° ± 10° abduction and 20° ± 10° anteversion [3]. Lewinnek et al. also reported a similar safe zone of 45° ± 10° abduction and 15° ± 10° anteversion; the frequency of dislocation increased substantially when the implant position was outside this zone [16]. In one study, approximately 15° anteversion for the femoral component is recommended [11].
Several authors suggest combined anteversion (CA), which is the sum of anteversion of the femoral and acetabular components, should be considered when implanting hip components [15, 25]. Jolles et al. reported the dislocation risk was 6.9 times greater if CA fell outside the range of 40° to 60° [15]. A CA ranging from 20° to 30° for males and approximately 45° for females was recommended in another study [25]. However, these studies did not consider the CA in patients with abnormal femoral versions. Femoral anteversion is increased in developmental dysplasia of the hip to a range of 35° to 60° [2, 13, 29], whereas anteversion typically is decreased in patients with osteoarthritis resulting from slipped capital femoral epiphysis or Legg-Calvé-Perthes’ disease [8, 9].
When the acetabular component is placed at 20° anteversion, the risk of anterior dislocation increases with excessive anteversion, whereas the risk of posterior dislocation is increased in those with retroversion [17]. It is critical to carefully adjust anteversion of the acetabular or femoral components; however, there are limitations to the degree of adjustment possible using the nonmodular components because these must fit bone and be covered by surrounding bone.
We therefore (1) determined the CA values that would satisfy the required ROM in normally and excessively anteverted or retroverted femurs, and (2) assessed the improvements in ROM using modular necks in cases where sufficient ROM otherwise could not be achieved.
Materials and Methods
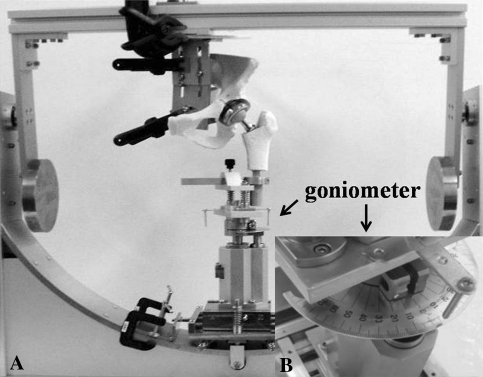
We developed a THA model based on that described by Amstutz et al. [1] (Fig. 1A). The femur was placed in the valgus position, 7° against the functional axis, whereas the center of the femoral head was set at the rotation center. The pelvis was fixed so that the plane formed by the anterior-superior iliac spine and pubic symphysis was perpendicular to the ground and parallel to the frame of the THA model. A cementless THA (JMM, Osaka, Japan) was inserted into a femoral model (Sawbones, Vashon, WA) using a standard technique. The apparatus had a built-in goniometer to measure ROM (Fig. 1B). This apparatus provided a precision of ± 1° in each measurement. In all cases, a femoral head with a diameter of 28 mm and a neck length of +3 mm were used. Springs were placed at the femoral installation site with a force of 20 N to keep the acetabular and femoral components engaged. The model could be moved in six dimensions (flexion, extension, abduction, adduction, internal rotation, and external rotation).
Fig. 1A–B.
(A) The THA model, which can be moved in six dimensions (flexion, extension, abduction, adduction, internal rotation, and external rotation), allows observation of bone-bone impingement and implant impingement. (B) A goniometer was set to this apparatus with the precision of ± 1° in each measurement. In all measurements, a femoral head with a 28-mm diameter and +3 mm neck length was used. Springs were placed at the femoral installation site with a force of 20 N to keep the acetabular and femoral components attached. A 52-mm acetabular component was fixed at 45° abduction.
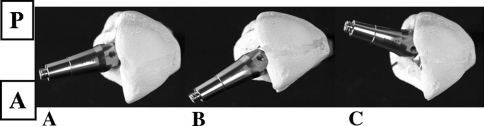
To compare the ROM of a normally anteverted femur with those of femurs with unusual anteversion, we tested three femoral anteversion values (described subsequently). To examine the effects of modular necks on insufficient ROM, modular necks ranging from 25° anteversion to 25° retroversion also were tested. Three different femoral component anteversion values were used in this study: normal anteversion of 20°, excessive anteversion of 60°, and 20° retroversion (Fig. 2). These anteversion values were measured against the posterior condylar line of the knee. Anteversion of the acetabular component was adjusted among six positions: 35°, 30°, 20°, 10°, 0°, and −10°. Accordingly, CA ranged between 95° and −30°. Anteversion of the acetabular component was the radiographic anteversion in this study. A 52-mm acetabular component was fixed at 45° abduction.
