Abstract
Background
There is emerging evidence that even mild slipped capital femoral epiphysis leads to early articular damage. Therefore, we have begun treating patients with mild slips and signs of impingement with in situ pinning and immediate arthroscopic osteoplasty.
Description of Techniques
Surgery was performed using the fracture table. After in situ pinning and diagnostic arthroscopy, peripheral compartment access was obtained and head-neck osteoplasty was completed.
Methods
Between March 2008 and August 2009, three male patients (age range, 11–15 years; BMI, 22–31 kg/m2) presented with slip angles between 15º and 30º. All were ambulatory without assistance but had 2 to 12 weeks of hip and/or knee pain, limited motion and a positive impingement test. Postoperatively, patients were assessed at 6 weeks; 3 and 6 months; then every 6 months for the first two years. Hip motion, epiphyseal-metaphyseal offsets and alpha angles were determined. Patients completed the UCLA activity scale at latest followup that ranged from 6 to 23 months.
Results
Arthroscopic evaluation revealed labral fraying, acetabular chondromalacia, and a prominent metaphyseal ridge. At last followup, each was pain-free and had returned to unrestricted activities. Hip motion improved in all and none demonstrated clinical impingement. Radiographs showed normalized epiphyseal-metaphyseal offsets and alpha angles.
Conclusions
In situ pinning with arthroscopic osteoplasty can limit impingement after mild slipped capital femoral epiphysis. Due to limited followup, we are unable to say whether this protocol reduces subsequent articular damage. Although we recommend performing these procedures concomitantly, they can be performed in a staged fashion, especially since hip arthroscopy following an epiphyseal slip can be challenging.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The natural history of mild slipped capital femoral epiphysis (SCFE) has traditionally been believed to follow a benign course. Several studies with followup periods between 31 and 41 years have suggested low rates of osteoarthrosis and functional disability [3, 7, 8]. Consistent with these reports, some surgeons advocate in situ pinning alone for mild SCFE [2, 20]. However, more recent studies have questioned whether the natural history of mild slips after in situ stabilization is truly benign. Reports of both arthroscopic [13, 15] and open [17–19, 25] evaluation of hips after mild SCFE suggests rates of acetabular cartilage and labral damage between 75% and 100%. Two studies [10, 12] with intermediate followup periods of 6.1 to 14.4 years reported pain in one-third of hips with slip angles between 0º and 31º as well as decreased Tegner and Lysholm scores compared to similarly aged counterparts. Computer models [22, 24] have demonstrated “inclusion”-type impingement [24] for mild to moderate slips as the prominent metaphysis enters the hip and “impaction”-type impingement as the femoral neck abuts the acetabular rim in more severe SCFE.
Since 1996, the senior authors (ML and RG) have treated, all moderate to severe slips with subcapital realignment [19]. Based on the increasing evidence of early articular damage after mild SCFE, one of the authors (ML) began treating all mild slips with in situ pinning and immediate arthroscopic head-neck osteoplasty in 2008. It is believed that by removing the prominent metaphyseal bone and reestablishing the head-neck offset, arthroscopic osteoplasty will eliminate impingement and reduce subsequent articular damage.
The purposes of this article are to present the surgical technique, describe the arthroscopic findings and report the early levels of pain, function and hip motion as well as alpha angles and epiphyseal-metaphyseal offsets for the first three patients treated with this protocol.
Surgical Technique
The patients were positioned supine on a standard fracture table. Both feet were inserted in secure, well-padded boots and a large, compressible perineal post was placed. We routinely used an adjustable hydraulic leg holder for the arthroscopic portion of the procedure. Using fluoroscopic guidance, a 6.5-mm partially threaded screw was driven into the center of the epiphysis perpendicular to the physis [2].
After in situ fixation, the legs were positioned in 40° of abduction, 0° to 20° of flexion, and maximal internal rotation. We applied gentle traction to the abducted operative hip with slight countertraction on the nonoperative hip. The operative hip was subsequently adducted to obtain sufficient joint distraction and verified fluoroscopically; distraction is easily achieved in most children. Standard anterolateral (AL) and midanterior (MA) portals were established [5, 6]. We used a Beaver blade to perform an “interportal” capsulotomy from the MA to the AL portal. The edges of the incised capsule were débrided with an arthroscopic shaver.