Fig. 2A–C.
Femoral anteversion settings of (A) 20° and (B) 60°, and (C) retroversion of 20° are shown. A = anterior, P = posterior.
ROM was recorded at the point when any impingement occurred before dislocation. Impingement was defined as the visual contact between the femoral component or bone and acetabular component or bone in this study. In addition, we recorded the site where impingement occurred. We determined three ROMs: (1) internal rotation at 90° flexion and 0° abduction (IR); (2) external rotation at 0° extension and abduction (ER); and (3) flexion at 0° adduction and abduction (Flex). All the measurements were performed three times; the average was used as the ROM. As a reference, we also defined a required ROM as the range of hip motion required for activities of daily living [21, 28, 31]. The required ROM was considered satisfied with values greater than 110° Flex, 40° IR, and 30° ER.
The version of the modular neck was varied from 25° anteversion to 25° retroversion in 11 increments of 5° each (Fig. 3). The cup was fixed at 20° anteversion when a modular neck was used. The ROM was determined by changing the angle in six increments from 0° to 25° retroversion for cases with 60° femoral anteversion and from 0° to 25° anteversion for cases with 20° femoral retroversion.
Fig. 3.
The version of the modular neck was varied from 25° anteversion to 25° retroversion in 11 increments of 5°. A = anterior; P = posterior.
Results
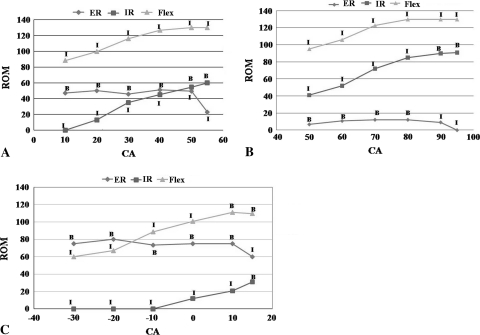
In the case with 20° femoral anteversion, CA ranging from 30° to 50° satisfied the required ROM without using the modular necks (Fig. 4A). In contrast, the required ROM was not achieved in the cases with 60° femoral anteversion or 20° femoral retroversion (Fig. 4B–C). At 60° femoral anteversion, ER was less than 10° even when the acetabular component was set at 10° retroversion, because the impingement occurred between the posterior acetabulum and the greater trochanter. Flex and IR reached the required ROM with minimum anteversion of the acetabular component (10° retroversion, 50° CA). At 20° femoral retroversion, impingement occurred between the anterior acetabular and femoral component with 101° flexion and 12° IR of the hip when acetabular component anteversion was set at 20°. The Flex and IR achieved were 109° and 31°, respectively, with maximum anteversion of the acetabular component (35° anteversion, 15° CA). ER was within the required ROM under all conditions.
Fig. 4A–C.
(A) CA ranging from 30° to 50° satisfied the required ROM without using the modular necks in the case at 20° anteversion. (B) At 60° anteversion, ER was less than 10° even when the acetabular component was set at 10° retroversion owing to the posterior bone impingement. (C) At 20° retroversion, the anterior bone and implant impingement led to the insufficient Flex and IR. ER = external rotation at 0° extension and abduction; IR = internal rotation at 90° flexion and 0° abduction; Flex = flexion at 0° adduction and abduction; required ROM = required range of motion; B = bone to bone impingement; I = implant to implant impingement; CA = combined anteversion.
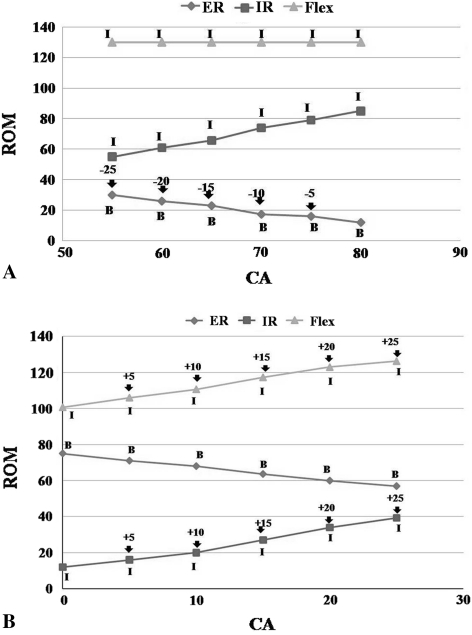
Retroverted modular necks improved ROM when femoral anteversion was 60° (Fig. 5A). The effects were angle-dependent and the posterior impingement was delayed. ROM eventually reached 30° when a modular neck with 25° was used with acetabular components anteversion of 20°. Flex and IR were within the required ROM for all modular necks. Anteverted modular necks delayed anterior impingement and improved ROM with 20° femoral retroversion (Fig. 5B). Flex improved to 115° and 124° with 20° and 25° anteverted modular necks, respectively. IR also improved by 34° and 40°, respectively. ER was within the required ROM for all modular necks.
Fig. 5A–B.
(A) Retroverted modular necks improved ROM at 60° femoral anteversion. The effects were in an angle-dependent manner. ROM eventually reached 30° when a modular neck with 25° was used. Flex and IR were within the required ROM with any modular neck. (B) Anteverted modular necks delayed anterior impingement and improved ROM at 20° femoral retroversion. Flex and IR improved to 124° and 40°, respectively, with 25° modular necks. ER was within the required ROM for all modular necks. ER = external rotation at 0° extension and abduction; IR = internal rotation at 90° flexion and 0° abduction; Flex = flexion at 0° adduction and abduction; B = bone to bone impingement; I = implant to implant impingement; CA = combined anteversion; ROM = range of motion. Arrows and indicated numbers were the versions of modular necks.
Discussion
Anteversion of the acetabular component is often difficult to determine in cases with excessively anteverted or retroverted femurs that may result in limited ROM after THA.
In this study, we determined the CA values that would satisfy the required ROM in normally and excessively anteverted or retroverted femurs and assessed improvements in ROM using modular necks in cases in which sufficient ROM could not be achieved.
This study had several limitations. First, the THA model we used did not have surrounding soft tissue such as muscles and the joint capsule. They provide substantial contributions to ROM when impingement occurs; however, it is difficult to emulate these effects in an experimental THA model, and therefore we focused on the effect of component positioning on ROM. Second, our data were derived from a limited number of anteversion settings of the acetabular and femoral components. A three-dimensional simulation study may provide the additional advantage with more design parameters. However, these advantages are based on the reliable software that makes it possible to measure not only the ROM, but also impingement point with modular necks. As far as we know, this kind of software is not commercially available; therefore, we performed an experimental study using a THA model. Third, the measured ROM in this study was the range until impingement, not until dislocation. We did not assess the effects of jumping distance of the femoral heads [18]. The jumping distance is determined mainly by the head size. Therefore, the ROM values we found were somewhat smaller than the range of hip motion required for daily living as defined in previous studies [5, 14, 21, 28, 31].
CA ranging from 30° to 50° satisfied the required ROM without requiring modular necks for 20° femoral anteversion. These observations with normal anteversion were similar to the results of previous studies. Recommended CA values range from 30° to 60° [19, 31]. In contrast, at 60° femoral anteversion, changing anteversion of the acetabular component did not achieve the required ROM. The posterior greater trochanter is located close to the ischium in these cases; thus, the frequency of anterior dislocation reportedly was greater in these cases [26]. The impingement between the posterior neck and liner was observed when the acetabular component was set at 35° anteversion. It changed to posterior bone to bone impingement when the acetabular component was set in a posterior direction. However, ER was always less than 20° even when the acetabular component was set at 10° retroversion in this study. The required ROM also was not achieved with 20° femoral retroversion. Because the greater trochanter is located close to the anterior acetabulum in these cases, flexion and internal rotation resulted in early impingement and posterior dislocation using standard cementless femoral components [17]. IR and flexion were less than 10° and 100°, respectively, with anteversion of the acetabular component less than 20° owing to the implant impingement. Even when the acetabular component was set at 35° anteversion, IR and flexion did not achieve the ROM because of bony impingement.