We performed a standard diagnostic arthroscopy of the central compartment. Labral and chondral pathology were evaluated and addressed. With the camera in the MA portal, attention was turned to the peripheral compartment. The retinacular branches of the medial femoral circumflex artery were visualized while traction is maintained and the hip extended. We then extended the capsulotomy along the anterolateral neck in a T configuration. Taking care to avoid the retinacular vessels, the Beaver blade was advanced toward the intertrochanteric line to provide additional exposure of the head-neck junction.
The anterior neck periosteum was removed with the shaver to further delineate the impingement lesion. Unlike hip arthroscopy for idiopathic femoroacetabular impingement, hyperextension of the hip is frequently required to visualize and treat the proximal metaphysis. Fluoroscopy was used to confirm the physeal location and identify a safe starting point for the osteoplasty. A 5.5-mm hooded high-speed burr was inserted through the AL portal and anterosuperior head-neck reshaping is performed. We used intermittent fluoroscopic imaging to confirm sufficient bone removal. The integrity of the retinacular vessels was visually assessed periodically during the osteoplasty.
Traction was released and the hip brought into 45º of flexion and 30º of abduction. With the camera in the MA portal, we identified the anteroinferior margin of the deformity. The inferior retinacula of Weitbrecht defines the anteroinferior limit of resection. The shaver was used to remove any remaining periosteum and the 5.5-mm burr used to complete the osteoplasty. We carried the resection to the level of the physis. Fluoroscopic imaging confirmed adequacy of the osteoplasty and restoration of a sufficient femoral head-neck offset. Dynamic flexion and extension of the hip under direct arthroscopic visualization is used to further verify the adequacy of resection. The camera was removed and portals are closed with absorbable sutures.
The patients were restricted to toe-touch weightbearing with crutches for 6 weeks and then advanced to full weightbearing. Gentle ROM was initiated immediately after surgery and progressed as tolerated. Care was taken to limit the aggressiveness of physical therapy so as not to incite hip flexor tendonitis. We permitted return to full, unrestricted activities at 6 months.
Patients and Methods
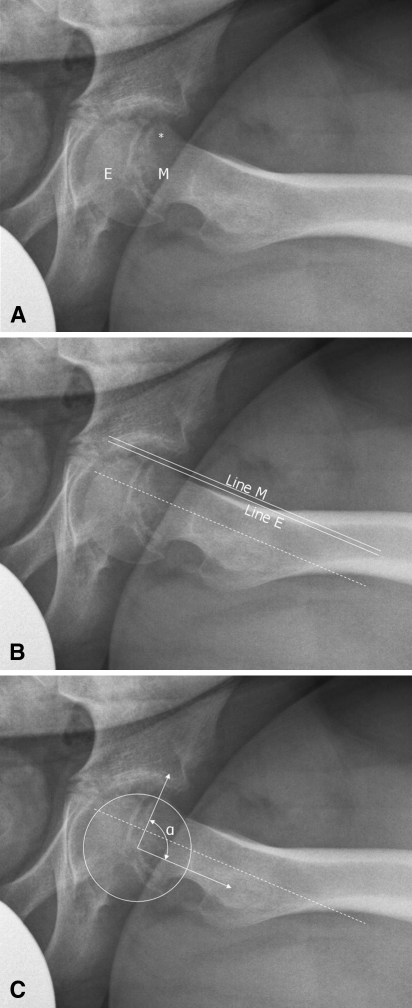
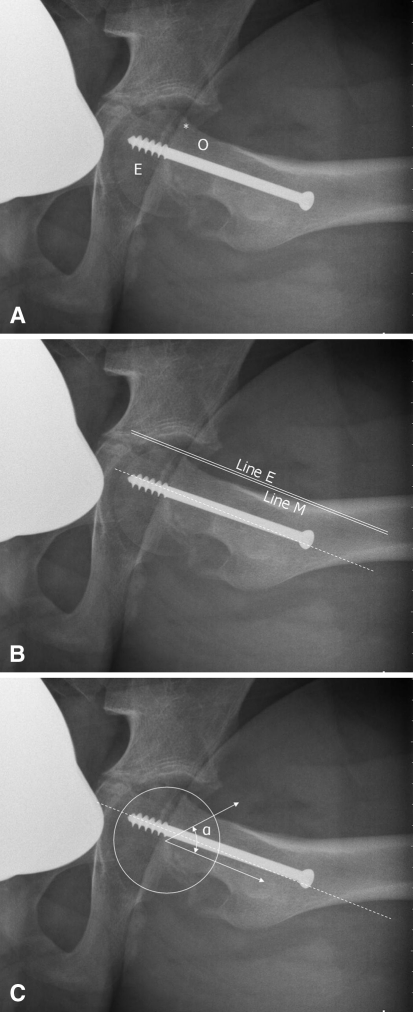
Three children presented to our institution with SCFE and a slip angle [26] between 15º and 30º between March 2008 and August 2009 (Table 1). All patients were able to ambulate without assistance but had been provided crutches by their referring physicians. Each had groin pain with ambulation, ranging in duration from 2 weeks to 3 months. Hip flexion and internal rotation were limited in all patients (Table 1). Impingement testing [21] consisting of hip flexion, adduction and internal rotation produced pain in each of the three hips. Frog-leg lateral radiographs showed Southwick slip angles of 18º, 23º, and 18º (Fig. 1A). The epiphyseal-metaphyseal offset was measured on the frog-leg lateral view as the difference between a line drawn along the anterior edge of the epiphysis parallel to the femoral neck and a line drawn along the proximal-anterior edge of the metaphysis also parallel to the femoral neck (Fig. 1B). A positive value indicates the epiphysis is more anterior, whereas a negative value indicates the metaphysis is more anterior. This technique is analogous to that previously described for determination of the head-neck offset [11]. Preoperative epiphyseal-metaphyseal offsets were determined to be −6.4 mm, −3.5 mm, and −4.5 mm (Table 2). Alpha angles were measured on the frog-lateral radiographs using a slight modification to the technique previously described [23]. As a result of the translation of the femoral head, the alpha angle was based on a line drawn through the center of the femoral head and parallel to the femoral neck instead of a line through the femoral neck (Fig. 1C). The preoperative alpha angles were measured as 80º, 90º, and 88º (Table 2). All patients underwent surgery within 48 hours of presentation.
Table 1.
Summary of demographic and clinical data for patients at initial presentation, intraoperatively, and at most recent followup
| Patient/hip data | Patient 1 | Patient 2 | Patient 3 |
|---|---|---|---|
| Initial presentation | |||
| Affected hip | Right | Left | Right |
| Southwick [26] slip angle | 18º | 23º | 18º |
| Gender | Male | Male | Male |
| Age at presentation | 11 years | 12 years | 15 years |
| Duration of symptoms | 3 months | 2 months | 2 weeks |
| BMI (kg/m2) | 21.5 | 28.6 | 30.9 |
| Obligate ER | + | − | + |
| Impingement test | + | + | + |
| Hip flexion | 90º | 90º | 85º |
| IR in flexion | Absent | Absent | ↓ 20º from L |
| Intraoperative findings | |||
| Extent of chondrolabral damage (clock phase system) | 12 to 3 | 11 to 3 | 12 to 2 |
| Head-neck junction | P | P | S |
| Most recent followup | |||
| Duration of followup | 23 months | 21 months | 6 months |
| Symptoms | None | None | None |
| Obligate ER | − | − | − |
| Impingement test | − | − | − |
| Hip flexion | 120º | 100º | 90º |
| IR in flexion | ↓ 10º from L | ↓ 10º from R | ↓ 10º from L |
| UCLA activity scale score | 9 | 9 | 8 |
BMI = body mass index; IR = internal rotation; ER = external rotation; P = prominences; S = separation; extent of chondrolabral damage shown according to clock face of right hip.
Fig. 1A–C.