Several studies have addressed the situation with unusual femoral anteversion [25, 31]. Decreasing anteversion of the acetabular component in cases with excessive anteversion has been attempted; however, that failed to result in the required ROM as shown in our study. In these cases, therefore, altering the femoral anteversion was believed to be effective for achieving the required ROM. This procedure included reducing femoral anteversion using an undersized cement stem [7, 20], using a cementless stem in combination with femoral osteotomy [12, 23, 33], and using a modular prosthesis in which the femoral version could be changed voluntarily. Altering femoral anteversion also changes the dynamic environment of the hip. Some concerns may arise regarding the effect of altered surrounding muscles on hip function. However, previous studies showed these adjustments of femoral versions usually resulted in improved hip function, including gait and ROM [4, 27]. We found the greater the extent to which modular necks achieved normal femoral anteversion, the better the ROM in cases with excessively anteverted and retroverted femurs. This type of femoral component could allow us to adjust femoral anteversion without any additional procedures such as femoral osteotomy and would be suitable for cases with unusual femoral versions.
The required ROM could not be achieved only by changing the version of acetabular components in cases with excessive anteversion or retroversion. The adjustment of femoral version using modular necks allows for additional improvement of ROM.
Acknowledgments
We thank Drs Takuaki Yamamoto, Taro Mawatari, and Goro Motomura for their kind opinions and advice for this study.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Amstutz HC, Lodwig RM, Schurman DJ, Hodgson AG. Range of motion studies for total hip replacements: a comparative study with a new experimental apparatus. Clin Orthop Relat Res. 1975;111:124–130. doi: 10.1097/00003086-197509000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Argenson JN, Flecher X, Parratte S, Aubaniac JM. Anatomy of the dysplastic hip and consequences for total hip arthroplasty. Clin Orthop Relat Res. 2007;465:40–45. doi: 10.1097/BLO.0b013e3181576052. [DOI] [PubMed] [Google Scholar]
- 3.Barrack RL, Lavernia C, Ries M, Thornberry R, Tozakoglou E. Virtual reality computer animation of the effect of component position and design on stability after total hip arthroplasty. Orthop Clin North Am. 2001;32:569–577. doi: 10.1016/S0030-5898(05)70227-3. [DOI] [PubMed] [Google Scholar]
- 4.Biant LC, Bruce WJ, Assini JB, Walker PM, Walsh WR. Primary total hip arthroplasty in severe developmental dysplasia of the hip: ten-year results using a cementless modular stem. J Arthroplasty. 2009;24:27–32. doi: 10.1016/j.arth.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 5.D’Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW., Jr The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82:315–321. doi: 10.2106/00004623-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Daly PJ, Morrey BF. Operative correction of an unstable total hip arthroplasty. J Bone Joint Surg Am. 1992;74:1334–1343. [PubMed] [Google Scholar]
- 7.Dunn HK, Hess WE. Total hip reconstruction in chronically dislocated hips. J Bone Joint Surg Am. 1976;58:838–845. [PubMed] [Google Scholar]
- 8.Eijer H, Berg RP, Haverkamp D, Pécasse GA. Hip deformity in symptomatic adult Perthes’ disease. Acta Orthop Belg. 2006;72:683–692. [PubMed] [Google Scholar]
- 9.Gelberman RH, Cohen MS, Shaw BA, Kasser JR, Griffin PP, Wilkinson RH. The association of femoral retroversion with slipped capital femoral epiphysis. J Bone Joint Surg Am. 1986;68:1000–1007. [PubMed] [Google Scholar]
- 10.Hedlundh U, Ahnfelt L, Hybbinette CH, Wallinder L, Weckström J, Fredin H. Dislocations and the femoral head size in primary total hip arthroplasty. Clin Orthop Relat Res. 1996;333:226–233. doi: 10.1097/00003086-199612000-00024. [DOI] [PubMed] [Google Scholar]
- 11.Hedlundh U, Sanzén L, Fredin H. The prognosis and treatment of dislocated total hip arthroplasties with a 22 mm head. J Bone Joint Surg Br. 1997;79:374–378. doi: 10.1302/0301-620X.79B3.7149. [DOI] [PubMed] [Google Scholar]