Frog-leg lateral radiographs of the hip show posterior tilt and translation of the epiphysis (E) with anterior prominence (*) of the proximal metaphysis (M). (A) Left hip of Patient 2. (B) Epiphyseal-metaphyseal offset of left hip of Patient 2. (C) Alpha angle of left hip of Patient 2. Dashed line = line along center of femoral neck; Line E = line along anterior epiphysis parallel to femoral neck; Line M = line along anterior metaphysis parallel to femoral neck; α = alpha angle.
Table 2.
Summary of preoperative and postoperative radiographic data
| Radiographic measure | Patient 1 | Patient 2 | Patient 3 |
|---|---|---|---|
| E-M offset | |||
| Preoperative | −6.4 mm (−2.0 mm) | −3.5 mm (+2.0 mm) | −4.5 mm (0.0 mm) |
| Postoperative | −1.2 mm (−2.0 mm) | +2.4 mm (+2.0 mm) | 0.0 mm (0.0 mm)* |
| Correction | 5.2 mm | 5.9 mm | 4.5 mm |
| Alpha angle | |||
| Preoperative | 80º (45º) | 90º (48º) | 88º (44º) |
| Postoperative | 42º (42º) | 50º (43º) | 54º (50º)* |
| Correction | 38º | 40º | 34º |
* Postoperative measurements for contralateral unaffected hip of Patient 3 were determined from cross-table lateral radiograph because frog-lateral was not obtained; values for the contralateral unaffected hip are shown in parentheses; E-M = epiphyseal-metaphyseal.
Postoperatively, patients were seen in followup at 6 weeks, 3 months, 6 months, and then every 6 months for the first two years. Physical examination at each visit included evaluation of gait, hip ROM testing, and assessment for hip impingement. AP pelvic and frog and/or cross-table lateral radiographs were obtained at each visit. The epiphyseal-metaphyseal offset and alpha angle were again determined from the frog-lateral radiographs. Patients completed the UCLA activity scale [1] at their most recent followup appointment, which ranged from 6 to 23 months postoperatively.
Results
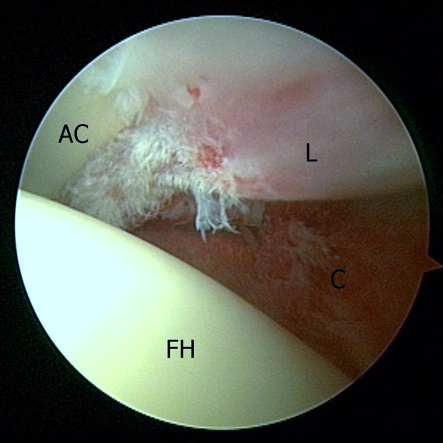
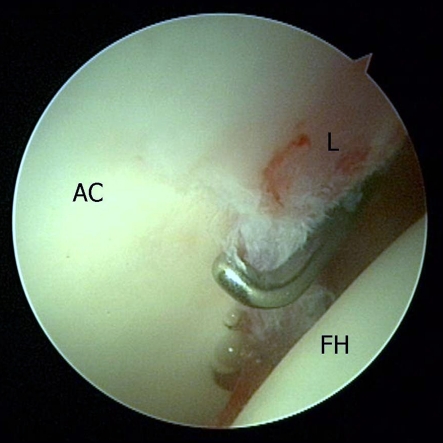
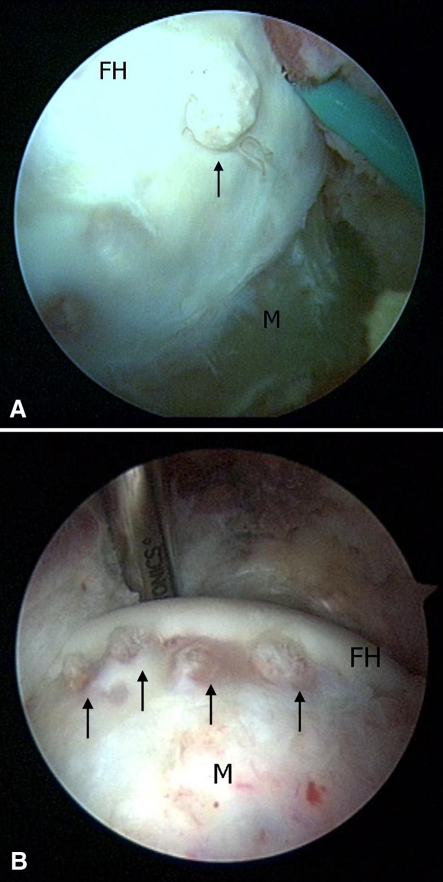
Diagnostic arthroscopy revealed synovitis with anterolateral labral hyperemia and fraying in all three hips (Fig. 2; Table 1). A narrow band of chondromalacia could be probed adjacent to the damaged labrum (Fig. 3). In two of the hips (Patients 1, 2), multiple punctate prominences were seen projecting anteriorly along the band of separation between the epiphysis and metaphysis (Fig. 4A–B). In the third hip (Patient 3), with a shorter duration of symptoms, clear separation could be seen between the slipped epiphysis and metaphysis (Fig. 5). Resection of the prominent anterior metaphysis with reshaping of the head-neck junction was performed to the level of the physis in all hips (Fig. 6).
Fig. 2.
Arthroscopic view of the right hip of Patient 1 shows fraying and hyperemia of the anterior labrum (L). Synovitis is present on the articular side of the joint capsule (C). FH = femoral head; AC = acetabular cartilage.
Fig. 3.
Arthroscopic view of the right hip of Patient 1 with a probe placed on softened but intact acetabular cartilage (AC). FH = femoral head (FH); L = labrum.
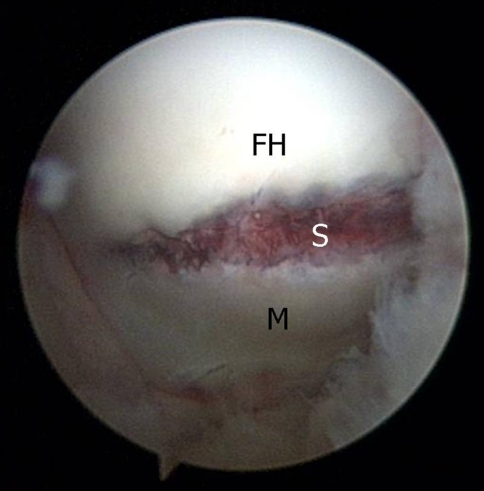
Fig. 4A–B.
Arthroscopic view of the anterior head-neck junction shows abrasive prominences (arrows) projecting anteriorly along the band of epiphyseal-metaphyseal separation. (A) Right hip of Patient 1. (B) Left hip of Patient 2. FH = femoral head; M = metaphysis.
Fig. 5.
Arthroscopic view of the left hip of Patient 3 shows the anterior separation (S) between the femoral head (FH) and metaphysis (M).
Fig. 6.
Arthroscopic view of the left hip of Patient 3 shows resection of the proximal anterior metaphysis (M). Resection is carried proximally to the level of the physis (P). FH = femoral head.
At most recent followup of 6 to 23 months postoperatively, all three patients were free of pain and had returned to full activities without pain. ROM testing produced no pain and demonstrated full flexion but showed slightly reduced internal rotation compared with the contralateral side (Table 1). Impingement testing was negative in all subjects and none had obligate external rotation. Frog-leg lateral radiographs showed a recontoured head-neck junction (Fig. 7A) and epiphyseal-metaphyseal offsets (Fig. 7B) of −1.2 mm, +2.4 mm, and 0.0 mm (Table 2), indicating an average offset correction of 5.2 mm. Alpha angles (Fig. 7C) were determined to be 42º, 50º, and 54º (Table 2), showing an average alpha angle correction of 37º. UCLA activity scores for the three patients were 9, 9, and 8 (Table 1).
Fig. 7A–C.
Frog-leg lateral hip radiographs demonstrate in situ pinning of the epiphysis (E) and head-neck osteoplasty (O). The proximal anterior metaphysis (*) is no longer prominent. (A) Left hip of Patient 2. (B) Corrected epiphyseal-metaphyseal offset of left hip of Patient 2. (C) Corrected alpha angle of the left hip of Patient 2. Dashed line = line along center of femoral neck; Line E = line along anterior epiphysis parallel to femoral neck; Line M = line along anterior metaphysis parallel to femoral neck; α = alpha angle.