- 12.Holtgrewe JL, Hungerford DS. Primary and revision total hip replacement without cement and with associated femoral osteotomy. J Bone Joint Surg Am. 1989;71:1487–1495. [PubMed] [Google Scholar]
- 13.Jacobsen S, Rømer L, Søballe K. Degeneration in dysplastic hips: a computer tomography study. Skeletal Radiol. 2005;34:778–784. doi: 10.1007/s00256-005-0019-7. [DOI] [PubMed] [Google Scholar]
- 14.Johnston RC, Smidt GL. Hip motion measurements for selected activities of daily living. Clin Orthop Relat Res. 1970;72:205–215. [PubMed] [Google Scholar]
- 15.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17:282–288. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 16.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 17.Malik A, Maheshwari A, Dorr LD. Impingement with total hip replacement. J Bone Joint Surg Am. 2007;89:1832–1842. doi: 10.2106/JBJS.F.01313. [DOI] [PubMed] [Google Scholar]
- 18.Matsushita A, Nakashima Y, Jingushi S, Yamamoto T, Kuraoka A, Iwamoto Y. Effects of the femoral offset and the head size on the safe range of motion in total hip arthroplasty. J Arthroplasty. 2009;24:646–651. doi: 10.1016/j.arth.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 19.McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970;52:148–159. [PubMed] [Google Scholar]
- 20.Mendes DG. Total hip arthroplasty in congenital dislocated hips. Clin Orthop Relat Res. 1981;161:163–179. [PubMed] [Google Scholar]
- 21.Miki H, Yamanashi W, Nishii T, Sato Y, Yoshikawa H, Sugano N. Anatomic hip range of motion after implantation during total hip arthroplasty as measured by a navigation system. J Arthroplasty. 2007;22:946–952. doi: 10.1016/j.arth.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Morrey BF. Instability after total hip arthroplasty. Orthop Clin North Am. 1992;23:237–248. [PubMed] [Google Scholar]
- 23.Paavilainen T, Hoikka V, Paavolainen P. Cementless total hip arthroplasty for congenitally dislocated or dysplastic hips: technique for replacement with a straight femoral component. Clin Orthop Relat Res. 1993;297:71–81. [PubMed] [Google Scholar]
- 24.Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202–1210. doi: 10.2106/00004623-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Ranawat CS, Maynard MJ. Modern techniques of cemented total hip arthroplasty. Tech Orthop. 1991;6:17–25. doi: 10.1097/00013611-199109000-00004. [DOI] [Google Scholar]
- 26.Ritter MA. Dislocation and subluxation of the total hip replacement. Clin Orthop Relat Res. 1976;121:92–94. [PubMed] [Google Scholar]
- 27.Sakai T, Sugano N, Ohzono K, Nishii T, Haraguchi K, Yoshikawa H. Femoral anteversion, femoral offset, and abductor lever arm after total hip arthroplasty using a modular femoral neck system. J Orthop Sci. 2002;7:62–67. doi: 10.1007/s776-002-8418-7. [DOI] [PubMed] [Google Scholar]
- 28.Seki M, Yuasa N, Ohkuni K. Analysis of optimal range of socket orientations in total hip arthroplasty with use of computer-aided design simulation. J Orthop Res. 1998;16:513–717. doi: 10.1002/jor.1100160418. [DOI] [PubMed] [Google Scholar]
- 29.Sugano N, Noble PC, Kamaric E, Salama JK, Ochi T, Tullos HS. The morphology of the femur in developmental dysplasia of the hip. J Bone Joint Surg Br. 1998;80:711–719. doi: 10.1302/0301-620X.80B4.8319. [DOI] [PubMed] [Google Scholar]
- 30.White RE, Jr, Forness TJ, Allman JK, Junick DW. Effect of posterior capsular repair on early dislocation in primary total hip replacement. Clin Orthop Relat Res. 2001;393:163–167. doi: 10.1097/00003086-200112000-00019. [DOI] [PubMed] [Google Scholar]
- 31.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–821. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 32.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]
- 33.Zadeh HG, Hua J, Walker PS, Muirhead-Allwood SK. Uncemented total hip arthroplasty with subtrochanteric derotational osteotomy for severe femoral anteversion. J Arthroplasty. 1999;14:682–688. doi: 10.1016/S0883-5403(99)90223-1. [DOI] [PubMed] [Google Scholar]