Discussion
Based on favorable outcomes from long-term studies [3, 7, 8], the standard treatment for mild SCFE has become in situ pinning. More recently, this protocol has been called into question by reports that even mild slips may lead to early acetabular labrum and cartilage damage [10, 12, 17]. Reports from several centers suggest treatment of mild SCFE should not only prevent further slippage, but also address potential impingement [12, 17–19, 25, 28]. The purposes of this article were to describe a novel treatment protocol for mild SCFE, report our initial experience with this technique, and present clinical evidence for and a conceptual basis to support additional surgical intervention after mild slips.
Our study is limited by only three patients and short followup. We therefore cannot say whether this treatment protocol will produce superior long-term function or reduce the risk of OA compared to in situ pinning alone. However, we believe the evidence [13, 17, 18, 25] indicating mild slips produce cartilage damage warrants intervention before patients become symptomatic and irreversible articular injury has resulted. In addition, the pathomechanical understanding of how this damage occurs [17, 22, 24] compels us to consider such treatment even before long-term results have accumulated. Although the natural history of articular cartilage damage is not clearly understood, we believe it is likely to progress unless the offending lesion is eliminated.
In support of in situ pinning alone, Boyer et al. [3] presented a series of 149 slips followed an average of 31 years. For patients treated without realignment, Iowa Hip Rating scores were 93 for mild and moderate slips and 85 for severe slips. Moderate or advanced arthrosis was seen in 6 of 39 mild slips, 3 of 22 moderate slips, and two of five severe slips. The realignment group fared worse with average Iowa Hip Rating scores of 90, 70, and 73 and substantial arthrosis in one of two, 14 of 18, and 21 of 24 hips. At mean followup of 41 years, this same patient population was reevaluated [8] demonstrating Iowa Hip Rating scores of 89, 81, and 73 and showing that12% of mild slips required additional surgery which was not specified.
In our opinion, however, there are limitations of these often-cited studies [3, 8]. First, the scoring system [16] used inadequately reflects moderate functional and motion losses that are important to this active population. Second, the 15% reported rate [3] of moderate or advanced arthrosis in subjects averaging 45 years is high when compared to a prevalence of 1.7% in those aged 45 to 49 [9]. Additionally, intermediate followup studies suggest patients have pain and functional limitation after mild SCFE [10, 12, 19]. Fraitzl et al. [12] evaluated 16 hips with slip angles ≤ 31º at average followup of 14.4 years. Tegner and Lysholm scores averaged 5.2 with nine subjects scoring 4 or less. This compares to an average score of 6.5 for similarly-aged asymptomatic volunteers [4]. Another series [10] of 49 hips treated with in situ pinning alone with an average followup of 6.1 years identified 15 painful hips, including 10 of 30 mild slips.
More importantly we believe, there is growing evidence that shows substantial articular damage after mild SCFE. Over 15 years ago, Futami et al. [13] assessed five hips arthroscopically at the time of in situ pinning. Anterosuperior acetabular cartilage erosion was present in all four hips visualized. Slip angles for these hips were 20°, 22°, and 31°; that for the fourth hip was not reported. Leunig et al. [17] treated 14 hips with prior SCFE and observed impingement in all hips. Acetabular cartilage damage was observed in 12 hips, including all three mild slips, 8 of 10 moderate slips, and the one severe slip. In mild to moderate slips, the metaphysis was observed to enter the joint, whereas in severe slips, the prominent metaphysis abutted the acetabular rim, preventing its entry into the acetabulum. In a subsequent evaluation of 30 hips [19], acetabular cartilage damage was graded as 2.3, 2.2, and 1.8 for mild, moderate, and severe slips. Most recently, a series [25] of 39 painful hips treated by dislocation revealed cartilage damage in 6 of 8 mild, 16 of 20 moderate, and 10 of 11 severe slips.
Consistent with this clinical evidence, computational studies have provided a clearer understanding of how articular damage occurs after mild SCFE. Rab [24], using a volume/surface model, identified the same two types of impingement that Leunig et al. [17] observed clinically. Rab termed them “inclusion” and “impaction” and proposed that “inclusion” may be more damaging. A CT modeling study of actual slips [22] demonstrated impingement in all slip severities.
Early followup of the first three hips treated with this protocol demonstrated asymptomatic patients, improved hip ROM, and no clinical evidence of impingement. Radiographic assessment showed increased epiphyseal-metaphyseal offsets and decreased alpha angles. Obviously, this combination of procedures can only be used for mild epiphyseal tilt and translation; for larger deformities, even substantial osteoplasty would not eliminate impingement and might critically decrease the neck’s structural integrity. Additionally, osteoplasty neither realigns the epiphysis with the femoral shaft nor increases the articular bearing area. Therefore, we recommend capital realignment for moderate and severe SCFE [19, 28].
We believe the ultimate goal of SCFE treatment should be to intervene before irreversible joint injury occurs and that, for mild SCFE, in situ pinning with immediate arthroscopic osteoplasty can reduce or even eliminate hip impingement, which is reported to lead to osteoarthritis of the hip [14, 27]. We recognize, however, that only long-term followup with comparison to a control group treated with in situ pinning alone can demonstrate whether our proposed technique decreases subsequent articular damage. Although we advise performing these procedures concomitantly, osteoplasty may be performed at a subsequent date. This is particularly true if the pinning surgeon is not a proficient hip arthroscopist, given that arthroscopy following an epiphyseal slip is technically demanding.
Acknowledgements
We thank James Voos, M.D. for his contribution to the design of this study and to the initial preparation of this manuscript.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Department of Orthopedics, Schulthess Clinic, Zürich, Switzerland.
References
- 1.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed] [Google Scholar]
- 2.Aronsson DD, Loder RT, Breur GJ, Weinstein SL. Slipped capital femoral epiphysis: current concepts. J Am Acad Orthop Surg. 2006;14:666–679. doi: 10.5435/00124635-200611000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Boyer DW, Mickelson MR, Ponseti IV. Slipped capital femoral epiphysis. Long-term follow-up study of one hundred and twenty-one patients. J Bone Joint Surg Am. 1981;63:85–95. [PubMed] [Google Scholar]
- 4.Briggs KK, Steadman JR, Hay CJ, Hines SL. Lysholm score and Tegner activity level in individuals with normal knees. Am J Sports Med. 2009;37:898–901. doi: 10.1177/0363546508330149. [DOI] [PubMed] [Google Scholar]
- 5.Byrd JW. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10:275–280. doi: 10.1016/S0749-8063(05)80111-2. [DOI] [PubMed] [Google Scholar]
- 6.Byrd JW, Pappas JN, Pedley MJ. Hip arthroscopy: an anatomic study of portal placement and relationship to the extra-articular structures. Arthroscopy. 1995;11:418–423. doi: 10.1016/0749-8063(95)90193-0. [DOI] [PubMed] [Google Scholar]
- 7.Carney BT, Weinstein SL. Natural history of untreated chronic slipped capital femoral epiphysis. Clin Orthop Relat Res. 1996;322:43–47. doi: 10.1097/00003086-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Carney BT, Weinstein SL, Noble J. Long-term follow-up of slipped capital femoral epiphysis. J Bone Joint Surg Am. 1991;73:667–674. [PubMed] [Google Scholar]
- 9.Dagenais S, Garbedian S, Wai EK. Systematic review of the prevalence of radiographic primary hip osteoarthritis. Clin Orthop Relat Res. 2009;467:623–637. doi: 10.1007/s11999-008-0625-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dodds MK, McCormack D, Mulhall KJ. Femoroacetabular impingement after slipped capital femoral epiphysis: does slip severity predict clinical symptoms? J Pediatr Orthop. 2009;29:535–539. doi: 10.1097/BPO.0b013e3181b2b3a3. [DOI] [PubMed] [Google Scholar]
- 11.Eijer H, Leunig M, Mahomed M, Ganz R. Cross-table lateral radiograph for screening of anterior femoral head-neck offset in patients with femoroacetabular impingement. Hip Int. 2001;11:37–41. [Google Scholar]
- 12.Fraitzl CR, Kafer W, Nelitz M, Reichel H. Radiological evidence of femoroacetabular impingement in mild slipped capital femoral epiphysis: a mean follow-up of 14.4 years after pinning in situ. J Bone Joint Surg Br. 2007;89:1592–1596. doi: 10.1302/0301-620X.89B12.19637. [DOI] [PubMed] [Google Scholar]
- 13.Futami T, Kasahara Y, Suzuki S, Seto Y, Ushikubo S. Arthroscopy for slipped capital femoral epiphysis. J Pediatr Orthop. 1992;12:592–597. [PubMed] [Google Scholar]
- 14.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ilizaliturri VM, Jr, Nossa-Barrera JM, Acosta-Rodriguez E, Camacho-Galindo J. Arthroscopic treatment of femoroacetabular impingement secondary to paediatric hip disorders. J Bone Joint Surg Br. 2007;89:1025–1030. doi: 10.1302/0301-620X.89B8.19152. [DOI] [PubMed] [Google Scholar]
- 16.Larson CB. Rating scale for hip disabilities. Clin Orthop Relat Res. 1963;31:85–93. doi: 10.1097/00003086-196300310-00011. [DOI] [PubMed] [Google Scholar]
- 17.Leunig M, Casillas MM, Hamlet M, Hersche O, Notzli H, Slongo T, Ganz R. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand. 2000;71:370–375. doi: 10.1080/000164700317393367. [DOI] [PubMed] [Google Scholar]
- 18.Leunig M, Fraitzl CR, Ganz R. Early damage to the acetabular cartilage in slipped capital femoral epiphysis. Therapeutic consequences [in German] Orthopade. 2002;31:894–899. doi: 10.1007/s00132-002-0378-x. [DOI] [PubMed] [Google Scholar]
- 19.Leunig M, Slongo T, Ganz R. Subcapital realignment in slipped capital femoral epiphysis: surgical hip dislocation and trimming of the stable trochanter to protect the perfusion of the epiphysis. Instr Course Lect. 2008;57:499–507. [PubMed] [Google Scholar]
- 20.Loder RT, Aronsson DD, Weinstein SL, Breur GJ, Ganz R, Leunig M. Slipped capital femoral epiphysis. Instr Course Lect. 2008;57:473–498. [PubMed] [Google Scholar]
- 21.MacDonald SJ, Garbuz D, Ganz R. Clinical evaluation of the symptomatic young adult hip. Sem Arthroplasty. 1997;8:3–9. [Google Scholar]
- 22.Mamisch TC, Kim YJ, Richolt JA, Millis MB, Kordelle J. Femoral morphology due to impingement influences the range of motion in slipped capital femoral epiphysis. Clin Orthop Relat Res. 2009;467:692–698. doi: 10.1007/s11999-008-0477-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 24.Rab GT. The geometry of slipped capital femoral epiphysis: implications for movement, impingement, and corrective osteotomy. J Pediatr Orthop. 1999;19:419–424. doi: 10.1097/00004694-199907000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Sink EL, Zaltz I, Heare T, Dayton M. Acetabular cartilage and labral damage observed during surgical hip dislocation for stable slipped capital femoral epiphysis. J Pediatr Orthop.30;1:26–30. [DOI] [PubMed]
- 26.Southwick WO. Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J Bone Joint Surg Am. 1967;49:807–835. [PubMed] [Google Scholar]
- 27.Wagner S, Hofstetter W, Chiquet M, Mainil-Varlet P, Stauffer E, Ganz R, Siebenrock KA. Early osteoarthritic changes of human femoral head cartilage subsequent to femoro-acetabular impingement. Osteoarthritis Cartilage. 2003;11:508–518. doi: 10.1016/S1063-4584(03)00075-X. [DOI] [PubMed] [Google Scholar]
- 28.Ziebarth K, Zilkens C, Spencer S, Leunig M, Ganz R, Kim YJ. Capital realignment for moderate and severe SCFE using a modified Dunn procedure. Clin Orthop Relat Res. 2009;467:704–716. doi: 10.1007/s11999-008-0687-4. [DOI] [PMC free article] [PubMed] [Google Scholar]